Abstract
Objective
To validate an association between new inflammation and frequent peritoneal dialysis-associated peritonitis (PDAP).
Materials and methods
In China, retrospective clinical data were collected on 208 patients who received continuous ambulatory peritoneal dialysis (CAPD) between 2010 and 2021. The patients were divided into two groups: non-frequent PDAP (the interval between two peritonitis episodes of more than one year) and frequent PDAP (the interval between two peritonitis episodes of less than one year). Patients with their first episode of peritonitis had their age, gender, history of hypertension, diabetic disease, underlying renal disease, bacterial infection, and laboratory data collected. The outcomes of bacterial dispersion, systemic immune-inflammation index (SII), high-density lipoprotein cholesterol (HDL-C), C-reactive protein (CRP), and risk variables associated with frequent PDAP were analyzed.
Results
There are differences between the two groups in dialysis time (p = 0.006), hypertensive nephropathy (p = 0.038), staphylococcus (p = 0.035), white blood cells (p = 0.001), neutrophil (p < 0.01), lymphocyte (p < 0.01), platelet(p = 0.01), SII(p < 0.01), CRP/HDL-C (p = 0.002), CRP (p < 0.001), serum creatinine (p = 0.007), blood urea nitrogen (p = 0.05), serum magnesium (0.03), serum potassium (p = 0.007), and dialysate polymorphonuclear cells (p = 0.004). Multifactorial logistic regression analysis found that SII (p < 0.001), CRP/HDL-C (p = 0.041), and Diabetes mellitus (p = 0.027) were independent risk factors for frequent PDAP. The ROC curve analysis revealed that combining SII with CRP/HDL-C resulted in the largest AUC area (AUC = 0.814).
Conclusions
Our findings offer clinical proof of the combination of SII and CRP/HDL-C in patients with frequent PDAP.
Similar content being viewed by others
Introduction
Peritoneal Dialysis (PD) has become one of the primary renal replacement therapies for patients with end-stage renal disease (ESRD) due to the benefits of preserving residual renal function and the ease of promotion. Given the rapid global spread of coronavirus 2019 (COVID-19), PD outperforms hemodialysis (HD) as an effective renal replacement therapy with a lower risk of bacterial illness [1]. However, the problem of PDAP (peritoneal dialysis-associated peritonitis) is becoming more prevalent in clinical practice. PDAP is a major complication of PD patients that can account for more than 15% of patient deaths [2,3,4]. Furthermore, peritoneal ultrafiltration capacity is reduced after a single episode of severe peritonitis or multiple episodes of peritonitis. They could even cause sclerosing encapsulated peritonitis. They are essential contributors to PD patients converting to long-term hemodialysis [5–6]. Frequent episodes of PDAP cause peritoneal fibrosis, which leads to peritoneal function loss, decreased residual renal function, and increased rates of extubation and withdrawal in PD patients [7]. A cohort study in Taiwan found an increase in adverse outcome events in PD patients as the times of peritonitis increased [8].
The relevance of inflammation in PD patients is noteworthy. Numerous well-known inflammatory markers, such as neutrophils, lymphocytes, platelet count, and CRP, have been linked to PDAP [9,10,11]. However, focusing on just one marker is ineffective because these biomarkers are constantly influenced. The systemic immune-inflammation index (SII) has recently been advocated as a convenient and comprehensive marker. SII is an emerging indicator of inflammation that can comprehensively reflect the inflammatory and immune status of the body. SII is the ratio of neutrophil count × platelet count/lymphocyte count, which has been shown to be an independent predictor of tumor recurrence metastasis and prognosis [12]. CRP is a pattern recognition molecule in inflammation processing [13]. PD patients with altered nutritional status and chronic inflammation are frequently combined with dyslipidemia. According to some studies, HDL-C in ESRD patients is less effective at promoting cholesterol efflux and has antioxidant and anti-inflammatory deficiencies. In uremic patients, HDL-C composition even shifts toward a pro-inflammatory phenotype [14]. Low HDL-C levels symbolize dyslipidemia in PD patients and have been attributed to cardiovascular disease (CVD) and mortality in numerous trials [15, 16]. Since CRP may reflect the degree of inflammation and HDL-C may reflect the organism’s anti-inflammatory effect. The combination allows for a comprehensive assessment of the organism’s balance of inflammatory and anti-inflammatory. A high CRP/HDL-C ratio was a potential indicator of poor patient prognosis and increased mortality in a study of patients with novel coronavirus pneumonia [17].
However, there are few scientific studies that combine SII and CRP/HDL-C to predict outcomes in patients with frequent PDAD. As a result, the purpose of this multicenter retrospective study was to investigate the factors associated with the emergence of frequent peritonitis in PD patients treated between 2010 and 2021.
Materials and methods
Study subjects
Patients who received regular PD treatment and developed PDAP were recruited for the study and followed up at the Peritoneal Dialysis Center of the Affiliated Hospital of Xuzhou Medical University, Xuzhou Central Hospital, and Xuzhou Mining Group General Hospital between 1/1/ 2010 and 1/9/ 2021. Depending on the number of times peritonitis occurred, patients were divided into two groups: frequent PDAP and non-frequent PDAP. According to ISPD [18, 19], frequent PDAP was defined as the interval between two peritonitis episodes being less than one year. Frequent PDAP includes recurrent peritonitis (an episode that occurs within 4 weeks of completion of therapy of a prior episode but with a different organism), relapsing peritonitis (the episode that occur within 4 weeks of completion of therapy of a prior episode with the same organism or being culture negative), repeat peritonitis (an episode that occurs > 4 weeks after completion of therapy of a prior episode with the same organism).
The inclusion criteria were: (1) Patients with clinically confirmed PDAP; (2) Patients who were older than 18 years old. Exclusion criteria: (1) Patients who died, renal transplantation, and conversion to hemodialysis within one year after the first occurrence of PDAP; (2) Patients with combined hematologic diseases, autoimmune diseases, and malignant tumors; (3) Patients who received PD treatment for less than one month; (4) Patients occurred to peritonitis intervals of less than one month; (5) Patients whose culture bacteria results were fungal infections. The Hospital Committee of Xuzhou Medical University approved this study in 2022. (Ethical number: XYFY2022-KL218)
PDAP diagnostic criteria and efficacy judgement
All patients received CAPD with lactate-buffered glucose dialysate via a Tenckhoff (Baxter International Inc) peritoneal dialysis catheter with a double bag connection system. All patients attended regularly scheduled PD training sessions led by qualified nursing professionals. In accordance with the 2016 ISPD recommendations, peritonitis was identified. More than two characteristics had to be present for PDAP to be diagnosed [19]: (1) abdominal pain or cloudy dialysate effluent; (2) dialysate WBC counts (WBCs) > 100/µl (after more than two hours of lingering), with polymorphonuclear of > 50%; (3) dialysate effluent culture that is positive.
Efficacy Judgement: (a) Effective Treatment: After three days of antibiotic medication, the symptoms of abdominal pain are eased. In the subsequent laboratory results, the effusion fluid’s turbidity is resolved, and its leukocyte count is either decreased or normalized; (b) Ineffective extubation: When PDAP therapy is unsuccessful, or the patient’s symptoms aggravate as a result of therapy, the PD is extubated and converted to hemodialysis or renal transplant. Due to peritoneal failure or a hernia that cannot be repaired well occurred during therapy; (c) Peritonitis-related death: Patients died from active peritonitis or hospitalization due to peritonitis or died within two weeks of the onset of peritonitis.
Basic demographic, clinical, and laboratory data
-
1)
Demographic characteristics: baseline data collected at the first PDAP episode. Data were collected when patients were first admitted to the hospital and were not receiving treatment. The information comprised the following: age, gender, comorbidities, history of hypertension (HD), history of diabetes mellitus (DM), cause of ESRD, PD duration, and results of pathogenic bacteria culture.
-
2)
Laboratory parameters: gather information before applying antibiotics. The data included white blood cell counts (WBC), neutrophil (NE), lymphocyte (LY), red blood cell counts (RBC), platelet (PLT), hemoglobin (HGB), red blood cell distribution width (RDW), C-reactive protein (CRP), serum albumin (ALB), serum creatinine (Cr), serum uric acid (UA), blood urea nitrogen(BUN),high-density lipoprotein (HDL-C), low-density lipoprotein (LDL), total cholesterol (TC), triglycerides (TG), serum calcium (Ca), serum phosphorus (P), serum magnesium (Mg), serum potassium (K), glucose (Glu).When suspected peritonitis, dialysate is gathered for dialysate leukocyte count, dialysate polymorphonuclear cells and pathogenic microorganisms.
Treatment
Dialysate is gathered for cell counting, Gram staining, and bacterial culture when peritonitis is suspected. At the bedside, 8 to 10 mL of dialysate is collected in two blood culture flasks (aerobic and anaerobic), and if there is no positive signal within 48 h, the culture may be extended to five days; another approximately 50 ml of dialysate is collected in sterile tubes for Gram staining and blood agar culture, agar plate culture may be continued under aerobic and anaerobic conditions for three days until microorganisms are detected. According to ISPD Guidelines, the current treatment are vancomycin or first-generation cephalosporin for Gram-positive organism coverage, and third-generation cephalosporin or aminoglycoside for Gram-negative organism coverage by intraperitoneal perfusion in combination [19].
Definition of SII
SII = platelet count × neutrophils/lymphocytes, NLR = neutrophil/lymphocyte ratio, and PLR = platelet/lymphocyte count, CRP/HDL-C = CRP/HDL-C ratio [9,10,11].
Study endpoint
Until they were removed from PD therapy or lost to follow-up owing to conversion to hemodialysis, kidney transplantation, death, etc., patients in this study group were constantly followed. Until September 1, 2022, patients who did not have any of these occurrences were monitored.
Statistical analysis
For the statistical analysis, SPSS 26.0 software was utilized. The normal distribution of data was expressed as x ± s, and the t-test was performed to distinguish between two groups; if the data did not follow the normal distribution, they were described as M (Q1, Q3), and a non-parametric test was utilized to contrast the groups. The rate of use was applied to represent the statistical data, and the χ² test was implemented to compare the groups.
The relationship between SII and CRP/HDL-C and the risk of developing frequent PDAP was discovered using logistic regression analysis. The ROC curve was used to assess the predictive value of SII and CRP/HDL-C for the development of frequent PDAP in PD patients. A statistically significant difference was regarded as P < 0.05.
Results
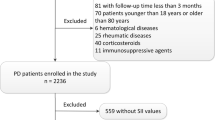
Flow diagram of the study population and comparison of the basic data of the two groups: In total, 208 patients with PDAP were recruited from three PD institutions for our study. There were 132 (63.5%) patients in the non-frequent PDAP group and 76 (36.5%) patients in the frequent PDAP group. The average age was 50.5 years, and 126 (60.6%) patients were male. A total of 100 patients (48.08%) had chronic glomerulonephritis, 46 had diabetic nephropathy, 37 (17.79%) had hypertensive nephropathy, and 25 (12.02%) had other diseases. Only the differences in dialysis time (p = 0.006), hypertensive nephropathy(p = 0.038), and staphylococcus (p = 0.035) were statistically significant when the baseline data of the two groups were compared. Gram-positive bacterial infections, particularly those caused by Staphylococcus aureus, were significantly more likely in the patients who had experienced more episodes. In other organisms, no distinction between the two groups could be discerned (P > 0.05) (Table 1) & (Fig. 1).
Laboratory data comparison between two groups: as shown in Table 2, there were statistically significant differences in WBC (p = 0.001), NE (p < 0.01), LY (p < 0.01), PLT (p = 0.01), SII (p < 0.01), CRP/HDL-C (p = 0.002), CRP (p < 0.001), Cr (p = 0.007), BUN (p = 0.05), Mg (p = 0.03), K (p = 0.007), and dialysate polymorphonuclear cells (p = 0.004) between the two groups. There was no difference between age, sex, hypertension, RBC, HGB, RDW, TC, TG, LDL, HDL-C, Ca, P, Glu, and dialysate leukocytes (P > 0.05) (Table 2).
Logistic Regression Analysis of Risk Factors in Patients with frequent PDAP: Univariate regression analyses revealed that diabetes mellitus, CRP/HDL-C, CRP, PLT, SII, LY, NE, WBC and PD duration were associated with frequent PDAP. When potential variables such as PD duration, diabetes, CRP/HDL-C, and SII were included, the multivariate stepwise regression analysis revealed that SII (β: 0.001; 95% CI:1.001 to 1.001; p < 0.001), CRP/HDL-C (β:0.004; 95% CI: 1 to 1.009; p = 0.041) and Diabetes mellitus (β:0.823; 95%CI: 1.1 to 4.72; p = 0.027) were independent variables related to frequent PDAP. (Table 3) & (Fig. 2).
ROC curves of SII, CRP/HDL-C, and SII combined with CRP/HDL-C for predicting frequent PDAP: excellent discrimination is indicated by the prognosis models, which have an area under the curve (AUC) of over 0.80. The discriminative ability of SII (AUC = 0.789, 95%CI:0.723 to 0.855, P < 0.001) and CRP/HDL-C (AUC = 0.706, 95%CI: 0.634 to 0.777, P < 0.001) was excellent. The most incredible AUC area was found when SII and CRP/HDL-C were combined (AUC = 0.814, 95%CI: 0.752 to 0.876, P < 0.001) (Fig. 3).
Discussion
PDAP has been one of the most prevalent and severe complications in PD patients, despite variations between nations, regions, and centers of various sizes and levels of care. A prospective cohort analysis conducted between 2014 and 2017 in seven countries revealed that the incidence of PDAP varied between 0.26 and 0.40 episodes/patient-year [20]. Based on our research, SII and CRP/HDL-C appear to have been independent risk factors for frequent PDAP in PD patients. In contrast to high SII levels and low CRP/HDL-C levels alone, high SII levels and concurrently low CRP/HDL-C levels were more strongly related to frequent PDAP in PD patients in our study. Inflammation is a permanent state in PD patients. It is attributed to several factors: microenvironment of uremia, infection, declined removal of pro-inflammatory cytokines, volume overload, oxidative stress, and some dialysis-related variables [10, 21,22,23,24]. The reasons for the poor prognosis of patients with healed peritonitis may be related to the presence of chronic inflammation (both systemic and localized in the abdominal cavity) in the patient [25]. The mechanism by which systemic inflammation is mainly related to the release of large amounts of inflammatory mediators causing a decrease in appetite and protein-energy depletion in patients. Although acute infections caused by pathogenic microorganisms resolve, systemic inflammation may persist, leading to frequent episodes of peritonitis as a result of the patient’s compromised immune system and inability to effectively fight off bacterial infection [26]. Localized inflammation in the abdominal cavity is manifested by a persistent increase in inflammatory cells and pro-inflammatory factors in the peritoneal fluid after the peritonitis has resolved [27]. The persistence of local inflammation in the peritoneal cavity can lead to peritoneal mesothelial degeneration, detachment and impaired regeneration, peritoneal fibroblast proliferation and extracellular matrix deposition. Secondly peritonitis decreases the ability of peritoneal solute removal and ultrafiltration, leading to impaired peritoneal structure and function [28].
In the initial phases of inflammation, neutrophils phagocytose pathogens and particles. They simultaneously release antimicrobial peptides and reactive oxygen and nitrogen species [29]. During inflammation, activated platelet count mix with monocytes and lymphocytes to create microparticles that promote the formation of neutrophil extracellular traps (NTEs). NTEs exacerbate the inflammatory response by stimulating the production of inflammatory factors [30]. By encouraging microthrombus, activated platelet count exacerbate the inflammatory response [31]. However, none of these biomarkers provides a comprehensive picture of the body’s inflammatory and immunological condition. SII provides an integrated view of inflammation, immunity, and microthrombus. It has been widely reported that this index can predict the frequency of contrast-induced acute kidney injury (CI-AKI), cancer survival, and cardiovascular disease [32,33,34,35,36]. In 2014, Bo [37] first defined SII as a new indicator of immune evaluation based on a study on the prognosis of patients with hepatocellular carcinoma, and higher SII indicates that patients have stronger inflammation and weaker immune response, suggesting a poor prognosis. The frequent PDAP patients in our study had higher SII scores, which indicated more severe inflammation and a weakened immune system. Increased neutrophil levels frequently indicate an infectious condition and an organism invasion by a specific pathogenic microorganism. The prediction of frequent PDAP is connected with a chronic, long-term, persistent microinflammatory state in patients after the initial infection since it does not depend on the degree of direct invasive overt infection, according to standardized anti-infective therapy for primary PDAP. Thus, this study demonstrates that high SII levels are individually bound to an elevated risk of frequent PDAP after accounting for the duration of PD and DM events. Increased neutrophil-to-lymphocyte ratio (NLR) levels have been exposed to a higher risk of PDAP treatment failure. NLR can also independently predict the severity of cardiovascular disease and mortality [9, 38]. According to earlier studies, a higher SII was tied to a more serious risk of patient death in critically sick patients with acute kidney damage [10].
Meanwhile, this study discovered that patients with frequent PDAP had lower HDL-C concentrations and higher CRP concentrations. The prognostic significance of CRP/HDL-C for frequent PDAP is demonstrated by our findings. HDL-C performs a significant anti-infective function in a variety of methods. Gram-negative bacterial lipopolysaccharide (LPS) and Gram-positive bacterial lip lactic acid (LTA) is bonded and neutralized by HDL-C. HDL-C suppresses the expression of pro-inflammatory cytokine-induced adhesion molecules such as ICAM-1, V-CAM-1, and E-selectin. Additionally, HDL-C blocks the activation and recruitment of monocytes. Reducing ROS generation and inhibiting LDL oxidation offers protection from oxidation [39–40]. HDL-C function was altered in studies comparing CKD patients to the general population, patients with CKD3 and CKD4 stages, and the population receiving hemodialysis. The study reveals that HDL-C mainly affects the apoptosis of polymorphonuclear leukocytes (PMNLs) and the expression of CD11b, leading to a systemic inflammatory response in ESRD patients [41]. Low HDL-C levels result in a reduction in antioxidation, which exacerbates the damage of infection [42]. Low HDL-C levels alone were insufficient to be an independent risk factor for frequent PDAP in our study. This can be since dyslipidemia in PD patients is a complicated process. Disorders of TG, CHOL, and LDL-C are a part of the pathological process of PDAP. The linkage between dyslipidemia and PD is fraught with controversy and uncertainty. As a result, more investigation is necessary to determine how dyslipidemia impacts the prognosis of peritonitis. C-reactive protein (CRP) is a sharp temporal reactive protein compounded by hepatocytes. A persistent increase in CRP indicates that the organism may be experiencing chronic inflammation [43]. Previous research has demonstrated that CRP can be influential in predicting cardiovascular mortality in PD patients [13]. According to retrospective research involving 402 PD patients, for every 1 mg/L increase in ultrasensitive CRP levels, the chance of mortality increased by 1.4% [44]. However, infection, nutritional status, and metabolic health all impact CRP. Therefore, the predictive value of CRP in PDAP patients is debatable. Inflammation severity and anti-inflammatory factors are represented by HDL-C and CRP. The balance of anti-inflammatory and pro-inflammatory factors in the body can be reflected by CRP/HDL-C. In contrast to HDL-C and CRP alone, it can more accurately depict the overall degree of inflammation in PD patients. HDL-C/CRP has been shown to reflect the severity of chronic kidney disease and to be predictive of its progression [45]. No research has examined the correlation between SII, CRP/HDL-C, and frequent PDAP with sizable sample sizes. Therefore, massive sample sizes and longer follow-up dates are still required to validate the study’s findings further.
Our research finds that diabetes mellitus increased the incidence of frequent PDAP (p = 0.022), although it was not an independent risk factor. DM has been reported to impair the immunity of peritoneal defenses, such as leukocyte adhesion, chemotaxis, and phagocytosis. Additionally, DM prevents phagocytes from entering the peritoneal cavity and decreases the phagocytic activity of peritoneal macrophages already there [46]. Diabetes increased all-cause mortality in PDAP patients, according to the multicenter retrospective cohort study [47]. According to several pieces of research, DM and low HDL-C levels enhance the likelihood that PDAP may occur [39]. Additionally, some PD patients with diabetes and diabetic retinopathy have an improper peritoneal fluid exchange. The procedure could fail as a result of manipulation problems caused by this. According to our research, the organisms that cause PDAP are more frequently distributed by Gram-positive bacteria. A study found that the Staphylococcus epidermidis that causes PDAP has weak immunogenicity, making it simpler to spread infection because the immune system finds it difficult to recognize it [48]. Staphylococcus epidermidis is mainly seen in contact with contaminated cases, and the finding that the rate of staphylococcal infection in patients in the frequent PDAP group was lower may be related to the fact that the center has strengthened the education on PD care recently, improved the quality of training in aseptic technique for patients, and paid more attention to the prevention of PDAP and optimized the follow-up system.
Limitations of this study are worth noting: (1) Because the study was designed as an observational study, we could not establish a causal relationship between SII, CRP/HDL-C levels, and the likelihood of frequent PDAP events. Additionally, we were unable to rule out the possibility of residual confounding. (2) Because the statistical analysis was based on a single laboratory parameter measurement, it is not possible that the association to remain stable over time. (3) This trial did not specifically document the precise number of episodes of peritonitis in patients with frequent PDAP during a year. (4) This experiment does not further explore the potential reasons of this event.
Conclusions
In conclusion, our research indicates that SII and CRP/HDL-C are independently attributed to a higher risk of frequent PDAP. SII and CRP/HDL-C are practical and affordable parameters that could serve as novel indicators for patients with repeated episodes of peritonitis. This finding needs further studies to elucidate the potential mechanisms linking SII and CRP/HDL-C to frequent PDAP.
Data availability
The data analyzed during this study are included in this published article.
Abbreviations
- CKD:
-
Chronic kidney disease
- ESRD:
-
end-stage renal disease
- PDAP:
-
peritoneal dialysis-associated peritonitis
- LDL:
-
low-density lipoprotein
- HDL:
-
high-density lipoprotein
- PTH:
-
parathyroid hormone
- SII:
-
platelet count × neutrophils/lymphocytes
- NLR:
-
neutrophil/lymphocyte ratio
- PLR:
-
platelet/lymphocyte count
- CRP:
-
C-reactive protein
References
Quintaliani G, Reboldi G, Di Napoli A, Nordio M, Limido A, Aucella F, et al. Exposure to novel coronavirus in patients on renal replacement therapy during the exponential phase of COVID-19 pandemic: survey of the Italian Society of Nephrology. J Nephrol. 2020;33(4):725–36.
Li PK, Chow KM, Van de Luijtgaarden MW, Johnson DW, Jager KJ, Mehrotra R, et al. Changes in the worldwide epidemiology of peritoneal dialysis. Nat Rev Nephrol. 2017;13(2):90–103.
Boudville N, Kemp A, Clayton P, Lim W, Badve SV, Hawley CM, et al. Recent peritonitis associates with mortality among patients treated with peritoneal dialysis. J Am Soc Nephrol. 2012;23(8):1398–405.
Szeto CC, Li PK. Peritoneal Dialysis-Associated Peritonitis. Clin J Am Soc Nephrol. 2019;14(7):1100–5.
Htay H, Cho Y, Pascoe EM, Darssan D, Nadeau-Fredette AC, Hawley C, et al. Multicenter Registry Analysis of Center Characteristics Associated with technique failure in patients on Incident Peritoneal Dialysis. Clin J Am Soc Nephrol. 2017;12(7):1090–9.
Jagirdar RM, Bozikas A, Zarogiannis SG, Bartosova M, Schmitt CP, Liakopoulos V. Encapsulating peritoneal sclerosis:pathophysiology and current treatment options. Int J Mol Sci. 2019;20(22):5765. Published 2019 November 16.
Burke M, Hawley CM, Badve SV, McDonald SP, Brown FG, Boudville N, et al. Relapsing and recurrent peritoneal dialysis-associated peritonitis: a multicenter registry study. Am J Kidney Dis. 2011;58(3):429–36.
Chung MC, Yu TM, Wu MJ, Chuang YW, Muo CH, Chen CH, et al. Impact of peritoneal dialysis-related peritonitis on PD discontinuation and mortality: a population-based national cohort study. Perit Dial Int. 2022;42(2):194–203.
He P, He LJ, Huang C, Hu JP, Sun SR. Neutrophil-to-lymphocyte ratio and treatment failure in Peritoneal Dialysis-Associated Peritonitis. Front Med (Lausanne). 2021 July;26:8:699502.
Jia L, Li C, Bi X, Wei F, Meng J, Sun G, et al. Prognostic value of systemic Immune-inflammation index among critically ill patients with acute kidney Injury: a retrospective cohort study. J Clin Med. 2022 July;8(14):3978.
Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The platelet-to-lymphocyte ratio as an inflammatory marker in Rheumatic diseases. Ann Lab Med. 2019;39(4):345–57.
Zhu M, Chen L, Kong X, Wang X, Li X, Fang Y, et al. The systemic Immune-inflammation index is an independent predictor of survival in breast Cancer patients. Cancer Manag Res. 2022;14:775–820.
Wang AY, Woo J, Lam CW, Wang M, Sea MM, Lui SF, et al. Is a single time point C-reactive protein predictive of outcome in peritoneal dialysis patients? J Am Soc Nephrol. 2003;14(7):1871–9.
Holzer M, Schilcher G, Curcic S, Trieb M, Ljubojevic S, Stojakovic T, et al. Dialysis modalities and HDL composition and function. J Am Soc Nephrol. 2015;26(9):2267–76.
Lin T, Xia X, Yu J, Qiu Y, Yi C, Lin J, et al. The predictive study of the relation between elevated low-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio and mortality in peritoneal dialysis. Lipids Health Dis. 2020;19(1):51.
Zhan X, Yang M, Zhou R, Wei X, Chen Y, Chen Q. Triglyceride to high-density lipoprotein cholesterol ratio is associated with increased mortality in older patients on peritoneal dialysis. Lipids Health Dis. 2019;18(1):199. Published 2019 November 15.
Li Y, Zhang Y, Lu R, Dai M, Shen M, Zhang J, et al. Lipid metabolism changes in patients with severe COVID-19. Clin Chim Acta. 2021;517:66–73.
Yuan J, Yang YQ, Liu L. Relationship between platelet/lymphocyte ratio and frequent peritoneal dialysis-associated peritonitis in peritoneal dialysis patients[J]. Chin J Nephrol 2021,37(4):327–32.
Li PK, Szeto CC, Piraino B, de Arteaga J, Fan S, Figueiredo AE, et al. ISPD Peritonitis recommendations: 2016 update on Prevention and Treatment. Perit Dial Int. 2016;36(5):481–508.
Perl J, Fuller DS, Bieber BA, Boudville N, Kanjanabuch T, Ito Y, et al. Peritoneal Dialysis-related infection rates and outcomes: results from the peritoneal Dialysis outcomes and practice patterns study (PDOPPS). Am J Kidney Dis. 2020;76(1):42–53.
Hung SC, Lai YS, Kuo KL, Tarng DC. Volume overload and adverse outcomes in chronic kidney disease: clinical observational and animal studies. J A-m Heart Assoc. 2015;4:e001918.
Obi Y, Qader H, Kovesdy CP, Kalantar-Zadeh K. Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr Opin Clin Nutr Metab Care. 2015;18:254–62.
Kalantar-Zadeh K, Ikizler TA, Block G, Avram MM, Kopple JD. Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis. 2003;42(5):864–81.
Sarnak MJ. Cardiovascular complications in chronic kidney disease. Am J Kidney Dis. 2003;41:11–7.
Qiao Yumeng X. Xiao, Dong Jie. Impact of systemic and local inflammation on clinical prognosis after recovery from peritoneal dialysis-associated peritonitis[J]. Chin J Nephrol 2022,38(6):567–71.
Lam MF, Leung JC, Lo WK, Tam S, Chong MC, Lui SL, et al. Hyperleptinaemia and chronic inflammation after peritonitis predicts poor nutritional status and mortality in patients on peritoneal dialysis. Nephrol Dial Transpl. 2007;22(5):1445–50.
Bellón T, Martínez V, Lucendo B, del Peso G, Castro MJ, Aroeira LS, et al. Alternative activation of macrophages in human peritoneum: implications for peritoneal fibrosis. Nephrol Dial Transpl. 2011;26(9):2995–3005.
Maraj M, Kuśnierz-Cabala B, Dumnicka P, Gala-Błądzińska A, Gawlik K, Pawlica-Gosiewska D, et al. Malnutrition, inflammation, atherosclerosis syndrome (MIA) and Diet recommendations among End-Stage Renal Disease patients treated with maintenance hemodialysis. Nutrients. 2018;10(1):69.
Jang HR, Rabb H. Immune cells in experimental acute kidney injury. Nat Rev Nephrol. 2015;11(2):88–101.
van der Meijden PEJ, Heemskerk JWM. Platelet biology and functions: new concepts and clinical perspectives. Nat Rev Cardiol. 2019;16(3):166–79.
Kertai MD, Zhou S, Karhausen JA, Cooter M, Jooste E, Li YJ, et al. Platelet counts, Acute kidney Injury, and mortality after coronary artery bypass grafting surgery. Anesthesiology. 2016;124(2):339–52.
Tang Y, Zeng X, Feng Y, Chen Q, Liu Z, Luo H, et al. Association of systemic Immune-inflammation index with short-term mortality of congestive heart failure: a retrospective cohort study. Front Cardiovasc Med. 2021;8:753133.
Xu M, Chen R, Liu L, Liu X, Hou J, Liao J, et al. Systemic immune-inflammation index and incident cardiovascular diseases among middle-aged and elderly Chinese adults: the Dongfeng-Tongji cohort study. Atherosclerosis. 2021;323:20–9.
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–22.
Chen JH, Zhai ET, Yuan YJ, Wu KM, Xu JB, Peng JJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017;23(34):6261–72.
Jiang H, Li D, Xu T, Chen Z, Shan Y, Zhao L, et al. Systemic Immune-inflammation index predicts contrast-Induced Acute kidney Injury in patients undergoing coronary angiography: a cross-sectional study. Front Med (Lausanne). 2022;9:841601.
Öztürk ZA, Yesil Y, Kuyumcu ME, Bilici M, Öztürk N, Yeşil NK, et al. Inverse relationship between neutrophil lymphocyte ratio (NLR) and bone mineral density (BMD) in elderly people. Arch Gerontol Geriatr. 2013 Jul-Aug;57(1):81–5.
Lu X, Wang S, Zhang G, Xiong R, Li H. High neutrophil-to-lymphocyte ratio is a significant predictor of Cardiovascular and all-cause mortality in patients undergoing peritoneal Dialysis. Kidney Blood Press Res. 2018;43(2):490–9.
Zhang R, Zhang X, Tang X, Tang L, Shang S, Wang X, et al. The association between diabetes coexisting with low levels of high-density lipoprotein cholesterol and peritoneal dialysis-related peritonitis. Diabetol Metab Syndr. 2022;14(1):60.
Groenen AG, Halmos B, Tall AR, Westerterp M. Cholesterol efflux pathways, inflammation, and atherosclerosis. Crit Rev Biochem Mol Biol. 2021;56(4):426–39.
Raupachova J, Kopecky C, Cohen G. High-density lipoprotein from chronic kidney Disease patients modulates polymorphonuclear leukocytes. Toxins (Basel). 2019;11(2):73.
Tanaka S, Couret D, Tran-Dinh A, Duranteau J, Montravers P, Schwendeman A, et al. High-density lipoproteins during sepsis: from bench to bedside. Crit Care. 2020;24(1):134.
Carrero JJ, Stenvinkel P. Persistent inflammation as a catalyst for other risk factors in chronic kidney disease: a hypothesis proposal. Clin J Am Soc Nephrol. 2009;4(Suppl 1):49–55.
Liu SH, Li YJ, Wu HH, Lee CC, Lin CY, Weng CH, et al. High-sensitivity C-reactive protein predicts mortality and technique failure in peritoneal dialysis patients. PLoS ONE. 2014;9(3):e93063.
Tang Leile G, Xinghua, Li Shaomin. The predictive role of high-density lipoprotein to C-reactive protein ratio on the progression of non-dialysis chronic kidney disease[J]. J Sun Yat-sen Univ (Medical Sciences). 2022;43(2):305–15.
Chow KM, Szeto CC, Leung CB, Kwan BC, Law MC, Li PK. A risk analysis of continuous ambulatory peritoneal dialysis-related peritonitis. Perit Dial Int. 2005;25(4):374–9.
Meng LF, Yang LM, Zhu XY, Zhang XX, Li XY, Zhao J, et al. Comparison of clinical features and outcomes in peritoneal dialysis-associated peritonitis patients with and without diabetes: a multicenter retrospective cohort study. World J Diabetes. 2020 October;15(10):435–46.
Jung K, Lüthje P, Lundahl J, Brauner A. Low immunogenicity allows Staphylococcus epidermidis to cause PD peritonitis. Perit Dial Int. 2011 Nov-Dec;31(6):672–8.
Acknowledgements
The author thanks the patients and doctors who participated in the research.
Funding
This work is supported by a grant from Wuxi Medical Innovation Team Project (CXTD2021010), Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (HB2023009), and Cohort and Clinical Research Program of Wuxi Medical Center, Nanjing Medical University(WMCC202316).
Author information
Authors and Affiliations
Contributions
JT contributed significantly to analysis and manuscript; DXW and YC performed the data analyses; JHF helped perform the analysis with constructive discussions. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the the Hospital Committee of Xuzhou Medical University approved this study in 2022. The ethical approval number is XYFY2022-KL218. Informed consent was obtained from all study participants. Legally Authorized Representatives of illiterate participants provided informed consent for the study. The study was conducted following the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
No conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tang, J., Wang, D., Chen, Y. et al. The association between new inflammation markers and frequent peritoneal dialysis-associated peritonitis. BMC Nephrol 25, 81 (2024). https://doi.org/10.1186/s12882-024-03496-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03496-z