Abstract
Background
Ruptured intracranial aneurysms resulting in subarachnoid haemorrhage can be treated by open surgical or endovascular treatment. Despite multiple previous studies, uncertainties on the optimal treatment practice still exists. The resulting treatment variation may result in a variable, potentially worse, patient outcome. To better inform future treatment strategies, this study aims to identify the effectiveness of different treatment strategies in patients with ruptured intracranial aneurysms by investigating long-term functional outcome, complications and cost-effectiveness. An explorative analysis of the diagnostic and prognostic value of radiological imaging will also be performed.
Methods
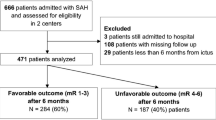
This multi-centre observational prospective cohort study will have a follow-up of 10 years. A total of 880 adult patients with a subarachnoid haemorrhage caused by a ruptured intracranial aneurysm will be included. Calculation of sample size (N = 880) was performed to show non-inferiority of clip-reconstruction compared to endovascular treatment on 1 year outcome, assessed by using the ordinal modified Rankin Scale. The primary endpoint is the modified Rankin Scale score and mortality at 1 year after the initial subarachnoid haemorrhage. Patients will receive ‘non-experimental’ regular care during their hospital stay. For this study, health questionnaires and functional outcome will be assessed at baseline, before discharge and at follow-up visits.
Discussion
Despite the major healthcare and societal burden, the optimal treatment strategy for patients with subarachnoid haemorrhage caused by ruptured intracranial aneurysms is yet to be determined. Findings of this comparative effectiveness study, in which in-between centre variation in practice and patient outcome are investigated, will provide evidence on the effectiveness of treatment strategies, hopefully contributing to future high value treatment standardisation.
Trial registration number
NCT05851989
Date of registration
May 10th, 2023
Similar content being viewed by others
Background
Spontaneous subarachnoid haemorrhage (SAH) is a life-threatening event, most frequently (around 85% of cases) caused by the rupture of an intracranial aneurysm (IA). The prevalence of unruptured IAs in the general population is estimated to be 1.8% at a mean age of 63.3 years and women are affected more often than men [1, 2]. In the Netherlands, the incidence of aneurysmal SAH (aSAH) is estimated to be 8–9 per 100.000 per year and the average annual incidence from 2014 to 2017 according to the Dutch Quality Registry for Neuro Surgery (QRNS) is 1014 cases [3,4,5]. It is generally believed that 8–10% of the patients die before hospital arrival after an SAH [6]. Mortality after aneurysmal SAH for Europe excluding northern Sweden and Finland is thought to be 44.4% [3, 4, 7]. The mortality rate, however, seems to be declining due to improved prehospital and hospital care [3, 7]. When considering functional outcome, it is assumed that approximately a third of all patients with an aSAH has a “good functional outcome”, i.e. mRS ≤ 2 [8].
An aSAH is a complex pathology requiring close monitoring in the first weeks following admission. The primary treatment for ruptured IAs is performed to prevent the high-risk occurrence of early rebleeding by exclusion of the aneurysm from the circulation. Furthermore, delayed cerebral ischemia (DCI) and hydrocephalus are both common and dangerous consequences of SAH, often prompting specific medical and/or surgical therapy [8]. Systemic complications including cardiac instability, hyponatremia and other metabolic dysregulation like hyperglycaemia can negatively affect patient outcome and require monitoring and treatment [9,10,11].
Nowadays, the most applied primary treatment modality of the ruptured aneurysm is endovascular treatment, which has replaced craniotomy with microsurgical clip-reconstruction in the majority of cases [12]. The best but conflicting evidence for this treatment strategy comes from the results of two randomized controlled trials: the Barrow Ruptured Aneurysm Trial (BRAT) and the International Subarachnoid Aneurysm Trial (ISAT) [13, 14]. The outcomes from the ISAT trial suggest that survival is slightly but significantly increased in patients treated by endovascular treatment compared to patients treated with microsurgical clip-reconstruction [13, 15, 16]. Initial results from the BRAT suggested superior functional outcome for patients treated with endovascular treatment, but these did not remain significant with longer follow-up [14, 17,18,19].
Results from the ISAT and BRAT demonstrate that the optimal evidence-based practice for treatment of acutely ruptured IAs has yet to be determined. The promising endovascular treatment, introduced two decades ago, seems to have a higher incidence of rebleeding and need for retreatment, necessitating intensive outpatient radiological follow-up and therefore keeps a large proportion of treated patients unsure about their future. This uncertainty is very debilitating as the risk of a recurring bleeding incident has an impact on the patient, their family and society (loss of work).
The choice of endovascular treatment or clip-reconstruction is primarily decided by the treating physician based on the aneurysm location, morphology and local and physician-bound treatment paradigms that take the clinical condition of the patient into account. Hospitals may have different treating algorithms for similar patients including endovascular techniques and microsurgical techniques. Aside from the treatment modality, even deciding whether to treat ruptured IAs immediately after presentation, to postpone treatment or to choose not to treat the causative aneurysm, especially in cases with severely affected patients (grades IV or V according to the World Federation of Neurosurgical Societies (WFNS)-grading system) is variable.
Study aim
The aim of this prospective observational cohort study is to identify the most effective treatment strategy for the best outcome in patients with a subarachnoid haemorrhage caused by a ruptured intracranial aneurysm.
Methods
Primary objective and research question
The primary objective is to determine the effect of clip-reconstruction versus endovascular treatment on the functional outcome at 1 year in patients presenting with an SAH due to a ruptured IA. We hypothesize that the functional outcome of clip-reconstruction is non-inferior to endovascular treatment at 1 year after treatment, but that inherent treatment differences might become apparent beyond this horizon.
Secondary objectives
Secondary objectives include the effect of clip-reconstruction versus endovascular treatment on the functional outcome and mortality of patients with ruptured AIs at 6 months, 2, 5 and 10 years after ictus. Besides functional outcome, this study will examine the effect of clip-reconstruction versus endovascular treatment on neuropsychological outcome, quality of life and the need for rehabilitation. Furthermore, timing of treatment and differences in outcome between primary treatment modalities, including advanced endovascular treatment techniques, will be examined. In addition, secondary treatments (for hydrocephalus or DCI) and the effect on the named outcome parameters will be studied. Also, computed tomography (CT)- and angiographic imaging data will be collected to evaluate prognostic factors for surgical outcome, functional outcome and risk of complications after primary or secondary treatment. Lastly, an estimate of the costs associated with primary treatment modalities, supportive care measures and care settings, different treatments for complications, long-term follow-up imaging and different rehabilitation strategies will be established. The role of different referral area, caseload and number of care providers when considering functional outcome after aSAH will be determined.
Study design
Study design
Longitudinal multicentre prospective observational cohort study.
During the study period, all SAH patients presenting at the study sites will be screened for inclusion eligibility. Following informed consent, eligible patients will be included as participants in the study. Treatment decisions and treatment methods (e.g. neurosurgical clip-reconstruction or endovascular treatment for primary treatment of the aneurysm) will not be influenced by inclusion in the study. Standard care tailored to the patient needs is provided, as is customary in the study site by the local treating team. Patient characteristics and initial treatment considerations will be collected for participants as baseline information.
Follow-up of the subjects is according the Dutch national quality regulations during the initial 6 months after aSAH ictus, and is tailored to the specific needs of the patient. At these regular follow-up visits, study questionnaires are completed. After regular follow-up visits, patients included in the study will have at least four more visits, at respectively 1, 2, 5 and 10 years after aSAH ictus. Additional visits may be necessary for patient-specific reasons and should be documented, but are not required by the study. During these study visits, patients will complete questionnaires and the local treating team will report on the treatment and clinical findings.
The primary outcome measurement will be evaluated after the 1-year follow-up of the last included patient. The study will be completed after 10 years of follow-up.
Study sites
To answer the research questions 5 centres from The Netherlands will include subjects.
Participating centres:
-
University Neurosurgical Centre Holland Leiden – The Hague (UNCH), including the Leiden University Medical Centre (LUMC) in Leiden, HAGA hospital in The Hague and Haaglanden Medical Centre (HMC) in The Hague.
-
Radboud University Medical Centre (Radboud UMC).
-
Academic Medical Centre Amsterdam (AMC).
-
Maastricht University Medical Centre (MUMC).
-
Erasmus Medical Centre (EMC).
All of these study sites will collect data from their own patients in an electronic database and centralised analysis will be performed from the main study location in Leiden – The Hague.
A steering committee will be established to include local investigators in the management aspects surrounding the study, including publication policy and for the sake of transparency.
Sample size / sample size calculation
Calculation of sample size was performed to show non-inferiority of clip-reconstruction compared to endovascular treatment on 1-year outcome, as assessed using the ordinal modified Rankin Scale. The software of Sealed Envelope was used for calculation of the sample size [20]. We assume that the rate of poor outcome (mRS < 2) after clip-reconstruction and endovascular treatment is equal (31%) based on the uncertainties in previous literature regarding selection of patients and biases [13,14,15,16,17,18,19]. The non-inferiority margin is set at 7% difference. This is based on the largest previous clipping versus coiling trial where an absolute risk reduction of death and dependency of 7% was found in coiling compared to clipping [13]. Alpha is set to 0.05 and beta to 0.8. Using these assumptions, we require a sample size of 1100 patients. Since analysing the full-modified Rankin Scale instead of dichotomizing it decreases the required sample size by approximately 20%, we therefore require 880 patients [21, 22].
Number of subjects
We will include 880 subjects.
Study duration
Based on the number of SAH patients that are admitted at the various study sites, we expect that inclusion of 880 patients will take around four to five years. Recruitment will start on July 2021 and is expected to finish on July 2026. Patients will have a maximum follow-up of 10 years, resulting in a maximum of 14 years data collection. Inclusion of patients stops when the targeted number of subjects is reached.
In the event of slower inclusion, the recruitment period may be extended.
Study population
Population (base)
All patients that present primarily or after acute referral (in-patient to in-patient) to the participating centres, with a spontaneous subarachnoid haemorrhage due to a ruptured IA will be screened for eligibility for this study by the treating physicians or local research nurses.
Inclusion criteria
In order to be eligible to participate in this study, a subject must meet all the following criteria:
-
Confirmed diagnosis of SAH on CT-scan or lumbar puncture (in the presence of a negative CT-scan).
-
IA related SAH as confirmed with radiological imaging.
-
Age 18 years or older at presentation.
-
Written informed consent.
Written informed consent for participation in the study will be obtained from the patient or the legal representative during the admission period by the local treating team.
Exclusion criteria
A potential subject who meets any of the following criteria on presentation to one of the participating centres or later during the clinical course will be excluded from participation in this study:
-
SAH deemed most likely of ’perimesencephalic’ origin after consideration of history, clinical examination and radiological findings (including angiographic imaging).
-
SAH deemed most likely of post-traumatic origin after consideration of history, clinical examination and radiological findings (including angiographic imaging).
-
Diagnosis of intracerebral arteriovenous malformations or dural arteriovenous fistula.
-
No diagnosis of IA at 6 months after onset of symptoms.
Participant does not master the Dutch language sufficiently.
Treatment of subjects
The treatment protocol for the patients included in the study is not specified by the study protocol, as the study is strictly observational with current practice care.
Study parameters/endpoints
Main study parameter/endpoint
The primary endpoint in this study is the score on the mRS at 1 year after onset of symptoms.
This will be collected through a case report form filled in by the local treating team at the 6 month and 1-year interval after onset of symptoms. The mRS will be obtained through a structured interview, either by phone or at a face-to-face assessment [20]. Additionally, mortality before this point will be documented by the local treating team.
Secondary study parameters/endpoints
To summarize some of the most used outcome parameters we will use the following terms:
‘Functional outcome’-data set:
-
mRS at 6 months, 1, 2, 5 and 10 years after onset of symptoms, as measured by completion of case report forms by the local treating teams.
-
Barthel index at 6 months, 1, 2, 5 and 10 years after onset of symptoms, as measured by completion of case report forms by the local treating teams.
‘Cognitive outcome’-data set, meaning general cognitive functioning and mood/fatigue:
-
Modified Telephone Interview for Cognitive Status (TICS-M) at 6 months, 1, 2, 5 and 10 years after onset as measured by completion of case report forms by the local treating teams.
-
Hospital Anxiety and Depression Scale (HADS) at 6 months, 1, 2, 5 and 10 years after onset of symptoms by completion of questionnaires by the subjects.
‘Quality of life and Costs’-data set:
-
The 5-level EQ-5D (EQ-5D-5 L) at 6 months, 1, 2, 5 and 10 years after onset of symptoms, as measured by completion of questionnaires by the subjects.
-
Estimation of societal costs by completion of a custom healthcare consumption and loss of productivity (paid and unpaid) questionnaire at 3 months, 6 months, 1 year, 2 years, 5 years and 10 years completed by the subjects.
Primary treatment
-
Case report form (CRF) on type of primary treatment, timing of treatment, reasoning for choice of treatment, per procedural complications, used material and time.
-
CRF on the occurrence of rebleeding and retreatment, reasoning for choice of retreatment, modality of retreatment, timing of retreatment, used material and time.
-
CRF on death of subject, timing of death, suspected cause of death.
-
Functional outcome data set (see above).
-
Cognitive outcome data set (see above).
-
Quality of life data set (see above).
Secondary treatment
-
CRF on the occurrence of DCI and its treatment, timing of treatment, reasoning for choice of treatment, per procedural complications, used material and time.
-
CRF on the occurrence of hydrocephalus and its treatment, timing of treatment.
-
CRF on the admission of patient to ICU or medium care unit, reasoning for choice of ward.
-
CRF on death of subject, timing of death, suspected cause of death.
-
Functional outcome data set (see above).
-
Cognitive outcome data set (see above).
-
Quality of life data set (see above).
Rehabilitation
-
CRF on the rehabilitation choice for patients, reasoning for choice, timing of rehabilitation and intensity of programme.
-
Functional outcome data set (see above).
-
Cognitive outcome data set (see above).
-
Quality of life data set (see above).
Follow-up and imaging
-
CRF on the follow-up schedule, reasoning for the schedule, used time and imaging requested.
-
CRF on aneurysm recanalization and recurrence, describing aneurysm morphology, changes, clinical course.
-
Initial CT and (CT-)angiography digital images and centralized analysis by blinded radiology panel.
Cost-effectiveness and organization of care
-
All CRF’s mentioned above, except the CRF’s on recanalization and death.
-
Hospital specific referral area, caseload, number of care providers.
-
Functional outcome data set (see above).
-
Cognitive outcome data set (see above).
-
Quality of life data set (see above).
Baseline information
-
Baseline patient information CRF on common data elements.
-
All CRF’s above.
-
Functional outcome data set (see above).
-
Cognitive outcome data set (see above).
-
Quality of life data set (see above).
Study procedures
Study procedures for inclusion in the study are the same in all study sites. The local treating physicians will obtain informed consent and treat patients according to local hospital protocol or their own clinical insight. The data collected in this study will be collected without interfering with treatment of the patient and is strictly observational, supplemented by questionnaires.
The procedure of informed consent for participation in the study will be discussed in the section ‘Recruitment and consent’.
Baseline information, treatment information, outcomes and imaging data will be collected according to specified time points. The follow-up of all patients will be 10 years after ictus. The local treating physician and other appropriate treatment providers will fill out the questionnaires and perform the necessary tests. The data will be entered into the database directly when possible. A research-assistant will enter the data into the database at a later point if this is not possible at some locations.
All measurements will be performed by qualified physicians or research nurses that have received training to perform the measurements. The measurements will take place during follow-up appointments, by phone, by (e-)mail and will be registered in Castor, an online data capture environment. In cases where patients have difficulty completing the form, legal representatives or family or close caregivers can assist them in completing the form. Patients that have a lowered level of consciousness will be evaluated by physicians or research nurses trained to handle these specific patients. After assignment of a patient-specific study code, the data will be entered into a centralised electronic database in the different study sites by treating physicians or study nurses, according to local organisation. The Masterfile containing the link between the identifiable patient data and the study code will be kept in the local study site. Process related variables and associated costs will be acquired from participating centres.
After collection of this data in the centralised database, analysis will be primarily performed by the sponsor and the coordinating researchers. Local investigators may use the data from their centre for separate analyses after consensus in the steering committee.
Timing of data acquisition
On baseline/admission
-
Informed consent form
-
Baseline information CRF.
-
Initial CT and (CT-)angiography digital images.
-
CRF on admission.
Primary treatment
-
CRF on primary treatment.
-
If rebleeding or retreatment, CRF on rebleeding and retreatment.
Secondary treatments
-
CRF on patient mobilisation and inpatient rehabilitation.
-
If hydrocephalus or DCI, CRF on hydrocephalus or DCI.
Hospital discharge
-
Deferred informed consent form if not yet consented.
-
If death, CRF on death.
Scheduled follow-up visits
-
CRF on follow-up schedule.
-
If rehabilitation referral, fill CRF on rehabilitation.
-
If recanalization/retreatment, fill CRF on recanalization/retreatment.
-
If death, fill CRF on death.
-
At 3 months: costs questionnaire.
-
At 6 months: mRS, TICS-m, Hospital Anxiety and Depression Scale (HADS), EQ-5D, Barthel ADL index, costs questionnaire.
-
At 1 year: mRS, TICS-m, HADS, EQ-5D, Barthel index, costs questionnaire.
-
At 2 year: mRS, TICS-m, HADS, EQ-5D, Barthel index, costs questionnaire.
-
At 5 year: mRS, TICS-m, HADS, EQ-5D, Barthel index, costs questionnaire.
-
At 10 year: mRS, TICS-m HADS, EQ-5D, Barthel index, costs questionnaire.
Withdrawal of individual subjects
Subjects can leave the study at any time for any reason if they wish to do so without any further consequences. The patient is then requested, however not required, to complete a questionnaire on withdrawal from the study.
Replacement of individual subjects after withdrawal
Subjects who are withdrawn from the study will not be replaced.
Follow-up of subjects withdrawn from treatment
General category of reason for withdrawal should be completed on the CRF. After this, there is no study follow up of patients after withdrawal. Regular clinical follow up is maintained as decided by the local treating team.
Safety reporting
Aneurysmal SAH is a life-altering event that can lead to temporary or permanent discomfort or injury and even death. This is unfortunately inherent to the disease and this study will not interfere with the clinical course of this disease by any intervention. As the study is observational in nature comparing different forms of accepted practice, it is unlikely that any events will occur that are caused by participation in the study.
Information on the course of the disease in the study subjects will be gathered in the study. As such, CRFs require local investigators to report complications of the SAH. We will not report AEs, SAEs or SUSARs to the METC but include them in the CRF.
No committee regarding the safety of patients will be established, as the safety is not at risk in the observational design of the study. A committee evaluating the correct performance of the study will be convened because of the long-term run of the study and multicentre design, a so-called data safety monitoring board. The charter is attached.
Statistical analysis
Primary study parameter
To examine effectiveness of the interventions, proportional odds logistic regression models with ordinal mRS as outcome variable will be used. This method increases statistical power when compared to reporting on a dichotomized ordinal scale. We will report the odds ratios per cut-off and an average (common) odds ratio to give insight in fulfilment of the requisites of the proportional odds model [23].
To account for the risk of confounding by indication in the observational design, correction will be performed based on the aneurysm location, morphology and current clinical patient status. Strongest predictors of outcome from literature (age, history of hypertension, WFNS grading on admission, CT blood clot burden, aneurysm location and size, treatment variables, cerebral ischemia [24,25,26,27]) will be added as covariates. Analysis will be performed in R and in the Statistical Package for the Social Sciences (SPSS) version 21. A p-value < 0.05 will be considered statistically significant.
Secondary study parameter(s)
As a secondary study parameter, we will analyse the between-hospital differences to correct for confounding. Conventional methods are likely unable to account for the (unmeasured) confounding in SAH, like in traumatic brain injury [28]. Therefore, the main analyses will use the between-hospital variation in treatment for determining effectiveness by comparing regional treatment strategies. This is an instrumental variable approach [28]. The instrument is treatment preference and is determined as the amount of either coiled or clipped patients of total amount of treated patients. The proportion (percentage) exposed to the intervention in each hospital (the instrument) is entered as an independent variable to the analyses. The unmeasured and measured confounding at the hospital level, for example hospitals that perform more surgery also more often perform other treatments, is overcome with a multilevel model [29]. In this model, the random intercept should capture the measured and unmeasured confounders at hospital level, resulting in unbiased treatment effect estimates. The random intercept for each hospital represents the unexplained hospital effect (beyond all factors included in the model, including the instrument treatment preference).
In sensitivity analyses, the instrument validity will be further explored by quantifying a priori collected data and the results of provider profiling of SPARTA and comparing these to the posthoc derived relative proportion exposed to the intervention per hospital.
Moreover, as an alternative to the instrumental variable approach of the primary analyses, the instrument is modelled as a categorical variable. Specifically, the hospitals are divided into halves, tertiles and/or quartiles based on their preference for the intervention.
As secondary analyses, conventional ordinal regression analyses are planned with actual treatment as binary treatment variable and mRS as outcome variable. For aneurysm treatment effectiveness, confounding will be controlled for by adding known predictors for outcome as covariates in the model.
A similar strategy will be utilized to analyse the effectiveness of clip-reconstruction versus endovascular treatment on longer time intervals, the effectiveness of flow diversion and Woven EndoBridge®-devices, the effectiveness of secondary treatment modalities, timing of mobilisation and different rehabilitation programmes on the functional outcome using mRS and proportional odds regression modelling.
HADS for anxiety and depression will be analysed in a dichotomized way because of the uncertainty of abnormality in the borderline categories. The total score will be analysed using a proportional odds logistic regression model as described above. Different timing of treatment will be analysed both as a categorical variable (within 6 h, within 24 h, within 72 h, within 1 week, within 2 weeks, first month) and as a continuous variable.
Multivariate regression analysis and stepwise univariate analyses will be used for correlation of the imaging, patient specific and treatment data and outcome measurements, including occurrence of complications. Proportional odds regression modelling will be used for the analysis of recanalization and rebleeding using the reported morphological changes and occurrence of rebleeding.
Cost-effectiveness and cost-utility analysis will be performed using mRS at one year and QALY respectively. Effectiveness in QALYs, costs and cost-effectiveness ratios will be calculated. The analysis will use direct and indirect healthcare costs from both self-reported and CRF provided data, aspiring an extensive list of the costs in and out of hospital and productivity losses. Sensitivity analyses will be performed to validate the results [30, 31].
Discussion
Spontaneous subarachnoid haemorrhage (SAH) caused by the rupture of an IA is a life-threatening event with high mortality rates [3, 4, 6]. Although mortality rates seem to be improving due to improved prehospital and in-hospital care [3, 6], only a third of all patients achieve a so called good outcome (mRS 0–2) [7]. Despite the major healthcare and societal burden, the optimal treatment strategy for these patients is yet to be determined. The overall objective of this study is to investigate the effectiveness of existing treatment strategies for patients with SAH caused by a ruptured IA in the Netherlands.
This study will evaluate the effect of clip-reconstruction versus endovascular treatment on functional and cognitive outcome, quality of life and cost-effectiveness at 1, 2, 5, and 10 years after onset of symptoms. As described earlier in this protocol, these essential pieces of information are largely unknown. Therefore, this study is a necessary addition to literature on the treatment of aSAH. The latter because the assessment of long-term treatment effectiveness is not possible due to insufficient data and because scientific analysis of these data is not permitted. This study also aims to improve insight into the full chain of care for these patients going through hospitals, rehabilitation centres, nursing homes or other outpatient settings. By employing comparative effectiveness analyses, in which in-between centre variation in clinical practice and patient outcome are investigated, the influence of treatment strategies on patient outcome will be investigated.
The longitudinal multicentre prospective observational cohort study design, instead of a randomized controlled trial (RCT), was selected to provide a more pragmatic and cost-effective assessment of treatment strategy effectiveness. Longitudinal observational studies are more feasible for long-term follow up of clinical outcomes and for investigating a relatively variable study population. This is more pragmatic and improves generalisability of study results. Investigating treatment- and cost-effectiveness through an RCT is complicated by the heterogeneity of aSAH patients, the sample size requirements, already established treatment strategies, the often life-threatening situation, and inadequate research budgets. The feasibility of this large-scale observational study is likely to be good due to its observational pragmatic design and due to the extensive experience obtained from participating in the CENTRE-TBI study [32]. The collection of extensive primary and secondary outcome measures is another strength of this study. Nonetheless, data collection could be challenging by its extent, but also by the nature of the investigated disease causing cognitive impairment and high emotional distress. The inevitable and likely substantial confounding by indication could limit the interpretability of observational research, but can be circumvented by using practice variation and statistical methods like instrumental variable analysis.
In conclusion, findings of this study will provide evidence on the effectiveness of treatment strategies in patients with subarachnoid haemorrhage caused by the rupture of an IA, hopefully contributing to future standardised high value care.
Data availability
Not applicable.
Abbreviations
- ABR:
-
ABR form, General Assessment and Registration form, is the application form that is required for submission to the accredited Ethics Committee (In Dutch, Algemene Beoordeling en Registratie)
- ADL:
-
Activities of Daily Life
- AE:
-
Adverse Event
- AR:
-
Adverse Reaction
- aSAH:
-
Aneurysmal Subarachnoid Haemorrhage
- AVG:
-
Algemene Verordening Gegevensbescherming
- AVM:
-
Arteriovenous Malformation
- BRT:
-
Barrow Ruptured Aneurysm Trial
- CA:
-
Competent Authority
- CI:
-
Confidence interval
- CCMO:
-
Central Committee on Research Involving Human Subjects (in Dutch: Centrale Commissie Mens-gebonden Onderzoek)
- CRF:
-
Case Report Form
- CSF:
-
Cerebrospinal Fluid
- CT:
-
Computed Tomography
- CV:
-
Curriculum Vitae
- dAVF:
-
Dural Arteriovenous Fistula
- DCI:
-
Delayed Cerebral Ischemia
- DSMB:
-
Data Safety Monitoring Board
- DCI:
-
Delayed cerebral ischemia
- EU:
-
European Union
- EudraCT:
-
European drug regulatory affairs Clinical Trials
- EQ-5D:
-
Health-related quality of life measurement instrument
- GCP:
-
Good Clinical Practice
- HADS:
-
Hospital Anxiety and Depression Scale
- HMC:
-
Haaglanden Medical Centre, The Hague
- IA:
-
Intracranial Aneurysm
- IB:
-
Investigator’s Brochure
- IC:
-
Informed Consent
- ISAT:
-
International Subarachnoid Aneurysm Trial
- IMP:
-
Investigational Medicinal Product
- IMPD:
-
Investigational Medicinal Product Dossier
- LUMC:
-
Leiden University Medical Centre, Leiden
- METC:
-
Medical research ethics committee (in Dutch: Medisch Ethische Toetsing Commissie)
- METC LDD:
-
Medical Ethics Committee Leiden The Hague Delft
- mRS:
-
Modified Rankin Scale
- QALY:
-
Quality Adjusted Life years
- RCT:
-
Randomized Controlled Trial
- (S)AE:
-
(Serious) Adverse Event
- SAH:
-
Subarachnoid Haemorrhage
- SPC:
-
Summary of Product Characteristics (in Dutch: officiële productinfomatie IB1tekst)
- Sponsor:
-
The sponsor is the party that commissions the organisation or performance of the research, for example a pharmaceutical company, academic hospital, scientific organisation or investigator. A party that provides funding for a study but does not commission it is not regarded as the sponsor, but referred to as a subsidising party
- SUSAR:
-
Suspected Unexpected Serious Adverse Reaction
- TICS-m:
-
Telephone Interview for Cognitive Status
- UNCH:
-
University Neurosurgical Centre Holland Leiden – The Hague
- WEB®:
-
Woven EndoBridge®
- WFNS:
-
World Federation of Neurosurgical Societies
- WMO:
-
Medical Research Involving Human Subjects Act (in Dutch: Wet Medisch- wetenschappelijk Onderzoek met Mensen
References
Vlak MHM, Algra A, Brandenburg R, Rinkel GJE. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol. 2011;10(7):626–36. https://doi.org/10.1016/S1474-422(11)70109-0.
Vernooij MW, Ikram MA, Tanghe HL, et al. Incidental findings on Brain MRI in the General Population. N Engl J Med. 2007;357(18):1821–8. https://doi.org/10.1056/NEJMoa070972.
Nieuwkamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol. 2009;8(7):635–42. https://doi.org/10.1016/S14744422(09)70126-7.
Dutch Quality Registry for Neuro Surgery. Accessed April 2., 2023.https://www.qrns.nl/.
Hughes JD, Bond KM, Mekary RA, et al. Estimating the Global Incidence of Aneurysmal Subarachnoid Hemorrhage: a systematic review for Central Nervous System Vascular lesions and Meta-Analysis of ruptured aneurysms. Volume 115. Elsevier Inc.; 2018. https://doi.org/10.1016/j.wneu.2018.03.220.
Sweeney K, Silver N, Javadpour M. Subarachnoid haemorrhage (spontaneous aneurysmal). BMJ Clin Evid. 2016;2016:1213. PMID: 26983641; PMCID: PMC4794735.
Lovelock CE, Rinkel GJE, Rothwell PM. Time trends in outcome of subarachnoid hemorrhage. Neurology. 2010;74(19):1494–501. https://doi.org/10.1212/WNL.0b013e3181dd42b3.
Pegoli M, Mandrekar J, Rabinstein AA, Lanzino G. Predictors of excellent functional outcome in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2014;122(2):414–8. https://doi.org/10.3171/2014.10.jns14290.
Crago EA, Kerr ME. Impact of Cardiac complications on outcomes in patients with subarachnoid hemorrhage. Crit Care Med. 2012;30(Supplement):A6. https://doi.org/10.1097/00003246-200212001-00020.
Mapa B, Taylor BES, Appelboom G, Bruce EM, Claassen J, Connolly ES. Impact of Hyponatremia on Morbidity, Mortality, and complications after Aneurysmal Subarachnoid Hemorrhage: a systematic review. World Neurosurg. 2016;85:305–14. https://doi.org/10.1016/j.wneu.2015.08.054.
Kruyt ND, Biessels GJ, De Haan RJ, et al. Hyperglycemia and clinical outcome in aneurysmal subarachnoid hemorrhage: a meta-analysis. Stroke. 2009;40(6):424–30. https://doi.org/10.1161/STROKEAHA.108.529974.
Vates GE, Lawton MT. Subarachnoid hemorrhage. N Engl J Med. 2017;377:257–66.
Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RSC. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet. 2015;385(9969):691–7. https://doi.org/10.1016/S0140-6736(14)60975-2.
Spetzler RF, McDougall CG, Zabramski JM, et al. The Barrow ruptured Aneurysm Trial: 6-year results. J Neurosurg. 2015;123(3):609–17. https://doi.org/10.3171/2014.9.jns141749.
Molyneux AJ, Kerr RS, Yu LM, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured IAs: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and. Lancet. 2005;366(9488):809–17. https://doi.org/10.1016/S0140-6736(05)67214-5.
Campi A, Ramzi N, Molyneux AJ, et al. Retreatment of ruptured cerebral aneurysms in patients randomized by coiling or clipping in the International Subarachnoid Aneurysm Trial (ISAT). Stroke. 2007;38(5):1538–44. https://doi.org/10.1161/STROKEAHA.106.466987.
Spetzler RF, Mcdougall CG, Albuquerque FC et al. The Barrow ruptured Aneurysm Trial: 3-year results. J Neurosurg. 2013;(September):146–57.
McDougall CG, Spetzler RF, Zabramski JM, et al. The Barrow ruptured Aneurysm Trial. J Neurosurg. 2012;116(1):135–44. https://doi.org/10.3171/2011.8.JNS101767.
Spetzler RF, McDougall CG, Zabramski JM, et al. Ten-year analysis of saccular aneurysms in the Barrow ruptured Aneurysm Trial. J Neurosurg. 2019;1–6. https://doi.org/10.3171/2018.8.JNS181846.
Sealed Envelope. https://www.sealedenvelope.com/power/binary-superiority/. Accessed June 2019.
Roozenbeek B, Lingsma HF, Perel P, et al. The added value of ordinal analysis in clinical trials: an example in traumatic brain injury. Crit Care. 2011;15(3):R127. https://doi.org/10.1186/cc10240.
Optimising Analysis of Stroke Trials Collaboration. Calculation of sample size for stroke trials assessing functional outcome: comparison of binary and ordinal approaches. Int J Stroke. 2008;3(2):78–84. https://doi.org/10.1111/j.1747-4949.2008.00184.x. PMID: 18705999.
Nobels-Janssen E, Postma EN, Abma IL, van Dijk JMC, Haeren R, Schenck H, Moojen WA, den Hertog MH, Nanda D, Potgieser ARE, Coert BA, Verhagen WIM, Bartels RHMA, van der Wees PJ, Verbaan D, Boogaarts HD. Inter-method reliability of the modified Rankin Scale in patients with subarachnoid hemorrhage. J Neurol. 2022;269(5):2734–42. Epub 2021 Nov 8. PMID: 34746964; PMCID: PMC8572691.
Koffijberg H, Buskens E, Granath F, et al. Subarachnoid haemorrhage in Sweden 19872002: Regional incidence and case fatality rates. J Neurol Neurosurg Psychiatry. 2008;79(3):294–9. https://doi.org/10.1136/jnnp.2007.123901.
Vergouwen MDI, Etminan N, Ilodigwe D, MacDonald RL. Lower incidence of cerebral infarction correlates with improved functional outcome after aneurysmal subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2011;31(7):1545–53. https://doi.org/10.1038/jcbfm.2011.56.
Jaja BNR, Lingsma H, Schweizer TA, Thorpe KE, Steyerberg EW, Macdonald RL. Prognostic value of premorbid hypertension and neurological status in aneurysmal subarachnoid hemorrhage: pooled analyses of individual patient data in the SAHIT repository. J Neurosurg. 2015;122(3):644–52. https://doi.org/10.3171/2014.10.jns132694.
Jaja BNR, Schweizer TA, Thorpe KE, Lingsma H, Steyerberg EW. Neuroimaging characteristics of ruptured aneurysm as predictors of outcome after aneurysmal subarachnoid hemorrhage: pooled analyses of the SAHIT cohort. J Neurosurg. 2016;124(6):1703–11. https://doi.org/10.3171/2015.4.JNS142753.
C MC, P S. Adjusting for confounding by indication in observational studies about traumatic brain injury. Eur J Epidemiol. 2015;30(8):757. http://ovidsp.ovid.com/ovidweb.cgi?T=JS. &PAGE=reference&D=emed17&NEWS=N &AN = 72274417.
Li B, Lingsma HF, Steyerberg EW, Lesaffre E. Logistic random effects regression models: a comparison of statistical packages for binary and ordinal outcomes. BMC Med Res Methodol. 2011;11(1):77. https://doi.org/10.1186/1471-2288-11-77.
Thiry N, Neyt M, Van De Sande S, Cleemput I. Belgian guidelines for economic evaluations: Second Edition. Int J Technol Assess Health Care. 2014;30(6):601–7. https://doi.org/10.1017/S0266462314000725.
Hakkaart-van Roijen L, van der Linden N, Bouwmans C, Kanters T, Swan Tan S, Kostenhandleiding. Methodologie Van kostenonderzoek en referentieprijzen voor economische evaluaties in de gezondheidszorg. Zorginstituut Ned. 2016:1–73. www.zorginstituutnederland.nl/publicaties/publicatie/2016/02/29/richtlijn-voor-hetuitvoeren-van-economische-evaluaties-in-de-gezondheidszorg.
Maas AIR, Menon DK, Steyerberg EW, et al. Collaborative European neurotrauma effectiveness research in traumatic brain injury (CENTRE-TBI): a prospective longitudinal observational study. Neurosurgery. 2015;76(1):67–80. https://doi.org/10.1227/NEU.0000000000000575.
Acknowledgements
The authors would like to thank Finn Seghers (Department of Internal Medicine, UZ Leuven, Belgium) and Thomas de Korte (Department of Radiology, Meander Medical Centre Groningen, The Netherlands) for their input in writing this study protocol.
Funding
This study is sponsored by the Sint Jacobus Stichting, a non-profit organisation. The sponsor has no role in the design of the study and the collection, analysis and interpretation of data.
Author information
Authors and Affiliations
Contributions
This study protocol is written by AH and JD. Furthermore, TV, MB, HS, RA and RF contributed to refinement of the study protocol. The final manuscript was approved by DV, RH, RD, JB, WP and WM.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study is approved by the Medical Ethics Committee Leiden The Hague Delft (METC LDD). The study will be conducted according to the principles of the Declaration of Helsinki (as last modified in October 2013 at the General Assembly in Brazil) and in accordance with the Medical Research Involving Human Subjects Act (WMO).
Recruitment and consent
Patients that present to one of the participating medical centres (primarily or after referral) will be asked to participate and will be consented after being informed about the study, risks, and advantages of participation to acquire informed consent. This procedure will be done according to the protocol “Samenwerkende Topklinische Ziekenhuizen Standard Operating Procedure Informed Consent”. If an eligible patient is identified, prospective data collection will start. This will be noted in the patient file. The written consent from the patient or legal representative should be obtained during the admission period. Information will be giving both verbally and in writing. After given time for consideration, informed consent will be obtained (from the patient or from a representative). The informed consent form will be signed by both the investigator and the patient or representative and participation in the trial will be registered in the patients’ medical file. Other outcomes of the informed consent procedure will also be logged in the patients’ file. After informed consent, prospective data collection will start. This will be noted in the patient file. If a patient withdraws their consent, all data up to the moment the participant withdrew consent will be used for analysis. If informed consent cannot be obtained from the patient or legal representative before emergency treatment or if the patients is incapacitated at time of inclusion and the legal representative is not available, consent will be assumed, and data acquisition started. The consent procedure will be attempted as soon as a legal representative is available, or the subject becomes competent. If patient or legal representative refuses to participate in the study at a first moment of deferred consent, all data will be destroyed.
Some exceptions that are possible on the abovementioned procedure are discussed and a solution is chosen based on both ethical and legal considerations as well as methodological considerations (diminishing of bias). If patients die before the informed consent procedure could be discussed and there is no legally appropriate shared decision making (SDM), no consent is necessary and patients remain included in the study as long as there is no clearly written objection in the chart from the patient against participation in scientific research projects. If patients die and there is a legally appropriate SDM, but there has been no possibility yet to discuss the informed consent procedure, no consent is necessary and patients remain included in the study as long as there is no clearly written objection in the chart from the patient against participation in scientific research projects. In both cases, the reason to deviate from the standard procedure as well as the decision that the patient remains included in the study has to be written clearly in the chart.
Objection by incapacitated subjects
This procedure will be done according to the protocol “Samenwerkende Topklinische Ziekenhuizen Standard Operating Procedure Informed Consent”. If an eligible patient is identified, prospective data collection will start. If the patient is incapacitated at time of inclusion, a representative will be informed about the study and is asked to read the information letter and sign the consent form.
In the case a patient becomes capacitated during the research, an information letter and informed consent form is provided, and informed consent of the patient is gained. If the patient refused to participate in the study, all study data will be destroyed. If a patient becomes incapacitated during the study period, informed consent will be gained again from the representative. In case the representative refused to further participate, all data up to the moment the participant became incapacitated will be used for analysis.
If a patient of whom the legal representative had previously given consent because of incompetence becomes competent and refuses consent to the trial, acquisition of data will cease and data acquired up until then will be used for analysis. If a subject dies during data acquisition before formal consent was given, consent will be assumed and information will be given to legal representatives on how to actively withdraw their consent.
Benefits and risks assessment, group relatedness
Patients will receive normal care during their hospital stay. For study purposes, health questionnaires and functional outcome will be assessed at follow-up. During follow-up, patients will be asked to complete several questionnaires to assess treatment success. These test and questionnaires will take approximately 2 h to complete.
Measurements will be done in the hospital, the outpatient clinic, the rehabilitation centre, or in the patient’s home (in the case of patient reported questionnaires). Patients may experience temporary fatigue from completing questionnaires.
Compensation for injury
The sponsor/investigator has asked the ethical committee to waive the obligatory liability insurance as described in article 7 of the WMO. This is based on the strictly observational nature of the study and the low possibility of damage occurring caused by the study.
Consent for publication
Not applicable.
Handling of data and materials
All data will be treated confidentially and coded and will be registered on data registration forms. Data management will be handled at the Department of Neurosurgery of Leiden University Medical Centre. Data will be stored in an electronic data capture and management system. Imaging data from participating centres will be stored separately in a picture archiving and communication system at the main study centre (imaging from admission and 1, 5- and 10-year follow-up). A list that contains the study participant and associated study identification code will be used to identify an individual study participant if necessary. Every study site has a specific identifier, and subjects will be assigned a study code based on an increasing number. This identification code will not be based on the participant’s initials or date of birth. The list that links the study identification code to the study participants will be kept on a designated partition on the hard drive of the research centre. This part will be protected by a password. People who have access to this partition are local researchers and quality monitor appointed by the principal investigator. These procedures comply with the European law: Algemene verordening gegevensbescherming (AVG). All raw data will be collected and stored at the main study site, including the trial master file, investigator site file, informed consent forms, study data and imaging data. The acquired data will be stored for 15 years after the study is finished and will be used for further research if the participant has provided consent for the data to be used in further studies.
Monitoring and quality assurance
Data monitoring and quality assurance will be handled by the Department of Neurosurgery at Haaglanden Medical Centre. Study monitoring will be done on a yearly basis in each participating centre. An auditing log will be enabled of all study events, changes in study settings and study data. The informed consent forms, the investigator site file and the trial master file, as well as the study data will be monitored.
Competing interests
JHDB has consultancy relationships with Stryker, a manufacturer of detachable coils and stents used for stent-assisted coiling. RHLH and HS from the MUMC started research on factors that cause DCI after SAH, in collaboration with Neuroplast B.V., a Dutch medical biotechnology company specialised in neurodegenerative diseases. WCP reports that LUMC has received research grants from The European Union seventh Framework Program (grant 602150) for CENTER-TBI, Hersenstichting Nederland (Dutch Brain Foundation) for Net-QuRe and CIAO@TBI. The authors have no other relevant affiliations with any organization or entity that have a financial conflict with the subject matter discussed in the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hamming, A.L., van Dijck, J.T., Visser, T. et al. Study on prognosis of acutely ruptured intracranial aneurysms (SPARTA): a protocol for a multicentre prospective cohort study. BMC Neurol 24, 68 (2024). https://doi.org/10.1186/s12883-024-03567-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03567-6