Abstract
Background
Migraine is a prevalent and disabling headache disorder that affects more than 1.04 billion individuals world-wide. It can result in reduction in quality of life, increased disability, and high socio-economic burden. Nevertheless, and despite the availability of evidence-based national and international guidelines, the management of migraine patients often remains suboptimal, especially for chronic migraine (CM) patients.
Methods
My-LIFE anamnesis project surveyed 201 General practitioners (GPs) from 5 European countries (France, Germany, Italy, Spain, and the UK) with the aim of understanding chronic migraine (CM) patients’ management in the primary care setting.
Results
In our survey, GPs diagnosed episodic migraine (EM) more often than CM (87% vs 61%, p < 0.001). We found that many CM patients were not properly managed or referred to specialists, in contrast to guidelines recommendations. The main tools used by primary-care physicians included clinical interview, anamnesis guide, and patient diary. Tools used at the first visit differed from those used at follow-up visits. Up to 82% of GPs reported being responsible for management of patients diagnosed with disabling or CM and did not refer them to a specialist. Even when the GP had reported referring CM patients to a specialist, 97% of them were responsible for their follow-up. Moreover, the treatment prescribed, both acute and preventive, was not in accordance with local and international recommendations. GPs reported that they evaluated the efficacy of the treatment prescribed mainly through patient perception, and the frequency of follow-up visits was not clearly established in the primary care setting. These results suggest that CM is underdiagnosed and undertreated; thereby its management is suboptimal in the primary care.
Conclusions
There is a need of guidance in the primary care setting to both leverage the management of CM patients and earlier referral to specialists, when appropriate.
Similar content being viewed by others
Background
Headache disorders are a notable public health concern and a significant cause of disability worldwide. Among headache disorders, migraine is the main cause of recurrent headache (> 90%) [1], affecting 80.8 million individuals in Western Europe, and more than 1.04 billion world-wide [2]. Migraine impacts personal life but also has significant socio-economic and public health-related implications [3]. The Global Burden of Diseases, Injuries, and Risk Factors (GBD) study reported that migraine was responsible for 5.6% of all years lived with disability (YLDs) in the world, and for 6.2% of YLDs in Western Europe, and consider it to be the leading cause of disability in people 15–49 years old, accounting for 8.2% of YLDs worldwide [4, 5]. Between 2.5–3.1% of people with episodic migraine (EM) develop chronic migraine (CM) within one year [6,7,8], which is defined by headache on ≥15 days per month for ≥3 months, of which at least 8 days/month have migraine headache features [9, 10]. CM is associated with substantially greater reduction in quality of life and increased disability compared to EM, resulting in even greater personal and socio-economic burden [11,12,13].
Despite being highly prevalent and having significant personal and social impact, migraine may not receive appropriate attention, probably because it is not a life-threatening disease and may result in invisible disability and is common among the population. As a result, migraine and particularly CM, is largely underdiagnosed and undertreated worldwide [14, 15].
Migraine is a clinical diagnosis with primarily subjective manifestations and there are no diagnostic tests either for this condition or any of the primary headache disorders, nor for secondary headache disorders such as medication overuse headache (MOH). Thus, medical history and anamnesis are crucial for proper diagnosis [16]. Together with the medical history, the anamnesis done by asking specific questions to the patient will provide the physician with useful information to formulate the diagnosis. According to the International Classification of Headache Disorders (ICHD) and European Headache Federation (EHF), EM can be managed in primary care, but CM requires specialist referral because diagnosis and, particularly, management can be difficult [9, 17]. Nevertheless, in the Eurolight study carried out in 10 European countries, 33.8% of patients reported frequent migraine (> 5 days/month), of which < 18% had seen a GP, and < 15% had visited a neurologist [15]. Moreover, although 1/3 of patients reported frequent migraine and, therefore, need of preventive medication, < 11% of patients were receiving adequate acute treatment, and even a lower proportion (< 6.4%) were receiving preventive medication [15]. An observational study on the use of antimigraine treatments by French GPs identified that acute headache treatment is prescribed according to national practice guidelines and is considered as effective and satisfactory. In contrast, it showed that the use of preventive medication is low [18].
Considering the low proportion of people consulting GP and migraine specialists, and the mishandling reported of the acute and preventive treatments, it is crucial to better understand management of CM patients in the primary care setting. Thus, the aim of the My-LIFE anamnesis project was to describe the real current clinical practice regarding disabling and CM identification, treatment, and referral in the primary care setting in 5 European countries (France, Germany, Italy, Spain, and the UK).
Methods
My-LIFE anamnesis project was designed as a survey to GPs from 5 European countries: France, Germany, Italy, Spain, and the UK using a structured online questionnaire.
The project involved two sets of participants: members of the Steering Committee (SC), and survey participants. The Pan-European SC included 7 members, well known clinical experts in migraine from Germany, Italy, Norway, Russia, Spain, Switzerland, and the UK. Their roles included performing literature reviews, defining the key objectives and the main content of the online questionnaire, and data interpretation.
For the survey, GPs from 5 European countries (France, Germany, Italy, Spain, and the UK) were invited to participate. In order to secure that participants had some background in the diagnosis and management of headache disorders the following selection criteria were defined: i) with at least 2 years of experience in general practice; ii) who were seeing at least 5 patients suffering from headache disorders per week; iii) usually proceeded with the medical history of their patients with headache disorders; iv) had currently at least 1 patient suffering from episodic and/or CM.
Ethics Committee approval was not applicable in this survey because its objective was to understand chronic migraine patients’ management in the primary care setting. There was no need to collect any type of patient data or information, hence the approval of an Ethics Committee or patient informed consent was not required. All survey participants gave their written consent.
Questionnaire
Development of the questionnaire was based on a literature search and on the clinical experience of the SC members. The 32-item questionnaire was divided in three main sections: Participants’ profile; Current clinical practice in disabling or CM identification and treatment; and Definition of a Migraine Anamnesis Guide (Additional file 1). The questionnaire was written in English and translated into local languages (French, German, Italian, and Spanish). It was administered to 201 GPs fulfilling the inclusion criteria between 14th January 2020 and 28th January 2020 through an online platform that ensured data anonymity and confidentiality as well as that all questions were answered in order to avoid any missing value.
Statistical analysis
Categorical variables were expressed in terms of means and standard deviations (SD) or range, or number and percentage of responses. Comparative analysis among countries was carried out with Chi-square test or ANOVA test for categorical and continuous variables, respectively. Data analysis was performed with the SPSS version 22, and p < 0.05 was considered to be statistically significant.
Results
Participants’ profile
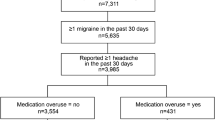
In the My-LIFE anamnesis project, 201 GPs from 5 European countries were included: 41 GPs from France, and 40 GPs each from Germany, Italy, Spain, and the United Kingdom. GPs had 24 (range 2–42) years of experience and each saw 202 patients per week, on average. Twelve percent of patients presented with headache disorders, and migraine was diagnosed in 38% of them. Among migraine patients, 66% presented with EM, and 34% with CM (Additional file 2).
Headache diagnosis
When the participants were asked about who did the diagnosis of EM or CM of their patients, the proportion of diagnosis ascertained by GP versus specialist significantly differed between EM (87% GP vs 13% specialist) and CM (61% GP vs 39% specialist) (p < 0.001). For EM diagnosis, no differences between countries were found; however, for CM significant differences (p = 0.015) were observed, ranging from 81% in France to 45% in Italy (Table 1).
Headache disorders to be managed at primary care include tension-type headache (TTH), MOH and migraine [9], and GPs were asked about the differential diagnosis of these conditions. During the anamnesis of a patient with a headache disorder, 61% of participants always considered TTH, and 57% always ruled out MOH, but significant differences were observed among countries: 80% of UK GPs and 78% of Spanish GPs always ruled out TTH vs. 38% of Italian GPs. Consideration of MOH varied from 85% in the UK to 30% in Italy (p < 0.001, for both comparisons) (Table 1).
There are several instruments available to aid primary-care physicians in both migraine diagnosis and management. In our survey, the tools used to assess patients with disabling and CM at the first visit differed from those used in the follow-up visits. At the first visit, all participants (100%) conducted a clinical interview (vs. 51% at follow-up visits, p < 0.001), and 46% of them used an anamnesis guide (a guide to support the physician during the diagnosis) to diagnose CM (vs. 26% at follow-up visits, p < 0.001). In contrast, patient diaries were more often used at follow-up visits (69% vs. 36% at the first visit, p < 0.001), and also imaging techniques (50% vs. 21% at the first visit, p < 0.001).
Validated scales to assess the impact of migraine and validated migraine screening tools were used by less than 35% of the participants at both the first and follow-up visits (Fig. 1a).
Tools used to assess patients with disabling or chronic migraine. a. Tools used at the first visit vs. tools used at the follow up visit (total). At the first visit,” others” included review of the medication and clinical examination including blood pressure; physical examination, and blood test. At the follow-up visit, “others” included physical examination, blood test, pain using a VAS, and patient information leaflets. *p < 0.05. b. Tools used at the first visit, by country. *p < 0.05
When considering the tools used by country in the first visit, significant differences were observed in patient diary use (p = 0.025), imaging techniques (p = 0.021), and validated scales to assess the impact of migraine (p = 0.006) (Fig. 1b).
Anamnesis guide characteristics
Sixty-four percent of participants reported using an anamnesis guide to diagnose CM at any time. The guides used were heterogeneous, either developed by themselves (41%) or by the centre where the GP worked (15%), or validated and published guides (44%). Spain and Italy had the highest percentage of GPs using a validated and published anamnesis guide (54 and 52%, respectively) (p = 0.012) (Table 2).
Inclusion of red flags i.e., signs or symptoms that can guide successive investigations and/or referral and decision-making, is common in primary care management of migraine. On average, 60% of the anamnesis guides used by GPs included red flags/warning features. Up to 93% of the anamnesis guides used in the UK and 89% in Spain included red flags vs. 19% in Italy (p < 0.001) (Table 2). There was no statistical difference between the anamnesis guide type used and the inclusion of red flags.
The main topics addressed during the anamnesis included frequency of attacks; medication use, frequency and effectiveness; and pain characteristics of the attacks, among others. These topics were independent of the anamnesis guide type used, and they were also independent of whether or not an anamnesis guide was used. However, when an anamnesis guide was not used, there was a trend to ask fewer questions and more differences between countries were found regarding the topics asked.
Patient diary characteristics
Overall, 85% of participant GPs asked the patient to complete a patient diary, headache diary or calendar at any time. Most of the participants (62%) recommended recording some items on a notebook used as a patient diary instead of using a formal headache diary or calendar, and 38% recommended either a standard diary or a validated/published tool, without differences among countries. The main items requested to be recorded were frequency (96%) and duration (91%) of the attack, followed by medication taken and intensity of the headache (Fig. 2). It is noteworthy that, when using a validated/standard patient diary, information was more consistent and comprehensive, and more items were recorded, with statistically significant differences regarding the headache characteristics (p = 0.005) and intensity (p = 0.001).
Other diagnostic tools
Up to 50% of GPs used imaging techniques at follow-up visits to assess patients with disabling or CM (Fig. 1a). In this context, 58% of GPs stated that imaging techniques were mainly used to rule out secondary headache disorders. Besides, around 48% of the participants used validated scales to assess patients with migraine at any time. Among these, ID-Migraine was the most used in the first visit (63% of participants, p < 0.001) (Fig. 3a), while ID-Chronic migraine (ID-CM) (32%) and Headache Under-Response to Treatment (HURT) scales (31%, p = 0.003) were the most used validated scales in the follow-up visit. The ID-CM scale was employed by up to 59% of Italian GPs at the first visit (p = 0.013) (Fig. 3b).
Validated scales used as diagnostic tools in patients with disabling or chronic migraine. a Validated scales used in the first visit vs. follow-up visit (total). *p < 0.050. b. Validated scales used by country in the first visit. *p < 0.050. †Other scales used with the patients with disabling or chronic migraine include KIEL HD questionnaire, Migraine Specific Quality of Life, and QVM score (Qualité de Vie et Migraine). HALT, Headache-Attributed Lost Time index. HIT-6, Headache Impact Test. HURT, Headache Under-Response to Treatment Questionnaire. MAT, Migraine Assessment Tool. MIDAS, Migraine Disability Assessment Score
Chronic migraine management by GPs
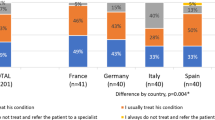
Overall, 82% of GPs reported that they usually managed patients diagnosed with disabling or CM themselves, without referral to a migraine specialist. Among these GPs, 82% reported prescription of acute medication and 72% of migraine preventive treatment when needed, with significant differences among countries for both acute (p < 0.001) and preventive treatment (p = 0.003). Up to 94% in Germany and 95% in France prescribed acute medication, and in the UK, 94% of the patients were prescribed preventive treatment (Fig. 4). There were no differences between countries, either in the percentage of patients prescribed acute medication prescribed or the percentage of patients prescribed preventive treatment.
Besides, GPs who reported that they were in charge of the treatment of CM patients considered that main reasons for referring patients include diagnostic uncertainty, lack of response to preventive or acute treatment, and or highly disabling migraine. Some differences were observed between countries: diagnostic uncertainty (p = 0.036), highly disabling migraine (p = 0.013), lack of response to preventive (p = 0.008) or acute treatment (p = 0.003).
Chronic migraine patients’ referral and follow-up
Eighteen percent of the GPs reported that they “usually referred patients diagnosed with disabling or CM to a migraine specialist”. Among them, 76% mentioned that the main reason for referral was diagnostic confirmation (Fig. 5). In all countries 80–100% of GPs mentioned diagnostic confirmation as the main reason for referral, with the exception of only 29% in Spain (p = 0.022). In Germany, 83% of the participants referred their patients to give them access to a preventive treatment (p = 0.038); whereas preventive treatment access was not a strong reason for referral in Italy (19%) or in the UK (17%) (Fig. 5).
Even when the GP reported referring CM patients to a specialist for treatment prescription, up to 97% of GPs were in charge of ongoing management of most patients. The evaluation of the efficacy of the treatment prescribed by the specialists was mainly done through the patient perception (72%). Although non-significant, Spain was the only country where the ongoing evaluation was mainly done through a patient diary (86%). Moreover, the frequency of the treatment efficacy evaluation was not clearly established in the primary care setting, since yearly, semester, quarterly, monthly basis, and as needed evaluation were performed equally. To note, all French participants reported weekly evaluation of treatment efficacy (Table 3).
In contrast, among GPs that usually treated CM patients themselves, the main indicators to evaluate the efficacy of acute and preventive treatments was the patient perception of the treatment (75%), and the frequency of the migraine attacks. On average, efficacy of the prescribed acute treatment was evaluated on a monthly basis by 50% of the participants. Of note, 10% of GPs evaluated the efficacy when the patient came back with complaints, without significant differences between countries (Table 3). The efficacy of the prescribed preventive treatment was evaluated on a monthly or quarterly basis by 81% of GPs on average. In the UK, Germany and Spain, 15–17% of GPs evaluated treatment efficacy when the patient came back complaining, while no GP reported this in Italy and France. In France up to 22% of GPs evaluated treatment efficacy on a weekly basis (p = 0.002) (Table 3). A small percentage of the participants used validated scales to evaluate the efficacy of treatment (acute or preventive) (Table 3); however, when the patient was referred and the GP was only in charge of follow up, GPs did not use validated scales.
Discussion
The outcomes of this project provide data on the diagnosis and management of CM from 201 randomly selected GPs from 5 European countries, that could reflect what is currently being done in the primary setting with regards to HD disorders management. The main results from this survey suggest that many patients are underdiagnosed and undertreated. Most patients are not referred to specialists, and treatments prescribed, both acute and preventive, are not in accordance with local and international recommendations being the management of CM patients clearly suboptimal.
CM affects approximately 2% of the world population [19] and up to 4% of the European individuals [20]. Despite being an uncommon headache disorders, entails significant burden and should be recognized in primary care [9, 10], and this study indicates the need of increased awareness of CM. In the present survey, we found that 61% of CM diagnosis was made by GPs. Considering that diagnosis of migraine and CM is made solely through a proper anamnesis, the percentage of GPs that proceeded with a clinical interview in the follow-up visit (51%) is low. This may be explained by the limited time that can be dedicated to the patients in the primary care setting. According to guidelines [9], migraine diagnosis should include differential diagnosis of MOH and TTH, but only 61% of participants always ruled out TTH and 57% MOH. MOH requires an underlying primary headache disorder (most commonly migraine) and up to 2/3 of CM patients present with MOH [21]. The presence of MOH may complicate CM diagnosis, and even if MOH is concomitant with CM, it must be recognized and managed independently [9, 10, 17].
Proper management of migraine and other headache disorders requires continued monitoring of symptoms over time. For symptom monitoring in primary care, patient diaries are recommended because they can help to monitor headache intensity and frequency of symptoms [9, 10]. A positive finding from our survey was that almost 70% of participants reported the use of diaries in the follow-up visits.
In the follow-up visits imaging techniques were reported to be used by 50% of participants suggesting that CM patients are being submitted to imaging techniques too often, increasing the cost of CM patients management of the health care systems; however, current guidelines state that patients with headache and a normal neurological examination have the same the risk as the normal population of serious secondary pathology findings in neuroimaging [17, 22, 23]. Neuroimaging is not indicated unless the history or examination suggests headache may be secondary to another condition [9]; therefore, diagnostic uncertainty increases the use of unnecessary investigations, in agreement with previous studies [1, 24]. In addition, these results also confirm that CM is associated with a greater use of healthcare resources in the primary care setting [17].
Forty-six percent of participants used an anamnesis guide to diagnose CM. Whether a guide is used or not, awareness of specific warning features in the patient history to guide diagnosis and management is recommended [9, 10]. Besides, the inclusion of red flags in the anamnesis guide was independent of the type of guide; however, more than 85% of the anamnesis guides used by Spanish and UK GPs included these red flags. The proper use of red flags would help to identify those patients where imaging is really needed, but these results do not seem to be related with a decrease in the use of imaging techniques to rule out secondary headache disorders. Current guidelines suggest specific warning features/red flags that should be detected in the medical history for differential diagnosis of the headache disorders relevant to primary care [9]. Recently, Phu Do et al. developed the systematic SNNOOP10, a list of red and orange flags useful for detecting secondary headache disorders in clinical practice [24].
Effective management of migraine needs to consider the impact on the patient’s life and lifestyle to establish the best treatment. In primary care, up to 18 scales are used to classify or screen for migraine [25]. Although most of the tools are quick, easy-to-use, self-completed screening questionnaires, their use is not widely widespread. In this line, we observed that fewer than 50% of the participants used a validated scale as a screening tool or during the follow-up. Considering how disabling migraine is, it would be of high interest to enhance relevant outcomes measurement in clinical routine in these patients.
The most widely used tool at the first visit was ID-Migraine (63% of participants). This scale has been validated in different languages and settings and is common among GPs [25,26,27,28]. Interestingly, 59% of participants from Italy were using the ID-CM at the first visit, which perhaps could be explained by the recent translation and validation of this scale into Italian [29]. The ID-CM scale is a self-administered tool to help identify individuals with CM [14]; however, it does not identify other chronic headache disorders since it does not include either warning features to identify secondary headache disorders, or referral recommendations.
The most used scales by GPs during follow-up included ID-CM, MIDAS, and HURT. Despite not being experts in migraine, the percentage of GPs using the MIDAS or the HURT scales suggests that the GPs in this survey had experience in migraine management, as these scales are not so widespread among GPs.
The anamnesis relies mostly on patient perception of attack frequency and the evaluation of treatment efficacy, both acute and preventive, reinforcing the importance of patients reported outcomes for migraine management in the real-life setting [30, 31].
Considering that the prescription of some preventive treatments (onabotulinum toxin A and CGRP antibodies) for disabling and CM patients is restricted to migraine specialists in most European countries, the low referral rate reported would support the fact that the majority of CM patients seem not to receive adequate preventive treatment. The low use of preventive medication among migraine patients has been previously reported [15, 18]. In Germany, 83% of participants stated that the main reason for referring their patients to a specialist is to give them access to a preventive treatment. Moreover, preventive treatment would also reduce the risk of MOH development in CM patients [17]. Nowadays, a range of effective and well tolerated preventive drugs for CM exists. Patient access to preventive drugs remains a challenge in Europe and it is important that all healthcare professionals managing CM are well informed about all treatment options and the specific prescription conditions in their country.
European and local current guidelines recommend referral of patients with CM from primary care to specialist care because diagnosis and management can be difficult [9, 17, 32]. The low referral rate reported by the GPs could also be explained by a long wait for patients to see a specialist, thus giving more pressure on the primary care setting and increasing the visit to the emergency departments. The assessment of headache disorders patients in the emergency department setting differs from the assessment in primary care. A recent retrospective study analysed migraine management in the emergency room (ER) to identify deficiencies that could be solved by a rapid referral to a headache centre. The concordance analysis between ER diagnosis and tertiary level headache centre diagnosis showed a significant moderate agreement for the diagnosis of migraine between triage and headache centre. Most patients attending ER complaining of headache received the same treatment independently of their diagnosis; thus, rapid referral to a headache centre is key to provide a definite diagnosis and appropriate treatment [33]. In this line, the Spanish Society of Neurology’s Headache Study Group (GECSEN) has issued a series of recommendations constituting a referral protocol to guide decision-making in patients with headache. This protocol for action and referral from ER and primary care is aimed to improve diagnosis and treatment in patients with headache (both primary and secondary) and/or craniofacial neuralgia [34, 35].
Despite the GP participants having knowledge and experience of migraine management, the results from this survey clearly show that CM patients are undertreated. Considering that this group of GP’s sees on average 40 patients a day, it would be very challenging to provide specialist management of CM patients giving an additional explanation to the undertreatment of these patients. All this suggesting that in a less experienced primary care setting, the under-treatment of CM patients could be more extensive. The Vancouver Declaration on Global Headache Patient Advocacy agreed on the need of adequate training in Headache Medicine of all HCP and that all patients affected by headache disorders should have reliable access to competent medical care [36].
Finally, it should be noted that some country differences may also be explained by differences in the local healthcare system, the patient’s journey and locally available guidelines. Nevertheless, the main strength of our findings derives from the participation of GPs from several European countries providing detailed information regarding the clinical management of CM patients.
This study has some limitations. It is based on a survey and therefore relies on participants’ recall; thus, the risk of a selection bias of the participating GPs cannot be excluded. Moreover, GPs included had clinical experience with headache disorders suggesting that results regarding under-treatment of CM in primary care could be even higher than reported.
In summary, this project provides information on chronic and disabling migraine management in Europe and suggests the need for guidance in the primary care setting in order to leverage the diagnosis and treatment in such patients.
Conclusions
Despite the availability of evidence-based national and international guidelines, our study emphasizes that there is a need to improve the diagnosis and management of migraine in the primary care setting and more specifically the diagnosis, management, and referral, when appropriate, of CM patients.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
15 January 2021
A space was added in the 4th author's last name in the original article. The article has been updated to rectify the error.
Abbreviations
- CM:
-
Chronic migraine
- EHF:
-
European Headache Federation
- EM:
-
Episodic migraine
- GBD:
-
Global Burden of Diseases, Injuries, and Risk Factors
- GP:
-
General practitioner
- ICHD:
-
International Classification of Headache Disorders
- MOH:
-
Medication-overuse headache
- TTH:
-
Tension-type headache
- YLD:
-
Years lived with disability
References
MacGregor A. Migraine Ann Intern Med. 2017;166:ITC49–64.
Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2018;17:954–76.
Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, et al. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15:1–11.
Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. 2018;19:17.
Vos T, Abajobir AA, Abbafati C, Abbas KM, Abate KHA-AF, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–59.
Xu J, Kong F, Buse DC. Predictors of episodic migraine transformation to chronic migraine: a systematic review and meta-analysis of observational cohort studies. Cephalalgia. 2020;40:503–16.
Manack AN, Buse DC, Lipton RB. Chronic migraine: epidemiology and disease burden. Curr Pain Headache Rep. 2011;15:70–8.
Bigal ME, Serrano D, Buse D, Scher A, Stewart WF, Lipton RB. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache. 2008;48:1157–68.
Steiner TJ, Jensen R, Katsarava Z, Linde M, MacGregor EA, Osipova V, et al. Aids to management of headache disorders in primary care (2nd edition): on behalf of the European headache federation and lifting the burden: the global campaign against headache. J Headache Pain. 2019;20:57.
Headache Classification Committee of the International Headache Society (IHS). Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1–211.
Lipton RB, Manack Adams A, Buse DC, Fanning KM, Reed ML. A comparison of the chronic migraine epidemiology and outcomes (CaMEO) study and American Migraine Prevalence and Prevention (AMPP) study: demographics and headache-related disability. Headache. 2016;56:1280–9.
Adams AM, Serrano D, Buse DC, Reed ML, Marske V, Fanning KM, et al. The impact of chronic migraine: the chronic migraine epidemiology and outcomes (CaMEO) study methods and baseline results. Cephalalgia. 2015;35:563–78.
Bigal ME, Serrano D, Reed M, Lipton RB. Chronic migraine in the population: burden, diagnosis, and satisfaction with treatment. Neurology. 2008;71:559–66.
Lipton RB, Serrano D, Buse DC, Pavlovic JM, Blumenfeld AM, Dodick DW, et al. Improving the detection of chronic migraine: development and validation of identify chronic migraine (ID-CM). Cephalalgia. 2016;36:203–15.
Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ. Poor medical care for people with migraine in Europe – evidence from the Eurolight study. J Headache Pain. 2018;19:1–9.
British Association for the study of headache (BASH). Guidelines for All Healthcare Professionals in the Diagnosis and Management od Migraine, Tension-Type, Cluster and Medication-Overuse Headache. 2010. http://www.bash.org.uk/wp-content/uploads/2012/07/10102-BASH-Guidelines-update-2_v5-1-indd.pdf.
British Association for the study of headache (BASH). National Headache Managment system for adults. 2019.
Ducros A, Romatet S, Saint Marc T, Allaf B. Use of antimigraine treatments by general practitioners. Headache. 2011;51:1122–31.
Natoli JL, Manack A, Dean B, Butler Q, Turkel CC, Stovner L, et al. Global prevalence of chronic migraine: a systematic review. Cephalalgia. 2010;30:599–609.
Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache Pain. 2010;11:289–99.
Diener H-C, Limmroth V. Medication-overuse headache: a worldwide problem. Lancet Neurol. 2004;3:475–83.
Kurth T, Buring JE, Rist PM. Headache, migraine and risk of brain tumors in women: prospective cohort study. J Headache Pain. 2015;16:501.
Sempere AP, Porta-Etessam J, Medrano V, Garcia-Morales I, Concepción L, Ramos A, et al. Neuroimaging in the evaluation of patients with non-acute headache. Cephalalgia. 2005;25:30–5.
Do TP, Remmers A, Schytz HW, Schankin C, Nelson SE, Obermann M, et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology. 2019;92:134–44.
Potter R, Probyn K, Bernstein C, Pincus T, Underwood M, Matharu M. Diagnostic and classification tools for chronic headache disorders: a systematic review. Cephalalgia. 2019;39:761–84.
Lipton RB, Dodick D, Sadovsky R, Kolodner K, Endicott J, Hettiarachchi J, et al. A self-administered screener for migraine in primary care: the ID migraine validation study. Neurology. 2003;61:375–82.
Brighina F, Salemi G, Fierro B, Gasparro A, Balletta A, Aloisio A, et al. A validation study of an Italian version of the “ID Migraine”. Headache. 2007;47:905–8.
Streel S, Donneau A-F, Hoge A, Albert A, Schoenen J, Guillaume M. One-year prevalence of migraine using a validated extended French version of the ID Migraine™: A Belgian population-based study. Rev Neurol (Paris). 2015;171:707–14.
Sacco S, Benemei S, Cevoli S, Coppola G, Cortelli P, De Cesaris F, et al. Development and validation of the ID-EC - the ITALIAN version of the identify chronic migraine. J Headache Pain. 2019;20:15.
Haywood KL, Mars TS, Potter R, Patel S, Matharu M, Underwood M. Assessing the impact of headaches and the outcomes of treatment: a systematic review of patient-reported outcome measures (PROMs). Cephalalgia. 2018;38:1374–86.
Lipton RB, Tepper SJ, Reuter U, Silberstein S, Stewart WF, Nilsen J, et al. Erenumab in chronic migraine: patient-reported outcomes in a randomized double-blind study. Neurology. 2019;92:e2250–60.
Diener H-C, Holle-Lee D, Nägel S, Dresler T, Gaul C, Göbel H, et al. Treatment of migraine attacks and prevention of migraine: Guidelines by the German Migraine and Headache Society and the German Society of Neurology. Clin Transl Neurosci. 2019;3:2514183X18823377.
Negro A, Spuntarelli V, Sciattella P, Martelletti P. Rapid referral for headache management from emergency department to headache Centre: four years data. J Headache Pain. 2020;21:1–11.
Gago-Veiga AB, Díaz de Terán J, González-García N, González-Oria C, González-Quintanilla V, Minguez-Olaondo A, et al. How and when to refer patients diagnosed with secondary headache and other craniofacial pain in the Emergency Department and Primary Care: Recommendations of the Spanish Society of Neurology’s Headache Study Group. Neurologia. 2020;35:323–31.
Gago-Veiga AB, García-Azorín D, Mas-Sala N, Ordás CM, Ruiz-Piñero M, Torres-Ferrús M, et al. How and when to refer patients diagnosed with primary headache and craniofacial neuralgia in the emergency department or primary care: recommendations of the Spanish Society of Neurology’s headache study group. Neurologia. 2020;35:176–84.
Dodick D, Edvinsson L, Makino T, Grisold W, Sakai F, Jensen R, et al. Vancouver declaration on global headache patient advocacy 2018. Cephalalgia. 2018;38:1899–909.
Acknowledgements
We thank the GPs that participated in the survey, to Maite Artés, Nathalie Bofarull and Malena Águila (Adelphi Targis S.L.) for the project management and contribution along the study, and to Alba Gomez and Alba Llopis for their medical writing assistance.
Funding
Novartis Pharma AG financially supported the development of this project and the medical writing assistance and the page processing charges for this article. The authors have received no payment to write this article.
Author information
Authors and Affiliations
Contributions
PR, KS, AN, RS, HI, CS, AM and AG were all involved in the writing and review of this article and meet criteria for authorship as recommended by the International Committee of Medical Journal Editors (ICMJE). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics Committee approval from each country of the HCP that answered the survey was deemed unnecessary according to the International Ethical Guidelines for Health-related Research Involving Humans (CIOMS, Geneva 2016), since no data from any patient was collected. Results analysed in this manuscript come from a survey among European GPs intended to gather their opinion on chronic migraine management. The survey was performed following the European General Data Protection Regulation. All survey participants gave their written consent to analyse their answers anonymously. The anonymity of the participants was secured as all answers were aggregated before their analysis.
Consent for publication
Not applicable.
Competing interests
Dr. Ryvlin reports personal fees from Novartis, during the conduct of the study and personal fees from Eli Lilly and Novartis outside the submitted work.
Dr. Skorobogatykh reports personal fees from Novartis during the conduct of the study; and personal fees from Novartis and Teva, outside the submitted work.
Dr. Negro reports personal fees from Novartis during the conduct of the study, and personal fees from Allergan, Eli Lilly and Teva, outside the submitted work.
Dr. Sanchez-De La Rosa reports he is an employee and stakeholder of Novartis Pharma AG.
Dr. Israel-Willner has nothing to disclose.
Dr. Sundal reports personal fees from Novartis, during the conduct of the study and personal fees from Allergan, outside the submitted work.
Dr. MacGregor reports personal fees from Novartis, during the conduct of the study; personal fees from Eli Lilly, outside the submitted work; and Co-author of Aids to management of headache disorders in primary care (2nd edition): On behalf of the European Headache Federation and Lifting the Burden: The Global Campaign against Headache. Vol. 20, Journal of Headache and Pain. The Journal of Headache and Pain; 2019.
Dr. Guerrero reports personal fees from Novartis during the conduct of the study, and personal fees from Allergan, Exeltis, Eli Lilly and Teva outside the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Online questionnaire. 32-item questionnaire run online among GPs.
Additional file 2.
Profile of patients attended by GPs in 1 week, on average.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ryvlin, P., Skorobogatykh, K., Negro, A. et al. Current clinical practice in disabling and chronic migraine in the primary care setting: results from the European My-LIFE anamnesis survey. BMC Neurol 21, 1 (2021). https://doi.org/10.1186/s12883-020-02014-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-020-02014-6