Abstract
Background
Gastric cancer is one of the four most common cancer that causing death worldwide. Genome-Wide Association Studies (GWAS) have shown that genetic diversities MUC1 (Mucin 1) and PSCA (Prostate Stem Cell Antigen) genes are involved in gastric cancer. The aim of this study was avaluating the association of rs4072037G > A polymorphism in MUC1 and rs2294008 C > T in PSCA gene with risk of gastric cancer in northern Iran.
Methods
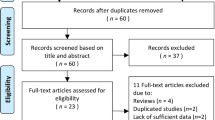
DNA was extracted from 99 formalin fixed paraffin-embedded (FFPE) tissue samples of gastric cancer and 96 peripheral blood samples from healthy individuals (sex matched) as controls. Two desired polymorphisms, 5640G > A and 5057C > T for MUC1 and PSCA genes were genotyped using PCR-RFLP method.
Results
The G allele at rs4072037 of MUC1 gene was associated with a significant decreased gastric cancer risk (OR = 0.507, 95% CI: 0.322–0.799, p = 0.003). A significant decreased risk of gastric cancer was observed in people with either AG vs. AA, AG + AA vs. GG and AA+GG vs. AG genotypes of MUC1 polymorphism (OR = 4.296, 95% CI: 1.190–15.517, p = 0.026), (OR = 3.726, 95% CI: 2.033–6.830, p = 0.0001) and (OR = 0.223, 95% CI: 0.120–0.413, p = 0.0001) respectively. Finally, there was no significant association between the PSCA 5057C > T polymorphism and risk of gastric cancer in all genetic models.
Conclusion
Results indicated that the MUC1 5640G > A polymorphism may have protective effect for gastric cancer in the Northern Iran population and could be considered as a potential molecular marker in gastric cancer.
Similar content being viewed by others
Background
Gastric cancer is the fourth most common cancer worldwide and the second leading cause of cancer-related death [1]. The prevalence of gastric cancer varies among different geographic populations around the world [2]. More than 70% of deaths from stomach cancer occur in developing countries [3, 4]. Northern and northwestern regions of Iran are at high risk for gastric cancer [2]. In addition, the mortality rate from stomach cancer is the first cause of death due to cancer in both sexes in Iran [5, 6]. From 2000 to 2005, the incidence rate was highest in northern Provinces, including Mazandaran, Golestan, and Ardabil [2]. It is believed that different environmental risk factors like alcohol consumption, smoking habits, diet and infectious agents (Helicobacter pylori) are involved in the development of gastric cancer [7,8,9], but a genetic predisposition to stomach cancer is unknown yet. Previous studies suggested an association between MUC1 and stomach [10], colon [11], lung [12], ovarian [13], breast [14], pancreas [15], and thyroid cancers [16]. In addition, Genome-Wide Association Studies (GWAS) proposed genetic diversities like rs4072037G > A (5640G > A) in MUC1 gene and rs2294008C > T (5057C > T) polymorphisms in PSCA (Prostate Stem Cell Antigen) gene as genetic risk factors in gastric cancer [17].
MUC1 (Mucin 1) gene is located on chromosome 1q21 and includes seven exons [18]. This gene encodes a membrane-bound glycoprotein with the transmembrane domain, which is attached to the upper surface of the gastrointestinal epithelium. It plays important roles in protecting epithelial surfaces against external agents [19, 20]. MUC1 protein in tumor cells or tumor-associated MUC1 (TA-MUC1) differs from MUC1 expressed in normal cells, with regard to its cellular distribution, biochemical features, and function. TA-MUC1 is hypoglycosylated and overexpressed in a variety of cancers, which plays a crucial role in progression of the disease [21]. It is believed that hypoglycosylation may potentiate MUC1 oncogenic signaling by decreasing its cell surface levels and increasing intracellular accumulation [21, 22].
PSCA gene is located on chromosome 8q24.3, which encodes a glycosylphosphatidyl inositol (GPI)-anchored protein with 114 amino acids. PSCA gene product has important role in proliferation, cell adhesion, and survival [23, 24]. PSCA is expressed in the epithelial cells of the bladder, stomach, kidney, skin, and esophagus. The function of PSCA in normal cells and carcinogenesis is not clearly known [25]. Several reports indicated that PSCA is associated with various cancers, such as prostate [26], bladder [27], and pancreatic cancer [28]. PSCA is up-regulated in the prostate, and pancreas cancers, while in the esophagus and stomach cancers it is down-regulated [29]. 5057C > T is a missense single nucleotide polymorphism (SNP) in 5′-UTR region of PSCA. This polymorphism leads to changes in transcriptional activity in the upstream regions of PSCA gene [30]. The C allele changes the initiation codon from ATG to the alternative start codon ACG (threonine instead of methionine) and leads to a truncated protein lacking nine amino acids from the N-terminus of PSCA protein. This alteration changes the protein folding and impairs intracellular processes [31].
The aim of this study is also evaluating the association between MUC1 gene polymorphism, rs4072037G > A and PSCA gene polymorphism rs2294008C > T with gastric cancer in northern Iran.
Methods
The study population
Ninety nine formalin fixed paraffin-embedded (FFPE) tissue samples (64 males and 35 females, average age 67.5 ± 10.9) were collected from gastric cancer patients who referred to the pathology department of the Sari Imam Khomeini hospital from 2009 to 2016 (Table 1) (Mazandaran Province). Tumor characteristics of the patients are summarized in Table 2. In addition, 96 blood samples were collected as control from healthy individuals (57 males and 39 females, average age 34.3 ± 7.0) who referred to Novin genetics laboratory of Sari for other reasons except gastric diseases (Table 1). The normal control individuals were not age-matched with patients, but they were selected randomly to find the allele/genotype frequency of the polymorphisms in the local population. Blood samples were collected in EDTA containing tubes and preserved at − 20 °C. This research was approved by the ethics committee in the Mazandaran University of Medical Sciences.
DNA extraction
To extracting DNA from paraffin-embedded tissues, a "YTA Genomic DNA Extraction mini kit (Yekta Tajhiz Azma, Iran) was used. Also a standard salting out methods was applied to extract DNA from blood samples, respectively. Finally, the extracted DNA was maintained at − 20 °C until it’s used for further study.
Genotyping using PCR-RFLP method
PCR (Polymerase chain reaction) was applied to amplify exon 2 of MUC1 and 5′-UTR region of PSCA genes, including desired polymorphisms using specific primers (Table 3). Each reaction consists of 2 μl template DNA, 11 μl ready 2x PCR master mix RED (Ampliqon, Denmark), 11 μl distilled water, 0.5 μl of each primer at 25 μM, in a total volume of 25 μl. The PCR reactions were carried out under the following conditions: 94 °C for 5 min, followed by 35 cycles 94 °C for 60 s; 72 °C for 60 s. The annealing temperature of 60 °C for 60 s was used for MUC1 gene and 56 °C for 60 s used for PSCA gene. PCR products were visualized on 1% agarose gel containing SYBR Safe staining. Then, PCR products were subjected to restriction digestion using 6 μl of the PCR products and five units of restriction enzyme. Briefly, 188 bp PCR fragment of the MUC1 gene was digested using AIWNI enzyme; a homozygous GG allele remained uncut, homozygous AA genotype was digested into 114 and 74 bp fragments, and heterozygous GA produced three fragments, 118, 114 and 74 bp, respectively (Fig. 1, a). Also, 139 bp PCR fragment of the PSCA gene was digested using a NIaIII restriction enzyme, genotype TT was digested to 2 fragments, 101 and 38 bp, genotype CC remained uncut and heterozygous CT showed three fragments, 139, 101 and 38 bp, respectively (Fig. 1, b).
3% agarose gel electrophoresis of the restriction enzyme digestion (a) 188 bp PCR fragment of the MUC1 gene restriction enzyme digestion results using AIWNI enzyme; lane 1 and 3 shows homozygous AA, lane 2 heterozygous GA genotype and lane 4 shows homozygous GG genotype respectively, lane 5 shows 100 bp DNA marker (b) Restriction enzyme map of the 139 bp PCR fragment of the PSCA gene using NIaIII enzyme. Lane 1 = 100 bp DNA marker, lane 2 heterozygous CT, lane 3 (101 and 39 bp) shows homozygous TT and lane 4, uncut PCR product shows homozygous CC genotype respectively
Statistical analysis
The statistical analysis was performed using the SPSS Statistics software (SPSS, Chicago, IL, USA). Different statistical analyses were applied to evaluate the data achieved in this study including Chi-Squre for distributions of demographic characteristics, a logistic regression model for the odds ratio (OR) and confidence interval (CI), respectively. A p-value < 0.05 was considered statistically significant. The Hardy–Weinberg equilibrium also was applied to evaluate the frequency of control genotypes against the patient’s samples.
Results
Demographic and clinical information of 99 patients with gastric cancer and 96 controls are shown in Tables 1 and 2, respectively. Ninety nine patient samples were genotyped for PSCA gene (rs2294008) and 91 patient samples for MUC1 gene (rs4072037) polymorphism. Genotype and allele frequencies of rs4072037 and rs2294008 and their associations with the risk of gastric cancer are presented in Tables 4 and 5, respectively.
The G allele frequency of rs4072037 is 64% in patients with gastric cancer compared with 78% in controls, respectively (Table 4). MUC1 rs4072037 polymorphism is associated with significant decreased gastric cancer risk in four genetic models: G vs. A (OR = 0.507, 95% CI: 0.322–0.799, p = 0.003); heterozygous AG compared with AA (OR = 4.296, 95% CI: 1.190–15.517, p = 0.026); dominant model AG + AA vs. GG (OR = 3.726, 95% CI: 2.033–6.830, p = 0.0001); and over-dominant model AA+GG vs. G (OR = 0.223, 95% CI: 0.120–0.413, p = 0.0001) (Table 4).
In the current study, no significant association was observed between the PSCA 5057C > T polymorphism and risk of gastric cancer in all genetic models (T vs. C (OR = 1.050, 95% CI: 0.652–1.693, p = 0.840); homozygous TT vs. CC (OR = 0.903, 95% CI: 0.327–2.492, p = 0.533); heterozygous CT vs. CC (OR = 1.228, 95% CI: 0.644–2.339, p = 0.533); dominant model CT + CC vs. TT (OR = 1.137, 95% CI: 0.420–3.080, p = 0.800); and recessive model CC vs. CT + TT (OR = 0.904, 95% CI: 0.505–1.620, p = 0.735)). As a result, There was no statistically significant differences between the genotype and allele frequency of PSCA (5057C > T) in cases and controls in this study (Table 5).
Furthermore, the result of interaction effects between MUC1 (rs4072037) and PSCA (rs2294008) genotypes with gender is summarized in Table 6.
Discussion
Different previous study demonstrated a decrease incidence in gastric cancer in the world, but it is still one the most frequent cancer in the northern part of Iran [2]. Mazandaran, Golestan, and Ardabil Provinces are high-risk for gastric cancer [2, 32]. Gastric cancer is a multi-factorial disease; a high dietary intake of salt, the high prevalence of Helicobacter pylori (H. pylori) infection, smoking and gastroesophageal reflux disease are the environmental factors in the pathogenesis of this disease in Iran [2, 9]. Among genetic risk factors, MUC1 (5640G > A) and PSCA (5057C > T) polymorphisms were reported in several studies earlier [33,34,35,36].
MUC1 is a large glycoprotein, which is produced at the apical surface as a transmembrane mucin in most simple epithelia including stomach. MUC1 protein functions are associated with mucins such as hydration of cell surfaces, degradative enzymes, lubrication and protection from microorganisms [37]. MUC1 protein contains three different domains: a large extracellular, transmembrane and a short cytoplasmic domain. The MUC1 gene in human is comprised of 7 exons that can be alternatively spliced to form different transcripts [37]. At least twelve splice variants of MUC1 have been described [38]. The SNP rs4072037G > A (5640 G > A) located in the 5′ side of the exon 2 and it is a splicing acceptor site, which produces two different MUC1 transcripts. The “G” allele determines MUC1/B or the variant type 2 and contains the first 27 bp of the exon 2. The “A”allele produce MUC1/A or variant type 3 that have 9 amino acid shorter in the N-terminal domain compared with “G”allele [39,40,41].
This additional sequence is potentially changing its intracellular trafficking or subsequent processing. The impact of the nine additional amino acids of MUC1/A on the signaling functions and intracellular localization was investigated by Imbert-Fernandez and colleagues [41]. They showed that COS-7 cell line transfected by plasmid containing MUC1/A or MUC1/B had similar protein expression and plasma membrane localization. This study also showed MUC1/B and MUC1/A differs in their ability to modulate tumor necrosis α (TNFα)-induced transcription of IL-1β and IL-8, inducing the basal TGFβ expression; finally they show different inflammatory activities [41].
MUC1 protein could work as a physical barrier and protect the gastric epithelial cells from H. pylori by inhibiting its binding to the epithelial cells. The carriers of the short-short (SS) homozygous variant genotype, were at a high risk of H. pylori infection, compared to the carriers of the long-long (LL) and long-short (LS) genotypes of MUC1 variable number of tandem repeats (VNTR) [42]. One of the previous study (Miao Li et al., 2013), tested the relation between three polymorphisms (rs4072037 at 1q22, rs13361707 at 5p13, and rs2274223 at 10q23) involved in the increase risk of gastric cancer due to the inflammatory response and H. pylori infection [43]. They reported that people infected by H. pylori, carrying the genotypes AA rs4072037, CT/CC rs13361707 and AG/GG rs2274223 showed an increased risk of gastric cancer [43].
Different studies (Hanze Zhang et al., 2011, J Kupcinskas et al., 2014) have shown that the G allele locus on rs4072037 was significantly associated with a decreased gastric cancer risk [35, 44]. Xinyang Liu et al., 2014 suggested the G allele at rs4072037 of the MUC1 gene might have a protective rule in people from Asian countries against gastric cancer. Also, they reported that the association was more prevalent in Asian population than in Caucasians [45].
In this study, allelic comparison (G vs. A), genotype comparison (GA vs. AA; GG vs. AA), were done and dominant model (AG + AA vs. GG), recessive model (AA vs. AG + GG), over-dominant model (AA+GG vs. AG) was tested [46]. We found that in this study, the rs4072037 AG genotype was significantly associated with the reduced risk of gastric cancer or it plays a protecting role [odds ratios (OR) = 4.296; 95% confidence interval (CI) = 1.190–15.517, p = 0.026 for AG vs. AA].
A study by Hye-Rim Song et al., 2014, with 3245 GC cases and 700 controls suggests that the rs4072037 AG genotype was significantly associated with a reduced risk of gastric cancer [odds ratios (OR) = 0.78; 95% confidence interval (CI) = 0.67–0.91 for AG vs. AA]. They showed an association between the rs4072037 G allele and a reduced risk of gastric cancer [47]. In the other meta-analysis study, with 12,551 cases and 13,436 controls in total from seventeen different case–control studies, suggests different genetic combination (G vs. A; AG vs. AA; GG vs. AA; AG + GG vs. AA) for the MUC1 rs4072037 polymorphism might decrease the risk of gastric cancer [48]. Also in this study, comparison of the people by ethnicity and the risk of gastric cancer along with the frequency of G allele showed a decrease among Asian population [48].
Another similar study (including 4220 cases and 6384 controls) by Duan F et al., 2014 also evaluated the association between the MUC1 rs4072037 polymorphism and susceptibility to the cancer [49]. Their study demonstrated that the MUC1 (rs4072037) polymorphism is associated with risk of cancer in all genetic models (G vs. A; GA vs. AA; GG vs. AA; AG + AA vs. GG; GG vs. AG + AA). They suggested MUC1 (rs4072037) polymorphism slightly decreased risk of gastric cancer among Asian population, and this was associated with decreased risk with different genotypes except for homozygous recessive (AA) in Caucasian population [49].
In this study, MUC1 rs4072037 polymorphism was significantly associated with a decreased risk of cancer in all genetic models except for homozygous GG vs. AA and recessive model AG + GG vs. AA (G vs. A: OR = 0.507, 95% CI: 0.322–0.799, p = 0.003; AG vs. AA: OR = 4.296, 95% CI: 1.190–15.517, p = 0.026; AG + AA vs. GG: OR = 3.726, 95%CI: 2.033–6.830, p = 0.0001; AA+GG vs. AG: (OR = 0.223, 95% CI: 0.120–0.413, p = 0.0001)). Data from this case-control study indicated that four genetic models G vs. A, heterozygous GA (GA vs. AA), dominant (AG + AA vs. GG), over-dominant model (AA+GG vs. AG), were significantly associated with the decreased risk of cancer. Therefore, MUC1 rs4072037 polymorphism was associated with decreased risk of gastric cancer in northern Iran.
The Prostate Stem Cell Antigen (PSCA) is expressed in the gastric epithelium of the isthmus area. This area includes immature epithelial cells. PSCA expression increases in prostate cancer but it is reduced in gastric cancer and gastric intestinal metaplasia [50, 51]. T allele carriers show lower transcriptional activity compared with the C allele carriers (5057C > T) in their gastric mucosa [31, 50]. T allele carriers have nine amino acids more than C allele carriers (natural protein of 114 amino acid residues) [52]. The association of PSCA (5057C > T) variant was described in Korea and Japan population for the first time and the T allele was reported as a risk factor for gastric cancer [31]. A study in Japan and Korea showed that 5057 T allele plays a more significant role in diffuse gastric cancer compared with the intestinal gastric cancer [31, 53]. Such results were also similar in the population of Poland and the United States [34]. Other studies in Caucasian and Chinese population also confirmed that this polymorphism is a risk factor for diffuse and intestinal gastric cancer [54].
In this study, PSCA rs2294008 polymorphism was not significantly associated with an increased risk of cancer in all genetic models (T vs. C (OR = 1.050, 95% CI: 0.652–1.693, p = 0.840); homozygous TT vs. CC (OR = 0.903, 95% CI: 0.327–2.492, p = 0.533); heterozygous CT vs. CC (OR = 1.228, 95% CI: 0.644–2.339, p = 0.533); dominant model CT + CC vs. TT (OR = 1.137, 95% CI: 0.420–3.080, p = 0.800); and recessive model CC vs. CT + TT (OR = 0.904, 95% CI: 0.505–1.620, p = 0.735) (Table 5). Therefore, PSCA rs2294008 polymorphism was not associated with increased risk of gastric cancer in Northern Iran.
Conclusion
In conclusion, this study evaluated the effect of MUC1 (rs4072037) and PSCA (rs2294008) polymorphisms on GC risk in the Northern Iran population. Data from this study revealed that the MUC1 rs4072037 polymorphism was significantly associated with decreased risk of gastric cancer. However, the results could be important, especially for the interpretation of a genetic variant, which cause susceptibility to gastric cancer, and could be used as diagnostic markers in gastric cancer. In addition, PSCA polymorphism did not show any relation to gastric cancer in our findings probably because of the type of gastric cancer or the small sample size.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the author for correspondence upon reasonable request.
Abbreviations
- GWAS:
-
Genome-Wide Association Studies
- MUC1:
-
Mucin 1
- PSCA:
-
Prostate Stem Cell Antigen
- FFPE:
-
Formalin fixed paraffin-embedded
- TA-MUC1:
-
tumor-associated MUC1
- GPI:
-
Glycosylphosphatidyl inositol
- SNP:
-
Single nucleotide polymorphism
- PCR:
-
Polymerase chain reaction
- RFLP:
-
Restriction fragment length polymorphism
- H. pylori :
-
Helicobacter pylori
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Malekzadeh R, Derakhshan MH, Malekzadeh Z. Gastric cancer in Iran: epidemiology and risk factors. Arch Iran Med. 2009;12(6):576–83.
Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46(4):765–81.
Wang T, Zhang L, Li H, Wang B, Chen K. Prostate stem cell antigen polymorphisms and susceptibility to gastric cancer: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev. 2012;21(5):843–50.
Derakhshan MH, Yazdanbod A, Sadjadi AR, Shokoohi B, McColl KE, Malekzadeh R. High incidence of adenocarcinoma arising from the right side of the gastric cardia in NW Iran. Gut. 2004;53(9):1262–6.
Almasi Z, Rafiemanesh H, Salehiniya H. Epidemiology characteristics and trends of incidence and morphology of stomach cancer in Iran. Asian Pac J Cancer Prev. 2015;16(7):2757–61.
McLean MH, El-Omar EM. Genetics of gastric cancer. Nat Rev Gastroenterol Hepatol. 2014;11(11):664–74.
Mocellin S, Verdi D, Pooley KA, Nitti D. Genetic variation and gastric cancer risk: a field synopsis and meta-analysis. Gut. 2015;64(8):1209–19.
Pourfarzi F, Whelan A, Kaldor J, Malekzadeh R. The role of diet and other environmental factors in the causation of gastric cancer in Iran--a population based study. Int J Cancer. 2009;125(8):1953–60.
Bafna S, Kaur S, Batra SK. Membrane-bound mucins: the mechanistic basis for alterations in the growth and survival of cancer cells. Oncogene. 2010;29(20):2893–904.
Xu Q, Yuan Y, Sun LP, Gong YH, Xu Y, Yu XW, et al. Risk of gastric cancer is associated with the MUC1 568 a/G polymorphism. Int J Oncol. 2009;35(6):1313–20.
Szabo E. MUC1 expression in lung cancer. Methods Mol Med. 2003;74:251–8.
Dong Y, Walsh MD, Cummings MC, Wright RG, Khoo SK, Parsons PG, et al. Expression of MUC1 and MUC2 mucins in epithelial ovarian tumours. J Pathol. 1997;183(3):311–7.
Rahn JJ, Dabbagh L, Pasdar M, Hugh JC. The importance of MUC1 cellular localization in patients with breast carcinoma: an immunohistologic study of 71 patients and review of the literature. Cancer. 2001;91(11):1973–82.
Monges GM, Mathoulin-Portier MP, Acres RB, Houvenaeghel GF, Giovannini MF, Seitz JF, et al. Differential MUC 1 expression in normal and neoplastic human pancreatic tissue. An immunohistochemical study of 60 samples. Am J Clin Pathol. 1999;112(5):635–40.
Wreesmann VB, Sieczka EM, Socci ND, Hezel M, Belbin TJ, Childs G, et al. Genome-wide profiling of papillary thyroid cancer identifies MUC1 as an independent prognostic marker. Cancer Res. 2004;64(11):3780–9.
Abnet CC, Freedman ND, Hu N, Wang Z, Yu K, Shu XO, et al. A shared susceptibility locus in PLCE1 at 10q23 for gastric adenocarcinoma and esophageal squamous cell carcinoma. Nat Genet. 2010;42(9):764–7.
Zhang L, Vlad A, Milcarek C, Finn OJ. Human mucin MUC1 RNA undergoes different types of alternative splicing resulting in multiple isoforms. Cancer Immunol Immunother. 2013;62(3):423–35.
Gendler SJ. MUC1, the renaissance molecule. J Mammary Gland Biol Neoplasia. 2001;6(3):339–53.
Sun H, Wu X, Wu F, Li Y, Yu Z, Chen X, et al. Associations of genetic variants in the PSCA, MUC1 and PLCE1 genes with stomach cancer susceptibility in a Chinese population. PLoS One. 2015;10(2):e0117576.
Nath S, Mukherjee P. MUC1: a multifaceted oncoprotein with a key role in cancer progression. Trends Mol Med. 2014;20(6):332–42.
Altschuler Y, Kinlough CL, Poland PA, Bruns JB, Apodaca G, Weisz OA, et al. Clathrin-mediated endocytosis of MUC1 is modulated by its glycosylation state. Mol Biol Cell. 2000;11(3):819–31.
Ono H, Saeki N. Five Gastric Cancer-Susceptibility Loci Identified by Genome-Wide Association Studies. J Gastroint Dig Sys. 2013;S12(015):1–5.
Reiter RE, Gu Z, Watabe T, Thomas G, Szigeti K, Davis E, et al. Prostate stem cell antigen: a cell surface marker overexpressed in prostate cancer. Proc Natl Acad Sci U S A. 1998;95(4):1735–40.
Argani P, Rosty C, Reiter RE, Wilentz RE, Murugesan SR, Leach SD, et al. Discovery of new markers of cancer through serial analysis of gene expression: prostate stem cell antigen is overexpressed in pancreatic adenocarcinoma. Cancer Res. 2001;61(11):4320–4.
Moore ML, Teitell MA, Kim Y, Watabe T, Reiter RE, Witte ON, et al. Deletion of PSCA increases metastasis of TRAMP-induced prostate tumors without altering primary tumor formation. Prostate. 2008;68(2):139–51.
Wang S, Tang J, Wang M, Yuan L, Zhang Z. Genetic variation in PSCA and bladder cancer susceptibility in a Chinese population. Carcinogenesis. 2010;31(4):621–4.
Grubbs EG, Abdel-Wahab Z, Tyler DS, Pruitt SK. Utilizing quantitative polymerase chain reaction to evaluate prostate stem cell antigen as a tumor marker in pancreatic cancer. Ann Surg Oncol. 2006;13(12):1645–54.
Yang X, Guo Z, Liu Y, Si T, Yu H, Li B, et al. Prostate stem cell antigen and cancer risk, mechanisms and therapeutic implications. Expert Rev Anticancer Ther. 2014;14(1):31–7.
Dudek AM, Grotenhuis AJ, Vermeulen SH, Kiemeney LA, Verhaegh GW. Urinary bladder cancer susceptibility markers. What do we know about functional mechanisms? Int J Mol Sci. 2013;14(6):12346–66.
Study Group of Millennium Genome Project for C, Sakamoto H, Yoshimura K, Saeki N, Katai H, Shimoda T, et al. Genetic variation in PSCA is associated with susceptibility to diffuse-type gastric cancer. Nat Genet. 2008;40(6):730–40.
Mohebbi M, Mahmoodi M, Wolfe R, Nourijelyani K, Mohammad K, Zeraati H, et al. Geographical spread of gastrointestinal tract cancer incidence in the Caspian Sea region of Iran: spatial analysis of cancer registry data. BMC Cancer. 2008;8:137.
Song HR, Kim HN, Piao JM, Kweon SS, Choi JS, Bae WK, et al. Association of a common genetic variant in prostate stem-cell antigen with gastric cancer susceptibility in a Korean population. Mol Carcinog. 2011;50(11):871–5.
Lochhead P, Frank B, Hold GL, Rabkin CS, Ng MT, Vaughan TL, et al. Genetic variation in the prostate stem cell antigen gene and upper gastrointestinal cancer in white individuals. Gastroenterology. 2011;140(2):435–41.
Zhang H, Jin G, Li H, Ren C, Ding Y, Zhang Q, et al. Genetic variants at 1q22 and 10q23 reproducibly associated with gastric cancer susceptibility in a Chinese population. Carcinogenesis. 2011;32(6):848–52.
Kupcinskas J, Wex T, Link A, Bartuseviciute R, Dedelaite M, Kevalaite G, et al. PSCA and MUC1 gene polymorphisms are associated with gastric cancer and pre-malignant gastric conditions [corrected]. Anticancer Res. 2014;34(12):7167–75.
Brayman M, Thathiah A, Carson DD. MUC1: a multifunctional cell surface component of reproductive tissue epithelia. Reprod Biol Endocrinol. 2004;2:4.
Williams SJ, McGuckin MA, Gotley DC, Eyre HJ, Sutherland GR, Antalis TM. Two novel mucin genes down-regulated in colorectal cancer identified by differential display. Cancer Res. 1999;59(16):4083–9.
Ng W, Loh AX, Teixeira AS, Pereira SP, Swallow DM. Genetic regulation of MUC1 alternative splicing in human tissues. Br J Cancer. 2008;99(6):978–85.
Saeki N, Sakamoto H, Yoshida T. Mucin 1 gene (MUC1) and gastric-cancer susceptibility. Int J Mol Sci. 2014;15(5):7958–73.
Imbert-Fernandez Y, Radde BN, Teng Y, Young WW Jr, Hu C, Klinge CM. MUC1/a and MUC1/B splice variants differentially regulate inflammatory cytokine expression. Exp Eye Res. 2011;93(5):649–57.
Giraldi L, Michelazzo MB, Arzani D, Persiani R, Pastorino R, Boccia S. MUC1, MUC5AC, and MUC6 polymorphisms, helicobacter pylori infection, and gastric cancer: a systematic review and meta-analysis. Eur J Cancer Prev. 2018;27(4):323–30.
Li M, Huang L, Qiu H, Fu Q, Li W, Yu Q, et al. Helicobacter pylori infection synergizes with three inflammation-related genetic variants in the GWASs to increase risk of gastric cancer in a Chinese population. PloS one. 2013;8:9.
Kupcinskas J, Wex T, Link A, Bartuseviciute R, Dedelaite M, Kevalaite G, et al. PSCA and MUC1 gene polymorphisms are linked with gastric cancer and pre-malignant gastric conditions. Anticancer Res. 2014;34(12):7167–75.
Liu X, Wang Z, Zhang X, Chang J, Tang W, Gan L, et al. MUC1 gene polymorphism rs4072037 and susceptibility to gastric cancer: a meta-analysis. Springerplus. 2014;3(1):599.
Horita N, Kaneko T. Genetic model selection for a case–control study and a meta-analysis. Meta Gene. 2015;5:1–8.
Song H-R, Kim HN, Kweon S-S, Choi J-S, Shim HJ, Cho SH, et al. Common genetic variants at 1q22 and 10q23 and gastric cancer susceptibility in a Korean population. Tumor Biol. 2014;35(4):3133–7.
Gu X, Feng J, Liu L, Lu M, Ma X, Cao Y, et al. Association of MUC1 rs4072037 functional polymorphism and Cancer risk: evidence from 12551 cases and 13436 controls. J Cancer. 2018;9(18):3343.
Duan F, Song C, Dai L, Cui S, Zhang X, Zhao X. The effect of MUC1 rs4072037 functional polymorphism on cancer susceptibility: evidence from published studies. PLoS One. 2014;9(4):e95651.
Toyoshima O, Tanikawa C, Yamamoto R, Watanabe H, Yamashita H, Sakitani K, et al. Decrease in PSCA expression caused by helicobacter pylori infection may promote progression to severe gastritis. Oncotarget. 2018;9(3):3936–45.
Gu Z, Thomas G, Yamashiro J, Shintaku IP, Dorey F, Raitano A, et al. Prostate stem cell antigen (PSCA) expression increases with high Gleason score, advanced stage and bone metastasis in prostate cancer. Oncogene. 2000;19(10):1288–96.
Tanikawa C, Urabe Y, Matsuo K, Kubo M, Takahashi A, Ito H, et al. A genome-wide association study identifies two susceptibility loci for duodenal ulcer in the Japanese population. Nat Genet. 2012;44(4):430–4 S1-2.
Matsuo K, Tajima K, Suzuki T, Kawase T, Watanabe M, Shitara K, et al. Association of prostate stem cell antigen gene polymorphisms with the risk of stomach cancer in Japanese. Int J Cancer. 2009;125(8):1961–4.
Lu Y, Chen J, Ding Y, Jin G, Wu J, Huang H, et al. Genetic variation of PSCA gene is associated with the risk of both diffuse- and intestinal-type gastric cancer in a Chinese population. Int J Cancer. 2010;127(9):2183–9.
Acknowledgements
We would like to thank Mazandaran University of Medical Sciences for its financial support, and all the volunteers who participated in this study.
Funding
The current study was financially supported by Mazandaran University of Medical Sciences (Grant No. 2138). The funding bodies played no role either in the design of the study, data collection, analysis, interpretation of data, or in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
MBHS conceived and designed the study. RA performed the experiments. AT analyzed the data. MBHS and RA wrote and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of Mazandaran University of Medical Sciences and complied with the guidelines and principles of the Declaration. All participants signed written informed consent.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alikhani, R., Taravati, A. & Hashemi-Soteh, M.B. Association of MUC1 5640G>A and PSCA 5057C>T polymorphisms with the risk of gastric cancer in Northern Iran. BMC Med Genet 21, 148 (2020). https://doi.org/10.1186/s12881-020-01085-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12881-020-01085-z