Abstract
Background
This study aimed to review evidence on the ability of red cell distribution width (RDW) to predict mortality and poor functional outcomes after acute ischemic stroke (AIS).
Methods
Databases of PubMed, CENTRAL, Scopus, Embase, and Web of Science were searched online from inception to 25th Jul 2023 for all studies reporting the association between RDW and outcomes as adjusted ratios. A random-effects meta-analysis was done. Meta-regression was conducted using multiple moderators.
Results
15 studies with 14,968 patients were included. Meta-analysis found that RDW, both as a categorical variable (OR: 2.10 95% CI: 1.74, 2.55 I2 = 42%) and continuous variable OR: 1.16 95% CI: 1.05, 1.28 I2 = 64%) was a significant predictor of mortality after AIS. Age and number of hypertensives were found to be significant moderators in the meta-regression. Also, high RDW, as a categorical variable (OR: 1.68 95% CI: 1.20, 2.35 I2 = 84%), was associated with significantly higher odds of poor functional outcomes after AIS, but not as a continuous variable (OR: 1.07 95% CI: 0.99, 1.16 I2 = 61%). Meta-regression showed that the association was stronger in small sample-sized studies.
Conclusion
RDW can be a useful, readily available, and cost-effective biomarker to rapidly stratify AIS patients at risk of poor outcomes. High RDW was consistently associated with an increased risk of mortality after AIS, however, its ability to predict poor functional outcomes needs to be verified by further studies.
Similar content being viewed by others
Introduction
Stroke is amongst the most common cerebrovascular diseases diagnosed around the world. About 16.9 million individuals suffer from stroke every year causing the second-highest number of deaths and a significant proportion of disability worldwide [1]. According to estimates about 87% of the cases are due to ischemia with age being the most important risk factor [2]. Nearly 3/4 of cases of stroke occur in patients aged ≥ 65 years [3]. Given the geriatric age group, patients with acute ischemic stroke (AIS) suffer routinely from long-term complications like neurological deficits, falls, fractures, infections, etc. The patients also frequently require rehabilitation and long-term nursing care which increases the emotional and financial burden on the caregivers and the healthcare system [4]. Owing to the high burden of stroke worldwide and the associated adverse events, it is necessary to identify markers that can accurately predict the prognosis of stroke.
Red blood cell distribution width (RDW) is a commonly used hematological marker that is based on the circulating red blood cell volume. It is routinely measured by automated cell counters during blood counts and is easily available in healthcare centers across the world. The marker demonstrates the red blood cell size variation in the blood sample and is derived from the distribution curve width and the mean cell size [5]. RDW is a good prognostic marker for several diseases like atrial fibrillation, cardiac failure, ischemic heart disease, pulmonary embolism, sepsis, renal disorders, hepatic disorders, AIS, and several malignant conditions [6,7,8,9,10,11,12]. Given its widespread availability and low cost, RDW is being recognized as an important biomarker that can provide early primary risk stratification of patients cost-effectively even in regions with scarce healthcare resources [13].
In recent times, several studies [14,15,16,17] have examined the ability of RDW to predict mortality and poor functional outcomes- the most important outcomes of AIS. However, the results of studies have differed owing to variations in the study populations, sample size, and cut-offs of RDW. Therefore, there is a need to assimilate data from published studies to provide quality evidence. With this aim, the current review was conducted to examine if RDW can predict mortality and poor functional outcomes after AIS.
Materials and methods
Search strategy and inclusion criteria
Based on the recommended guidelines, we prepared the review protocol and uploaded it on the international register PROSPERO (CRD42023445726). The study was performed based on the criteria of the Preferred Reporting Items for Statistic Reviews and Meta-Analyses statement [18]. Databases of PubMed, CENTRAL, Scopus, Embase, and Web of Science were searched online from inception to 25th Jul 2023 for English-language articles. Conference proceedings and unpublished or non-peer-reviewed data were not considered during the search.
All eligible studies had to meet the following criteria: (1) Prospective or retrospective cohort studies conducted on AIS patients or reporting AIS as a subgroup of all stroke patients. (2) Reporting association between RDW and mortality or poor functional outcomes after a stroke at any follow-up period. (3) The examined association was reported as a multivariable-adjusted effect size with 95% confidence intervals (CI). (4) Used RDW as either a continuous variable or divided it into groups for the analysis (as a categorical variable).
Studies not specifically reporting on AIS, not reporting outcomes, not conducting adjusted analysis, and duplicate studies were excluded.
The search strategy was formulated using the keywords: “RDW”, “red cell distribution”, “stroke”, “cerebral ischemia”, “brain infarction”, and “cerebral infarction”. Further details are demonstrated in Supplementary Table 1.
Two reviewers were involved in the search process which first began with title and abstract screening. Studies were excluded if the title or the abstract did not conform with the aims of this review. Full text was then obtained for all identified acceptable studies, or when the relevance of an article could not be determined. Disagreements were settled by consensus. The same process was performed for the full-text review. The bibliography of included studies was cross-referenced to discover further eligible studies.
Data extraction
Two reviewers performed the data extraction and assimilated information related to the year of the study, the author’s first name, sample size, age and gender, hypertension, diabetes, hyperlipidemia, timing of blood sample, cut-off of RDW, method of determination of cut-off, number of patients with high RDW, treatment of AIS, and follow-up. Outcome data of interest were mortality and poor functional outcome. Poor functional outcome was defined as a score of 3–6 on the modified ranking scale (mRS) [14,15,16,17].
According to the guidelines of the Newcastle-Ottawa Scale (NOS) [19], the included studies were judged for bias by two independent reviewers in the domains of selection of cohort, comparability, and outcome assessment. The three components were given points for questions included in the NOS. The total points available are: selection: 4; comparability: 2; and outcome assessment: 3.
Statistical analysis
All extracted numerical data were expressed as absolute numbers or proportions. The effect size on the association between RDW and outcome was pooled using Odds ratio (OR) with 95% CI. Separate analyses were conducted for RDW expressed as a continuous variable or as a categorical variable. Meta-analysis was conducted in a random-effects model using the software “Review Manager” (RevMan, version 5.3). Outliners were assessed using a sensitivity analysis involving the removal of one study at a time. The chi-square-based Q statistics and I2 statistic was used for inter-study heterogeneity. A p-value of < 0.10 for Q statistic and I2 > 50% meant substantial heterogeneity.
To examine the effect of various moderators, a meta-regression analysis was performed using “metaHUN: a web tool for meta-analysis” (Available at: http://softmed.hacettepe.edu.tr/metaHUN/). The moderators selected were sample size, age, male gender, hypertension, diabetes, hyperlipidemia, and cut-off of RDW. Meta-regression was performed only for the meta-analysis based on RDW as a categorical variable (high vs. low) and not for RDW as continuous variables. This was done owing to the paucity of data for the latter analysis.
Results
The two reviewers found 1376 articles from the databases. After electronic deduplication using EndNote, 594 were screened and 26 articles were identified by the reviewers for further analysis. The inter-reviewer rating for the selection of studies was high (kappa = 0.9). Finally, based on the inclusion criteria, 15 studies were included in the review [14,15,16,17, 20,21,22,23,24,25,26,27,28,29,30] (Fig. 1). No additional study was found from the reference list of included studies.
Baseline study details extracted by the authors are shown in Table 1. All were retrospective cohort studies. The articles were published in 14 years between 2009 and 2023. There was a predominance of Asian studies with seven studies from China, two from Korea, and one from Taiwan. The remaining studies were from the USA, Portugal, Italy, and Turkey. The pooled sample size of all studies was 14,968. All studies included elderly patients with a mean/median age of > 60 years. In five studies, the blood samples for RDW were taken within 24 h of admission while in the remaining studies, it was on admission. Three studies used RDW only as a continuous variable. In the remaining studies, the cut-off for high RDW varied from 13 to 16%. Absolute numbers of AIS patients with high RDW were not mentioned in most studies. Similarly, treatment was also not specified in the majority of studies. The follow-up duration ranged from reporting only in-hospital outcomes to up to 75 months. The reviewers judged the studies on NOS and awarded points ranging from 6 to 9. Raw data from the included studies analyzed in the meta-analysis is presented as Supplementary Table 2.
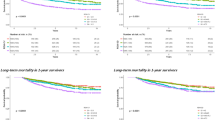
Examining the association between RDW as a categorical variable with a study-defined cut-off of high and low RDW, this meta-analysis noted that RDW was a significant predictor of mortality after AIS (OR: 2.10 95% CI: 1.74, 2.55 I2 = 42%) (Fig. 2). The review results failed to change on the exclusion of any study during the sensitivity analysis (results are not shown). Meta-regression outcomes are shown in Table 2. A significant positive association was noted for the moderators’ age and hypertensives. Higher age and percentage of hypertensives were associated with a stronger association between RDW and mortality. Only five studies used RDW as a continuous variable. Pooled analysis showed a significant association between the incremental increase of RDW and mortality after AIS (OR: 1.16 95% CI: 1.05, 1.28 I2 = 64%) (Fig. 3). Results remained significant on sensitivity analysis (results are not shown).
Using RDW as a categorical variable with a study-defined cut-off of high and low RDW, we found that high RDW was associated with significantly higher odds of poor functional outcomes after AIS (OR: 1.68 95% CI: 1.20, 2.35 I2 = 84%) (Fig. 4). The effect size did not lose its significance on sensitivity analysis (results are not shown). Outcomes of meta-regression are shown in Table 3. Except for the sample size, none of the moderators had a significant association with the effect size. It was noted that studies with lower sample sizes found a stronger association between RDW and poor functional outcomes. Only three studies used RDW as a continuous variable for examining poor functional outcomes. The meta-analysis did not find a significant association between the incremental increase of RDW and poor functional outcomes after AIS (OR: 1.07 95% CI: 0.99, 1.16 I2 = 61%) (Fig. 5).
Discussion
AIS is a leading cause of mortality around the world but there still exists a deficiency of simple biomarkers with can rapidly identify high-risk populations. Biomarkers are important for initial screening and prioritization of treatment to reduce the risk of adverse outcomes. In this context, RDW is a potential biomarker that is part of routine blood counts and can be examined dynamically in a cost-effective manner. Higher RDW means reduced deformability of the erythrocyte indicating damage to the microcirculatory blood flow which reduces tissue level oxygen supply [6]. Indeed, several studies have demonstrated a strong association between RDW and poor outcomes in multiple diseases [6,7,8,9,10,11,12]. Focusing on cerebrovascular diseases, high RDW has been associated with an increased risk of cerebral infarction and poor outcomes after aneurysmal subarachnoid hemorrhage [31]. RDW also predicts 30-day mortality after traumatic brain injury [32]. Lorente et al [33] have shown that RDW can be a good biomarker to predict mortality after spontaneous intracerebral hemorrhage. A previous meta-analysis has found that high RDW in the general population increases the risk of stroke occurrence by 53% [34]. In the same study, the authors also evaluated the prognostic ability of RDW for stroke but could include just eight studies. Furthermore, the study combined both crude and adjusted associations between RDW and outcomes.
The current review consolidated data from 15 studies in the literature to examine the prognostic ability of RDW for mortality and poor functional outcomes after AIS. We pooled only adjusted data from studies to reduce the risk of confounding. Owing to differences in the presentation of data, a separate analysis was conducted for studies using RDW as a continuous or categorical variable. In the first part of the meta-analysis, pooled data from eight studies showed that high RDW (ranging from 13 to 14.6%) was associated with a statistically significant 2.1 times increased risk of mortality as compared to those with lower RDW at or within 24 h of admission. Scrutiny of the forest plot revealed consistency of outcomes amongst studies for such association albeit with a difference in overall effect size. Individual studies found a 1.7 to 6.5 times increased risk of mortality amongst those with high RDW. On the other hand, when RDW was used as a continuous variable, the effect was subdued with pooled analysis showing only a 16% increased risk of mortality. These results show that when used as a categorical variable, RDW in the range of 13 to 14.6% is associated with significantly increased risk of mortality. Also, per unit increase in RDW is also associated with increased mortality. Given the baseline differences amongst studies for several variables which can modify survival after AIS, a meta-regression analysis was conducted. It was found that studies including more elderly patients and a higher number of hypertensives reported a stronger association between RDW and mortality. It is well known that the number of comorbidities increases with age. Also, the elderly have lower medicine compliance, altered metabolism, and higher drug interactions with polypharmacy which make them a unique risk group [35]. Research has shown that older age is a significant risk factor for mortality after AIS [36]. Likewise, elevated baseline blood pressure has been associated with higher clot burden, reduced chances of recanalization and good functional outcomes, increased infarct volumes, higher mortality, and early AIS recurrence [37, 38].
In the second part of the meta-analysis, we examined the relationship between RDW and poor functional outcomes after AIS only to find that patients with high RDW had a statistically significant 68% increased risk of poor functional outcomes. Unlike mortality outcome, the results of individual studies differed for this variable with two of the six studies demonstrating no significant prognostic role of AIS for poor functional outcomes. Scarce data with RDW as a continuous variable also demonstrated a non-significant effect. Importantly, the meta-regression analysis which examined the effect of several moderators for any influence on the pooled effect size showed a significant relationship for sample size. Studies with smaller sample sizes showed a stronger association between RDW and poor functional outcomes as compared to larger studies. This is a classic example of small study effects noted in the literature, wherein the effect size of smaller studies is often large due to publication bias. Smaller studies with significant results tend to be published irrespective of their quality and even there is a bias among authors to report significant results [39].
The mechanism between high RDW and AIS outcomes is still unclear but several explanations have been put forward. Inflammation has an important role in the pathophysiology of AIS with higher levels of inflammatory markers predicting poor functional outcomes and mortality after stroke [40]. High RDW may reflect higher baseline systemic inflammation since inflammatory cytokines can inhibit the bone marrow and delay erythropoietin-induced erythrocyte maturation [41]. Higher levels of C-reactive protein, interleukins, and tumor necrosis factor-alpha have been associated with higher RDW [42]. High oxidative stress levels have also been linked with anisocytosis and higher RDW [43]. Inflammation and oxidative stress can cause the development of atherosclerosis and research shows that RDW is positively associated with intima-media thickness of the carotid arteries [44]. Higher RDW also indicates a dysregulated state of erythrocyte homeostasis and impaired red blood cell production which can reduce tissue oxygenation after AIS contributing to delayed healing and poor outcomes [6].
The limitations of this review need to be commented on. Data used in this study is primarily from observational studies which have some inherent biases. Secondly, the study cohorts differed on multiple counts like baseline AIS severity, comorbidity levels, treatment protocols, and follow-up. It was unclear what medications were the patients prescribed at the time of sample collection and what were the erythrocyte sedimentation rate values. These differences could be the primary drivers of high heterogeneity noted in the meta-analyses. To partially overcome such variations, we used only adjusted data in the meta-analysis and conducted a meta-regression analysis to look for confounders. However, it is plausible that many unknown confounders could have been missed by the studies and affected the results. Thirdly, the variable cut-offs of RDW were a significant drawback. The meta-analysis showed the prognostic value of RDW for poor outcomes after AIS but could not suggest the optimal cut-off to identify high-risk patients. Lastly, the predominance of Asian and especially Chinese studies restricts the applicability of results to the global population.
To conclude, RDW can be a useful, readily available, and cost-effective biomarker to rapidly stratify AIS patients at risk of poor outcomes. High RDW was consistently associated with an increased risk of mortality after AIS, however, its ability to predict poor functional outcomes needs to be verified by further studies. Future studies should be of large sample sizes, from different geographical regions, and use similar cut-offs for better assessment of RDW as a biomarker for AIS.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Bushnell CD, Chaturvedi S, Gage KR, Herson PS, Hurn PD, Jiménez MC, et al. Sex differences in stroke: challenges and opportunities. J Cereb Blood Flow Metab. 2018;38:2179–91. https://doi.org/10.1177/0271678X18793324.
Saini V, Guada L, Yavagal DR. Global Epidemiology of Stroke and Access to acute ischemic stroke interventions. Neurology. 2021;97(20 Suppl 2):S6–16. https://doi.org/10.1212/WNL.0000000000012781.
Nimjee SM, Akhter AS, Zakeri A, Herson PS. Sex differences in thrombosis as it affects acute ischemic stroke. Neurobiol Dis. 2022;165:105647.
Chohan SA, Venkatesh PK, How CH. Long-term complications of stroke and secondary prevention: an overview for primary care physicians. Singap Med J. 2019;60:616–20. https://doi.org/10.11622/SMEDJ.2019158.
Evans TC, Jehle D. The red blood cell distribution width. J Emerg Med. 1991;9 Suppl 1 SUPPL. 1:71–4. https://doi.org/10.1016/0736-4679(91)90592-4.
Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. 2015;52:86–105. https://doi.org/10.3109/10408363.2014.992064.
Zhang L, Yu CH, Guo KP, Huang CZ, Mo LY. Prognostic role of red blood cell distribution width in patients with sepsis: a systematic review and meta-analysis. BMC Immunol. 2020;21. https://doi.org/10.1186/S12865-020-00369-6.
Zhang T, Li J, Lin Y, Yang H, Cao S. Association between Red Blood cell distribution width and all-cause mortality in chronic kidney Disease patients: a systematic review and Meta-analysis. Arch Med Res. 2017;48:378–85. https://doi.org/10.1016/J.ARCMED.2017.06.009.
Wen ZL, Zhou X, Xiao DC. Is red blood cell distribution width a prognostic factor for colorectal cancer? A meta-analysis. Front Surg. 2022;9. https://doi.org/10.3389/FSURG.2022.945126.
Xing X, Deng Y, Zhu Y, Xu S, Liu J, Zhang C, et al. Red cell distribution width for prognosis in patients with pulmonary embolism: a systematic review and meta-analysis. Clin Respir J. 2020;14:901–7. https://doi.org/10.1111/CRJ.13227.
Frentiu AA, Mao K, Caruana CB, Raveendran D, Perry LA, Penny-Dimri JC, et al. The Prognostic significance of red cell distribution width in cardiac surgery: a systematic review and Meta-analysis. J Cardiothorac Vasc Anesth. 2022. https://doi.org/10.1053/J.JVCA.2022.11.015.
Montagnana M, Danese E. Red cell distribution width and cancer. Ann Transl Med. 2016;4. https://doi.org/10.21037/ATM.2016.10.50.
Lippi G, Mattiuzzi C, Cervellin G. Learning more and spending less with neglected laboratory parameters: the paradigmatic case of red blood cell distribution width. Acta Biomed. 2016;87:323–8. https://pubmed.ncbi.nlm.nih.gov/28112703/. Accessed 29 Jan 2023.
Ani C, Ovbiagele B. Elevated red blood cell distribution width predicts mortality in persons with known stroke. J Neurol Sci. 2009;277:103–8. https://doi.org/10.1016/J.JNS.2008.10.024.
Kim J, Kim YD, Song TJ, Park JH, Lee HS, Nam CM, et al. Red blood cell distribution width is associated with poor clinical outcome in acute cerebral infarction. Thromb Haemost. 2012;108:349–56. https://doi.org/10.1160/TH12-03-0165.
Turcato G, Cervellin G, Cappellari M, Bonora A, Zannoni M, Bovi P, et al. Early function decline after ischemic stroke can be predicted by a nomogram based on age, use of thrombolysis, RDW and NIHSS score at admission. J Thromb Thrombolysis. 2017;43:394–400. https://doi.org/10.1007/S11239-016-1456-Y.
Pinho J, Marques SA, Freitas E, Araújo J, Taveira M, Alves JN, et al. Red cell distribution width as a predictor of 1-year survival in ischemic stroke patients treated with intravenous thrombolysis. Thromb Res. 2018;164:4–8. https://doi.org/10.1016/J.THROMRES.2018.02.002.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. https://doi.org/10.1016/j.ijsu.2021.105906.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al. Oct. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 30 2020.
Kim DY, Hong DY, Kim SY, Park JJ, Kim JW, Park SO, et al. Prognostic value of red blood cell distribution width in predicting 3-month functional outcome of patients undergoing thrombolysis treatment for acute ischemic stroke. Med (Baltim). 2021;100. https://doi.org/10.1097/MD.0000000000027255.
Guan Y, Zuo W, Jia K, Yu C, Liu F, Lv Z, et al. Association of Red Blood Cell Distribution Width with stroke prognosis among patients with small artery occlusion: a hospital-based prospective Follow-Up study. Int J Gen Med. 2022;15:7449–57. https://doi.org/10.2147/IJGM.S381160.
Wang Z, Liu Y. Red cell distribution width as a predictor of one-year prognosis and mortality of endovascular therapy for Acute Anterior circulation ischemic stroke. J Stroke Cerebrovasc Dis. 2022;31. https://doi.org/10.1016/J.JSTROKECEREBROVASDIS.2021.106243.
Xue J, Zhang D, Zhang XG, Zhu XQ, Xu XS, Yue YH. Red cell distribution width is associated with stroke severity and unfavorable functional outcomes in ischemic stroke. Front Neurol. 2022;13. https://doi.org/10.3389/FNEUR.2022.938515.
Li M, Wang L, Zhu X, Huang J, Zhang Y, Gao B, et al. Dose-response relationship between red blood cell distribution width and In-Hospital mortality in Oldest Old patients with Acute ischemic stroke. Gerontology. 2023;69:379–85. https://doi.org/10.1159/000527504.
Chen CM, Lee M, Yang YH, Huang SS, Lin CH. Association between Clinical and Laboratory Markers and 5-year mortality among patients with stroke. Sci Rep. 2019;9. https://doi.org/10.1038/S41598-019-47975-Y.
Güneş M. Is neutrophil/eosinophil ratio at admission a prognostic marker for in-hospital mortality of acute ischemic stroke? J Stroke Cerebrovasc Dis. 2020;29. https://doi.org/10.1016/J.JSTROKECEREBROVASDIS.2020.104999.
Wang L, Wang C, Wu S, Li Y, Guo W, Liu M. Red blood cell distribution width is associated with mortality after acute ischemic stroke: a cohort study and systematic review. Ann Transl Med. 2020;8:81–81. https://doi.org/10.21037/ATM.2019.12.142.
Ye WY, Li J, Li X, Yang XZ, Weng YY, Xiang WW, et al. Predicting the one-year prognosis and mortality of patients with Acute ischemic stroke using red blood cell distribution Width before Intravenous Thrombolysis. Clin Interv Aging. 2020;15:255–63. https://doi.org/10.2147/CIA.S233701.
Akpinar CK, Gurkaş E, Aykac O, Uysal Z, Ozdemir AO. Elevated red blood cell distribution Width May be a Novel Independent Predictor of poor functional outcome in patients treated with mechanical thrombectomy. Neurointervention. 2021;16:34–8. https://doi.org/10.5469/NEUROINT.2020.00262.
Zhao H, Zhao Y, Wu Z, Cheng Y, Zhao N. Red cell distribution width is associated with all-cause mortality in patients with acute stroke: a retrospective analysis of a large clinical database. J Int Med Res. 2021;49. https://doi.org/10.1177/0300060520980587.
Siegler JE, Marcaccio C, Nawalinski K, Quattrone F, Sandsmark DK, Maloney-Wilensky E, et al. Elevated Red Cell Distribution Width is Associated with cerebral infarction in Aneurysmal Subarachnoid Hemorrhage. Neurocrit Care. 2017;26:26–33. https://doi.org/10.1007/S12028-016-0306-2.
Palabiyik O, Tomak Y, Acar M, Erkorkmaz U, Tuna AT, Suner KO, et al. Relationship between platelet indices and red cell distribution width and short-term mortality in traumatic brain injury with 30-day mortality. Rev Assoc Med Bras. 2023;69:18–23. https://doi.org/10.1590/1806-9282.00210889.
Lorente L, Martín MM, González-Rivero AF, Pérez-Cejas A, Sabatel R, Ramos L, et al. Red blood cell distribution width and mortality of spontaneous intracerebral hemorrhage patients. Clin Neurol Neurosurg. 2020;195. https://doi.org/10.1016/J.CLINEURO.2020.106066.
Song SY, Hua C, Dornbors D, Kang RJ, Zhao XX, Du X, et al. Baseline red blood cell distribution width as a predictor of stroke occurrence and outcome: a Comprehensive Meta-Analysis of 31 studies. Front Neurol. 2019;10. https://doi.org/10.3389/FNEUR.2019.01237.
Wenger NK. Enrollment and maintenance of elderly patients in cardiovascular clinical trials. Am J Geriatr Cardiol. 2006;15:352–6. https://doi.org/10.1111/J.1076-7460.2006.05824.X.
Saposnik G, Cote R, Phillips S, Gubitz G, Bayer N, Minuk J, et al. Stroke outcome in those over 80. Stroke. 2008;39:2310–7. https://doi.org/10.1161/STROKEAHA.107.511402.
Katsanos AH, Malhotra K, Ahmed N, Seitidis G, Mistry EA, Mavridis D, et al. Blood pressure after endovascular thrombectomy and outcomes in patients with Acute ischemic stroke: an individual Patient Data Meta-analysis. Neurology. 2022;98:E291–301. https://doi.org/10.1212/WNL.0000000000013049.
Leonardi-Bee J, Bath PMW, Phillips SJ, Sandercock PAG. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke. 2002;33:1315–20. https://doi.org/10.1161/01.STR.0000014509.11540.66.
Hong C, Salanti G, Morton SC, Riley RD, Chu H, Kimmel SE, et al. Testing small study effects in multivariate meta-analysis. Biometrics. 2020;76:1240. https://doi.org/10.1111/BIOM.13342.
Dziedzic T. Systemic inflammation as a therapeutic target in acute ischemic stroke. Expert Rev Neurother. 2015;15:523–31. https://doi.org/10.1586/14737175.2015.1035712.
Pierce CN, Larson DF. Inflammatory cytokine inhibition of erythropoiesis in patients implanted with a mechanical circulatory assist device. Perfusion. 2005;20:83–90. https://doi.org/10.1191/0267659105PF793OA.
Förhécz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohászka Z, Jánoskuti L. Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am Heart J. 2009;158:659–66. https://doi.org/10.1016/J.AHJ.2009.07.024.
Kara H, Degirmenci S, Bayir A, Ak A, Akinci M, Dogru A, et al. Red cell distribution width and neurological scoring systems in acute stroke patients. Neuropsychiatr Dis Treat. 2015;11:733–9. https://doi.org/10.2147/NDT.S81525.
Söderholm M, Borné Y, Hedblad B, Persson M, Engström G. Red cell distribution width in relation to incidence of stroke and carotid atherosclerosis: a population-based cohort study. PLoS ONE. 2015;10. https://doi.org/10.1371/JOURNAL.PONE.0124957.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
HS and LS: designed the paper, conducted the literature search, did study selection and analysis, wrote the paper, and approved the final revisions of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shen, H., Shen, L. Red blood cell distribution width as a predictor of mortality and poor functional outcome after acute ischemic stroke: a meta-analysis and meta-regression. BMC Neurol 24, 122 (2024). https://doi.org/10.1186/s12883-024-03610-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03610-6