Abstract
Background
Physical examinations may reveal the instability of a glenohumeral joint but cannot diagnose the bony Bankart lesions. Soft tissue Bankart lesion cannot be visualized on traditional radiogram. Magnetic resonance images have high cost and availability issues. The purpose of the study was to access the diagnostic performance of the Computed Tomography (CT) in the assessment of patients with shoulder instability and to diagnose the Bankart and bony Bankart lesions.
Methods
A total of 145 patients with shoulder instability were included in the study. Patients were subjected to clinical examination tests, traditional radiography, and CT. Two orthopedic surgeons, two engineers (trained in musculoskeletal imaging), and two physiotherapists have analyzed the radiological images, CT scans, and the clinical examination tests respectively. The Chi-square test or one-way ANOVA/ Dunnett Multiple comparisons test was performed at 99% of confidence level.
Results
Sensitivity (0.972 ± 0.18 vs. 1, p = 0.11) and accuracy (0.942 ± 0.17 vs. 1, p < 0.0001, q = 3.88) for the clinical examination tests combining the traditional radiological images were same to CT. However, the clinical examination tests combining the traditional radiological images had more inconclusive results (5 vs. 1), false-positive results (6 vs. 5), and false negative results (4 vs. 1) than CT. The area that detects the Bankart and bony Bankart lesions at least one time for CT was higher than that of the clinical examination tests combining the traditional radiological images.
Conclusion
CT should be considered for evaluation in patients with shoulder instability and suspected Bankart and bony Bankart lesions.
Trial registration
Researchregistry3990 dated 15 December 2014 (www.researchregistry.com).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
A glenohumeral joint is most frequently dislocated [1]. The recurrent shoulder instability affected patients can develop significant functional deficiencies and symptoms of chronic instability [2]. The reason behind recurrent instability is a glenoid bone loss or the Bankart lesion. Anterior shoulder dislocation due to structural damage to the anterior-inferior labrum with tearing of the anterior capsule is called the Bankart lesion. When it includes osseous fragments, it is called the bony Bankart lesion. The treatment involved in the reattachment of the lesion is arthroscopy with surgical suture [3]. The reason behind the Bankart lesion is a loss of 25% and/or more of the width of the inferior glenoid, which leads to a loss of bony support [4]. The glenoid bone loss is frequent in shoulders with the Bankart lesion [5].
The complexity of the combined motions of the degree of the scapulothoracic and the glenohumeral joints creates difficulties in preoperative quantification and identification of the Bankart and bony Bankart lesions for decision making of arthroscopy or open procedures [6]. Surgeons may fail in the surgical repair of the Bankart and bony Bankart lesions if not follow protocol for workup and have addressed a bony problem without being aware of it by the differential diagnosis. Moreover, the management of the Bankart and bony Bankart lesions after a failed surgery could be challenging. Therefore, an adaptation of proper diagnostic modality is crucial in the detection of the Bankart and bony Bankart lesions [7]. The optimal treatment for the Bankart and bony Bankart lesions remains controversial [8]. The accepted diagnostic method of quantifying the Bankart and bony Bankart lesions is not available [9] because physical examinations may reveal instability of the glenohumeral joints but cannot diagnose the Bankart or bony Bankart lesions. Generally, orthopedic surgeons have preferred radiography, the Computed Tomography (CT), and magnetic resonance imaging (MRI) in the decision making of surgeries [6].
Soft tissue Bankart lesion cannot be visualized on traditional radiogram. With a Grashey view, an external and internal rotation view, an axillary lateral view, a scapular-Y view, a West Point view, a Stryker notch view, and an apical oblique (Garth) view, the sensitivity of traditional radiography for detection of significant glenoid bone loss is not more than 50% [2]. Moreover, an acute fracture of the glenoid rim is often inaccurately quantified by traditional radiography [10]. Therefore, traditional radiography is underestimated bone defects. MRI has high cost and availability issues [3]. MR images are suggested only if the traditional radiography will fail to provide the necessary information for decision making of surgeries [11]. Therefore, there is a strong need for a consensus on the universally accepted diagnostic method of quantifying the Bankart and bony Bankart lesions.
The goal of the study was to access the diagnostic performance of the simple method of CT in the assessment of patients with shoulder instability and to diagnose the Bankart and bony Bankart lesions. The secondary endpoint of the study was to compare sensitivity and accuracy of the clinical examination tests combining the traditional radiological images with CT for decision making of arthroscopy or open procedures for repair of the bony problem of shoulder(s) at level 2 of evidence (Table 1) without conflict of interest.
Methods
The study had adhered 2013 Declarations of Helsinki, standards for reporting of diagnostic accuracy studies (STARD) guidelines, and the law of China. The work has been reported in line with the strengthening the reporting of cohort studies in surgery (STROCSS) criteria [12].
Inclusion criteria
Patients age 18 years and above, with a complaint of progressively reduced shoulder function, pain located at the front and lateral side of the shoulder, load-dependent pain, or/and delocalization of the shoulder available with outpatient setting of the PLA general hospital, China, Affiliated Hospital of Nantong University, China, and Dingbian County People’s Hospital, China from 18 December 2014 to 1 February 2018 were included in the study. Patients who had a bony problem of shoulder(s) and signed an informed consent form were subjected to a pre-index test (the pre-index tests were performed for eligible participants screening purposes).
Pre-index tests
Functional outcomes were measured in pre-index tests as follows to confirm glenoid bone loss:
Oxford instability shoulder score
It contains 12 items questionnaires with four responses (0–3). The total score (the sum of 12 items) ranged from 0 (excellent) to 48 (the worst) [13].
Western Ontario shoulder instability index
It has 21 items questionnaires on a visual analog scale score. The total score (the sum of 21 items) ranged from 0 (the excellent) to 100 (the worst) [13].
Simple shoulder test score
It consists of 12 questions with dichotomous response options, which are scored 0 or 1. The total score (the sum of 12 items) ranged from 0 (the worst) to 12 (the excellent) [13].
Disability of the arm, shoulder, and hand score
It is a measurement of physical function and symptoms in patients with musculoskeletal disorders from any condition in any joint in the upper extremity. It has 30-questions (grading 0–3). The average of item scores, subtracting one, and multiplying the result by 25 is the resulting score. It has the range from 0 (no disability) to 100 (extreme disability) [14].
Exclusion criteria
Patients age younger than 18 years and not signed informed consent form were excluded from the study. Patients who had frozen shoulder and arthritis were excluded from the study. Patients who had oxford instability shoulder score, four and less than four were excluded from the study.
A total of 145 patients with the proved shoulder instability were enrolled in a prospective cohort study. The demographic parameters of the enrolled patients are presented in Table 2. STARD flow diagram of the study is presented in Fig. 1.
Diagnosis of the Bankart and bony Bankart lesions
Clinical examination tests
Physical examinations of shoulders were performed as follows:
Apprehension test
The enrolled patients had kept in supine position with the arm in 900 abductions, the elbow in 900 flexions, and maximum external rotation. The evaluator had applied an anterior, external, rotatory force [15].
The relocation test
In apprehension test position, the force was applied to the humeral head in the posterior direction [16].
The anterior release/ the surprise test
The patient’s affected arm was maintained in the position of apprehension and the pressure on the humeral head was suddenly released by the evaluator [17].
The anterior drawer test
Patients were kept in supine positions and affected hand was on the examiner’s axilla, the arm was held in 80–1200 of abduction, 0–200 of forwarding flexion, and 0–300 of external rotation. With one hand, the evaluator had stabilized the scapula by applying force on the coracoid process. The other hand was grasped the humeral and drew it out anteriorly [18].
The load and shift test/ the push-pull test
Patients were kept in set positions. With the dominant hand, the evaluator was grasped the patient’s elbow and the non-dominant hand (of the evaluator) was grasped the patient’s upper arm. The evaluator was positioned the patient’s arm in 900 of abduction in the scapular plane with no rotation and centered the humeral head of subject on the glenoid by applying a force along the axis of the humeral with the dominant hand to shift the humeral head in the anterior direction [19].
The Hyperabduction test
Patients were kept in standing positions, the elbow was flexed at 900, the forearm was horizontal, and the evaluator was standing behind the patients. With the evaluator’s forearm of the dominant hand, the shoulder girdle was pushed down firmly, while the evaluator’s non-dominant hand was lifted the patient’s upper limb, which was relaxed in the abduction [13].
All tests were performed by two physiotherapists (evaluators; three years of experience) who were blinded regarding radiological images and in order of those have written. The interpretation of observations of all the tests for considering them positive or negative are presented in Table 3.
Traditional radiographs
All enrolled patients were subjected to axillary traditional radiographs (GE Healthcare, Chicago, IL, USA) at an axial position and at 900. Conventional axillary lateral, anteroposterior (in exo-rotation or in endo-rotation) radiographs and the Grashey view of the affected shoulder were performed (Fig. 2).
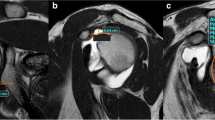
CT scans
Spiral CT (CATIA, France) was performed at 1.25 mm thickness and 0.625 mm interval of affected shoulder to confirm or exclude the Bankart and Bony Bankart lesions (Fig. 3).
Image analysis
Radiological images were checked by a radiologist (three years of experience) under the lightbox (Efftronics Systems Pvt. Ltd., China). A small bone spur in traditional radiological images of the shoulder was considered as the Bankart or bony Bankart lesions present (Fig. 4). The surgeons had decided the Bankart or bony Bankart lesions and taken the decision of arthroscopy or open procedures. CT scans were evaluated using CATIA (CATIA V5R21; Dassault Systemes, France). The percentage missing area was calculated by surface area missing and the inferior glenoid circle (Fig. 5) as per Eq. 1 (surface area method) [20]. The Bankart and/or bony Bankart lesions was confirmed if the percentage missing area was minimum 20% [3].
Surface area method of the simple Computed Tomography in the assessment of patients with shoulder instability and to diagnose the Bankart and bony Bankart lesions. Images were checked by two engineers (diploma course in musculoskeletal imaging assessments in PR. China after MD radiology) trained in musculoskeletal imaging. The Bankart and/or bony Bankart lesions was confirmed if the percentage missing area was minimum 20%
Surgery curative was considered as ‘gold standard’ in all the operative case. If any kind of bony problem (e.g. inflammation, rupture, ligament straitening, Hill–Sachs lesion) had found in diagnosis, which was lead to arthroscopy or opens surgical procedure and actually it was the Bankart and/or bony Bankart lesions considered as a ‘false negative’. If the Bankart and/or bony Bankart lesions had found in diagnosis, which was lead to surgery and actually it was the other than the bony problem (frozen shoulder, arthritis, Hill–Sachs lesion) considered as a ‘false positive’. The accurate Bankart and bony Bankart lesions absent category were also found in all diagnosis because all patients who had to complain of the shoulder(s) instability were included and there is no any accurate clinical test until the time to confirm the Bankart and bony Bankart lesions.
Beneficial analysis of diagnostic methods
Decision-making curve for detection of the Bankart and bony Bankart lesions was drawn by decision curve analysis as per Eqs. 2 and 3 [21]:
Weighting factor: The risk of overdiagnosis.
Inter-and intra-observer reliability
For purposes of the reliability of assessments, two orthopedic surgeons were analyzed twice times the traditional radiological images, two engineers trained in musculoskeletal imaging assessments (this is diploma course for musculoskeletal imaging assessments in PR. China after MD radiology; three years of experience in image analysis) were evaluated the CT scans twice, and two physiotherapists were evaluated clinical examination tests twice (each patient underwent physical examinations four times). All were blinded to the others’ conclusions.
Cost of diagnosis
Cost of diagnosis was included hospitalization, charges of experts, and radiographers.
Statistical analysis
Kappa statistics (considering kappa value (k) ≤ 0.4 low, 0.41–0.6 moderate, 0.61–0.8 substantial, and ≥ 0.81 perfect inter-and intra-observer reliabilities) were used to determine reliability [22]. One-way analysis of variance (ANOVA) following Dunnett Multiple comparisons tests (considering critical value (q) > 4.148 as significant) was performed to compare constant diagnostic parameters [23] and the Chi-square test was performed for categorical data. All results were considered significant at 99% of confidence level. InStat (vWindow, GraphPad, IL, USA) was used for statistical analysis.
Results
Functional outcome measures were strongly correlated with the Bankart and bony Bankart lesions. k for physiotherapists, orthopedic surgeons, and trained engineers (in musculoskeletal imaging) were greater than 0.81 indicated perfect inter-and intra-observer reliabilities (Table 4).
Among clinical examination tests, surprise test has high sensitivity (0.917 ± 0.15) and the anterior drawer test has high accuracy (0.811 ± 0.18). The area under the curve for the clinical examination tests combining the traditional radiological images was fallen down than CT (0.76 ± 0.11 vs. 0.89 ± 0.14, p < 0.0001, q = 9.39). Overall, the clinical examination tests combining the traditional radiological images had provided limited information for decision making of surgeries (Fig. 6). With respect to CT, sensitivity for the clinical examination tests combining the traditional radiological images had no statistical significance difference (0.972 ± 0.18 vs. 1, p = 0.11) even for accuracy there were no statistical significance difference (0.942 ± 0.17 vs. 1, p < 0.0001, q = 3.88). However, the clinical examination tests combining the traditional radiological images had more inconclusive results (5 vs. 1), false-positive results (6 vs. 5), and false negative results (4 vs. 1) than CT (Table 5). CT was flawless in the decision making of surgeries for the Bankart and bony Bankart lesions than the clinical examination tests combining the traditional radiological images (Table 6).
The analogy of diagnostic modalities for decision making of surgeries of the Bankart and bony Bankart lesions. Accuracy and sensitivity of Computed Tomography were considered as 1. One-way repeated-measures ANOVA following Dunnett Multiple comparisons tests was used for statistical analysis. A p-value < 0.01 and q-value > 4.148 were considered significant. TRI: The traditional radiological images, CT: The Computed Tomography, Ap: Apprehension test, Re: Relocation test, Sp: Surprise test, Ad: Anterior drawer test, LS: Load and shift test, Hb: Hyperabduction test, CET + TRI: Clinical examination tests combining the traditional radiological images
The area that detects the Bankart and bony Bankart lesions at least one time for CT was higher than that of clinical examination tests combining the traditional radiological images (Table 7). At 0–50% level of diagnostic confidence, orthopedic surgeons had preferred the clinical examination tests combining the traditional radiological images but these tests did not give any sufficient information for decision making of surgery. However, above 50% of the level of diagnostic confidence for the clinical examination tests combining the traditional radiological images, patients had a risk of overdiagnosis and overtreatment. In the range of 0–75% of the level of diagnostic confidence, CT was the most reliable imaging modality and above 75% of the level of diagnostic confidence, CT had a risk of overdiagnosis and overtreatment (Fig. 7).
Decision-making curve analysis for detection of the Bankart and bony Bankart lesions. Radiological images were checked by two radiologists. The Computed Tomographic images were checked by two engineers (diploma course in musculoskeletal imaging assessments in PR. China after MD radiology) trained in musculoskeletal imaging. Two physiotherapists evaluated clinical examination tests twice
The costs of clinical examination tests, the traditional radiological images, clinical examination tests combining the traditional radiological images, and CT were 8.59 ± 0.59 $/patient, 12.64 ± 1.21 $/patient, 21.11 ± 1.68 $/patient, and 47.65 ± 4.24 $/patient respectively. The cost of CT examinations was higher than the clinical examination tests combining the traditional radiological images (p < 0.0001, q = 95.05, Fig. 8).
Costs of techniques for the diagnosis of the Bankart and bony Bankart lesions. CET: Clinical examination tests, TRI: The traditional radiological images, CET + TRI: Clinical examination tests combining the traditional radiological images, CT: The Computed Tomography. Data were represented as mean ± SD. Patients enrolled in the study (sample size: n): 145. One-way ANOVA following the Dunnett Multiple comparisons tests was used for statistical analysis. A p-value < 0.01 and q-value > 4.148 were considered significant
After surgeries radiographs showed the union of the grafts and no incidents of re-dislocation during the follow-up period (Fig. 9).
Discussion
In the study, clinical examination tests alone were not provided sufficient information and surgeons were preferred radiological images for decision making of surgeries. There are high varieties of diagnostic modalities available for diagnosis of the instability of shoulders. Among the available methods, apprehension tests are the most frequently used combing traditional radiological images [24]. The Bankart and bony Bankart lesions are difficult to diagnose and there are more chances for failure of surgical procedures [25] because of the low sensitivity of radiological modalities [23]. Moreover, the adoption of the diagnostic method before the surgical procedure for the repair of the bony problem(s) of the shoulder is based on a number of dislocations and prior shoulder trauma [13]. The results of the study were not in line with an available study [13] but in line with the review article [26]. Clinical examination tests combing traditional radiological images have limited information to guide the surgeons in the decision making of surgeries for repair of the bony problem(s) of the shoulder [15]. In respect to the decisions of surgeons during the study, clinical examination tests combing traditional radiological images are failed in finding limitations of CT for quantification of the Bankart and bony Bankart lesions.
In the study, CT was provided the best visualization and clinical examination tests combing traditional radiological images were provided insufficient details of the Bankart and bony Bankart lesions for decision making of surgeries. This was because clinical examination tests combing traditional radiological images are failed to provide exact loss of the inferior glenoid [27]. These results were in line with available diagnostic studies [3, 28]. A retrospective study [29], literature reviews [4, 5, 25, 27], and a simulated study [30] are also concluded the same. But the published study is on fewer subjects (sample size: 70) [3] and more numbers of observers (four observers) [3, 28], which have less intra-observer and inter-observer reliabilities [22]. However, the results were not in line with the quantitative assessment of radiography and CT [30]. In respect to the results of the twin study, CT assessments have good agreements for decision making of surgeries of the Bankart and bony Bankart lesions.
CT method was the increased financial burden of the patients. The traditional radiological images and clinical examination tests are cheaper than CT for diagnosis of the Bankart and bony Bankart lesions. However, CT has also prevented the future recurrence and/or failure of surgeries by exact diagnosis [3]. Further research is required to justify the selection of CT for the diagnosis of the Bankart and bony Bankart lesions.
In the limitations of the study, for examples, the study was limited to diagnose the Bankart and bony Bankart lesions only no other type of shoulder delocalization was addressed in the study. The study was not differentiated the Bankart and bony Bankart lesions. The evaluators of clinical examination tests were not blind to the demographic parameters of the enrolled patients. Imaging modalities like CT arthrography, MRI, MRI arthrography provide better soft tissue details compare to CT alone. The lack of ‘gold standard’ or further MRI. The possible justification is that further MRI only for head-to-head comparisons of diagnostic methods is vague in clinical practice. Therefore, researchers have not performed Further MRI.
Conclusion
The study concluded that the Computed Tomography has better performance parameters than clinical examination tests combining the traditional radiological images and should be considered for evaluation in patients with shoulder instability and the suspected Bankart and bony Bankart lesions.
Abbreviations
- ANOVA:
-
Analysis of variance
- CT:
-
Computed Tomography
- k:
-
kappa value
- MRI:
-
Magnetic resonance imaging
- STARD:
-
Standards for reporting of diagnostic accuracy studies
- STROCSS:
-
The strengthening the reporting of cohort studies in surgery
References
Antunes JP, Mendes A, Prado MH, Moro OP, Miro RL. Arthroscopic Bankart repair for recurrent shoulder instability: a retrospective study of 86 cases. J Orthop. 2016;13:95–9.
Auffarth A, Mayer M, Kofler B, Hitzl W, Bogner R, Moroder P, Korn G, Koller H, Resch H. The interobserver reliability in diagnosing osseous lesions after first-time anterior shoulder dislocation comparing plain radiographs with computed tomography scans. J Shoulder Elb Surg. 2013;22:1507–13.
Delage RA, Balg F, Bouliane MJ, Canet-Silvestri F, Garant-Saine L, Sheps DM, Lapner P, Rouleau DM. Indication for computed tomography scan in shoulder instability: sensitivity and specificity of standard radiographs to predict bone defects after traumatic anterior glenohumeral instability. Orthop J Sports Med. 2017;5. https://doi.org/10.1177/2325967117733660.
Auffarth A, Matis N, Koller H, Resch H. An alternative technique for the exact sizing of glenoid bone defects. Clin Imaging. 2012;36:574–6.
Skupinski J, Piechota MZ, Wawrzynek W, Maczuch J, Babinska A. The bony Bankart lesion: how to measure the glenoid bone loss. Pol J Radiol. 2017;82:58–63.
Weel H, Tromp W, Krekel PR, Randelli P, van den Bekerom MP, van Deurzen DF. International survey and surgeon's preferences in diagnostic work-up towards treatment of anterior shoulder instability. Arch Orthop Trauma Surg. 2016;136:741–6.
Ho AG, Gowda AL, Michael WJ. Evaluation and treatment of failed shoulder instability procedures. J Orthopaed Traumatol. 2016;17:187–97.
Wang L, Liu Y, Su X, Liu S. A meta-analysis of arthroscopic versus open repair for treatment of bankart lesions in the shoulder. Med Sci Monit. 2015;21:3028–35.
Bois AJ, Fening SD, Polster J, Jones MH, Miniaci A. Quantifying glenoid bone loss in anterior shoulder instability: reliability and accuracy of 2-dimensional and 3-dimensional computed tomography measurement techniques. Am J Sports Med. 2012;40:2569–77.
Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BR Jr, Dewing CB, LeClere L, Romeo AA. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92:133–51.
Hendry JH, Simon SL, Wojcik A, Sohrabi M, Burkart W, Cardis E, Laurier D, Tirmarche M, Hayata I. Human exposure to high natural background radiation: what can it teach us about radiation risks? J Radiol Prot. 2009;29:A29–42.
Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP, STROCSS Group. The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int J Surg. 2017;46:198–202.
van Kampen DA, van den Berg T, van der Woude HJ, Castelein RM, Terwee CB, Willems WJ. Diagnostic value of patient characteristics, history, and six clinical tests for traumatic anterior shoulder instability. J Shoulder Elb Surg. 2013;22:1310–9.
van der Linde JA, van Kampen DA, van Beers LW, van Deurzen DF, Terwee CB, Willems WJ. The Oxford shoulder instability score; validation in Dutch and first-time assessment of its smallest detectable change. J Orthop Surg Res. 2015;10. https://doi.org/10.1186/s13018-015-0286-5.
Kumar K, Makandura M, Leong NJ, Gartner L, Lee CH, Ng DZ, Tan CH, Kumar VP. Is the apprehension test sufficient for the diagnosis of anterior shoulder instability in young patients without magnetic resonance imaging (MRI)? Ann Acad Med Singap. 2015;44:178–84.
Ebrahimzadeh MH, Moradi A, Zarei AR. Minimally invasive modified latarjet procedure in patients with traumatic anterior shoulder instability. Asian J Sports Med. 2015;6. https://doi.org/10.5812/asjsm.26838.
Lizzio VA, Meta F, Fidai M, Makhni EC. Clinical evaluation and physical exam findings in patients with anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10:434–41.
Park JY, Kim Y, Oh KS, Lim HK, Kim JY. Stress radiography for clinical evaluation of anterior shoulder instability. J Shoulder Elb Surg. 2016;25:e339–47.
Morita W, Tasaki A. Intra- and inter-observer reproducibility of shoulder laxity tests: comparison of the drawer, modified drawer and load, and shift tests. J Orthop Sci. 2018;23:57–63.
Barchilon VS, Kotz E, Barchilon Ben-Av M, Glazer E, Nyska M. A simple method for quantitative evaluation of the missing area of the anterior glenoid in anterior instability of the glenohumeral joint. Skelet Radiol. 2008;37:731–6.
Fitzgerald M, Saville BR, Lewis RJ. Decision curve analysis. JAMA. 2015;13:409–10.
Dixon SN, Donner A, Shoukri MM. Adjusted inference procedures for the interobserver agreement in twin studies. Stat Methods Med Res. 2016;25:1260–71.
Thomazeau H, Courage O, Barth J, Veillard D, Boileau P, Society FA. Can we improve the indication for Bankart arthroscopic repair? A preliminary clinical study using the ISIS score. Orthop Traumatol Surg Res. 2010;96:S77–88.
Bushnell BD, Creighton RA, Herring MM. Bony instability of the shoulder. Arthroscopy. 2008;24:1061–73.
Arciero RA, Parrino A, Bernhardson AS, Diaz-Doran V, Obopilwe E, Cote MP, Golijanin P, Mazzocca AD, Provencher MT. The effect of a combined glenoid and hill-Sachs defect on glenohumeral stability: a biomechanical cadaveric study using 3-dimensional modeling of 142 patients. Am J Sports Med. 2015;43:1422–9.
Hanchard NC, Lenza M, Handoll HH, Takwoingi Y. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD00742.
Sugaya H. Techniques to evaluate glenoid bone loss. Curr Rev Musculoskelet Med. 2014;7:1–5.
Milano G, Saccomanno MF, Magarelli N, Bonomo L. Analysis of agreement between computed tomography measurements of glenoid bone defects in anterior shoulder instability with and without comparison with the contralateral shoulder. Am J Sports Med. 2015;43:2918–26.
Loh B, Lim JB, Tan AH. Is clinical evaluation alone sufficient for the diagnosis of a Bankart lesion without the use of magnetic resonance imaging? Ann Transl Med. 2016;4. https://doi.org/10.21037/atm.2016.11.22.
Itoi E, Lee SB, Amrami KK, Wenger DE, An KN. Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med. 2013;31:112–1128.
Acknowledgments
Authors are like to thank for radiological, anesthetic, surgical, medical, and physiotherapist staff of PLA General Hospital, Beijing, China, Affiliated Hospital of Nantong University, Nantong Shi, China, and Dingbian County People’s Hospital, Dingbian, China.
Funding
The research did not receive any specific financial motivation from government, non-government, or non-profitable sector to perform research.
Availability of data and materials
All information regarding patients were available from patients’ Digital Imaging and Communications in Medicine files of Affiliated Hospital of Nantong University, China, Dingbian County People’s Hospital, China, and PLA General Hospital, China.
Author information
Authors and Affiliations
Contributions
All authors had read and approved a submission for publication. TL and JM contribute equally to conceptualization and methodology of the study. HC contributed to methodology, data curation, and formal analysis of the study. DH contributed to investigation, resources, and software of the study. LX was project administrator, contributed to data curation, the manuscript preparation, the manuscript editing, and the manuscript review for the intellectual content. The author agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study had been registered in the research registry (www.researchregistry.com), UID No.: researchregistry3990 dated 15 December 2014. The protocol (DI/HR/27/14, dated 15 November 2014) had been approved by the PLA General Hospital review board. The enrolled patients signed an informed consent form regarding radiology and surgeries.
Consent for publication
The enrolled patients signed an informed consent form regarding the publication of the study including patients’ personal images (if any) in all formats (hard and/or electronics) irrespective of time and language.
Competing interests
Authors have reported that they have no commercial or associated interest that represents a conflict of interest in connection with results and/or discussion reported the submitted manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Liu, T., Ma, J., Cao, H. et al. Evaluation of the diagnostic performance of the simple method of computed tomography in the assessment of patients with shoulder instability: a prospective cohort study. BMC Med Imaging 18, 45 (2018). https://doi.org/10.1186/s12880-018-0290-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-018-0290-4