Abstract
Background
Post-stroke neurocognitive disorder, though common, is often overlooked by clinicians. Moreover, although the Montreal Cognitive Assessment (MoCA) has proven to be a valid screening test for neurocognitive disorder, even more time saving tests would be preferred. In our study, we aimed to determine the diagnostic accuracy of the Clock Drawing Test (CDT) for post-stroke neurocognitive disorder and the association between the CDT and MoCA.
Methods
This study is part of the Norwegian Cognitive Impairment After Stroke study, a multicentre prospective cohort study following patients admitted with acute stroke. At the three-month follow-up, patients were classified with normal cognition, mild neurocognitive disorder, or major neurocognitive disorder according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria. Any neurocognitive disorder compromised both mild- and major neurocognitive disorder. The CDT at the three-month assessment was given scores ranging from 0 to 5. Patients able to complete the CDT and whose cognitive status could be classified were included in analyses. The CDT diagnostic accuracy for post-stroke neurocognitive disorder was identified using receiver operating characteristic curves, sensitivity, specificity, positive predictive value, and negative predictive value. The association between the MoCA and CDT was analysed with Spearman’s rho.
Results
Of 554 participants, 238 (43.0%) were women. Mean (SD) age was 71.5 (11.8) years, while mean (SD) National Institutes of Health Stroke Scale score was 2.6 (3.7). The area under the receiver operating characteristic curve of the CDT for major neurocognitive disorder and any neurocognitive disorder was 0.73 (95% CI, 0.68–0.79) and 0.68 (95% CI, 0.63–0.72), respectively. A CDT cutoff of < 5 yielded 68% sensitivity and 60% specificity for any neurocognitive disorder and 78% sensitivity and 53% specificity for major neurocognitive disorder. Spearman’s correlation coefficient between scores on the MoCA and CDT was 0.50 (95% CI, 0.44–0.57, p < .001).
Conclusions
The CDT is not accurate enough to diagnose post-stroke neurocognitive disorder but shows acceptable accuracy in identifying major neurocognitive disorder. Performance on the CDT was associated with performance on MoCA; however, the CDT is inferior to MoCA in identifying post-stroke neurocognitive disorder.
Trial registration
ClinicalTrials.gov (NCT02650531). Retrospectively registered January 8, 2016.
Similar content being viewed by others
Background
Although the incidence of stroke has decreased, increased longevity, population ageing, and the improved survival of stroke patients have increased the prevalence of stroke survivors [1]. Half of all survivors develop cognitive impairment following stroke [2], which increases the burden for them, their relatives and the healthcare system [3,4,5].
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [6] has introduced the terms mild- and major neurocognitive disorder (NCD), replacing the traditionally used terms mild cognitive impairment and dementia, respectively. Clinical experience has shown that post-stroke NCD is often overlooked in stroke care, often due to the lack of time and capacity needed to perform extensive evaluation of all stroke survivors. In response, a brief and valid screening tool could be the first step to identify patients who need more comprehensive diagnostic assessment and tailored follow-up [7].
In assessing post-stroke NCD, the Mini Mental State Exam (MMSE) exhibits a ceiling effect, and its diagnostic accuracy among stroke survivors is debated [8,9,10]. The Montreal Cognitive Assessment (MoCA), by contrast, has shown more promising results [8, 11,12,13]. Although the MoCA was developed as a 10-min screening tool [14], clinicians experience that it often is more lengthy to perform. To minimise the risk of overlooking post-stroke NCD in busy clinical practice, less time-consuming screening tools would be favourable, such as the Clock Drawing Test (CDT) [15]. The CDT assesses a variety of cognitive domains, including perceptual-motor function, executive function, complex attention (selective and sustained), memory (semantic), and language (receptive) [16,17,18]. Its diagnostic accuracy for non-stroke NCD is well documented with good intra- and interrater reliability [19, 20]. To our knowledge, only one previous study has examined the diagnostic accuracy of the CDT for post-stroke NCD, presenting adequate levels of sensitivity and specificity [21]. The study’s sample of 98 participants was small. Therefore, a replication of this study with a larger sample size is requested.
We aimed to determine the diagnostic accuracy of the CDT as a screening tool for post-stroke NCD diagnosed according to the DSM-5 criteria, and the association between patients’ CDT score and MoCA score three months post-stroke.
Methods
Our study is part of the Norwegian Cognitive Impairment After Stroke (Nor-COAST) study, a multicentre prospective cohort study involving 815 patients admitted with acute stroke at five hospitals in Norway [22]. Consecutive patients with confirmed diagnoses of acute stroke, were included during the initial hospital stay. The inclusion criteria were admission with acute stroke within seven days of symptom debut to a stroke unit in one of the participating hospitals, being at least 18 years old and being able to communicate in a Scandinavian language. Exclusion criteria were a life expectancy less than three months, as clinically assessed by trained study nurses and stroke physicians. Participant recruitment proceeded from May 2015 through May 2017, and participants were followed up at three, 18 and 36 months after the stroke. The Nor-COAST study is described in greater detail elsewhere [22, 23]. Patients able to complete the CDT as part of the MoCA and whose cognitive status could be classified were included in our study.
Baseline characteristics
Information about the patients’ socio-demographic characteristics, medical history and premorbid function was collected during their initial hospital stays from medical records and through interviews with participants and/or caregivers. The modified Rankin Scale, with scores 0–6, was used to evaluate global function before and after stroke [24, 25], while activities of daily living were assessed using the Barthel Index [26]. Stroke severity was evaluated using the National Institutes of Health Stroke Scale (NIHSS) [27], on the day after admission, whereas ischemic stroke subtype was classified according to the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification [28]. Last, information about pre-stroke cognitive impairment was assessed by trained nurses using the Global Deterioration Scale [29], originally developed for assessment of primary degenerative dementia, but proven valid also for vascular dementia [30, 31].
Cognitive assessments
At the three-month follow up, participating patients underwent cognitive assessment with a neurocognitive test battery and the MoCA at the hospitals’ outpatient clinics. The neurocognitive test battery was based on recommendations from the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network [32], the 30-min version. The tests used had previously been translated into Norwegian and assessed the following cognitive domains: complex attention (Trail Making Test A [33]), executive function (Trail Making Test B [33] and Verbal Fluency test letter [FAS] [34, 35]), memory (Word List Recall [36]), language (Verbal Fluency Test Category-Animals [37]), and perceptual-motor function (visuospatial/executive subtest of MoCA [14]). Social cognition was not assessed. In previous work in the Nor-COAST study, cognitive status was classified according to the DSM-5 criteria for NCD [23]. NCD was defined as a score less than − 1.5 standard deviation (SD) in at least one cognitive domain. Mild NCD was defined as NCD and independence in instrumental activities of daily living and major NCD as NCD and dependency in instrumental activities of daily living [23].
All participants were assessed by the MoCA, a global cognitive screening test with maximum score of 30, with an additional point for education ≤ 12 years [14]. After initial testing, the CDT tasks from MoCA were rescored in accordance with a 6-point Norwegian scoring method, previously published by Strobel et al., and commonly used by Norwegian clinicians ([38, 39], for English adaptation please see Supplementary Material, Table S1 and Fig. S1-S4). In Strobel et al.’s scoring method, participants are handed a pre-printed circle used to draw a clock. In the CDT task of MoCA, participants are instructed to draw the circle by hand. In accordance with the scoring method by Strobel et al., the ability to draw a circle was not assessed. Strobel et al. recommend a cutoff < 4 for the diagnosis of NCD. To investigate the impact of different cutoff values on the CDT’s diagnostic accuracy for post-stroke NCD, we performed analyses with two cutoff values: < 4 (i.e., scores of 0–3 indicating NCD, and scores of 4–5 indicating normal cognition) and < 5 (i.e., scores 0–4 indicating NCD, and a score of 5 indicating normal cognition).
Statistics
To minimise bias and the loss of sample size due to excluded participants, missing items in the MoCA scores were imputed by the mean of the available MoCA items for the same participant. The three-category cognitive status was dichotomised into normal cognition and any NCD (i.e., mild- or major NCD) and into normal cognition/mild NCD and major NCD [40]. The CDT’s accuracy in diagnosing any NCD and major NCD was quantified in terms of sensitivity and specificity for the CDT score cutoff values of < 4 and < 5, as well as in terms of positive predictive value and negative predictive value. Confidence intervals (CI) for proportions were calculated using the Wilson score method [41]. We also calculated the area under the receiver operating characteristic curve (AUC) for both any- and major NCD. We interpret AUC values as suggested by Hosmer et al. [42] as 0.5 to 0.7 indicating poor discrimination, 0.7 to 0.8 as acceptable, 0.8 to 0.9 as excellent, and above 0.9 as outstanding. The association between scores on the MoCA and CDT was quantified using Spearman’s correlation. All statistical analyses were performed using IBM SPSS Statistics version 28.0.1.
Results
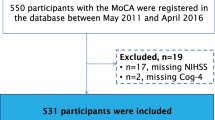
As shown by Kuvås et al. [43], 2505 patients with the diagnosis of stroke were admitted to the participating hospitals during the recruitment period, of these, 559 were not eligible. The rest were not included because they were declining participation, discharged early, failed to be screened or for other reasons. Of the 815 included participants in the Nor-COAST study, 261 were not assessed or had missing data at three-months. These tended to be older and to have more severe strokes (Fig. 1).
Our study included 554 participants able to complete the CDT task from the MoCA and whose cognitive status could be classified at the three-month follow-up. All included participants were able to draw a circle for the clock. Of them, 238 (43.0%) were women, the mean (SD) age was 71.5 (11.8) years, and patients suffered mostly minor strokes (Table 1). Pre-stroke Global Detoriation Scale scores revealed that few patients had NCD prior to stroke. At three months post-stroke, 253 participants (45.7%) had normal cognition, 161 (29.1%) had mild NCD and 140 (25.3%) had major NCD according to the DSM-5 criteria [23].
Diagnostic accuracy of the Clock Drawing Test (CDT)
Cross-tabulations for the CDT score cutoff values of < 4 and < 5 and the three-category cognitive status are shown in Table 2. Using CDT cutoff < 4, 129 and 64 participants with any- and major NCD, respectively, were false negatives due to having CDT scores above the cutoff value. A CDT cutoff < 5 identified a larger number of participants with NCD; however, the number of false positives increased to 100. The corresponding measures for diagnostic accuracy are shown in Table 3. Sensitivity for major NCD given a cutoff value of < 5 was 78% (95% CI, 70–84), whereas specificity was 53% (95% CI, 48–58). For any NCD, a CDT cutoff < 5 yielded a sensitivity of 68% (95% CI, 62–73) and a specificity of 61% (95% CI, 54–66). As expected, a CDT cutoff < 4 yielded lower sensitivity but higher specificity for both any- and major NCD (Table 3).
Receiver operating characteristic (ROC) curves of the CDT for any- and major post-stroke NCD with corresponding AUC values are shown in Fig. 2.
Association between the Montreal Cognitive Assessment (MoCA) and Clock Drawing Test (CDT)
Spearman’s correlation coefficient between MoCA and CDT scores was 0.50 (95% CI, 0.44–0.57). Table 4 shows the mean MoCA scores for patients with CDT scores 0–5 and CDT scores above or below the cutoff values of < 4 and < 5, respectively. Patients receiving lower scores on the CDT tend to receive lower scores on the MoCA.
Discussion
For the purpose of identifying patients with post-stroke NCD, the CDT demonstrated acceptable diagnostic accuracy for major NCD but failed to identify a substantial number of patients with any NCD (i.e., mild and major NCD). Moreover, despite an observed association between performance on the CDT and performance on the MoCA, the CDT is inferior to MoCA in screening for post-stroke NCD.
The purpose of a cognitive screening test is to identify patients who need a more comprehensive assessment for NCD, with sensitivity being of greater importance than specificity. In our study, the best balance between sensitivity and specificity was achieved by employing a CDT cutoff < 5. The CDT proved to have acceptable diagnostic accuracy for major NCD; however, its sensitivity for any NCD was lower with a similarly lower AUC. Thus, in using only the CDT, healthcare professionals are liable to overlook a substantial proportion of patients with mild NCD. If undetected, mild NCD is associated with an increased risk of reduced quality of life and poorer prognosis due to weak adherence to medication and a lack of tailored cognitive and physical stimulation that could prevent further cognitive decline [5, 44,45,46].
To our knowledge, only one study to date has investigated the CDT’s accuracy in diagnosing NCD among stroke survivors. In that research, Cova et al. observed a sensitivity of 80%, specificity of 76% and an AUC of 0.86 [21]. Several methodological differences between our studies might explain the divergence in our results. For one, Cova et al. employed a rather more comprehensive scoring system for the CDT, one with scores ranging from 0 to 13. For another, patients were evaluated in the acute phase following stroke, and the diagnosis of NCD was based on clinical judgment of the evaluating neurologist, not on the results of a neurocognitive test battery. As part of the Nor-COAST study, Munthe-Kaas studied the diagnostic accuracy of MoCA for NCD [12]. In that research, the MoCA had an AUC approaching 0.80 with 71% sensitivity and 73% specificity for post-stroke NCD, and other studies have revealed similar results [13, 21, 47, 48]. Compared to the results of our study, the CDT is inferior to the MoCA as a screening tool for post-stroke NCD.
All cognitive domains mentioned in DSM-5 except social cognition were assessed in the Nor-COAST study. Of these, all, except motor function were impaired, with memory most severely affected [2]. Although the CDT requires semantic memory regarding what a clock look like, it is better at assessing visuospatial and executive impairments [16,17,18]. This might somewhat explain why so many patients with NCD earn CDT scores above the cutoff values (i.e., false negatives). Ideally, to achieve high sensitivity for post-stroke NCD, a cognitive screening tool should assess all six cognitive domains [49]. In that light, the CDT falls short of the MoCA, which provides a more extensive cognitive evaluation [14, 50]. However, the CDT might be less influenced than the MoCA by verbal impairments, which are highly prevalent after stroke [51]. For that reason, the CDT may be more feasible among stroke patients with impairments in verbal expression following stroke.
A major strength of our study was its multicentre design with a high number of participants from five stroke units in different health regions in Norway [43]. Another strength was that we defined NCD according to the DSM-5 criteria and assessed patients using a neurocognitive test battery recommended for stroke patients [23, 32]. Finally, the CDT is generally quick and easy to administer and widely used in clinical practice, and we applied a scoring system well-known to many clinicians.
Our findings have some limitations. Although, the Nor-COAST population can be regarded as representative of the majority of the stroke population [43], patients included in the present study were younger and had milder strokes, which lowers their risk for post-stroke NCD. This may have affected the applicability of our results to the general stroke population. As expected, CDT and MoCA scores were associated, but we compared the MoCA with a sub-test of MoCA, which might have weakened the credibility of our results. However, we applied a different scoring method, which may have reduced the significance of this. An optimal study design would be to perform the entire CDT in accordance with Strobel’s method, including giving participants a pre-drawn circle and the ability to redo the test if unsatisfied. In this study, participants were instructed to draw a circle. These were sometimes small or uneven, and the numbers and hands of the clock were sometimes poorly aligned, which in our scoring method meant lower scores [38]. This could have increased the rate of false positives.
Conclusion
Our findings suggest that although the CDT has acceptable diagnostic accuracy for major NCD following stroke, many patients with mild impairments are likely to be overlooked. The CDT is inferior to the MoCA in screening for post-stroke NCD, and though the CDT is better than no screening whatsoever, based on the present study, we do not recommend it as a routine screening test for post-stroke NCD. Clinicians should rely on other neurocognitive tests, such as MoCA. It may be hypothesized that the CDT applied together with reports on subjective cognitive difficulties or a brief neurocognitive test assessing memory, would increase diagnostic accuracy for post-stroke NCD. Further research on these subjects is needed, as well as on which specific domains are associated with impaired CDT scores.
Availability of data and materials
The datasets used in the study are not publicly available but are available from the corresponding author upon reasonable request.
Abbreviations
- Nor-COAST study:
-
Norwegian Cognitive Impairment After Stroke study
- NCD:
-
Neurocognitive disorder
- CDT:
-
Clock Drawing Test
- MoCA:
-
Montreal Cognitive Assessment
- MMSE:
-
Mini Mental State Examination
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- NIHSS :
-
National Institutes of Health Stroke Scale
- ROC curve :
-
Receiver operating characteristic curve
- AUC :
-
Area under the receiver operating characteristic curve
- CI :
-
Confidence interval
- SD :
-
Standard deviation
References
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383(9913):245–54.
Aam S, Einstad MS, Munthe-Kaas R, Lydersen S, Ihle-Hansen H, Knapskog AB, et al. Post-stroke Cognitive Impairment-Impact of Follow-Up Time and Stroke Subtype on Severity and Cognitive Profile: The Nor-COAST Study. Front Neurol. 2020;11:699.
Claesson L, Lindén T, Skoog I, Blomstrand C. Cognitive impairment after stroke - impact on activities of daily living and costs of care for elderly people. The Göteborg 70+ Stroke Study. Cerebrovasc Dis. 2005;19(2):102–9.
Leys D, Hénon H, Mackowiak-Cordoliani MA, Pasquier F. Poststroke dementia. Lancet Neurol. 2005;4(11):752–9.
Lo Coco D, Lopez G, Corrao S. Cognitive impairment and stroke in elderly patients. Vasc Health Risk Manag. 2016;12:105–16.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Helsedirektoratet. Nasjonal faglig retningslinje for behandling og rehabilitering ved hjerneslag [National Clinical Guideline for Treatment and Rehabilitation of Stroke] Oslo: Helsedirektoratet; 2017 (updated 27.04.2020; cited 20.05.2022). Available from: https://www.helsedirektoratet.no/retningslinjer/hjerneslag. Norwegian.
Pendlebury ST, Cuthbertson FC, Welch SJ, Mehta Z, Rothwell PM. Underestimation of cognitive impairment by Mini-Mental State Examination versus the Montreal Cognitive Assessment in patients with transient ischemic attack and stroke: a population-based study. Stroke. 2010;41(6):1290–3.
Blake H, McKinney M, Treece K, Lee E, Lincoln NB. An evaluation of screening measures for cognitive impairment after stroke. Age Ageing. 2002;31(6):451–6.
Srikanth V, Thrift AG, Fryer JL, Saling MM, Dewey HM, Sturm JW, et al. The validity of brief screening cognitive instruments in the diagnosis of cognitive impairment and dementia after first-ever stroke. Int Psychogeriatr. 2006;18(2):295–305.
Dong Y, Sharma VK, Chan BP, Venketasubramanian N, Teoh HL, Seet RC, et al. The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke. J Neurol Sci. 2010;299(1–2):15–8.
Munthe-Kaas R, Aam S, Saltvedt I, Wyller TB, Pendlebury ST, Lydersen S, et al. Test Accuracy of the Montreal Cognitive Assessment in Screening for Early Poststroke Neurocognitive Disorder: The Nor-COAST Study. Stroke. 2021;52(1):317–20.
Pendlebury ST, Mariz J, Bull L, Mehta Z, Rothwell PM. MoCA, ACE-R, and MMSE versus the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network Vascular Cognitive Impairment Harmonization Standards Neuropsychological Battery after TIA and stroke. Stroke. 2012;43(2):464–9.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry. 2000;15(6):548–61.
Shulman KI, Shedletsky R, Silver IL. The challenge of time: Clock-drawing and cognitive function in the elderly. Int J Geriatr Psychiatry. 1986;1(2):135–40.
Royall DR. Comments on the executive control of clock-drawing. J Am Geriatr Soc. 1996;44(2):218–9.
Mendez MF, Ala T, Underwood KL. Development of scoring criteria for the clock drawing task in Alzheimer’s disease. J Am Geriatr Soc. 1992;40(11):1095–9.
Park J, Jeong E, Seomun G. The clock drawing test: A systematic review and meta-analysis of diagnostic accuracy. J Adv Nurs. 2018;74(12):2742–54.
Pinto E, Peters R. Literature review of the Clock Drawing Test as a tool for cognitive screening. Dement Geriatr Cogn Disord. 2009;27(3):201–13.
Cova I, Mele F, Zerini F, Maggiore L, Cucumo V, Brambilla M, et al. Neuropsychological screening in the acute phase of cerebrovascular diseases. Acta Neurol Scand. 2020;142(4):377–84.
Thingstad P, Askim T, Beyer MK, Bråthen G, Ellekjær H, Ihle-Hansen H, et al. The Norwegian Cognitive impairment after stroke study (Nor-COAST): study protocol of a multicentre, prospective cohort study. BMC Neurol. 2018;18(1):193.
Munthe-Kaas R, Aam S, Ihle-Hansen H, Lydersen S, Knapskog AB, Wyller TB, et al. Impact of different methods defining post-stroke neurocognitive disorder: The Nor-COAST study. Alzheimers Dement (N Y). 2020;6(1):e12000.
Rankin J. Cerebral vascular accidents in patients over the age of 60 II. Prognosis Scott Med J. 1957;2(5):200–15.
Farrell B, Godwin J, Richards S, Warlow C. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991;54(12):1044–54.
Mahoney FI, Barthel DW. FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Md State Med J. 1965;14:61–5.
Lyden PD, Lu M, Levine SR, Brott TG, Broderick J. A modified National Institutes of Health Stroke Scale for use in stroke clinical trials: preliminary reliability and validity. Stroke. 2001;32(6):1310–7.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–9.
Paul RH, Cohen RA, Moser DJ, Zawacki T, Ott BR, Gordon N, et al. The global deterioration scale: relationships to neuropsychological performance and activities of daily living in patients with vascular dementia. J Geriatr Psychiatry Neurol. 2002;15(1):50–4.
Choi SH, Lee BH, Kim S, Hahm DS, Jeong JH, Yoon SJ, et al. Interchanging scores between clinical dementia rating scale and global deterioration scale. Alzheimer Dis Assoc Disord. 2003;17(2):98–105.
Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37(9):2220–41.
Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8(3):271–6.
Bechtoldt HP, Benton AL, Fogel ML. An application of factor analysis in neuropsychology. Psychological Record. 1962;12(2):147–56.
Fogel ML. The gerstmann syndrome and the parietal symptom-complex. Psychological Record. 1962;12(1):85–99.
Morris JC, Mohs RC, Rogers H, Fillenbaum G, Heyman A. Consortium to establish a registry for Alzheimer’s disease (CERAD) clinical and neuropsychological assessment of Alzheimer’s disease. Psychopharmacol Bull. 1988;24(4):641–52.
Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology. 1989;39(9):1159–65.
Strobel C, Aga O, Bekkhus-Wetterberg P, Brierley M, Bystad M, Engedal K, et al. Norsk Revidert Klokketest (KT-NR3) [Norwegian Revised Clock Drawing Test (KT-NR3)]: Aldring og Helse, nasjonal kompetansetjeneste; 2021 (cited 21.05.2022). Available from: https://www.aldringoghelse.no/wp-content/uploads/2021/09/kt-nr3-testskjema2021-master.pdf. Norwegian.
Strobel C, Aga O, Bekkhus-Wetterberg P, Brierley M, Bystad M, Engedal K, et al. Skåringsillustrasjoner Klokketest [The Clock Drawing Test Visual Scoring Templates, English]: Aldring og Helse, nasjonal kompetansetjeneste; 2021 (cited 07.10.2023). Available from: https://www.aldringoghelse.no/wp-content/uploads/2021/09/skaringsillustrasjoner-klokketest-2021-master.pdf. Norwegian.
Schellhorn T, Aamodt EB, Lydersen S, Aam S, Wyller TB, Saltvedt I, et al. Clinically accessible neuroimaging predictors of post-stroke neurocognitive disorder: a prospective observational study. BMC Neurol. 2021;21(1):89.
Fagerland M, Lydersen S, Laake P. Statistical Analysis of Contingency Tables. Boca Raton, FL: Chapman & Hall/CRC; 2017.
Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2013.
Kuvås KR, Saltvedt I, Aam S, Thingstad P, Ellekjær H, Askim T. The Risk of Selection Bias in a Clinical Multi-Center Cohort Study. Results from the Norwegian Cognitive Impairment After Stroke (Nor-COAST) Study. Clin Epidemiol. 2020;12:1327–36.
Ismail Z, Elbayoumi H, Fischer CE, Hogan DB, Millikin CP, Schweizer T, et al. Prevalence of Depression in Patients With Mild Cognitive Impairment: A Systematic Review and Meta-analysis. JAMA Psychiat. 2017;74(1):58–67.
Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119(4):252–65.
Jekel K, Damian M, Wattmo C, Hausner L, Bullock R, Connelly PJ, et al. Mild cognitive impairment and deficits in instrumental activities of daily living: a systematic review. Alzheimers Res Ther. 2015;7(1):17.
Godefroy O, Fickl A, Roussel M, Auribault C, Bugnicourt JM, Lamy C, et al. Is the Montreal Cognitive Assessment superior to the Mini-Mental State Examination to detect poststroke cognitive impairment? A study with neuropsychological evaluation. Stroke. 2011;42(6):1712–6.
Cumming TB, Churilov L, Linden T, Bernhardt J. Montreal Cognitive Assessment and Mini-Mental State Examination are both valid cognitive tools in stroke. Acta Neurol Scand. 2013;128(2):122–9.
Brainin M, Tuomilehto J, Heiss WD, Bornstein NM, Bath PM, Teuschl Y, et al. Post-stroke cognitive decline: an update and perspectives for clinical research. Eur J Neurol. 2015;22(2):229–38, e13-6.
Ismail Z, Rajji TK, Shulman KI. Brief cognitive screening instruments: an update. Int J Geriatr Psychiatry. 2010;25(2):111–20.
Berthier ML. Poststroke aphasia : epidemiology, pathophysiology and treatment. Drugs Aging. 2005;22(2):163–82.
Acknowledgements
We wish to thank all patients for their contributions to our study, as well as the Nor-COAST research group and the dedicated staff at St. Olavs Hospital, Haukeland University Hospital, Ålesund Hospital, Vestre Viken Hospital Trust, Bærum Hospital and Oslo University Hospital (Ullevål). We would also like to thank Carsten Strobel, Peter Bekkhus-Wetteberg, Martin Brierley, and Katinka Odner for providing us with the English adaptation of the scoring table for the CDT and The Clock Drawing Test Visual Scoring Templates.
Funding
Open access funding provided by Norwegian University of Science and Technology The Nor-COAST study is funded by the Norwegian Health Association, with additional funding provided by the Department of Neuromedicine and Movement Science in the Faculty of Medicine and Health Science at Norwegian University of Science and Technology.
Author information
Authors and Affiliations
Contributions
EN, IS and SA planned and designed the study. EN, IS, SL and SA planned the statistical analyses, EN and SL performed the analyses, and all authors contributed to interpretation of the data. EN, IS and SA were the main contributors in writing-up the manuscript, which all authors, including RMK, HIH and RG, subsequently reviewed and approved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. Participants provided their informed written consent, and if patients could not provide consent due to severe dementia or other illness, then their informed written consent was obtained from their next of kin. The study was approved by Regional Committee for Medical and Health Research Ethics (REC Nord 2015/171), UiT Norges arktiske universitet, University of Science and Technology.
Consent for publication
Not applicable.
Competing interests
SA has been a consultant in Eisai's National Norwegian Alzheimer disease advisory board meeting. The remaining authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Scoring table for CDT, English adaptation 2023 and Clock Drawing Test Visual Scoring Templates, English adaptation 2023.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Navickaite, E., Saltvedt, I., Lydersen, S. et al. Diagnostic accuracy of the Clock Drawing Test in screening for early post-stroke neurocognitive disorder: the Nor-COAST study. BMC Neurol 24, 22 (2024). https://doi.org/10.1186/s12883-023-03523-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-023-03523-w