Abstract
Objective
We examined the relationship between trimester of SARS-CoV-2 infection, illness severity, and risk for preterm birth.
Study design
We analyzed data for 6336 pregnant persons with SARS-CoV-2 infection in 2020 in the United States. Risk ratios for preterm birth were calculated for illness severity, trimester of infection, and illness severity stratified by trimester of infection adjusted for age, selected underlying medical conditions, and pregnancy complications.
Result
Pregnant persons with critical COVID-19 or asymptomatic infection, compared to mild COVID-19, in the second or third trimester were at increased risk of preterm birth. Pregnant persons with moderate-to-severe COVID-19 did not show increased risk of preterm birth in any trimester.
Conclusion
Critical COVID-19 in the second or third trimester was associated with increased risk of preterm birth. This finding can be used to guide prevention strategies, including vaccination, and inform clinical practices for pregnant persons.
Similar content being viewed by others
Introduction
Pregnant persons with SARS-CoV-2 infection are at increased risk of preterm birth [1,2,3,4,5]. However, the relationship between trimester of SARS-CoV-2 infection, illness severity, and preterm birth is not fully understood. SARS-CoV-2 infection is associated with maternal systemic inflammatory response and placental inflammation which may contribute to preterm birth [6]. Placental hypoperfusion can contribute to fetal growth restriction and non-reassuring fetal heart rate tracing which can increase risk of fetal demise and small-for-gestational age [6,7,8,9,10,11].
Observational studies show neonates were delivered earlier to persons with symptomatic, rather than asymptomatic, COVID-19 [2, 12]. Previous studies suggest increased risk of preterm birth among persons with severe COVID-19, however, study populations were limited to those with infection detected at hospital admission for delivery, or included those no longer at risk of preterm delivery (i.e., those with SARS-CoV-2 infection ≥37 weeks gestation) [2, 3, 13, 14]. A study including SARS-CoV-2 infection at any point during pregnancy reported that pregnant persons may be more susceptible to preterm delivery if SARS-CoV-2 infection occurred after 24 weeks gestation; however, the role of illness severity in this association is unclear [15].
Using data from a mother-infant linked longitudinal surveillance cohort, we examined trimester of SARS-CoV-2 infection and COVID-19 severity among pregnant persons and risk of preterm birth, adjusting for maternal age, selected underlying conditions, and pregnancy complications. We also investigated how trimester of infection modifies the relationship between COVID-19 severity and preterm birth. Understanding the association of trimester of SARS-CoV-2 infection and COVID-19 severity with preterm birth may guide strategies to improve uptake in prevention efforts against SARS-CoV-2, such as vaccination. We hypothesize that moderate-to-severe and critical COVID-19 during the third trimester is associated with increased risk of preterm birth.
Methods
The Surveillance for Emerging Threats to Mothers and Babies Network (SET-NET) conducts population-based longitudinal surveillance of pregnant persons and their infants to understand the impact of emerging and reemerging threats. Methods have been described previously [16]. Briefly, state, local, or territorial health departments from 21 jurisdictions in the United States (Arkansas, California [excluding Los Angeles County], Georgia, Houston, Iowa, Los Angeles County, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Nebraska, New Hampshire, New Jersey, New York [excluding New York City], Pennsylvania [excluding Philadelphia], Philadelphia, Puerto Rico, Tennessee, US Virgin Islands, and Washington) collected information on pregnancy outcomes among persons with SARS-CoV-2 infection in pregnancy during January 20-December 31, 2020, and reported these data to CDC by September 3, 2021. CDC receives these data on pregnant persons with positive SARS-CoV-2 infection confirmed by nucleic acid amplification testing (NAAT) during pregnancy through the day of delivery [17].
Reporting jurisdictions collect data on pregnant persons through reporting of pregnancy status in COVID-19 case surveillance, or through linkages of case surveillance data with existing local data systems, such as birth certificates, to determine if infection occurred during a pregnancy. Additional data elements are abstracted from maternal and infant medical records from the birth hospitalization. Of the 21 jurisdictions included in this analysis, trained staff from seventeen participating jurisdictions abstracted medical records for all mother-infant pairs meeting inclusion criteria, while staff from four jurisdictions used a random sampling approach to identify a subset of pregnancies for medical record abstraction. We weighted records abstracted based on the random sample to account for selection probability and nonresponse such that the sampling weights totaled the number of pregnancies meeting the case definition [18].
Preterm birth (<37 weeks gestation) among liveborn infants was the primary outcome. Information about gestational age at birth was obtained from birth certificates or abstracted from medical records. For birth certificate data, obstetric estimate of gestational age was obtained [19]. For medical records, gestational age was estimated from reported information on gestational age at birth or by calculating gestational age from reported estimated delivery date (EDD) or last menstrual period (LMP); abstractors were instructed to prioritize EDD determined by first trimester ultrasound.
We also assessed labor induction and mode of delivery in this analysis. Indications for induction included past due date or post-dates; prelabor rupture of membranes; maternal or labor-related conditions such as pre-eclampsia, maternal respiratory distress, and abnormal labor (failure to progress or descend); and fetal conditions such as non-reassuring antenatal fetal test, oligohydramnios, fetal growth restriction, and poor interval fetal growth. Emergent cesarean deliveries included those indicated for urgent maternal conditions such as maternal decompensation, or fetal conditions such as non-reassuring fetal testing, or uterine rupture. Non-emergent cesarean deliveries included those planned, scheduled, or indicated for reasons such as breech presentation, history of previous cesarean deliveries, failed induction, arrest of labor in the first or second stage.
Trimester of infection was determined by gestational age at date of first positive SARS-CoV-2 molecular test. Trimester was categorized as first: <14 weeks, second: 14–27 weeks, and third: 28–36 weeks.
Illness severity categories (asymptomatic infection, mild, moderate-to-severe, and critical), defined in a previous analysis of SET-NET data [20], were adapted from National Institutes of Health (NIH) and World Health Organization (WHO) severity of illness categories [21, 22]. We classified illness severity using a hierarchy prioritizing indications of critical disease first (intensive care unit [ICU] admission, invasive ventilation, complications, such as acute respiratory distress syndrome or extracorporeal membrane oxygenation, and death), followed by moderate-to-severe disease (use of COVID-19 therapies and severe symptoms, such as shortness of breath with fever or cough), followed by mild symptomatic disease and asymptomatic infection. Asymptomatic infection required report of no symptoms; absence of reported symptoms was not sufficient to meet this criterion. Pregnant persons with missing data on these indications were classified as having insufficient information and were excluded from analysis. We conducted a sensitivity analysis and compared the prevalence of preterm birth, underlying conditions, and trimester of SARS-CoV-2 infection among pregnant persons excluded from the analysis due to insufficient information with our included study population.
The current analysis was limited to pregnant persons with laboratory-confirmed SARS-CoV-2 infection occurring at <37 weeks gestation in 2020 and who delivered a live singleton infant. To avoid overestimating the risk of preterm birth from reporting bias, we limited our analysis to pregnancies with at least 47 weeks (43 weeks gestation plus 4 weeks of reporting lag) between calculated LMP (using the gestational dating methods described above) and the end of the reporting period (September 3, 2021).
Unadjusted and adjusted risk ratios (aRR) and 95% confidence intervals (CI) for preterm birth for trimester of SARS-CoV-2 infection (referent = first), illness severity (referent = mild), and illness severity stratified by trimester of infection were estimated by Cox regression with constant time at risk, which estimates prevalence ratios using survey procedures to account for sampling [23]. Mild illness was used as the referent, given the potential detection bias of asymptomatic people presenting for preterm delivery and detected incidentally because of universal screening protocols. Minimum sufficient adjustment variables were determined using a directed acyclic graph (Appendix 1) and included maternal age (in years) as a continuous variable, presence of one or more of the following underlying conditions: pre-pregnancy obesity, chronic lung disease, chronic hypertension, diabetes mellitus type 1 or 2, cardiovascular disease, immunosuppression, and presence of gestational diabetes or hypertensive disorders of pregnancy. We conducted a sensitivity analysis to include adjustment for race/ethnicity to compare any differences in the magnitude or direction of associations. In addition, a time-to-event analysis examined days to delivery after SARS-CoV-2 infection. Kaplan-Meier curves were generated to compare the percentage of persons still pregnant after SARS-CoV-2 infection by illness severity, stratified by trimester of infection. The Wilcoxon test was used to determine differences in days to delivery after infection among persons with mild, moderate-to-severe, or critical COVID-19. Analyses were conducted using SAS 9.4 software and survey procedures to account for jurisdiction, strata, and sampling weights [24]. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy [25].
Results
Jurisdictions reported 22,278 pregnant persons infected with SARS-CoV-2 between January 20 and December 31, 2020. Of these, 8754 (39.3%) had sufficient information for illness severity classification; however, 27.6% of those with sufficient information were excluded due to one of the following reasons: <47 weeks duration between calculated LMP and the end of the reporting period, multiple gestation pregnancy, did not deliver between 22 and <43 weeks, or infection at ≥37 weeks gestation. Overall, 6336 (28.4%) persons met inclusion criteria (Fig. 1). Pregnant persons were most commonly 25–34 years of age (57.1%), Hispanic or Latino ethnicity (52.2%), enrolled in Medicaid at delivery (50.7%), infected in the third trimester with SARS-CoV-2 (46.5%), and had term deliveries (89.0%) (Table 1). Black, non-Hispanic pregnant persons represented 13.0% of the population. At least one underlying medical condition was reported for 37.5% of pregnant persons, with prepregnancy obesity being the most common condition (36.6%). Gestational diabetes was reported in 12.3% of people and hypertensive disorders of pregnancy were reported in 13.1%. Illness severity varied as follows: 57.3% experienced mild COVID-19, 25.0% moderate-to-severe, 3.5% critical, and 14.2% asymptomatic infection.
SARS-CoV-2 severe acute respiratory syndrome coronavirus 2, NAAT nucleic acid amplification testing 1To avoid overestimating preterm birth from reporting bias, we limited to pregnancies with at least 47 weeks (43 weeks gestation plus 4 weeks of reporting lag) between calculated LMP and the end of the reporting period (September 3, 2021). 2We weighted records abstracted based on the random sample to account for selection probability and nonresponse such that the sampling weights totaled the number of pregnancies meeting the case definition.
Among 862 infants born preterm (11.0%), 5.5% were extremely preterm (22–27 weeks), 9.6% were early preterm (28–31 weeks), 9.7% were moderately preterm (32–33 weeks), and 75.2% were late preterm (34–36 weeks) (Table 1). Among persons who delivered preterm, most had mild COVID-19 (39.7%), were infected with SARS-CoV-2 in the third trimester (56.9%) (Table 2) and were infected at least 15 days before delivery (58.5%) (data not shown).
Persons infected with SARS-CoV-2 in the third trimester were at increased risk of preterm birth compared with those infected in the first trimester (aRR: 1.8; 95% CI: 1.3–2.7) (Table 2). Compared with pregnant persons who experienced mild COVID-19, those with critical COVID-19 (aRR: 4.6; 95% CI: 3.0–6.9) or asymptomatic infection (aRR: 2.6; 95% CI: 1.7–3.9) were at increased risk of preterm birth. Pregnant persons experiencing moderate-to-severe COVID-19, compared with mild, did not have an increased risk of preterm birth (aRR: 1.0; 95% CI: 0.7–1.5).
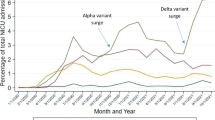
When stratified by trimester of infection, risk of preterm birth was elevated for pregnant persons with critical COVID-19 (aRRs 4.0–4.6) in the second and third trimesters and with asymptomatic infection in all three trimesters (aRRs 2.1–3.4) (Table 2). The association between preterm birth and critical COVID-19 in the first trimester was not estimated due to small cell sizes. Among infections occurring during the second or third trimester, critical COVID-19 was associated with shorter time from infection to delivery, compared with mild COVID-19 (p < 0.001 and p = 0.02, respectively) (Fig. 2). The median number of days to delivery from SARS-COV-2 infection for pregnant persons with critical COVID-19 was 86 among those infected in the second trimester, and 13 among those infected in the third trimester.
SARS-CoV-2 severe acute respiratory syndrome coronavirus 2, COVID-19 Coronavirus disease 2019 Dotted lines indicated median time from infection to birth at each level of COVID-19 severity. A SARS-CoV-2 infection occurring in the first trimester. B SARS-CoV-2 infection occurring in the second trimester. C SARS-CoV-2 infection occurring in the third trimester.
Nearly two-thirds of pregnant persons did not have an induction of labor (65.7%), regardless of disease severity or trimester of infection (Table 3). Among those induced, the most common reason for induction was maternal condition (58.3%). Where mode of delivery was known (96.7%), most persons delivered vaginally (64.7%), whereas 35.3% delivered by cesarean. Among those who delivered by cesarean, non-emergent was reported in 71.3%, and emergent was reported in 28.7%. Rates of cesarean deliveries remained similar by trimester of infection and for asymptomatic and mild COVID-19. Nearly half of those with moderate-to-severe or critical COVID-19 delivered by cesarean, with most critical COVID-19 cesarean deliveries as emergent (76.2%). Among persons with critical COVID-19 who delivered by emergent cesarean, the most reported reason for emergent cesarean was maternal condition (75.4%).
Discussion
In this analysis of pregnant persons with SARS-CoV-2 infection from 2020, those with critical COVID-19 in the second or third trimester had four times the risk of preterm birth compared with pregnant persons with mild COVID-19. Moderate-to-severe COVID-19 in any trimester was not associated with increased risk of preterm birth. Critical COVID-19, compared with mild, was associated with shorter time to delivery when infection occurred during the second or third trimester. Pregnant persons with asymptomatic infection in any trimester had increased risk of preterm birth. Although we observed an increased risk of preterm birth for pregnant persons with critical COVID-19 or asymptomatic infection in the second trimester, confidence intervals were wide, suggesting that associations be interpreted with caution.
Among persons with critical COVID-19, we observed higher frequency of emergent cesarean deliveries due to maternal condition, and maternal condition as the most common reason for labor induction. This is consistent with previous studies in which preterm birth was increased among mothers whose worsening COVID-19 symptoms led to obstetric intervention [26, 27]. Studies reported an increased risk of medically-indicated preterm birth among pregnant persons with COVID-19, and a higher prevalence of medically-indicated preterm birth among persons with severe-critical COVID-19 [2, 14].
Preterm birth rates are higher among non-Hispanic Black persons than for White non-Hispanic, Asian, or Hispanic persons in the United States [28, 29]. We conducted a sensitivity analysis by including race/ethnicity in our models, and adjusted risk ratios did not differ.
Findings from our study can be used to counsel patients about the importance of vaccination in order to reduce risk of preterm birth. Pregnant persons are at increased risk for severe COVID-19 [4, 30, 31], and our findings suggest that those with critical COVID-19 are at higher risk of preterm birth. Our study did not find increased risk of preterm birth among persons with moderate-to-severe COVID-19; however, it is important to note that the grouping of moderate and severe disease may mask any increased risk of preterm birth among persons with severe COVID-19. Our study was unable to distinguish between moderate and severe COVID-19, as the surveillance system does not collect data on use of supplemental oxygen.
Little is known about the impact of asymptomatic SARS-CoV-2 infection on pregnancy outcomes or placental pathology. In this study, asymptomatic persons had increased risk of preterm birth, however this may be attributed to screening bias, residual confounding, or subclinical processes impacting gestation. Among asymptomatic persons infected with SARS-CoV-2 prior to 37 weeks gestation, the proportion of preterm deliveries was high (20%). Pregnant persons may have been diagnosed upon admission for delivery, however, to assess risk of preterm birth, we excluded those with infection > =37 weeks gestation, potentially overestimating the risk of preterm delivery among asymptomatic persons. However, screening at admission does not account completely for the increased risk, as asymptomatic persons infected in the first trimester also had elevated risk of preterm birth. Further research is needed to understand whether this finding could be due to subclinical processes that may contribute to preterm birth. Placental inflammation in the setting of COVID-19 has been described and has been proposed as a possible mechanism for adverse pregnancy outcomes (including stillbirth) and may be part of the pathway for preterm delivery among pregnant people with COVID-19. Given a lack of systematic testing and reporting of placental testing and pathology, we are unable to assess the impact of otherwise asymptomatic infection on the placenta in this surveillance network.
It is possible that the increased risk of preterm birth seen in pregnant persons with critical COVID-19 works through the mechanism of systemic inflammation and hypercoagulability. Among pregnant persons with severe COVID-19, an association between COVID-19 and higher rates of preeclampsia has been reported [7, 32]. It is unclear if COVID-19 causes a preeclampsia-like syndrome or if SARS-CoV-2 infection results in increased risk for preeclampsia. Systemic inflammation and hypercoagulability are features seen both in nonpregnant COVID-19 patients [33] and in preeclampsia [8, 10, 11].
Strengths of this study include the ability to define COVID-19 severity using data abstracted from medical records. In addition, analysis was limited to those at risk of preterm birth (i.e., SARS-CoV-2-infection <37 weeks), and to those who had at least 47 weeks between LMP and end of reporting period to prevent overestimating the risk of preterm birth.
Study findings are subject to at least five limitations. First, a large proportion of pregnant persons (49%) could not be classified for COVID-19 severity due to insufficient information and were excluded from analysis. However, a sensitivity analysis revealed that prevalence of preterm birth, underlying conditions, and trimester of SARS-CoV-2 infection among excluded persons were similar to our included population. Second, data were gathered from sources that varied across jurisdictions, which might have led to misclassification of variables of interest, such as preterm birth and trimester of infection due to differing sources of gestational age. However, we implemented a conservative gestational dating approach to avoid overestimating preterm births [34, 35]. Third, mild COVID-19 or asymptomatic infection may be under ascertained or misclassified as such patients may not have sought care and, therefore, had no medical record. Fourth, our population captures infections occurring in 2020 when COVID-19 vaccinations were not yet available and before circulation of Delta (B.1.617.2) and Omicron (B.1.1.529) variants. Fifth, SET-NET data do not capture history of preterm delivery, nor whether the preterm delivery was medically indicated.
This study describes a large population-based cohort of persons with SARS-CoV-2 infection during pregnancy and preterm birth. Critical COVID-19 occurring in the second or third trimester was associated with increased risk of preterm birth and delivery occurred sooner after infection compared with mild COVID-19. In addition to being at increased risk for severe COVID-19 [4, 30, 31], pregnant persons with SARS-CoV-2 infection are at increased risk for preterm birth [36], and these data further suggest the association is particularly evident for those who experience critical illness. Individuals who are pregnant or planning to become pregnant should be vaccinated against COVID-19 to mitigate serious illness, death, and adverse pregnancy outcomes such as preterm birth [37].
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to their protection under an Assurance of Confidentiality (Section 308(d) of the Public Health Service Act, 42 U.S.C §242 m(d)), which prohibits use or disclosure of any identifiable or potentially identifiable information collected under the Assurance for purposes other than those set out in the Assurance, but could be made available from the corresponding author on reasonable request.
References
Martinez-Perez O, Prats Rodriguez P, Muner Hernandez M, Encinas Pardilla MB, Perez Perez N, Vila Hernandez MR, et al. The association between SARS-CoV-2 infection and preterm delivery: a prospective study with a multivariable analysis. BMC Pregnancy Child. 2021;21:273 https://doi.org/10.1186/s12884-021-03742-4.
Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: The INTERCOVID multinational cohort study. JAMA Pediatr. 2021. https://doi.org/10.1001/jamapediatrics.2021.1050.
Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. Can Med Assoc J. 2021;193:E540–8. https://doi.org/10.1503/cmaj.202604.
Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. https://doi.org/10.1136/bmj.m3320.
McClymont E, Albert AY, Alton GD, Boucoiran I, Castillo E, Fell DB, et al. Association of SARS-CoV-2 infection during pregnancy with maternal and perinatal outcomes. JAMA. 2022;327:1983–91. https://doi.org/10.1001/jama.2022.5906.
Patberg ET, Adams T, Rekawek P, Vahanian SA, Akerman M, Hernandez A, et al. Coronavirus disease 2019 infection and placental histopathology in women delivering at term. Am J Obstet Gynecol. 2021;224:382.e1–82.e18. https://doi.org/10.1016/j.ajog.2020.10.020.
Mendoza M, Garcia-Ruiz I, Maiz N, Rodo C, Garcia-Manau P, Serrano B, et al. Pre-eclampsia-like syndrome induced by severe COVID-19: a prospective observational study. BJOG. 2020;127:1374–80. https://doi.org/10.1111/1471-0528.16339.
Meyer JA, Roman AS, Limaye M, Grossman TB, Flaifel A, Vaz MJ, et al. Association of SARS-CoV-2 placental histopathology findings with maternal-fetal comorbidities and severity of COVID-19 hypoxia. J Matern Fetal Neonatal Med. 2021:1-7. https://doi.org/10.1080/14767058.2021.1977791.
Girolamo RD, Khalil A, Alameddine S, D’Angelo E, Galliani C, Matarrelli B, et al. Placental histopathology after SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2021:100468. https://doi.org/10.1016/j.ajogmf.2021.100468.
Shanes ED, Mithal LB, Otero S, Azad HA, Miller ES, Goldstein JA. Placental pathology in COVID-19. Am J Clin Pathol. 2020;154:23–32. https://doi.org/10.1093/ajcp/aqaa089.
Narang K, Enninga EAL, Gunaratne MDSK, Ibirogba ER, Trad ATA, Elrefaei A, et al. SARS-CoV-2 infection and COVID-19 during pregnancy: a multidisciplinary review. Mayo Clin Proc. 2020;95:1750–65. https://doi.org/10.1016/j.mayocp.2020.05.011.
Dumitriu D, Emeruwa UN, Hanft E, Liao GV, Ludwig E, Walzer L, et al. Outcomes of neonates born to mothers with severe acute respiratory syndrome coronavirus 2 infection at a large medical center in New York City. JAMA Pediatr. 2021;175:157–67. https://doi.org/10.1001/jamapediatrics.2020.4298.
Lokken EM, Huebner EM, Taylor GG, Hendrickson S, Vanderhoeven J, Kachikis A, et al. Disease severity, pregnancy outcomes, and maternal deaths among pregnant patients with severe acute respiratory syndrome coronavirus 2 infection in Washington State. Am J Obstet Gynecol. 2021;225:77.e1–77.e14. https://doi.org/10.1016/j.ajog.2020.12.1221.
Metz TD, Clifton RG, Hughes BL, Sandoval G, Saade GR, Grobman WA, et al. Disease severity and perinatal outcomes of pregnant patients with Coronavirus disease 2019 (COVID-19). Obstet Gynecol. 2021;137:571–80. https://doi.org/10.1097/aog.0000000000004339.
Badr D, Picone O, Bevilacqua E, Carlin A, Meli F, Sibiude J, et al. Severe acute respiratory syndrome coronavirus 2 and pregnancy outcomes according to gestational age at time of infection. Emerg Infect Dis. 2021;27:2535 https://doi.org/10.3201/eid2710.211394.
Woodworth KR, Reynolds MR, Burkel V, Gates C, Eckert V, McDermott C, et al. A preparedness model for mother-baby linked longitudinal surveillance for emerging threats. Matern Child Health J. 2021;25:198–206. https://doi.org/10.1007/s10995-020-03106-y.
Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19) 2020 Interim Case Definition, Approved August 5, 2020. Accessed November 2, 2021. https://ndc.services.cdc.gov/case-definitions/coronavirus-disease-2019-2020-08-05.
Centers for Disease Control and Prevention. Sampling and Weighting Methods for COVID-19 End of Pregnancy Medical Record Abstraction. Accessed December 1, 2021. https://www.cdc.gov/ncbddd/set-net/documents/set-net-pregnancy-sampling-white-paper-508.pdf.
Centers for Disease Control and Prevention. Obstetric estimate of gestation at delivery. Accessed December 27, 2021. https://www.cdc.gov/nchs/nvss/facility-worksheets-guide/30.htm?Sort=URL%3A%3Aasc&Categories=Newborn%20Information.
Galang RR, Newton SM, Woodworth KR, Griffin I, Oduyebo T, Sancken CL, et al. Risk factors for illness severity among pregnant women with confirmed severe acute respiratory syndrome Coronavirus 2 Infection-Surveillance for Emerging Threats to Mothers and Babies Network, 22 State, Local, and Territorial Health Departments, 29 March 2020-5 March 2021. Clin Infect Dis. 2021;73:S17–23. https://doi.org/10.1093/cid/ciab432.
National Institutes of Health – COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines 2020. Accessed December 27, 2021. https://www.covid19treatmentguidelines.nih.gov.
World Health Organization. Clinical management of COVID-19: interim guidance. Accessed December 27, 2021. https://apps.who.int/iris/handle/10665/332196.
Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21 https://doi.org/10.1186/1471-2288-3-21.
SAS/ACCESS 9.4 Interface to ADABAS: Reference [program]. Cary, NC: SAS Institute Inc., 2013.
Department of Health and Human Services. 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq. Accessed November 2, 2021. https://www.hhs.gov/ohrp/sites/default/files/ohrp/policy/ohrpregulations.pdf.
Sentilhes L, De Marcillac F, Jouffrieau C, Kuhn P, Thuet V, Hansmann Y, et al. Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol. 2020;223:914.e1–14.e15. https://doi.org/10.1016/j.ajog.2020.06.022.
Angelidou A, Sullivan K, Melvin PR, Shui JE, Goldfarb IT, Bartolome R, et al. Association of maternal perinatal SARS-CoV-2 infection with neonatal outcomes during the COVID-19 pandemic in Massachusetts. JAMA Netw Open. 2021;4:e217523 https://doi.org/10.1001/jamanetworkopen.2021.7523.
Grobman WA, Parker CB, Willinger M, Wing DA, Silver RM, Wapner RJ, et al. Racial disparities in adverse pregnancy outcomes and psychosocial stress. Obstet Gynecol. 2018;131:328–35. https://doi.org/10.1097/aog.0000000000002441.
Braveman P, Dominguez TP, Burke W, Dolan SM, Stevenson DK, Jackson FM, et al. Explaining the black-white disparity in preterm birth: a consensus statement from a multi-disciplinary scientific work group convened by the March of dimes. Front Reprod Health. 2021;3. https://doi.org/10.3389/frph.2021.684207.
Martinez-Portilla RJ, Sotiriadis A, Chatzakis C, Torres-Torres J, Espino YSS, Sandoval-Mandujano K, et al. Pregnant women with SARS-CoV-2 infection are at higher risk of death and pneumonia: propensity score matched analysis of a nationwide prospective cohort (COV19Mx). Ultrasound Obstet Gynecol. 2021;57:224–31. https://doi.org/10.1002/uog.23575.
Zambrano LD, Ellington S, Strid P, Galang RR, Oduyebo T, Tong VT, et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1641–7. https://doi.org/10.15585/mmwr.mm6944e3.
Di Mascio D, Khalil A, Saccone G, Rizzo G, Buca D, Liberati M, et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2020;2:100107–07. https://doi.org/10.1016/j.ajogmf.2020.100107.
Yin S, Huang M, Li D, Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolys. 2021;51:1107–10. https://doi.org/10.1007/s11239-020-02105-8.
The American College of Obstetricians and Gynecologists. Methods for Estimating the Due Date. Accessed November 18, 2021. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/05/methods-for-estimating-the-due-date.
Martin JA, Osterman MJ, Kirmeyer SE, Gregory EC. Measuring gestational age in vital statistics data: transitioning to the obstetric estimate. Natl Vital- Stat Rep. 2015;64:1–20.
Centers for Disease Control and Prevention. Pregnant and Recently Pregnant People. Accessed December 27, 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html.
Centers for Disease Control and Prevention. COVID-19 Vaccination for Pregnant People to Prevent Serious Illness, Deaths, and Adverse Pregnancy Outcomes from COVID-19 2021. Accessed December 2, 2021. https://emergency.cdc.gov/han/2021/han00453.asp.
Acknowledgements
We acknowledge Theo Calloway, William Greenfield, Mallory Jayroe, Rachel Lee Jones, Tabatha M. Scarborough, Wanda Simon, Arkansas Department of Health; Valorie Eckert, Similoluwa Sowunmi, Barbara Warmerdam, California Department of Health; Susan Manning, CDC, Massachusetts Department of Public Health; Erika Fuchs, CDC, Nebraska Department of Health and Human Services; Amber Palmer, Chickasaw Health Consulting; J. Michael Bryan, Raghav Mehta, Cristina Meza, Victoria Sanon, Anam Syed, Bill Williamson, Georgia Department of Public Health; Jaimee Maranon, Danacamile Roscom, High Sierra AHEC; Tahani Hamdan, Kirstin Short, Houston Health Department; Kimberly N. Piper, Iowa Department of Public Health; Savij Apichon, Emily Barnes, Alison Ryan, Jordan Sontz, Los Angeles County Department of Public Health; Ademilola Badejo, Aliya Marroquin, Maryland Department of Health; Hanna M. Shephard, Mahsa Yazdy, Massachusetts Department of Public Health; Shannon Baack, Ona Loper, Kristen Ojo, Minnesota Department of Health; Natasha Nyquist-Smith, High Sierra AHEC; Ashlyn Torrez, Nevada Department of Health and Human Services; Suzann Beauregard, Mariko Geiger, Katrina Hansen, Hannah Thomas, New Hampshire Department of Health and Human Services; Nadia Thomas, New York State Department of Health; Abigail Davis, Allison Longenberger, Lauren Orkis, Bethany Reynolds, Sharon Watkins, Pennsylvania Department of Health; My-Phuong Huynh, Philadelphia Department of Public Health; Leishla Nieves-Ferrer, Miguel Valencia-Prado, Puerto Rico Department of Health; Wendy Nembhard, University of Arkansas for Medical Sciences; Kristin M. Conway, Soman Puzhankara, University of Iowa College of Public Health; Cosme Harrison, USVI Department of Health; Vivian Hawkins, Deborah Mbotha, Washington State Department of Health.
Funding
This study was performed as regular work of the Centers for Disease Control and Prevention (CDC). This work is supported by the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement (CK19–1904) and through contractual mechanisms, including the Local Health Department Initiative. This project was supported in part by an appointment to the Research Participation Program at the CDC administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the CDC.
Author information
Authors and Affiliations
Contributions
SN, EO, KRW, SF, RG, CSM, and VT conceptualized the analysis, drafted the initial manuscript, and reviewed and revised the manuscript. ER and EO carried out all analyses and reviewed and revised the manuscript. MR, EH, JS, EN, JB, VN, ML, NL, PD, LI, AS, SS, CDL, TC, EM, SK, PR, CF, EE, KS, AH, EAB, and SG assisted in interpreting findings and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Newton, S.M., Reeves, E.L., O’Malley Olsen, E. et al. Preterm birth among pregnant persons with severe acute respiratory syndrome Coronavirus 2 infection. J Perinatol 42, 1328–1337 (2022). https://doi.org/10.1038/s41372-022-01467-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01467-6
- Springer Nature America, Inc.