Abstract
Background
The computed tomography (CT) finding of a pseudo-subarachnoid hemorrhage (SAH) may lead the treating physician into a diagnostic dilemma. We present a case of a pseudo-SAH in a patient with post-resuscitative encephalopathy, secondary to a newly diagnosed bleeding pulmonary arterio-venous malformation (AVM).
Case presentation
A 19-year-old female presented acutely with massive hemoptysis. Cardiopulmonary resuscitation (CPR) followed, and the patient was subsequently intubated for airway protection with intensive care unit (ICU) admission. Urgent CT angiography of the thorax showed a bleeding pulmonary AVM, with evidence of hemothorax. Non-contrasted cranial CT initially revealed cerebral edema. Day 3 post admission, repeat cranial CT showed worsening cerebral edema, with evidence of pseudo-SAH. Patient passed away the next day.
Conclusions
Pseudo-SAH, if present, carries a poor prognosis. It should be recognized as a potential CT finding in patients with severe cerebral edema, due to various causes. The diagnosis is vital, to avoid wrongful treatment institution, as well as determination of cause of death.
Similar content being viewed by others
Background
Acute SAH is seen on cranial CT as increased density of the basal cisterns and subarachnoid spaces [1]; the finding of which, in the absence of trauma, may necessitate further tests to determine the cause. However, a false positive diagnosis of an acute SAH may bring about potential problems – wrongful treatment, unnecessary workup for genetic predispositions, and difficulties in determining cause of death. A potential mimic to a true acute SAH, among others, is an entity called pseudo-SAH. This condition usually arises in the setting of a hypoxic encephalopathy, due to various causes. A combination of cerebral edema (with resultant reduced attenuation of the brain parenchyma), effacement of the subarachnoid spaces, as well as engorgement of venous structures in the pial surfaces leads to its perceptual high attenuation on cranial CT – leading to a false diagnosis of an acute SAH [2]. We report, in our experience, a young female who initially presented with massive hemoptysis, whom on serial cranial CT had findings of a pseudo-SAH.
Case presentation
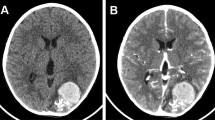
A 19-year-old female, with no underlying medical illness presented acutely to the Emergency Department with massive hemoptysis. Upon arrival, she was noted to be in asystole. Pupils were 4 mm bilaterally, non-reactive. CPR was commenced, and continued for 20 min until she was revived. Urgent blood work revealed a hemoglobin of 2.3 g/dL (normal range 12–15 g/dL), normal coagulation profile, and arterial blood gases indicative of metabolic acidosis. She was intubated for airway protection, and transferred to the ICU for further management. An urgent CT angiography of the thorax showed a right sided pulmonary AVM, with evidence of active bleeding (hemothorax) (Fig. 1). Non-contrasted cranial CT revealed cerebral edema (Fig. 2a). At this juncture, a decision was made to embolize the bleeding pulmonary AVM, should cerebral resuscitation show improvement. On day 3 of admission, repeat cranial CT showed dense basal cisterns and subarachnoid spaces (Fig. 2b), with marked worsening of the initially seen cerebral edema. A neurological consult was sought at this point, to assess the brain function, anticipating a possibility of brain death. The brain stem reflexes were absent, compatible with brain death. Additionally, the deep tendon reflexes were depressed, and the Babinski’s response was up-going. An electroencephalography was not pursued. Taking into account the previous history of resuscitation, worsening cerebral edema with a clinical diagnosis of brain death, stable hemoglobin level post transfusion, as well as fixed and dilated pupils (7 mm bilaterally), this is recognized to be a pseudo-SAH. Combined with the worsening cerebral edema and loss of grey-white matter differentiation, findings are suggestive of hypoxic-ischemic injury. The family was counselled, and decided to discontinue life support. Patient subsequently passed away.
a Non-contrasted cranial CT, on day of admission, taken at the level of the basal cisterns, in axial section showing evidence of cerebral edema, with mild loss of grey-white matter differentiation. b Non-contrasted cranial CT, on day 3 of admission, taken at the level of the basal cisterns, showing evidence of high density areas (red arrows) indicative of pseudo-SAH. Note that the cerebral edema is worse compared to the initial CT (a)
Discussion and conclusions
The radiological sign of pseudo-SAH was initially described in 1986, by Spiegel et al. [3]. At the beginning, diffuse cerebral edema was the attributed cause of this finding. Avrahami et al. [4] later reported that contrary to the previous understanding that this is a rare phenomenon, it is in fact common; detected in younger patients (below 40 years old) with high cerebral/skull volume, usually in the context of drug abuse, trauma, or cardiorespiratory arrest, leading to cerebral edema as a result of the hypoxic-ischemic injury. At present, multiple reports and studies have documented other causes of this finding, which include meningitis, subdural hemorrhage, infarction, contrast administration, spontaneous intracranial hypotension, post myelography, polycythemia, and chronic hypoxaemia, among others [5,6,7].
The dilemma between diagnosing a pseudo-SAH and a true acute SAH lies most importantly in the knowledge of the existence of such a phenomenon. Opeskin and Bedford et al. [8, 9], in their experience, encountered cases where antemortem acute SAH was diagnosed, leading to autopsy for confirmation. Upon reviewing the cranial CT scans available, as well as post mortem examination, there was no evidence of hemorrhage in the subarachnoid spaces. This highlights the importance of knowing the possible etiological factors of a pseudo-SAH and recognizing it when encountered. This avoids unnecessary post mortem examinations and wrongful determination of cause of death in some cases. Additionally, since one of the causes of a non-traumatic subarachnoid hemorrhage is a Berry aneurysm, which is potentially inherited, this avoids unnecessary screening of family members.
Yuzawa et al. [10] in 2008 showed that pseudo-SAH can be diagnosed using the CT parameters available at the physician’s disposal. In their study, they compared those with a pseudo-SAH, against those without. The Hounsfield unit (HU) of the high density areas were measured and compared. In those with pseudo-SAH, the HU values at the high density areas were in the range of 30–42 HU, with slight fluctuation with time. This is in contrast with those with a true SAH; where the values were higher (and decreased with time). Our patient had a HU value between 40 and 42 at the basal cisterns, corroborating this finding. In addition, they also looked at the onset of pseudo-SAH in their series. On day 3 of imaging, all of their patients exhibited CT findings of pseudo-SAH. This was also seen in our experience.
The underlying mechanism for the development of a pseudo-SAH till this day remains uncertain, although many postulations have been put forward [4, 5, 10, 11]. Among these, the most mentioned pathogenetic mechanism is the compression of the dural sinuses, leading to compromise of venous flow resulting in superficial veins engorgement – which appears as high dense areas in the background of low attenuated, edematous brain matter. Despite being engorged, this venous blood is still within the vasculature. Blood leaking from the vasculature has higher attenuation values due to the rapid plasma absorption, thus strengthening the study findings by Yuzawa et al. [10], that lower attenuation values seen in the high density areas suggest a pseudo-SAH, rather than a true SAH.
In conclusion, pseudo-SAH, despite being an entity that till this day remains unknown in frequency, should be recognized when encountered by treating physicians. Knowledge of the risk factors, pathogenetic mechanisms, and appearance on CT enables accurate and timely diagnosis – avoiding unnecessary tests and procedures.
Abbreviations
- Pseudo-SAH :
-
Pseudo-subarachnoid hemorrhage
- Pulmonary AVM:
-
pulmonary arterio-venous malformation
- CT:
-
Computed tomography
- CPR:
-
Cardiopulmonary resuscitation
- ICU:
-
Intensive care unit
- HU:
-
Hounsfield unit
References
Van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid hemorrhage. Lancet 2007; 369: 306-318.
Marder CP, Narla V, Fink JR, Fink KRT. Subarachnoid hemorrhage: beyond aneurysms. AJR. 2014;202:25–37.
Spiegel SM, Fox AJ, Vinuela F, Pelz DM. Increased density of tentorium and falx: a false positive CT sign of subarachnoid hemorrhage. Can Assoc Radiol J. 1986;37(4):243–7.
Avrahami E, Katz R, Rabin A, Friedman V. CT diagnosis of non-traumatic subarachnoid hemorrhage in patients with brain edema. Eur J Radiol. 1998;28(3):222–5.
Chun YL, Ping HL, Jui HF, Po CW, Huay BP. Pseudo-subarachnoid hemorrhage: A potential imaging pitfall. Can Assoc Radiol J. 2014;65:225–31.
Coady G, Brewer M, Maillloux P. Pseudosubarachnoid hemorrhage in a 42-year-old male with meningitis. Radiol Case Rep. 2011;6(2):470.
Patzig M, Laub C, Janssen H, Ertl L, Fesl G. Pseudo-subarachnoid hemorrhage due to chronic hypoxaemia: case report and review of the literature. BMC Neurology. 2014;14:219.
Opeskin K, Silberstein M. False positive diagnosis of subarachnoid hemorrhage on computed tomography scan. Journal of Clinical Neuroscience. 1998;5(4):382–6.
Bedford P, O’Donnell C. Pseudosubarachnoid hemorrhage on clinical computed tomography: The forensic implications of incorrect diagnosis. Am J Forensic Med Pathol. 2013;34(2).
Yuzawa H, Higano S, Mugikura S, Umetsu A, Murata T, Nakagawa A, et al. Pseudo-subarachnoid hemorrhage found in patients with postresuscitation encephalopathy: Characteristics of CT findings and clinical importance. AJNR Am J Neuroradiol. 2008;29:1544–9.
Given CA, Burdette JH, Elster AD, Williams DW. Pseudo-subarachnoid hemorrhage: A potential imaging pitfall associated with diffuse cerebral edema. AJNR Am J Neuroradiol. 2003;24:254–6.
Availability of data and materials
All in the manuscript.
Author information
Authors and Affiliations
Contributions
MSF was involved in the writing of this manuscript, literature search, as well as obtaining consent. AM was involved in critical analysis of the manuscript, as well as obtaining clinical information. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our institution does not require ethical approval for publication of single case reports.
Consent for publication
Written informed consent was obtained from the family members, for publication of this case report as well as accompanying images. Copy of the informed consent is available upon request.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Md Noh, M.S.F., Abdul Rashid, A.M. Development of pseudo-subarachnoid hemorrhage secondary to hypoxic-ischemic injury due to bleeding pulmonary arterio-venous malformation. BMC Neurol 18, 157 (2018). https://doi.org/10.1186/s12883-018-1161-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-018-1161-x