Abstract
Background
Amnestic mild cognitive impairment (aMCI) is characterized by cognitive functional decline, especially in memory. Resting-state functional magnetic resonance imaging (fMRI) has been widely used in neuroimaging studies that explore alterations between patients and normal individuals to elucidate the pathological mechanisms of different diseases. The current study was performed to investigate alterations in the functional connectivity of the default mode network (DMN) in aMCI patients compared to healthy elderly controls, as well as further define the association between neurological alterations and memory function.
Methods
Twenty-five aMCI patients and 25 healthy individuals were recruited and underwent both fMRI and neuropsychological examinations. fMRI data was analyzed by independent component analysis.
Results
Compared to healthy individuals, aMCI patients exhibited a significant increase in functional connectivity between the DMN and right-middle and right-superior frontal gyri, left-middle occipital gyrus, and left-middle temporal gyrus, but reduced functional connectivity between the DMN and left-middle and left-inferior frontal gyri and left insula. These alterations were found to be associated with reduced memory function.
Conclusions
aMCI patients exhibited abnormal functional connectivity between the DMN and certain brain regions which is associated with changes in memory function associated with aMCI.
Similar content being viewed by others
Background
Current evidence suggests that approximately 44 million individuals suffer from dementia or Alzheimer disease (AD) worldwide, and this figure is expected to more than triple by 2050 due to a rapidly expanding older adult population [1]. AD is a neurodegenerative disorder characterized by progressive dementia with widespread cognitive decline [2]. Mild cognitive impairment (MCI) is considered to be an intermediate stage between normal aging and AD [3, 4]. MCI patients show decline in cognitive functiongreater than that expected for one’s age and education level, but the severity is not enough to be classified as dementia; however, these individuals have a higher risk of developing dementia or AD than their age-matched, normal controls (10–15% annually for MCI versus 1–4% for controls) [5,6,7]. Moreover, the subtype of MCIwith memory complaint and deficit, namely amnestic MCI (aMCI), is consistently shown to have a higher risk of dementia than those without memory impairment [6]. More and more attention has been paid to preventative therapies and pathological processes associated with each stage of MCI in recent years because clinical trials of treatments for AD have failed. The growing consensus is that the target population for more effectively interventions is not individuals with diagnosed dementia but rather those with aMCI [8, 9].
Recently, resting-state functional magnetic resonance imaging (fMRI) has been increasingly utilized for studying the pathogenesis of MCI. Many researchers have begun to explore alterations within the resting-state brain network which may directly relate to disease pathology. The idea of the default mode network (DMN) has attracted many neuroimaging experts to examine alterations in the resting-state brain physiology of normal aging subjects and those with neurological disorders predominantly via fMRI [10]. The DMN is believed to anatomically involve the precuneus (PCu)/posterior cingulate cortex (PCC), medial prefrontal cortex (MPFC), medial temporal lobe, including the hippocampus and adjacent cortex, and inferior parietal lobule, as well as temporoparietal junction,retrosplenial cortex and the lateral temporal cortex, which play vital roles in cognition and memory [11,12,13]. Many studies have demonstrated that breakdown of DMN connectivity may underlie cognitive function loss in MCI subjects. For example, the intrinsic functional connectivity in the hippocampus, parahippocampal gyrus, PCu [14], PCC, inferior parietal lobule [15], and medial temporal and/or bilateral medial frontal lobes [16] has been shown to be decreased in MCI subjects compared with healthy controls. The functional connectivity between different regions within the DMN, such as between the hippocampus and PCC [17, 18], PCC and MPFC, and/or PCC and PCu [19], has also been reported to be absent or decreased in MCI patients. Hence, such neuroimaging findings could be considered as potential biomarkers of MCI. However, most previous results were obtained based on region-of-interest analyses, making it difficult for researchers to come to a unanimous conclusion considering the limitations of this approach with the relative arbitrariness of the region-of-interest [20].
In the present study, we investigated the presence of DMN alterations in aMCI patients compared with healthy, elderly controls using independent component analysis (ICA). In particular, we examined the relationship between network functional connectivity and different brain regions in aMCI patients to better clarify the neuropathological mechanism associated with aMCI. Furthermore, we assessed whether the changes in brain network functional connectivity correlated with severity of global cognitive performance.
Methods
Participants
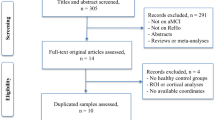
Twenty-five participants diagnosed with aMCI according to Peterson diagnostic criteria were recruited from the Cangxia and Fengdanbailu communities in Fuzhou City (China) [21]. All patients were males or females aged 60 years or older, had recent subjective memory complaint, showed objective memory decline defined by a Wechsler Memory Scale-Chinese Revision (WMS-CR) score less than 1.5standard deviations below normative means, normal or near-normal general cognitive function defined by a Mini-Mental State Examination (MMSE) score less than normality with adjustment for age and education, a preserved activities of daily living (ADL) scale score less than 18, and absence of dementia. Another 25 healthy, elderly control subjects without memory complaint were also recruited. All aMCI and control participants were right-handed and were without MRI contraindications.
fMRI data acquisition
Images were collected using a 3.0-Tesla General Electric scanner (Milwaukee, WI, USA) with an eight-channel phased-array head coil. All subjects were instructed to lie still with their eyes closed without falling asleep, stay relaxed, and not think of anything in particular. Resting-state scans were acquired using an echo planar imaging sequence with the following parameters: time resolution = 2100 ms, echo time = 30 ms, field of view = 200 × 200 mm, flip angle = 90°, slice thickness = 3 mm with a 0.6-mm gap, 42 slices, 64 × 64 matrix, and phases per location = 160. T1 three-dimensional magnetization-prepared rapid gradient-echo imaging was acquired in the same session with the following parameters: echo time = min, field of view = 240 × 240 mm, flip angle = 15°, inversion time = 450 ms, slice thickness = 1 mm, and 164 slices per acquisition). Both behavioral examinations and fMRI scans were completed within a week after enrollment.
fMRI data preprocessing
fMRI data preprocessing was performed using the Oxford Centre for Functional MRI of the Brain’s (FMRIB) Software Library (FSL version 5.0.8, Oxford, UK; http://www.fmrib.ox.ac.uk/fsl). Nine-parameter nuisance signals, including global, white matter, and cerebral spinal fluid signals and six head motion parameters, were extracted and removed using the Brain Extraction Tool in FMRIB, and a mean functional image was created for each subject. Next, functional images were spatially smoothed with a 6-mm full-width at half-maximum Gaussian smoothing kernel in FMRIB. Data were then band-pass filtered at 0.01 to 0.10 Hz to reduce the influence of low frequency noise and effects of higher frequencies, such as respiratory and cardiac signals. In addition, each participant’s functional images were coregistered to their corresponding skull-stripped anatomical image and then registered to the Montreal Neurological Institute 152 stereotactic template using linear affine transformations with 12 degrees of freedom.
fMRI data analysis
Analysis of fMRI data was performed using multivariate exploratory linear optimized decomposition into independent components [22]. Probabilistic ICA was applied to derive each group’s (n = 50 total) resting-state network activity at 20 components. The DMN was identified according to functional networks described in earlier studies, and the similarity between our data and the template networks derived from 1414 participants was calculated [23].
Then, a dual-regression technique was applied [23]. First, the priori defined DMN was used as a spatial regressor in a general linear model (GLM) to extract each subject’s temporal dynamics. These time-courses were then used as a set of temporal regressors in our GLM to generate subject-specific maps associated with the different group-level independent components. Finally, group analysis was performed with the whole brain and subject-specific maps from the second GLM, which represented the functional connectivity strength of each voxel with the DMN.
To explore the relationship between changes in functional connectivity and cognitive behavior, a regression analysis was performed between subject-specific network maps and each subject’s WMS-CR memory quotient (MQ). A threshold of voxel-wise Z > 2.3 and cluster-level family wise error (FWE) correction for multiple comparison corrections of P < 0.05were used. Moreover, age, gender, and education level were considered as covariates in this GLM.
Statistical analysis
Statistical analyses were performed with SPSS version 18.0 software (SPSS Inc., Chicago, IL, USA) for demographic and neuropsychological data, as well as correlation analyses. The normality of continuous variables was examined using the Shapiro-Wilk test. Normally distributed data were expressed as means ± standard deviations and analyzed by Student’s t-test. Non-normally distributed data were analyzed using the nonparametric Mann-Whitney U-test and reported as the median and interquartile range. A Chi-square test was used to assess gender differences between the two groups. The mean Z-values of DMN regions with significant differences between the two groups were extracted, and correlations with neuropsychological scores were analyzed using a Spearman correlation analysis or Pearson correlation analysis if data had non-normal distribution. A P < 0.05 was considered to be significantly different.
Results
Demographic and neuropsychological data
Demographic and neuropsychological characteristics of both groups are described in Table 1. Gender, age, and MMSE and ADL scores were not significantly different between aMCI and control groups (all P > 0.05). Interestingly, the education level of aMCI patients was significantly higher than for healthy controls (P = 0.012), but their memory ability measured by WMS-CR was significantly lower than the healthy control group (P < 0.001).
Differences in DMN functional connectivity
The DMN obtained from ICA was in conformity with previously published results [23], which included the MPFC, anterior cingulate cortex, parietal cortex, and Pcu/PCC (Fig. 1). The correlation coefficent (r-value) between the independent component we chose and the template network was 0.56. All valid resting-state components derived from ICA are shown in Additional file 1: Table S1.
Compared with healthy controls, aMCI subjects exhibited a significant increase in functional connectivity between the DMN and right-middle and right-superior frontal gyri, left-middle occipital gyrus, and left-middle temporal gyrus. On the other hand, reduced functional connectivity was found between the DMN and the left-middle and left-inferior frontal gyri and left insula (Fig. 2a-b; Table 2).
Abnormal functional connectivity of the DMN in MCI patients compared to healthy controls. a The yellow color indicates brain regions exhibiting increased functional connectivity (A: right-middle frontal gyrus; B: right-superior frontal gyrus, left-middle occipital gyrus, and left-middle temporal gyrus) in MCI patients compared with healthy controls. b The red color indicates brain regions exhibiting decreased functional connectivity (A: left-middle frontal gyrus; B: left-inferior frontal gyrus; C: left insula) in MCI patients compared to healthy controls
Correlations between DMN functional connectivity and WMS-CR MQ
Regression analysis between the DMN and WMS-CR MQ showed a negative association between the DMN and the left-middle frontal gyrus, right-middle and left-inferior occipital gyri, and left-middle temporal gyrus. A positive association was found between the DMN and right-middle and right-superior frontal gyri and right cingulate gyrus (Fig. 3a-b; Table 3). Pearson correlation analysis showed that WMS-CR MQ changes were positively correlated with functional connectivity alterations in the right-middle occipital gyri (r = 0.490, P = 0.0004) and left-inferior occipital gyri (r = 0.516, P = 0.0001),where as negatively correlated with functional connectivity alteration in the right-middle frontal gyrus (r = −0.555, P = 0.0003) (Fig. 4).
Correlation between functional connectivity alterations in the DMN and WMS-CR MQ changes across all participants. a The yellow color indicates brain regions exhibiting increased functional connectivity in MCI versus control subjects; the blue color indicates brain regions exhibiting a negative association between their DMN functional connectivity alterations with corresponding WMS-CR MQs across all participants. b The red color indicates brain regions exhibiting decreased functional connectivity in MCI patients compared to healthy controls; the green color indicates brain regions exhibiting a positive association between their DMN functional connectivity alterations with corresponding WMS-CR MQs across all participants
Discussion
Several previous studies have compared differences in the DMN between MCI and healthy subjects [14,15,16,17,18,19, 24, 25]. Most of them used region-of-interest (ROI) and task-fMRI to explore the functional connectivity or activation of regions within the DMN. However, results of previous studies varied widely due to different ROIs and tasks the researchers chose and therefore analysis of functional connectivity via resting-state fMRI requires a less complex task design and data-driven approach. Moreover, ICA can determine distinct components by capturing spatial independence and time-courses of resting-state data and thereby, reliably define different resting-state networks. In the current study, we examined functional connectivity within the DMN in a sample of aMCI patients and healthy controls using the ICA method and found an increase in functional connectivity between the DMN and right-middle and right-superior frontal gyri, left-middle occipital gyrus, and left-middle temporal gyrus, as well as decreased functional connectivity between the DMN and left-middle and inferior frontal gyri and left insula in aMCI patients compared to healthy controls. In addition, our findings also indicated these alterations in functional connectivity between the DMN and specified brain regions were closely associated with memory decline.
The frontal lobe is one of the most complicated brain regions and is involved in a variety of cognitive functions, especially memory [26, 27]. aMCI patients, characterized by memory deficits, often exhibit abnormal functional connectivity between the frontal lobe and other brain regions. As a result, the frontal lobe is considered to be a “hub” that is profoundly relevant to memory processing in MCI [28]. Sui et al. [29] reported that long-range functional connectivity density in the superior and middle frontal gyri was increased in MCI patients compared to healthy controls and also correlated with cognitive performance, allowing differentiation of MCI brain from controls. Zhao et al. [30] found that aMCI patients showed increased amplitude of low-frequency fluctuation (ALFF) signals in the left-superior and middle-frontal gyri compared with normal subjects. Similarly, our results showed that aMCI patients showed a significant increase in functional connectivity between the DMN and right-middle and right-superior frontal gyri.
The middle occipital gyrus is an important part of the primary visual cortex considered to play a role in the processing of visual recognition. Its abnormal connectivity might lead to impaired visual cognition in aMCI patients [31]. Cai et al. [32] reported that aMCI patients exhibited a significant increase in ALFF in the left-middle occipital gyrus and increased functional connectivity between the left-middle occipital gyrus and other regions. Golby et al. [33] also found that AD patients exhibited deficient explicit memory but had normal implicit memory, which was encoded in the occipital cortex. In the current study, results revealed an increase in functional connectivity between the DMN and left-middle occipital gyrus in aMCI patients compared with healthy controls, which might be helpful for maintaining normal implicit memory in patients with aMCI. In addition, current results also demonstrated a significant decrease in functional connectivity between the DMN and left-inferior frontal gyrus in MCI patients, which is consistent with a prior study [34]. This is likely because encoding and retrieval of memory in healthy older adults is primarily driven by the hippocampus and inferior frontal gyrus [35]. Thus, the decreased functional connectivity of aMCI patients may result in problems with encoding and retrieval of memory.
Some possible limitations to the current study may exist. First, our sample size was relatively small (n = 25 per group), which might have affected the statistical power of results and might induce sampling biases. Second, considering the difficulty associated with recruitment, we did not use a matched-pair study design. This likely led to the significant difference in education level between the two groups and may have induced bias regarding cognitive measures between groups. Additionally, it is difficult to derive causal associations between changes in functional connectivity and cognitive ability due to the cross-sectional design of our study. Further studies with larger sample sizes are needed to strengthen the results, and might apply a matched-pair design with a control group that is age-, gender- and education-level- matched to reduce bias. Moreover, longitudinal studies with follow-up periods are needed to investigate whether functional connectivity alterations of the DMN in aMCI could be an early biomarker for higher risk of conversion to dementia in the future.
Conclusions
In summary, the present study was conducted to explore the alterations of the resting-state functional connectivity of the DMN in patients with MCI. The results demonstrated that MCI exhibited significantly increased functional connectivity between the DMN and right-middle and right-superior frontal gyri, left-middle occipital gyrus, and left-middle temporal gyrus, but reduced functional connectivity between the DMN and the left-middle and left-inferior frontal gyri and left insula. These alterations were associated with memory changes in MCI patients, which suggested that the altered DMN functional connectivity might be useful for the preclinical identification of dementia.
Abbreviations
- AD:
-
Alzheimer disease
- ADL:
-
Activities of daily living
- ALFF:
-
Amplitude of low-frequency fluctuation
- aMCI:
-
Amnestic mild cognitive impairment
- DMN:
-
Default mode network
- fMRI:
-
Functional magnetic resonance imaging
- FMRIB:
-
Functional MRI of the brain’s
- FSL:
-
Functional MRI of the brain’s software library
- GLM:
-
General linear model
- ICA:
-
Independent component analysis
- MMSE:
-
Mini-mental state examination
- MPFC:
-
Medial prefrontal cortex
- MQ:
-
Memory quotient
- PCC:
-
Posterior cingulate cortex
- PCu:
-
Precuneus
- WMS-CR:
-
Wechsler memory scale-chinese revision
References
Lindbergh CA, Dishman RK, Miller LS. Functional disability in mild cognitive impairment: a systematic review and meta-analysis. Neuropsychol Rev. 2016;26(2):129–59.
Blennow K, de Leon MJ, Zetterberg H. Alzheimer's disease. Lancet. 2006;368(9533):387–403.
Chetelat G, Landeau B, Eustache F, Mézenge F, Viader F, de la Sayette V, et al. Using voxel-based morphometry to map the structural changes associated with rapid conversion in MCI: a longitudinal MRI study. NeuroImage. 2005;27(4):934–46.
Karas GB, Scheltens P, Rombouts SA, Visser PJ, van Schijndel RA, Fox NC, et al. Global and local gray matter loss in mild cognitive impairment and Alzheimer’s disease. NeuroImage. 2004;23(2):708–16.
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303–8.
Gauthier S, Reisberg B, Zaudig M, Petersen RC, Ritchie K, Broich K, et al. Mild cognitive impairment. Lancet. 2006;367(9518):1262–70.
Farias S, Mungas D, Reed B, Harvey D, DeCarli C. Progression of mild cognitive impairment to dementia in clinic-vs community-based cohorts. Arch Neurol. 2009;66(9):1151–7.
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–92.
Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. JIntern Med. 2014;275(3):214–28.
Ouchi Y, Kikuchi M. A review of the default mode network in aging and dementia based on molecular imaging. Rev Neurosci. 2012;23(3):263–8.
Spreng RN, Sepulcre J, Turner GR, Stevens WD, Schacter DL. Intrinsic architecture underlying the relations among the default, dorsal attention, and frontoparietal control networks of the human brain. J Cogn Neurosci. 2013;25(1):74–86.
Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci U S A. 2005;102(27):9673–8.
Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1–38.
Wang Y, Risacher SL, West JD, McDonald BC, Magee TR, Farlow MR, et al. Altered default mode network connectivity in older adults with cognitive complaints and amnestic mild cognitive impairment. J Alzheimers Dis. 2013;35(4):751–60.
Esposito R, Mosca A, Pieramico V, Cieri F, Cera N, Sensi SL. Characterization of resting state activity in MCI individuals. PeerJ. 2013;1:e135.
Lee ES, Yoo K, Lee YB, Chung J, Lim JE, Yoon B, et al. Default mode network functional connectivity in early and late mild cognitive impairment: results from the Alzheimer’s Disease Neuroimaging Initiative. Alzheimer Dis Assoc Disord. 2016;30(4):289–96.
Sorg C, Riedl V, Muhlau M, Calhoun VD, Eichele T, Läer L, et al. Selective changes of resting-state networks in individuals at risk for Alzheimer's disease. Proc Natl Acad Sci U S A. 2007;104(47):18760–5.
Dunn CJ, Duffy SL, Hickie IB, Lagopoulos J, Lewis SJ, Naismith SL, et al. Deficits in episodic memory retrieval reveal impaired default mode network connectivity in amnestic mild cognitive impairment. Neuroimage Clin. 2014;4:473–80.
Wang Z, Liang P, Jia X, Jin G, Song H, Han Y, et al. The baseline and longitudinal changes of PCC connectivity in mild cognitive impairment: a combined structure and resting-state fMRI study. PLoS One. 2012;7(5):e36838.
Sbardella E, Petsas N, Tona F, Pantano P. Resting-state fMRI in MS: general concepts and brief overview of its application. Biomed Res Int. 2015;2015:212693. doi:10.1155/2015/212693.
Peterson R. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256(3):183–94.
Beckmann CF, Smith SM. Probabilistic independent component analysis for functional magnetic resonance imaging. IEEE TransMed Imaging. 2004;23(2):137–52.
Biswal BB, Mennes M, Zuo XN, Gohel S, Kelly C, Smith SM, et al. Toward discovery science of human brain function. Proc Natl Acad Sci U S A. 2010;107(10):4734–9.
Wang P, Zhou B, Yao H, Zhan Y, Zhang Z, Cui Y, et al. Aberrant intra- and inter-network connectivity architectures in Alzheimer’s disease and mild cognitive impairment. Sci Rep. 2015;5:14824.
Garces P, Angel PJ, Canuet L, Aurtenetxe S, López ME, Marcos A, et al. The default mode network is functionally and structurally disrupted in amnestic mild cognitive impairment - a bimodal MEG-DTI study. Neuroimage Clin. 2014;6:214–21.
Fuster JM. Frontal lobe and cognitive development. J Neurocytol. 2002;31(3–4):373–85.
Centeno M, Thompson PJ, Koepp MJ, Helmstaedter C, Duncan JS. Memory in frontal lobe epilepsy. Epilepsy Res. 2010;91(2–3):123–32.
Yao Z, Zhang Y, Lin L, Zhou Y, Xu C, Jiang T, et al. Abnormal cortical networks in mild cognitive impairment and Alzheimer’s disease. PLoS Comput Biol. 2010;6(11):e1001006.
Sui X, Zhu M, Cui Y, Yu C, Sui J, Zhang X, et al. Functional connectivity hubs could serve as a potential biomarker in Alzheimer’s disease: a reproducible study. Curr Alzheimer Res. 2015;12(10):974–83.
Zhao Z, Lu J, Jia X, Chao W, Han Y, Jia J, et al. Selective changes of resting-state brain oscillations in aMCI: an fMRI study using ALFF. Biomed Res Int. 2014;2014:920902.
Cai S, Chong T, Zhang Y, Li J, von Deneen KM, Ren J, et al. Altered functional connectivity of fusiform gyrus in subjects with amnestic mild cognitive impairment: a resting-state fMRI study. Front Hum Neurosci. 2015;9:471.
Cai S, Chong T, Peng Y, Shen W, Li J, von Deneen KM, et al. Altered functional brain networks in amnestic mild cognitive impairment: a resting-state fMRI study. Brain Imaging Behav. 2016 Mar;14 [Epub ahead of print]
Golby A, Silverberg G, Race E, Gabrieli S, O'Shea J, Knierim K, et al. Memory encoding in Alzheimer’s disease: an fMRI study of explicit and implicit memory. Brain. 2005;128(Pt 4):773–87.
De Vogelaere F, Santens P, Achten E, Boon P, Vingerhoets G. Altered default-mode network activation in mild cognitive impairment compared with healthy aging. Neuroradiology. 2012;54(11):1195–206.
Hampstead BM, Khoshnoodi M, Yan W, Deshpande G, Sathian K. Patterns of effective connectivity during memory encoding and retrieval differ between patients with mild cognitive impairment and healthy older adults. NeuroImage. 2016;124(Pt A):997–1008.
Acknowledgements
The authors would like to thank the Medical Imaging Division, Affiliated Rehabilitation Hospital of Fujian University of Traditional Chinese Medicine, and we also thank all of the participants involved in the study.
Funding
This study was funded by the National Natural Science Foundation of China (www.nsfc.gov.cn, Grant No.81574045) and the Fujian Collaboration Innovation Center for Rehabilitation Technology (Grant No.×2015001- Collaboration).
Availability of data and materials
All relevant data and materials of the findings are anonymised and stored at the Scientific Research Division of the Fujian University of Traditional Chinese Medicine. And the data are available on request from the corresponding author.
Author information
Authors and Affiliations
Contributions
GZ, LC conceived of the study and participated in its design. ML supervised the study process, collected data and wrote the manuscript. GZ revised the manuscript critically. YZ, ZX and WZ carried out the recruitment of participants and acquisition of data. RX helped to develop the study measures and performed analysis and interpretation of data. JT was in charge of coordination and implementation. ML, SL and QW performed the statistical analysis of data. All authors have read and given approval of the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was carried out in accordance with the declaration of Helsinki, and Ethical approval was given by the Medical Ethics Committee of the Second People’s Hospital of Fujian Province, China (approval number: 2014-KL045–02). All participants have been fully informed about the study and have signed the informed consent form prior to participation.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: Table S1.
Valid resting-state components derived from ICA. (DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Li, M., Zheng, G., Zheng, Y. et al. Alterations in resting-state functional connectivity of the default mode network in amnestic mild cognitive impairment: an fMRI study. BMC Med Imaging 17, 48 (2017). https://doi.org/10.1186/s12880-017-0221-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-017-0221-9