Abstract
Background
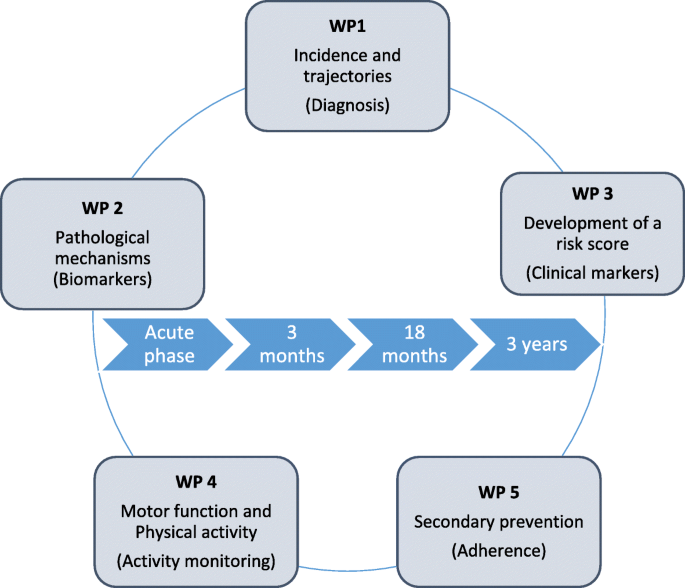
Early and late onset post-stroke cognitive impairment (PCI) contributes substantially to disability following stroke, and is a high priority within stroke research. The aetiology for PCI is complex and related to the stroke itself, brain resilience, comorbid brain diseases, prestroke vulnerability and complications during the hospital stay. The aim of the Norwegian Cognitive Impairment After Stroke study (Nor-COAST) is to quantify and measure levels of cognitive impairments in a general Norwegian stroke population and to identify biological and clinical markers associated with prognosis for cognitive disorders following incident stroke. The study will be organised within five work packages: 1) Incidence and trajectories 2) Pathological mechanisms 3) Development of a risk score 4) Impact of physical activity and 5) Adherence to secondary prevention.
Methods
Nor-COAST is an ongoing multicentre (five participating hospitals), prospective, cohort study with consecutive inclusion during the acute phase and with follow-up at three and 18 months, and at three years. Inclusion criteria are stroke defined according to the WHO criteria. During the recruitment period from 18.05.2015 to 31.03.2017, 816 participants have been included. Cognitive impairment will be classified according to the DSM-5 criteria using a consensus group. Cognitive function is assessed by a standardised neuropsychological test battery, the Montreal Cognitive Assessment, Trail making A and B, ten-word immediate and delayed recall test, the Controlled Oral Word Association, Global Deterioration Scale and proxy based information by and the Ascertain Dementia 8 item informant questionnaire. Biomarkers include magnetic resonance imaging, routine blood samples and bio-banking. Clinical assessments include characteristics of the stroke, comorbidity, delirium, frailty and tests for cognitive and physical function, sensor based activity monitoring and adherence to secondary prophylaxis.
Discussion
Nor-COAST is the first Norwegian multicentre study to quantify burden of PCI that will provide reliable estimates in a general stroke population. A multidisciplinary approach aiming to identify biomarkers and clinical markers of overall prognosis will add new knowledge about risk profiles, including pre-stroke vulnerability and modifiable factors such as physical activity and secondary prophylaxis of relevance for clinical practice and later intervention studies.
Trial registration
ClinicalTrials.gov: NCT02650531. Retrospectively registered January 8, 2016. First participant included May 18, 2015.
Similar content being viewed by others
Background
Stroke and cognitive impairment are common in old age. One in three persons will develop stroke, dementia or both [1], and the two conditions commonly coexist [2]. Impaired cognitive function contributes to the disability following stroke [3] and affects both the individual and the family and caregivers. With increased longevity and ageing population, stroke and dementia will constitute a substantial part of the disease burden in the years to come [4] with a potentially large socioeconomic gain when improving treatment and preventive strategies.
Cognitive function is therefore defined as a top priority for stroke research, especially studies of the links between cerebrovascular and degenerative disease are requested [5,6,7]. The term post-stroke cognitive impairment (PCI) is used to describe both mild cognitive impairment (MCI) and dementia that either become manifest three to six months after incident stroke (early-onset PCI) or develops over months and years (late-onset PCI). The observed delayed and accelerated decline in cognitive function after incident stroke suggest there is a therapeutic window for intervention and prevention of PCI [7]. Identification of biomarkers and clinical markers for risk of progression of PCI, could improve our understanding of the underlying pathological processes and help develop new strategies to reduce the burden of PCI.
Incidence and trajectories of PCI
Reported rates for PCI varies considerably between studies. Many studies reports dementia but not MCI, and in studies that include MCI the operational definition has a large impact on the reported rate [8]. Pooled dementia rates suggest that 10% of first ever stroke survivors develop incident dementia within the first year, and 30% after recurrent stroke [9]. A Norwegian study reported an incidence of MCI and dementia one year after first ever stroke of 37.5 and 19.6%, respectively [10]. Heterogenity in reported rates of cognitive impairment following stroke can be explained by casemix differences resulting from population selection and attrition bias [6] and by varying assessment time and tools, operational definitions and diagnostic criteria [8]. Further there are few studies on the course of PCI, especially of late-onset PCI, and it is hypothesised that the course of PCI strongly depends on the underlying mechanisms [11,12,13,14]. To quantify the overall burden of PCI and explore distinct trajectories and their determinants, larger inclusive studies with longer follow-up are warranted.
Biomarkers and predictors of PCI
A complex interplay of vascular pathology, neurodegenerative and inflammatory processes contributes to the progression of PCI [11, 14,15,16]. Cognitive impairment predisposes to stroke [15, 16] and patients with dementia get more severe strokes [17], supporting that the two conditions are related. Several imaging characteristics associated with PCI have been identified. Some imaging findings are more extensively studied, especially the relationship between white matter hyperintensities and cognitive impairment [18]. However, recently there has been more attention on the association between degenerative and vascular changes in the brain [2]. Chronic inflammation seems to be involved in the pathogenesis of both cerebrovascular disorders and Alzheimer’s disease. Immune activation and immune depression are present in the acute, sub-acute and chronic stage after a stroke and diminished or impaired inflammatory mechanisms are likely to be important factors in the pathways leading to dementia [19]. Cytokines are potential drivers in addition to neurovascular dysfunction, endothelial activation [20, 21] and genetic risk including Apolipoprotein Eε4 (APOE ε4) carrier status [22]. Several clinical markers are predictors of PCI, and the risk appears to increase with increasing number of predictors. Predictors include age, pre-stroke cognitive impairment, pre-stroke functioning and frailty as well as characteristics of the stroke lesion. In addition, complications in the acute and sub-acute phase as delirium, infections, falls and seizures seem to increase the risk [6].
Early and late-onset PCI is probably driven by somewhat different mechanisms, with brain resilience and characteristics of the stroke lesion being the dominant driver for early-onset PCI, while small vessel disease, Alzheimer pathology and recurrent strokes are more pronounced in late-onset PCI [11, 14, 23, 24].
Secondary prevention, adherence and physical activity
Prevention of recurrent strokes is important in preventing PCI [6] and can probably be achieved in up to 80% by optimal secondary prevention [25]. A multi domain intervention including vascular risk monitoring and physical activity has shown to prevent cognitive decline in at-risk stroke free elderly people suggesting that secondary prevention could have an additional and independent effect on cognition and overall brain health [26]. However, guidelines for secondary prevention are rather complex, involving secondary preventive medications and healthy lifestyle including smoking cessation, moderate alcohol consumption, healthy diet and regular physical activity [27]. Adherence to both medication and lifestyle interventions have been reported to be suboptimal in many patients [28], and adherence to secondary prevention may be problematic in patients with cognitive impairment after stroke.
There is evidence that physical activity enhances cognitive function after stroke [29], and especially executive function in individuals with MCI [30]. A recent meta-analysis, representing data from 736 participants included in 14 randomized controlled trials, demonstrated a significant positive effect of physical activity on cognition post-stroke [31]. Possible mechanisms involved are reduced levels of inflammation [32], improved brain circulation, neurogenesis and increased size of hippocampus [33, 34]. On the other hand, sedentary behaviour has been identified as a risk factor for vascular disease, and hypothesized to increase the risk of cognitive impairment after stroke [35].
Study aims
The aim of the Norwegian Cognitive Impairment After Stroke study (Nor-COAST), is to quantify and measure levels of cognitive impairments in a Norwegian general stroke cohort and to identify biomarkers and clinical markers associated with overall prognosis for early and late onset PCI.
The Nor-COAST study is organised within five work packages (WP). The aim of WP 1 is to describe incidence and distinct trajectories of PCI. In WP 2, the aim is to increase knowledge concerning the pathogenesis of early and late-onset PCI by analysing brain imaging, APOE ε4 typing and blood markers, and to explore associations between neurodegenerative disease, underlying vascular disease, inflammation and stroke characteristics. In WP 3, we aim to identify predictors for PCI in order to develop a novel risk score consisting of a few clinical markers that will enable planning of individualized prevention and treatment. The aim of WP 4 is to study the impact of physical activity and sedentary behaviour on PCI in the short and long term, and to explore associations between motor function measured by performance based tests and progression of PCI. WP 5 aims to explore the impact of cognitive function on adherence to secondary prevention and evaluate whether optimal secondary prophylaxis is protective against decline in cognitive function over time Fig. 1.
Methods/design
The Nor-COAST study is a multicentre, prospective, cohort study following participants for three years from the stroke incident. Recruitment started successively at the different sites between 18.05.2015 and 01.09.2016 and was ended as preplanned 31.03.2017, with 816 participants included. Participants were recruited from five Norwegian stroke units at the following hospitals; St. Olavs University Hospital, Trondheim (n = 400); Ålesund Hospital, Møre and Romsdal Health Trust, Ålesund (n = 33), Haukeland University Hospital, Bergen (n = 142); Bærum Hospital, Vestre Viken Hospital Trust, Drammen (n = 142) and Oslo University Hospital, Ullevål, Oslo (n = 99). All patients admitted to the participating stroke-units were consecutively screened for eligibility and approached as soon as the diagnosis was confirmed. Informed consent was given prior to data collection by the participant or by proxy if the participant lacked capacity to give informed consent. All participants received treatment and routine follow-up as usual in accordance with national and international guidelines [36, 37].
Sample size
Based on the Norwegian stroke registry we estimated that about 1000 stroke patients in total would be available for inclusion per year in the participating hospitals. Experience from earlier studies at the same hospitals involved [10, 38] indicated that about half of eligible participants would be included and that 20–25% would be lost to follow-up during the data collection period of 18 months. With 750 patients available for follow-up, we will be able to detect an association corresponding to a correlation of 0.11 or higher (power 86% at significance level 5%). Inclusion of approximately 1000 participants would therefore be sufficient to answer the main research questions within each work package. Based on these assumptions we decided on a preplanned inclusion stop at 1000 participants or a maximum of two years inclusion period.
Participants
Eligibility criteria are: 1) Admittance to one of the five centres within seven days after symptom debut. 2) Acute stroke diagnosed according to the World Health Organisation (WHO) criteria or with findings of acute infarction or intra-cerebral haemorrhage on MRI. 3) Scandinavian speaking 4) over > 18 years and 5) living in the catchment area of the recruiting hospitals. Exclusion criteria were expected survival less than three months.
Data collection and assessments
Assessments during the hospital stay are performed at discharge or the seventh day of the stay for participants with longer hospital stay. Study related follow-ups are performed at the outpatient clinic three and 18 months, and three years’ post-stroke. Participants unable to attend the outpatient clinic are assessed by telephone interview and/or proxy information is collected. Assessments and interviews are performed by trained research assistants, using a standardised paper Case Report Form (CRF), and then plotted in web-based CRF developed by the Unit for Applied Clinical Research, NTNU. Table 1 provides an overview of data collected by time and data source.
Outcomes and measurements
Demographics, health history and disability
Sociodemographic characteristics are registered based on medical records and interviews with patients and/or caregivers. Information of health history, premorbid function and life style habits are recorded using standardised questionnaires from the Norwegian stroke registry and the North-Trøndelag Health (HUNT) Study. Charlson comorbidity index identifies comorbidity, [39] and a measure of frailty is achieved by the FRAIL scale [40]. The Modified Rankin Scale (mRS) evaluates the global function, and instrumental activities of daily living (I-ADL) is assessed by the Nottingham Extended ADL scale [41] with the 4 subdomains of mobility, leisure time activity, kitchen and domestic work. For basic ADL, the Barthel Index [42] is used assessing independence in 10 basic ADL functions. Health related quality of life is assessed using EQ-5D-5 L, [43] and fatigue by the seven-item version of the Fatigue severity scale (FSS-7) [44].
Stroke characteristics, complications and medical treatment
Stroke symptoms and severity is assessed by National Institutes of Health Stroke Scale (NIHSS). Strokes are classified according to the Oxfordshire Stroke Classification Project (OSCP) [45] and the TOAST classification [46]. The confusion assessment method (CAM four item version) for delirium evaluation is performed by the nurses the first two days of hospital stay [47]. Acute treatment, including thrombolysis and thrombectomies is obtained from medical records. Use of medication at the time of admission and at discharge is recorded based on information from participants, proxies and medical records. All drugs are classified by using the ATC-classification system. Evaluation of the adherence to medication at three and 18 months are based on self-reports according to the 4-item Morisky Medication Adherence Scale (MMAS-4) [48]. Follow-up routines in primary health care will be investigated in a substudy.
Neuropsychological assessment
MCI and dementia are diagnosed according to the DSM-5 criteria [49], an expert panel will make consensus on how to classify the cases. The neuropsychological test battery in Nor-COAST is based on recommendations from the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network (NINDS-CSN) using the medium, 30 min version [50], including Trail making A and B (TMT A and B) [51], ten word memory and recall test (CERAD) [52] and the controlled oral word association test (COWAT) [53].
Screening of global cognitive function is performed using the Montreal Cognitive Assessment (MoCA) [54]. MoCA evaluates several cognitive domains like memory, visuospatial abilities, executive function, language, abstraction, attention, subtraction, digits forward and backward and orientation and is also validated for telephone interview [55]. Proxy based information on cognition is collected using the Ascertain Dementia 8-item informant questionnaire (AD-8) [56]. The Global Deterioration Scale (GDS) [57] measures global cognition and is scored by the assessor, based on the combination of available information from tests and interviews.
Neuropsyciatric Inventory (NPI-Q) [29] is a 12-item questionnaire assessing occurrence and severity of observed neuropsychiatric symptoms based on self-report or proxy information. Symptoms of anxiety and depression are screened for using Hospital Anxiety and Depression Scale (HADS) [58] for self-reported symptoms. If the participants are not able to respond, proxy information on depression is collected by the Cornell scale [59].
Physical function and activity monitoring
Lower extremity function is measured by Short Physical Performance Battery (SPPB) consisting of three subtasks: 4-m gait speed, balance and chair rise [60]. Additional balance tests include one-leg-stance and 360* turning [61]. Grip strength is measured by using a Jamar handhold dynamometer. The nine-hole peg test is used to measure dexterity [62]. Gait speed at preferred and fast speed, and during dual task-performance (counting backwards) are measured across 10 m with flying start.
Physical activity is measured using a three-axial accelerometer, ActivePAL monitors (PAL Technologies Ltd., Glasgow, United Kingdom), attached to the front of the unaffected thigh during the hospital stay and for a minimum of four days at three and 18 months’ and three years’ follow-up. The inertial sensor produces a signal related to thigh inclination and can thus identify posture (sitting/lying from upright activity) [63]. This method is shown to be valid in the stroke population [64].
Blood samples
Blood samples are analysed during the index stay and at three and 18 months and three years for haemoglobin, low density lipoprotein (LDL), high density lipoprotein (HDL) and total cholesterol, glucose, glycosylated haemoglobin (HbA1c), creatinine, high sensitive CRP and troponin T. In addition, blood has been sampled in BioBank 1, Central-Norway Regional Health Authority, at baseline, three and 18 months and three years for analyses regarding genetics and inflammation. If full blood can not be sampled, saliva is collected in order to make genetic analyses (APOE ε4 carrier status).
Neuroimaging
All patients undergo an acute CT scan to establish the stroke diagnosis and the majority have a brain MRI scan as part of routine diagnostic work-up. In addition, participants are recruited for a study specific MRI brain scan within the first 14 days after stroke. The MRI study protocol consists of 3D-T1, axial T2, 3D-FLAIR, DWI and SWI sequences. A follow-up scan with identical MRI protocol is performed after 18 months and at three years. Protocols were harmonized between centres after scanning of the same healthy volunteer and stroke volunteer in all scanners.
A standardized assessment of the MR findings includes systematically scoring for global atrophy, focal atrophy and vascular disease. For evaluation of white matter hypertensities (WMH) we will use the Fazekas scale [65]. For parietal atrophy we will use the posterior atrophy scale [66]. Lacunes and cortical infarcts will be registered and microbleeds will be assessed using the Bombs scale [67]. Assessment of medial temporal lobe atrophy (MTA) will be done using the Scheltens scale [68]. We will follow the suggested STandards for ReportIng Vascular changes on nEuroimaging (STRIVE) [69]. Quantitative group analysis of the study specific MRI with automated and semi-automated techniques will also be performed.
National registries
Additional information on diagnosis, treatment, and cause of death will be obtained from the Norwegian Stroke Register, the Norwegian cardiovascular disease registry, the Norwegian Prescription Database, the Norwegian Patient Registry and the Norwegian cause of death registry. Administrative permission to access data from registries will be obtained within each workpackage according to the specific research questions.
Statistical analysis
Demographics and participant characteristics will be presented using descriptive statistics. Prevalence and incidence of dementia will be presented by crosstabs. Statistical analyses for trajectories will be performed with group-based trajectory modelling, which uses maximum likelihood to identify groups of individuals with statistically similar trajectories Two primary outputs of the estimations in group-based trajectory modelling are 1) shapes of trajectories of each group as specified by group-specific polynomial functions of time and 2) estimated percentages of the population following each identified trajectory [70]. Both results from visual and volumetric brain analyses will be used to identify MRI predictors of early or delayed of cognitive impairment after stroke. Brain MRI analyses will be combined with machine learning techniques to explore eventual clusters in the study population and to build predictive models. Network analysis with the “NetworkX” software package [71]. is used to discover patient clusters. Predictive models are build with classification algorithms like decision trees with “scikit-learn” [72]. and gradient boosting with “XGBoost” [73]. Linear regression, logistic regression and other statistical methods will be used according to the specific research questions within each work package. A statistician is part of the project managing group and will be involved in developing analysis plans for the main publications and quality insurance of statistical approach in each work package.
Discussion
The current paper describes the protocol of the Nor-COAST study, an ongoing prospective, cohort study following 816 participants for three years after incident stroke. This will be the first study to quantify and report levels of cognitive impairment in a large Norwegian stroke cohort. The study will focus on the diagnosis, incidence and clinical entity of PCI, and provide estimates for the burden of both early and late onset PCI in a general stroke population.
The neuropsychological test battery used in the study is sensitive to the mild cognitive impairments including non-amnestic deficits [74] that are common in the stroke population. This will be among the first studies to use the DSM-5 criteria to diagnose MCI and dementia. In contrast to the ICD-10 criteria, the DSM-5 criteria do not require memory deficit for PCI diagnosis and are consistent with the VASCOG criteria for diagnosing vascular cognitive disorders [75] . Three years’ follow-up will allow study of the mechanisms for late-onset PCI for which there are currently few data.
Using registry data from the Norwegian stroke registry allow us to account for some of the methodological challenges associated with bias, drop-outs and testability in a heterogenic population [76,77,78]. This along with collection of proxy based information and systematic registrations of reason for missing data should be an advantage compared to many earlier studies aiming to describe the overall burden of PCI.
By neuroimaging and identification of genetic, vascular and inflammatory response-factors, we hope to achieve insight of stroke as a trigger for degenerative brain processes and the relevance of pre-existing risk factors, including brain pathologies, for development of PCI. Both results from visual and volumetric brain analyses will be used to identify MRI predictors of early or late onset cognitive impairment. The longitudinal design of Nor-COAST enables us to look for the contribution of vascular and degenerative changes to delayed onset PCI, and to study the characteristics of patients with augmented and prolonged inflammatory response.
We aim to develop a reliable and accurate tool to identify patients at risk of developing PCI based on clinical markers in early phase after stroke. This will provide insight into the relative importance of patient vulnerability in terms of frailty, comorbidity, pre-stroke function and cognition, and the relation between cognitive outcome and stroke and non-stroke factors such as location and severity of stroke, specific treatment and complications including delirium. Further, we aim to explore whether inclusion of biomarkers will increase the predictive value of the score. Identifying stroke survivors at high risk at an early stage would enable early, personalized and appropriate intervention for prevention.
Physical activity will be measured by use of body worn sensors. This will make it possible to monitor physical activity continuously for up to one week at inclusion and at each follow-up, and thereby avoid some of the methodological challenges, such as recall bias and overestimation of activity, associated with the most commonly used self-reported measures [79,80,81,82]. These data will give the opportunity to investigate the underlying mechanisms of the possible preventive effect of physical activity or the negative effects of sedentary behaviour on early and late onset of PCI. Identifying characteristics associated with sedentary behaviour could further help targeting individuals who might benefit from closer follow-up. Gait speed, lower extremity function, balance and dexterity are assessed during the acute stay and at each follow-up and will allow us to explore how different aspects of motor function are associated with and predict PCI. There are studies indicating that screening of motor function early after stroke might help identify individuals at risk of PCI [83], however, larger studies are required.
The concept of adherence, will be assessed by combining information from subjective and objective sources. With supplementary information and evaluation of follow-up routines in primary health care, this sub-study constitutes a valuable approach to a challenging and sparsely studied research area where further data are warranted [84, 85]. Secondary prevention is important for the prognosis following a stroke, both because the risk of PCI is strongly increased by a subsequent stroke, but also because optimal treatment of vascular risk factors seem to impact neurodegeneration and small vessel disease. The Nor-COAST study, collecting crucial data for three years after a stroke, will give unique insight into how PCI influences adherence to preventive measures and achievement of treatment goals and secondly influences the risk of stroke and PCI.
The results of our comprehensive approach, combining assessment of biomarkers and clinical markers along with modifiable factors including physical activity and adherence, holds potential to reveal knowledge that could inform routine clinical practice and be easily applicable in clinical practice. We aim to develop a tool for the early identification of persons at risk and to improve knowledge about modifiable factors such as physical activity and secondary prophylaxis important for prevention, treatment, rehabilitation and overall prognosis. Increased knowledge of adherence to a healthy lifestyle and pharmacological treatments will enable us to give realistic and feasible individualised advice to prevent recurrent stroke and PCI.
Combination of biomarkers and clinical markers allow us to explore the relationship between inflammation and APOE status, chronic inflammation, sedentary behaviour, stroke recurrence and cognition. Brain MRI analyses will be combined with advanced statistical techniques to find combinations of MRI findings and clinical variables associated with the development of PCI. The multidisciplinary approaches applied in the present study unite dementia, geriatrics, stroke and physiotherapy research. This gives us an opportunity to extend existing perspectives for cooperation and to exploring the impact of for example frailty and neurodegeneration on long-term outcome after stroke.
There are some limitations of the Nor-COAST study. Although the neuropsychological test battery contains most of the cognitive domains in the DSM 5, symptoms related to behavior and social cognition are not extensively assessed. Further, some selection bias may have occurred despite the inclusive nature of the study: potential participants may not have been included because of worse health status. Also the recommended neuropsychological battery is cited as taking up to 30 min to perform, but many patients needed longer or testing had to be abandoned. In addition, some assessments, eg the MRI study and parts of the cognitive testing, were not feasible for all participants because of severe illness or specific impairments.
Summary and conclusions
The Nor-COAST study will provide reliable estimates of the burden of PCI in a general Norwegian stroke population. Further, the study will add new and important knowledge on the early detection of individuals at risk for progression of PCI, extend understanding of the underlying pathophysiology and the impact of pre-stroke vulnerability, early physical activity and adherence to secondary prevention on prognosis. The results will contribute to the development of new guidelines for routine clinical practice in stroke and better understanding of mechanisms underlying PCI allowing the development of more specific hypotheses and the design of future intervention studies.
Abbreviations
- 3D-FLAIR:
-
Three-dimensional Fluid-attenuated inversion recovery (FLAIR)
- AD8:
-
Ascertain Dementia 8-item informant questionnaire
- APOE:
-
ε4 Apolipoprotein Eε4
- ATC:
-
Anatomical Therapeutic Chemical (ATC) Classification System
- CAM:
-
The Confusion Assessment Method
- CERAD:
-
Consortium to Establish a Registry for Alzheimer’s Disease
- COWAT:
-
Controlled Oral Word Association Test
- CRF:
-
Standardised case report form
- CRP:
-
C-reactive protein
- CT:
-
Computer Tomography
- DSM-5:
-
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- DWI:
-
Diffusion-weighted magnetic resonance imaging
- EQ5D-5 L:
-
The five level EuroQol five dimension
- FSS-7:
-
Seven Item Fatigue Severity Scale
- GDS:
-
The Global Deterioration Scale
- HADS:
-
Hospital Anxiety and Depression Scale
- HbA1c:
-
Glycosylated haemoglobin
- HDL:
-
High density lipoprotein
- HUNT:
-
Population based health survey in North-Trøndelag
- I-ADL:
-
Instrumental Activities of Daily living
- LDL:
-
Low Density Lipoprotein
- MCI:
-
Mild Cognitive Impairment
- MMAS-4:
-
4-item Morisky Medication Adherence Scale
- MoCA:
-
Montreal Cognitive Assessment
- MRI:
-
Magnetic Resonance Imaging
- mRS:
-
Modified Rankin Scale
- MTA:
-
Medial temporal lobe atrophy
- NIHSS:
-
National Institutes of Health Stroke Scale
- NINDS-CSN:
-
The National Institute for Neurological Disorders and Stroke and Canadian Stroke Network
- Nor-COAST:
-
Norwegian Cognitive impairment After STroke study
- NPI-Q:
-
Neuropsyciatric Inventory
- OSCP:
-
Oxfordshire Stroke Classification Project
- PCI:
-
Poststroke cognitive impairment
- SPPB:
-
Short Physical Performance Battery
- STRIVE:
-
STandards for ReportIng Vascular changes on Euroimaging
- SWI:
-
Susceptibility weighted imaging
- TMT A and B:
-
Trail making A and B
- TOAST:
-
The Trial of Org 10,172 in Acute Stroke Treatment
- WMH:
-
White Matter Hypertensities
- WP:
-
Work Package
References
Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, et al. The lifetime risk of stroke: estimates from the Framingham study. Stroke. 2006;37(2):345–50.
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42(9):2672–713.
Leys D, Henon H, Mackowiak-Cordoliani MA, Pasquier F. Poststroke dementia. Lancet Neurol. 2005;4(11):752–9.
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223.
Pollock A, St George B, Fenton M, Firkins L. Top ten research priorities relating to life after stroke. Lancet Neurol. 2012;11(3):209.
Pendlebury ST. Stroke-related dementia: rates, risk factors and implications for future research. Maturitas. 2009;64(3):165–71.
Brainin M, Tuomilehto J, Heiss WD, Bornstein NM, Bath PM, Teuschl Y, et al. Post-stroke cognitive decline: an update and perspectives for clinical research. Eur J Neurol. 2015;22(2):229–38 e13-6.
Pendlebury ST, Mariz J, Bull L, Mehta Z, Rothwell PM. Impact of different operational definitions on mild cognitive impairment rate and MMSE and MoCA performance in transient ischaemic attack and stroke. Cerebrovasc Dis. 2013;36(5–6):355–62.
Pendlebury ST. Dementia in patients hospitalized with stroke: rates, time course, and clinico-pathologic factors. Int J Stroke. 2012;7(7):570–81.
Ihle-Hansen H, Thommessen B, Wyller TB, Engedal K, Oksengard AR, Stenset V, et al. Incidence and subtypes of MCI and dementia 1 year after first-ever stroke in patients without pre-existing cognitive impairment. Dement Geriatr Cogn Disord. 2011;32(6):401–7.
Sachdev PS, Chen X, Brodaty H, Thompson C, Altendorf A, Wen W. The determinants and longitudinal course of post-stroke mild cognitive impairment. J Int Neuropsychol Soc. 2009;15(6):915–23.
Liman TG, Heuschmann PU, Endres M, Floel A, Schwab S, Kolominsky-Rabas PL. Changes in cognitive function over 3 years after first-ever stroke and predictors of cognitive impairment and long-term cognitive stability: the Erlangen stroke project. Dement Geriatr Cogn Disord. 2011;31(4):291–9.
Altieri M, Di Piero V, Pasquini M, Gasparini M, Vanacore N, Vicenzini E, et al. Delayed poststroke dementia: a 4-year follow-up study. Neurology. 2004;62(12):2193–7.
Mok VC, Lam BY, Wong A, Ko H, Markus HS, Wong LK. Early-onset and delayed-onset poststroke dementia - revisiting the mechanisms. Nat Rev Neurol. 2017;13(3):148–59.
Jin YP, Di Legge S, Ostbye T, Feightner JW, Hachinski V. The reciprocal risks of stroke and cognitive impairment in an elderly population. Alzheimers Dement. 2006;2(3):171–8.
Rostamian S, Mahinrad S, Stijnen T, Sabayan B, de Craen AJ. Cognitive impairment and risk of stroke: a systematic review and meta-analysis of prospective cohort studies. Stroke. 2014;45(5):1342–8.
Appelros P, Nydevik I, Seiger A, Terent A. Predictors of severe stroke: influence of preexisting dementia and cardiac disorders. Stroke. 2002;33(10):2357–62.
Love S, Miners JS. Small vessel disease, neurovascular regulation and cognitive impairment: post-mortem studies reveal a complex relationship, still poorly understood. Clin Sci (Lond). 2017;131(14):1579–89.
Kamel H, Iadecola C. Brain-immune interactions and ischemic stroke: clinical implications. Arch Neurol. 2012;69(5):576–81.
Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12(3):204–12.
Lee YJ, Han SB, Nam SY, Oh KW, Hong JT. Inflammation and Alzheimer's disease. Arch Pharm Res. 2010;33(10):1539–56.
Wagle J, Farner L, Flekkoy K, Wyller TB, Sandvik L, Eiklid KL, et al. Cognitive impairment and the role of the ApoE epsilon4-allele after stroke--a 13 months follow-up study. Int J Geriatr Psychiatry. 2010;25(8):833–42.
Thiel A, Cechetto DF, Heiss WD, Hachinski V, Whitehead SN. Amyloid burden, neuroinflammation, and links to cognitive decline after ischemic stroke. Stroke. 2014;45(9):2825–9.
Thompson CS, Hakim AM. Living beyond our physiological means: small vessel disease of the brain is an expression of a systemic failure in arteriolar function: a unifying hypothesis. Stroke. 2009;40(5):e322–30.
Rothwell PM, Giles MF, Chandratheva A, Marquardt L, Geraghty O, Redgrave JN, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007;370(9596):1432–42.
Ngandu T, Lehtisalo J, Solomon A, Levalahti E, Ahtiluoto S, Antikainen R, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–63.
Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42(1):227–76.
Hankey GJ. Secondary stroke prevention. Lancet Neurol. 2014;13(2):178–94.
Cumming TB, Tyedin K, Churilov L, Morris ME, Bernhardt J. The effect of physical activity on cognitive function after stroke: a systematic review. Int Psychogeriatr. 2012;24(4):557–67.
Liu-Ambrose T, Eng JJ. Exercise training and recreational activities to promote executive functions in chronic stroke: a proof-of-concept study. J Stroke Cerebrovasc Dis. 2015;24(1):130–7.
Oberlin LE, Waiwood AM, Cumming TB, Marsland AL, Bernhardt J, Erickson KI. Effects of physical activity on Poststroke cognitive function: a meta-analysis of randomized controlled trials. Stroke. 2017;48(11):3093–100.
Nicklas BJ, Brinkley TE. Exercise training as a treatment for chronic inflammation in the elderly. Exerc Sport Sci Rev. 2009;37(4):165–70.
Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2008;2:CD005381.
Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci U S A. 2011;108(7):3017–22.
Janssen H, Dunstan DW, Bernhardt J, Walker FR, Patterson A, Callister R, et al. Breaking up sitting time after stroke (BUST-stroke). Int J Stroke. 2017;12(4):425–9.
European Stroke Organisation (ESO) Executive Committee; ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008;25(5):457–507.
Indredavik B SR, Næss H, Thorsvik D. Treatment and rehabilitation after stroke (Clinical guidelines). Norwegian Directorate of Health. https://helsedirektoratetno/retningslinjer/nasjonal-faglig-retningslinje-for-behandling-og-rehabilitering-ved-hjerneslag. Accessed 27 Oct 2017.
Askim T, Langhammer B, Ihle-Hansen H, Gunnes M, Lydersen S, Indredavik B, Group LC. Efficacy and safety of individualized coaching after stroke: the LAST study (life after stroke): a pragmatic randomized controlled trial. Stroke. 2018;49(2):426–32.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–8.
Gladman JR, Lincoln NB, Adams SA. Use of the extended ADL scale with stroke patients. Age Ageing. 1993;22(6):419–24.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–5.
Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol group. Ann Med. 2001;33(5):337–43.
Lerdal A, Kottorp A. Psychometric properties of the fatigue severity scale-Rasch analyses of individual responses in a Norwegian stroke cohort. Int J Nurs Stud. 2011;48(10):1258–65.
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337(8756):1521–6.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, et al. National Institute of Neurological Disorders and Stroke-Canadian stroke network vascular cognitive impairment harmonization standards. Stroke. 2006;37(9):2220–41.
RM. R. Validity of the trail making test as an indicator of organic brain damage. Percept Mot Skills. 1958;8:271–6.
Morris JC, Mohs RC, Rogers H, Fillenbaum G, Heyman A. Consortium to establish a registry for Alzheimer's disease (CERAD) clinical and neuropsychological assessment of Alzheimer's disease. Psychopharmacol Bull. 1988;24(4):641–52.
Loonstra AS, Tarlow AR, Sellers AH. COWAT metanorms across age, education, and gender. Appl Neuropsychol. 2001;8(3):161–6.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Pendlebury ST, Welch SJ, Cuthbertson FC, Mariz J, Mehta Z, Rothwell PM. Telephone assessment of cognition after transient ischemic attack and stroke: modified telephone interview of cognitive status and telephone Montreal cognitive assessment versus face-to-face Montreal cognitive assessment and neuropsychological battery. Stroke. 2013;44(1):227–9.
Galvin JE, Roe CM, Powlishta KK, Coats MA, Muich SJ, Grant E, et al. The AD8: a brief informant interview to detect dementia. Neurology. 2005;65(4):559–64.
Reisberg B, Ferris SH, de Leon MJ, Crook T. The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–9.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell scale for depression in dementia. Biol Psychiatry. 1988;23(3):271–84.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94.
Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl 2):S7–11.
Heller A, Wade DT, Wood VA, Sunderland A, Hewer RL, Ward E. Arm function after stroke: measurement and recovery over the first three months. J Neurol Neurosurg Psychiatry. 1987;50(6):714–9.
Grant PM, Ryan CG, Tigbe WW, Granat MH. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. 2006;40(12):992–7.
Taraldsen K, Askim T, Sletvold O, Einarsen EK, Bjastad KG, Indredavik B, et al. Evaluation of a body-worn sensor system to measure physical activity in older people with impaired function. Phys Ther. 2011;91(2):277–85.
Wahlund LO, Barkhof F, Fazekas F, Bronge L, Augustin M, Sjogren M, et al. A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke. 2001;32(6):1318–22.
Koedam EL, Lehmann M, van der Flier WM, Scheltens P, Pijnenburg YA, Fox N, et al. Visual assessment of posterior atrophy development of a MRI rating scale. Eur Radiol. 2011;21(12):2618–25.
Cordonnier C, Potter GM, Jackson CA, Doubal F, Keir S, Sudlow CL, et al. Improving interrater agreement about brain microbleeds: development of the brain observer MicroBleed scale (BOMBS). Stroke. 2009;40(1):94–9.
Scheltens P, Leys D, Barkhof F, Huglo D, Weinstein HC, Vermersch P, et al. Atrophy of medial temporal lobes on MRI in "probable" Alzheimer's disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol Neurosurg Psychiatry. 1992;55(10):967–72.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12(8):822–38.
Nagin DS. Group-based trajectory modeling: an overview. Ann Nutr Metab. 2014;65(2–3):205–10.
Hagberg AA, Schult DA, Swart PJ. Exploring network structure, dynamics, and function using NetworkX. In: Varoquaux G, Vaught T, Millman J, editors. Proceedings of the 7th Python in Science Conference; 2008. p. 11–5.
Pedregosa F, et al. Scikit-learn: Machine Learning in Python. JMLR. 2011;12:2825–30.
Chen T, Guestrin C. XGBoost: A scalable tree boosting system. In proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining (KDD '16). New York: ACM; 2016. p. 785–94.
Chiti G, Pantoni L. Use of Montreal cognitive assessment in patients with stroke. Stroke. 2014;45(10):3135–40.
Sachdev P, Kalaria R, O'Brien J, Skoog I, Alladi S, Black SE, et al. Diagnostic criteria for vascular cognitive disorders: a VASCOG statement. Alzheimer Dis Assoc Disord. 2014;28(3):206–18.
Pendlebury ST, Chen PJ, Bull L, Silver L, Mehta Z, Rothwell PM, et al. Methodological factors in determining rates of dementia in transient ischemic attack and stroke: (I) impact of baseline selection bias. Stroke. 2015;46(3):641–6.
Pendlebury ST, Chen PJ, Welch SJ, Cuthbertson FC, Wharton RM, Mehta Z, et al. Methodological factors in determining risk of dementia after transient ischemic attack and stroke: (II) effect of attrition on follow-up. Stroke. 2015;46(6):1494–500.
Pendlebury ST, Klaus SP, Thomson RJ, Mehta Z, Wharton RM, Rothwell PM, et al. Methodological factors in determining risk of dementia after transient ischemic attack and stroke: (III) applicability of cognitive tests. Stroke. 2015;46(11):3067–73.
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8.
Bernhardt J, Dewey H, Thrift A, Donnan G. Inactive and alone: physical activity within the first 14 days of acute stroke unit care. Stroke. 2004;35(4):1005–9.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Rand D, Eng JJ, Tang PF, Jeng JS, Hung C. How active are people with stroke?: use of accelerometers to assess physical activity. Stroke. 2009;40(1):163–8.
Ursin MH, Bergland A, Fure B, Torstad A, Tveit A, Ihle-Hansen H. Balance and mobility as predictors of post-stroke cognitive impairment. Dement Geriatr Cogn Dis Extra. 2015;5(2):203–11.
Ullberg T, Zia E, Petersson J, Norrving B. Doctor’s follow-up after stroke in the south of Sweden: an observational study from the Swedish stroke register (Riksstroke). Eur Stroke J. 2016;1(2):114–21.
Ullberg T, Glader EL, Zia E, Petersson J, Eriksson M, Norrving B. Associations between ischemic stroke follow-up, socioeconomic status, and adherence to secondary preventive drugs in southern Sweden: observations from the Swedish stroke register (Riksstroke). Neuroepidemiology. 2017;48(1–2):32–8.
Acknowledgements
The Nor-COAST collaboration group: Askim T., Aam S., Aaslund M.K., Aamodt E., Beyer M.K., Ellekjær H., Einstad M.S., Fure B., Gynnild M.A., Hamre C., Ihle-Hansen H., Knapskog A.B., Kummeneje C.S., Munthe-Kaas R., Næss H., Pendlebury S.T., Saltvedt I., Schellhorn T., Seljeseth Y., Thingstad P., Ursin M.
Funding
The Nor-COAST study is funded by the Norwegian Health Association.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
All authors have been involved in the planning and design of the study. TA, GB, HIH, RMK, MKB, ABK, HN, HE, YS, and IS as members of the steering committee and/or responsible at each study site. STP as external advisor/collaborator. SL has been involved in planning and writing of statistical analyses. PT, IS, and TA have been the major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Authors’ information
The Nor-COAST study is a collaboration between the Norwegian Health Authorities, five hospitals and Universities in Norway represented through a steering committee with project leadership at Department of Neuromedicine and Movement Science, NTNU, Trondheim. Participating partners are 1. Central Norway Regional Health Authority: a) St. Olav University Hospital, b) Ålesund Hospital, Møre and Romsdal Health Trust, 2. South-Eastern Norway Regional Health Authority: a) Vestre Viken Hospital Trust, Bærum Hospital b) Department of Radiology and Nuclear Medicine Oslo University Hospital c) Department of Geriatrics, Oslo University Hospital: 3. Western Norway Regional Health Authority: Haukeland University Hospital.
Ethics approval and consent to participate
The research is performed according to the Helsinki declaration. Participation is based on informed written consent. For participants who were unable to provide informed consent due to medical condition or severe dementia, participation was based on proxy consent given by family proxies. The study protocol has been approved by the regional committees for medical and health research, REK Nord (REK number: 2015/171).
Consent for publication
Not applicable
Competing interests
Hege Ihle Hansen is associate Editor in BMC Neurology.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Thingstad, P., Askim, T., Beyer, M.K. et al. The Norwegian Cognitive impairment after stroke study (Nor-COAST): study protocol of a multicentre, prospective cohort study. BMC Neurol 18, 193 (2018). https://doi.org/10.1186/s12883-018-1198-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-018-1198-x