Abstract
Background
Impulse control and related disorders (ICRDs) are clinically complications in Parkinson’s disease (PD). However, the clinical characteristics of ICRDs in Chinese PD patients were rarely reported. We aimed to explore the prevalence and the clinical profile of ICRDs in Chinese patients with PD.
Methods
142 Chinese PD patients were consecutively enrolled. The symptoms of ICRDs were assessed with the Questionnaire for Impulsive-Compulsive Disorders. The clinical characteristics of patients with ICRDs and without ICRDs were compared.
Results
ICRDs were present in 31% of our patients. The most common ICRDs were compulsive medication use (11.3%) and punding (9.2%); the least frequent were walkabout (1.4%). Variables independently associated with ICRDs were earlier onset of the disease (≤55 years), severe cognitive impairment (MMSE 10–20), the dose of dopamine agonist (>1 mg/d) and dyskinesia.
Conclusions
ICRDs was commonly found in Chinese PD patients. Earlier onset of the disease, the dose of dopamine agonist, severe cognitive impairment and dyskinesia are independent factors associated with ICRDs. Our results will be benefit for clinicians to assess the risk of developing ICRDs before delivering dopaminergic medication.
Similar content being viewed by others
Background
Impulse control and related disorders (ICRDs) were defined as a number of behaviors involving repetitive, excessive and compulsive activities that interferes in major areas of life functioning [1]. Pathological gambling(PG), hypersexuality(HS), compulsive buying(CB) and binge eating(BE) were major symptoms of ICRDs. Other ICRDs are composed of punding, hobbyism, walkabout and compulsive medication use [1]. As a relatively recent addition to the behavioral spectrum of Parkinson’s disease (PD) related non-motor symptoms, ICRDs are becoming increasingly concerned.
The prevalence of ICRDs in PD was reported by different studies in different population, ranging from3.5% to 42.8% [2, 3]. These studies showed many factors may play a role in the risk of ICRDs in PD patients, including the use of dopamine agonists (DA), male gender, young patient, depression, smoking, drug abuse, genetic factors, family history of ICRDs and so on [4,5,6]. Especially, dopamine agonists were thought to be the major predictors for ICRDs [6]. Recently, Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s disease (QUIP) was developed and widely used to screen ICRDs in PD patients [7]. It is well known that, Chinese PD patients are typically treated with lower dosages of medications and present cultural differences in perceptions of disease [8]. This raises the question that whether the prevalence of ICRDs is lower in Chinese PD patients and which factors affect the risk of ICRDs in Chinese PD patients. Therefore, our study aims to study the prevalence and the possible impact factors of ICRDs in Chinese PD patients.
Methods
Participants
142 subjects were enrolled at the department of neurology, Xin Hua Hospital affiliated to Shanghai Jiaotong University School of Medicine from December 2014 to October 2016. Patients were diagnosed as PD according to the UK Brain Bank criteria [9]. The records of PD medication and dosage were taken at the time of assessment. Patient with secondary Parkinsonism, deep brain stimulation, stroke, brain tumor and treated with levodopa infusion were excluded. Once those patients included in the study, a structured interview for clinical and demographic variables was performed by a neurologist. All participants had written informed consent. This study was performed with the approval of the Ethics Committee of Xin Hua Hospital affiliated to Shanghai Jiaotong University School of Medicine.
Clinical assessment
The following demographic and clinical features data were retrieved from subjects: gender, age, education,alcoholism and smoking status, age at PD onset, duration of disease, predominant symptoms at PD onset, the history of dopamine replacement therapy and related complications (Total levodopa equivalent daily dose, LEDD, was calculated according to previously suggested conversion formulae) [10], Hoehn-Yahr stage (H&Y), Unified Parkinson’s disease Rating Scale (UPDRS), the scale for freezing of gait, Minimum Mental State Examination (MMSE), non-motor symptom (NMS), REM Sleep Behavior Disorder Questionnaire Hong Kong (RBDQ-HK), Hamilton Anxiety Scale (HAMA), Hamilton Depression Scale (HAMD), and Parkinson’s Disease Questionaire-39 (PDQ-39). The symptoms of ICRDs were assessed with QUIP.
Statistical analysis
Statistical analysis was performed using SPSS 20.0; Categorical variables were compared using the Pearson’s Chi-Square test or the Mann-Whitney test or Student’s t-test; Binary logistic regression model was performed to evaluate factors that could independently associate with ICRDs. Level of significance was set at p < 0.05. Odds ratio (OR) are presented with their 95% confidence intervals (95% CI).
Results
Subject characteristics
142 Chinese PD patients participated in our study. Demographic and clinical information of our patients are listed in Table 1. Of them, 73 (51.4%) were male and 69 (48.6%) were female. Their mean age at study was 68.39 ± 8.14 years, mean age at onset of PD motor symptoms was 62.06 ± 9.27 years and mean disease duration was 6.00 ± 5.56 years. The mean MMSE score was 26.18 ± 4.07 and the mean Hoehn-Yahr stage was 2.25 ± 0.84 (stage 1 and 1.5, n = 41; stage 2 and 2.5, n = 69; stage 3, n = 21, and stage 4 and 5, n = 11). The mean UPDRS motor score for the entire study group was 19.32 ± 12.42.The mean total UPDRS score for the entire group was 33.23 ± 19.06, the mean UPDRS IV(motor complication) score was 0.99 ± 2.27,and the mean UPDRS 32 + 33(dyskinesia)score was 0.29 ± 1.00. Antiparkinsonian drugs with DA was reported in 49.3% (DA-LEDD 41.90 ± 52.13) and L-dopa in 68.3% (LEDD 314.09 ± 320.63) of patients. The total LEDD was 389.40 ± 373.72. The most common medication was a combination of levodopa and DA, which was used by 63 (44.4%) of the patients, with 10 of them using additionally a MAO-B inhibitor. The combination of DA and MAO-B inhibitor was used by 10 (7%) patients. Monotherapy was used by 25 (17.6%) of the patients (19 (13.4%) levodopa, 6 (4.2%) DA). None of our patients was reported to have family history of impulse control disorders.
3.2. Frequency of ICRDs.
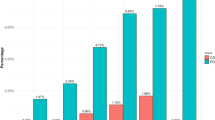
The frequencies and clinical features of ICRDs screening with QUIP are illustrated in Fig. 1.We identified 44(31.0%) patients with ICRDs (28 presented 1 ICRDs, and 16 presented multiple ICRDs). compulsive medication use (11.3%) was the most frequent, followed by punding (9.2%), pathological gambling (7.0%), hobbyism (6.3%), binge eating (5.6%), compulsive buying (4.9%), hypersexuality (2.8%) and walkabout (1.4%). Male patients are prone to report compulsive medication use and hypersexuality.
3.3. Association between ICRDs and clinical variables
Compared with PD patients without any ICRDs, ICRDs positive patients were younger, earlier onset of PD, and had a longer disease course. More smokers and lower MMSE score were found in patients with any ICRDs. Then, ICRDs patients were more likely to have higher scores in UPDRS IV, UPDRS 32 + 33(dyskinesia), HAMA and the scale for freezing of gait. In ICRDs group, the DA-LED was 61.61 ± 61.37 mg/d while the DA-LED in non-ICRDs group was much lower (30.36 ± 42.97 mg/d). The doses of levodopa did not show any difference between two groups. However, there was no statistically significant difference in gender, marriage status, education background, the PD phenotype at PD onset, depression, quality of life, RBD, non-motor symptoms, UPDRS or H&Y stage between two groups.
Variables entered into the multiple logistic regression analysis were: age at PD onset, DA LEDD, UPDRS 32 + 33 score and L-dopa treatment duration, after adjusting for all the covariates that were associated with ICRDs (sex, age, age of onset, smoking, TLEDD,DA-LEDD, levodopa dosage and the MMSE, HAMA, UPDRS 32 + 33, freezing of gait) in multivariable analysis. In the analysis, earlier onset of the disease (p = 0.001,OR 5.99,95%CI 2.10–17.09), the dose of oral DA LEDD (p<0.001, OR 15.94,95%CI 3.66–69.45), lower MMSE score(p=0.002, OR 6.71,95%CI 2.03–22.17)and dyskinesia (UPDRS32 + 33 score)(p = 0.04,OR 4.94,95%CI 1.07–19.99) were significantly increased the odds of ICRDs (Table 2).
Discussion
Identification of ICRDs in PD patients will be benefit for clinicians to making therapeutic decisions and avoiding important social, economic and legal problems for patients. In our study, nearly one third of our subjects present at least one kind of ICRDs (31%), which is similar in some population, such as Malaya (35%) [11], India (31.6%) [3], Finland (34.8%) [5] and Denmark (35.9%) [12]. However, the incidence of phenotypes of ICRDs was diverse in different population. In our patients, the most common ICRDs were compulsive medication use (11.3%). On the contrary, the most frequent ICRDs was PG in North America (DOMINION study) [6], punding in India [3], hypersexuality in Finland [5], hobbyism and punding in Denmark [11]. The cause of these differences may be that the questionnaire used for screening ICRDs in those studies were different with ours. On the other hand, cultural, social and economic factors might also play a role on the phenotype of ICRDs in Chinese PD patients (e.g., casino is illegal and patients were ashamed to report sexual behavior to doctor in China). The overall prevalence of ICRDs was similar among male and female in this study, however, there are some slightly differences exist in the incidence of phenotypes of ICRDs, HS was more frequency in male, but BE, PG and CB was more frequency in female. Our results indicated QUIP has high sensitivity, and patients need to be evaluate the risk of developing ICRDs when exposure to dopaminergic medication. Deep brain stimulation is rarely implemented in Chinese PD patient. Furthermore, the mechanisms of deep brain stimulation inducing impulsive controlling disorders might be different with drug induced impulse control disorders. Therefore, we exclude those patients treated with deep brain stimulation and will investigate the role of deep brain stimulation on ICRDs in future.
Consistent with previously studies [6], usage of DA is correlates with ICRDs among Chinese patients with PD. We did not carry on the sub-analysis of dopamine subtype,especially of D3 receptor stimulus agonist, since only pramipexole and piribedil are available in China. In addition, only 6 of our patients took piribedil, sub-analysis was not suitable for our study. Furthermore, the regression analyses suggest that the dosages of DA (>1 mg/d) was the strongest association factor for ICRDs, so we should be more careful in the course of increasing the dose of DA.
In addition, our study indicated that dyskinesia was independently associated with ICRDs. There might be many reasons for this result. Firstly, from common risk factor perspective, both ICRDs and dyskinesia might be affected by excessive dopaminergic drug stimulation, earlier onset of the disease and severe cognitive impairment [13, 14]. Secondly, from pathophysiology perspective, both ICRDs and dyskinesia might be induced by excessive stimulation in the motor or limbic territories of the striatum. But the detail mechanism of biochemical, molecular and functional changs need further investigation. These findings remind clinicians that youth patients with PD who intake high dose of dopamine agonist and have poor cognitive function should be prevent from both ICRDs and dyskinesia.
The relatively serious cognitive impairment appeared in PD patients with ICRDs (measured by MMSE) in our study. It may be caused by impaired top-down inhibitory control from prefrontal cortical area. However, the association between cognition and ICRDs in PD subjects is still debatable according to previous studies [12, 15, 16]. Moreover, freezing of gait was also related to ICRDs, even though it did not enter the regression model. It consist with PD patients have gait disturbance were more prone to developed ICRDs which have been reported in other studies [17]. The limitations of our investigation may be from the recruitment of subjects from a single movement disorder center, the lack of an age matched control group, cross-sectional evaluation at a single time point, the small sample size and the questionnaire we used.
Conclusions
ICRDs are common in Chinese PD patients. QUIP was a useful screening instrument for ICRDs in PD. Early onset of PD, dyskinesia and dopamine replacement therapies were significantly associated with ICRDs. Clinicians need to routine elevate the risk of developing ICRDs before delivering dopaminergic medication, especially those with certain clinical and demographic characters, such as earlier onset of the disease, cognitive impairment, higher dosage of DA and dyskinesia.
Abbreviations
- ICRDs:
-
Impulse control and related disorders
- PD:
-
Parkinson’s disease
- PG:
-
Pathological gambling
- HS:
-
Hypersexuality
- CB:
-
Compulsive buying
- BE:
-
Binge eating
- DA:
-
Dopamine agonists
- QUIP:
-
Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s disease
- H&Y:
-
Hoehn-Yahr stage
- UPDRS:
-
Unified Parkinson’s disease Rating Scale
- MMSE:
-
Minimum Mental State Examination
- NMS:
-
Non-motor symptom
- RBDQ-HK:
-
REM Sleep Behavior Disorder Questionnaire Hong Kong
- HAMA:
-
Hamilton Anxiety Scale
- HAMD:
-
Hamilton Depression Scale
- PDQ-39:
-
Parkinson’s Disease Questionaire-39
- OR:
-
Odds ratio
- LEDD:
-
Levodopa equivalent daily dose
References
Weintraub D, David AS, Evans AH, Grant JE, Stacy M. Clinical spectrum of impulse control disorders in Parkinson's disease. Mov Disord. 2015;30:121–7.
Sharma A, Goyal V, Behari M, Srivastva A, Shukla G, Vibha D. Impulse control disorders and related behaviours (ICD-RBs) in Parkinson's disease patients: assessment using “questionnaire for impulsive-compulsive disorders in Parkinson's disease” (QUIP). Ann Indian Acad Neurol. 2015;18:49–59.
Sarathchandran P, Soman S, Sarma G, Krishnan S, Kishore A. Impulse control disorders and related behaviors in Indian patients with Parkinson's disease. Mov Disord. 2013;28:1901–2.
Vela L, Martinez Castrillo JC, Garcia Ruiz P, Gasca-Salas C, Macias Macias Y, Perez Fernandez E, Ybot I, Lopez Valdés E, Kurtis MM, Posada Rodriguez IJ, Mata M, Ruiz Huete C, Eimil M, Borrue C, Del Val J, López-Manzanares L, Rojo Sebastian A, Marasescu R. The high prevalence of impulse control behaviors in patients with early-onset Parkinson's disease: a cross-sectional multicenter study. J Neurol Sci. 2016;368:150–4.
Joutsa J, Martikainen K, Vahlberg T, Voon V, Kaasinen V. Impulse control disorders and depression in Finnish patients with Parkinson's disease. Parkinsonism Relat Disord. 2012;18:155–60.
Weintraub D, Koester J, Potenza MN, Siderowf AD, Stacy M, Voon V, Whetteckey J, Wunderlich GR, Lang AE. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol. 2010;67:589–95.
Weintraub D, Hoops S, Shea JA, Lyons KE, Pahwa R, Driver-Dunckley ED, Adler CH, Potenza MN, Miyasaki J, Siderowf AD, Duda JE, Hurtig HI, Colcher A, Horn SS, Stern MB, Voon V. Validation of the questionnaire for impulsive–compulsive disorders in Parkinson's disease. Mov Disord. 2009;24:1461–7.
Zhang ZX, Chen H, Chen SD, Shao M, Sun SG, Qu QM, Zhang BR, Liu YM, Xu Q, Wan X, Li L, Wen HB, Chen X, Chen HB, Liu ZG, Wang J, Wang G. Chinese culture permeation in the treatment of Parkinson disease: a cross-sectional study in four regions of China. BMC Res Notes. 2014;30(7):65.
Daniel SE, Lees AJ. Parkinson’s disease society brain Bank, London: overview and research. J Neural Transm Suppl. 1993;39:165–72.
Fenelon G, Mahieux F, Huon R, Ziegler M. Hallucinations in Parkinson’s disease: prevalence, phenomenology and risk factors. Brain. 2010;123:733–45.
Lim SY, Tan ZK, Ngam PI, Lor TL, Mohamed H, Schee JP, Tan AK, Ooi E, Soh PC. Impulsive-compulsive behaviors are common in Asian Parkinson's disease patients: assessment using the QUIP. Parkinsonism Relat Disord. 2011;17:761–4.
Callesen MB, Weintraub D, Damholdt MF, Moller A. Impulsive and compulsive behaviors among Danish patients with Parkinson's disease: prevalence, depression, and personality. Parkinsonism Relat Disord. 2014;20:22–6.
Jiménez-Urbieta H, Gago B, de la Riva P, Delgado-Alvarado M, Marin C, Rodriguez-Oroz MC. Dyskinesias and impulse control disorders in Parkinson’s disease: from pathogenesis to potential therapeutic approaches. Neurosci Biobehav Rev. 2015;56:294–314.
Voon V, Napier TC, Frank MJ, Sgambato-Faure V, Grace AA, Rodriguez-Oroz M, Obeso J, Bezard E, Fernagut PO. Impulse control disorders and levodopa-induced dyskinesias in Parkinson's disease: an update. Lancet Neurol. 2017 Mar;16(3):238–50.
Alzahrani H, Venneri A. Cognitive and neuroanatomical correlates of neuropsychiatric symptoms in Parkinson's disease: a systematic review. J Neurol Sci. 2015;356:32–44.
Siri C, Cilia R, Reali E, Pozzi B, Cereda E, Colombo A, Meucci N, Canesi M, Zecchinelli AL, Tesei S, Mariani CB, Sacilotto G, Zini M, Pezzoli G. Long-term cognitive follow-up of Parkinson's disease patients with impulse control disorders. Mov Disord. 2015;30:696–704.
Leroi I, Andrews M, McDonald K, Harbishettar V, Elliott R, Byrne EJ, Burns A. Apathy and impulse control disorders in Parkinson’s disease: a direct comparison. Parkinsonism Relat Disord. 2012;18:198–203.
Acknowledgments
We are grateful to the professor Weindraub D for the permission of using QUIP and appreciate all patients participating in this study.
Author contributions
YZ and ZGL designed the original study and wrote the manuscript. AQH, LL and WC recruited the patients and analysed the data: YZ and AQH revised the manuscript and supervised the study. All authors gave their final approval to the study to be published and agree to be accountable for all aspects of the work.
Funding
This study was granted by the National Natural Science Foundation of China (Number 81301081). The funder had no role in the design of the study, collection, analysis, interpretation of data and writing the manuscript.
Availability of data and materials
Characteristics of study population are included in the Tables and figure. Further data set could be obtained on request if required.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
All participants and author provided written consent for publication.
Ethics approval and consent to participate
Ethical approval for the original study was obtained from the Ethics Committee of Xin Hua Hospital affiliated to Shanghai Jiaotong University School of Medicine. And all participants provided written informed consent.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhang, Y., He, A.q., Li, L. et al. Clinical characteristics of impulse control and related disorders in Chinese Parkinson’s disease patients. BMC Neurol 17, 98 (2017). https://doi.org/10.1186/s12883-017-0874-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-017-0874-6