Abstract
Background
Sepsis is a frequent cause of admission to intensive care units (ICUs). High mortality rates are estimated globally, and in our country, few studies have reported one-year survival. The objective of this study is to determine one-year survival in patients with sepsis admitted to the ICU in Colombia, compared with the survival of patients admitted for other conditions.
Methods
Retrospective cohort study using administrative databases from the Ministry of Health of Colombia. One-year survival and the adjusted hazard ratio for survival, adjusted for comorbidities included in the Charlson Index, were determined using a Cox proportional hazards model for patients admitted for other causes as well as for those admitted for sepsis. This was then compared with an inverse propensity score weighting model.
Results
A total of 116.407 patients were initially admitted to the ICUs, with 12.056 (10.36%) diagnosed with sepsis. Within the first year, 4.428 (36.73%) patients died due to sepsis. Age and male gender were associated with an increased risk of death from sepsis, and the covariates associated with one-year mortality were as follows: age over 80 years with HR 9.91 (95% CI: 9.22–10.65), renal disease with HR 3.16 (95% CI: 3.03–3.29), primary tumoral disease with HR 2.07 (95% CI: 1.92–2.23), liver disease with HR 2.27 (95% CI: 2.07–2.50), and metastatic solid tumor with HR 2.03 (95% CI: 1.92–2.15).
Conclusion
This study revealed a high one-year sepsis mortality rate in the population, associated with variables such as age over 80 years, the presence of renal disease, liver disease, connective tissue diseases, and cancer. Men exhibited higher mortality compared to women.
Similar content being viewed by others
Introduction
Sepsis continues to be one of the leading causes of patient admissions to intensive care units (ICUs) [1]. The estimated incidence of sepsis in the last decade is 276 cases per 100,000 person-years [2]. Hospital mortality rates range from 12.5 to 32.2%, which may vary depending on the sepsis origin, comorbidities, and geographical regions such as North America, Europe, and Oceania [3, 4]. Rudd et al. [5]. described 48.9 million incident cases and 11.0 million sepsis-related deaths in a global disease burden study with administrative data from 1990 to 2017. Despite efforts made for timely diagnosis and treatment, a reduction in sepsis incidence and mortality has not been achieved [6,7,8,9].
Abu-Kaf et al. [10], in 2018, reported a mortality rate of 4.5% for patients diagnosed with sepsis, compared to 0.7% for those admitted to the ICU for other reasons. Bauer et al. [11], in a systematic review of 170 studies, described sepsis mortality rates at 30 and 90 days ranging from 3.26 to 46.71% and 13.04–56.67%, respectively. Liu et al. [12] reported sepsis mortality in China between 20.6% and 50.8%.
Characterizing the burden of sepsis in different regions and identifying influencing factors could enable the development of strategies for timely diagnosis and treatment, positively impacting clinical outcomes [9, 13]. This study aims to determine the mortality of sepsis patients admitted to ICUs in Colombia and their one-year survival.
Methods
A retrospective cohort study was conducted using administrative data from the Integrated Social Protection Information System (SISPRO) of the Colombian Ministry of Health.
Population
Patients over 18 years of age who were admitted to approximately 300 ICUs across Colombian territory from January 1 to December 31, 2019, with a diagnosis of sepsis were included. In the case of patients with multiple admissions, data from the first hospitalization were used. Patients were identified by procedure codes related to ICU admission.
Data sources
Data were sourced from the capitation unit (UPC) databases of the Integrated Protection System (SISPRO) of the Colombian Ministry of Health. This database comprises reports of services provided by health promotion companies to 22.4 million Colombians, representing 45% of the population enrolled in the contributory regime. The database is highly standardized and includes service codes (CUPS), service date, age, gender, insurance provider, municipality, and ICD-10 codes (See supplementary Table 1). Mortality information, date of death, and diagnoses related to the cause of death were obtained from death certificates (RUAF). The datasets utilized and/or analyzed in the current study are available upon reasonable request from the corresponding author.
Studied variables
The primary outcome was one-year mortality and the diagnosis of sepsis. Other variables considered included demographic characteristics such as age, gender, and place of origin. Coexisting conditions identified using the Charlson Index, validated for the Colombian population [14], were also included. The mortality records were efficiently integrated with hospitalization records and death dates by using a unique identification number and death certificates (RUAF) to determine one-year mortality. All patients were followed for a minimum of one year, with administrative censoring as of December 31, 2020, or until the occurrence of the death event.
Statistical analysis
Baseline demographic and clinical characteristics for patients with and without sepsis were determined and compared using standardized differences to assess balance between the two groups. Hazard ratios (HR) for one-year survival were then calculated between patients with sepsis and those without sepsis. To control for confounding due to systematic differences between patients with and without sepsis with respect to survival, demographic characteristics, and coexisting conditions were included in the Cox proportional hazards model. These variables included age, gender, hypertension, diabetes mellitus, cerebrovascular disease, connective tissue disease, liver disease, cancer, neoplastic disease, and metastatic disease.
Finally, to assess the consistency of the Cox model, it was compared with hazard coefficients obtained from a pseudo-population created by weighting inverse scores from propensity scores derived from a logistic regression model of the probability of sepsis occurrence based on patient characteristics and comorbidities. Data processing and statistical analyses were performed using the following software: EmEditor 22.3, Python 3.9, and the R statistical package (See supplementary Table 2).
Results
Out of a total of 120.902 patients admitted for the first time to 300 ICUs in Colombian territory during the period from January 1 to December 31, 2019. 4.500 patients were excluded due to incomplete data, leaving a total of 116.407 patients. We identified 12.056 (10.36%) patients with a sepsis diagnosis, which corresponds to 54.8 cases per 100.000 person-years. Among these, 1.826 (15.15%) patients died within 30 days of ICU admission, and 4.428 (36.73%) patients within the first year. Another 104.351 (89.64%) patients were admitted for other reasons, with 7.744 (7.42%) deaths at 30 days and 15.979 (17.31%) deaths within the year (Fig. 1).
General population characteristics
The most prevalent comorbidities among the population of patients admitted to the ICU were arterial hypertension in 74.280 patients (63.79%), diabetes mellitus in 26.470 (22.73%), chronic obstructive pulmonary disease in 20.535 (17.63%), and acute myocardial infarction in 19.792 (17.01%). General population characteristics are presented in Table 1.
One-year survival in sepsis patients
The crude one-year survival of sepsis patients had an HR of 2.71 (95% CI: 2.62–2.80). The adjusted HR was 1.81 (95% CI: 1.75–1.88), and the HR adjusted by IPW was 2.10 (95% CI: 2.02–2.18).
Factors associated with one-year survival in ICU admitted patients
In the general population of patients admitted to the ICU, conditions associated with a higher risk of one-year mortality included renal disease (HR 3.17, 95% CI: 3.04–3.31), liver disease (HR 2.22, 95% CI: 2.00–2.46), primary tumoral disease (HR 2.07, 95% CI: 1.97–2.13), and metastatic solid tumor (HR 2.01, 95% CI: 1.90–2.13) (Table 2 and Supplementary Fig. 1).
Factors associated with one-year survival in sepsis patients
In the population of sepsis patients, variables associated with one-year mortality were age over 80 years (HR 9.91, 95% CI: 9.22–10.65), renal disease (HR 3.16, 95% CI: 3.03–3.29), primary tumoral disease (HR 2.07, 95% CI: 1.92–2.23), liver disease (HR 2.27, 95% CI: 2.07–2.50), metastatic solid tumor (HR 2.03, 95% CI: 1.92–2.15), and connective tissue disease (HR 1.2, 95% CI: 1.16–1.32) (Table 3 and Supplementary Fig. 2).
Factors associated with one-year survival in no sepsis patients
In the population of sepsis patients, variables associated with one-year mortality were age over 80 years (HR 10.4, 95% CI: 9.69–11.35), renal disease (HR 3.56, 95% CI: 3.40–3.73), liver disease (HR 2.67, 95% CI: 2.40–2.97), primary tumoral disease (HR 2.34, 95% CI: 2.16–2.54), metastatic solid tumor (HR 2.18, 95% CI: 2.05–2.32), and connective tissue disease (HR 1.20, 95% CI: 1.12–1.29) (Table 3 and Supplementary Fig. 3).
Propensity score matching and inverse weighting model
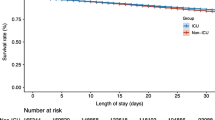
After matching with propensity scores and calculating the inverse weight model (IPW), it was found that sepsis led to an increased risk of one-year mortality with an HR of 2.10 (95% CI: 2.02–2.18) (Table 4). Figure 2 displays one-year survival curves adjusted for Inverse Probability Weighting (IPW).
One-year survival rate and regional mortality
The one-year survival rate in different regions of the country is described in the supplementary Fig. 4. It can be observed that males had an increased mortality risk, expressed with an adjusted HR of 1.11 (95% CI: 1.08–1.14), and age was up to 10 times higher for sepsis patients over 80 years.
Discussion
The proportion of patients diagnosed with sepsis admitted to the ICU was 10.36% (12.054), representing a rate of 54.8 cases per 100.000 person-years in 2019. Both the proportion and the found rate align with what has been reported in the literature. The 30-day sepsis mortality of 15.2% falls within the wide range of mortality reported in various studies, which varies depending on coexisting conditions and the source of sepsis. Regarding comorbidities associated with one-year mortality in the entire patient cohort, renal disease was the leading factor, followed by cancer, liver disease, metastatic neoplastic disease, and, finally, connective tissue diseases. However, the variable with the highest hazard ratio for mortality was age over 80 years, with a ninefold higher risk for octogenarian patients compared to younger patients [13, 15,16,17,18].
Population-level estimates of sepsis incidence and mortality have commonly relied on administrative databases [7, 8]. Oh et al. [9] used data from the Korean National Health Insurance Service to examine patients hospitalized with a sepsis diagnosis. In 2007, the incidence rate was 173.8 cases per 100.000, which increased to 233.6 cases per 100-000 by 2016. Our study showed a rate of ICU-hospitalized patients of 54.8 cases per 100.000 person-years, similar to the rate reported by Fleischmann et al. in a meta-analysis encompassing 30 studies published from 1979 to 2019, which found a rate of 58 cases per 100.000 person-years.
Fleischmann et al. [13] described a lower annualized sepsis incidence between 2010 and 2015 in Germany compared to other studies. This difference was attributed to limitations and biases in administrative data, including omitted clinical diagnoses of sepsis, varying thresholds, and variability in disease diagnosis and coding practices. In our results, we used administrative data, which could have influenced the extrapolation of the findings to the general population, as described by Fleischmann. However, the algorithms used to identify sepsis patients considered not only ICD-10 codes but also the administration of broad-spectrum antibiotics, increasing sensitivity in patient identification.
Abe et al. [17] found that 67.0% of patients had at least one comorbidity, with the most common being diabetes mellitus (23.0%), malignancy (17.7%), cerebrovascular diseases (11.8%), and heart failure (10.8%). Our study aligns with diabetes being the most common coexisting disease in ICU-admitted patients, with chronic obstructive pulmonary disease and systemic arterial hypertension having the highest prevalence. Similar to overall ICU patient mortality, in patients with a sepsis diagnosis, age over 80 years was the variable with the highest one-year mortality risk. Strandberg et al. [19] found an association between age over 80 years and sepsis as the reason for ICU admission (HR = 3.87; 95% CI: 3.44–4.35) and the need for renal replacement therapy in the ICU (HR = 1.11, 95% CI: 1.01–1.21).
In our study, we observed higher mortality among male patients diagnosed with sepsis, while Sakr et al. [20] reported higher mortality in women with severe sepsis compared to men (63.5% vs. 46.4%, p = 0.007). Additionally, we found lower sepsis mortality in regions with more advanced healthcare infrastructure and intensive care facilities. These findings suggest that access to specialized medical care and adequate resources can positively influence sepsis patient outcomes.
Limitations of the study include the inability to determine sepsis severity upon ICU admission due to data source constraints. However, coexisting conditions reported in the Charlson Index were taken into account. Systematic differences between patients admitted with a sepsis diagnosis and those with other diagnoses were assessed through standardized mean differences, and inverse propensity score weighting was employed to adjust hazard ratios obtained.
Conclusions
This study revealed a high one-year sepsis mortality rate in the population, associated with variables such as age over 80 years, the presence of renal disease, liver disease, connective tissue diseases, and cancer. Men exhibited higher mortality compared to women.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Vincent JL. Current sepsis therapeutics. EBioMedicine. 2022;86:104318.
Fleischmann-Struzek C, Mellhammar L, Rose N, Cassini A, Rudd KE, Schlattmann P, et al. Incidence and mortality of hospital- and ICU-treated sepsis: results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 2020;46(8):1552–62.
Bauer M, Gerlach H, Vogelmann T, et al. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit Care. 2020;24(1):239.
Paoli CJ, Reynolds MA, Sinha M, et al. Epidemiology and costs of Sepsis in the United States-An Analysis based on timing of diagnosis and severity level. Crit Care Med. 2018;46(12):1889–97.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of Disease Study. Lancet. 2020;395(10219):200–11.
Srzić I, Nesek Adam V, Tunjić Pejak D. Sepsis definition: what’s new in the treatment guidelines. Acta Clin Croat. 2022;61(Suppl 1):67–72.
Rubens M, Saxena A, Ramamoorthy V, et al. Increasing Sepsis Rates in the United States: results from National Inpatient Sample, 2005 to 2014. J Intensive Care Med. 2020;35(9):858–68.
Holler JG, Jensen JUS, Engsig FN, et al. Existing data sources in clinical epidemiology: database of Community Acquired infections Requiring Hospital Referral in Eastern Denmark (DCAIED) 2018–2021. Clin Epidemiol. 2023;15:939–55.
Oh SY, Cho S, Kim GH, et al. Incidence and outcomes of Sepsis in Korea: a Nationwide Cohort Study from 2007 to 2016. Crit Care Med. 2019;47(12):e993–8.
Abu-Kaf H, Mizrakli Y, Novack V, et al. Long-term survival of young patients surviving ICU admission with severe Sepsis. Crit Care Med. 2018;46(8):1269–75.
Bauer M, Gerlach H, Vogelmann T, et al. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit Care. 2020;24(1):239.
Liu YC, Yao Y, Yu MM, et al. Frequency and mortality of sepsis and septic shock in China: a systematic review and meta-analysis. BMC Infect Dis. 2022;22(1):564.
Fleischmann-Struzek C, Mikolajetz A, Schwarzkopf D, et al. Challenges in assessing the burden of sepsis and understanding the inequalities of sepsis outcomes between National Health Systems: secular trends in sepsis and infection incidence and mortality in Germany. Intensive Care Med. 2018;44(11):1826–35.
Oliveros H, Buitrago G. Validation and adaptation of the Charlson Comorbidity Index using administrative data from the Colombian health system: retrospective cohort study. BMJ Open. 2022;12(3):e054058.
Caraballo C, Ascuntar J, Hincapié C, et al. Association between site of infection and in-hospital mortality in patients with sepsis admitted to emergency departments of tertiary hospitals in Medellin, Colombia. Rev Bras Ter Intensiva. 2019;31(1):47–56.
Mendoza D, Ascuntar J, Rosero O, et al. Improving the diagnosis and prognosis of sepsis according to the sources of infection. Emerg Med J. 2022;39(4):279–83.
Abe T, Ogura H, Shiraishi A, et al. Characteristics, management, and in-hospital mortality among patients with severe sepsis in intensive care units in Japan: the FORECAST study. Crit Care. 2018;22(1):322.
Grande E, Grippo F, Frova L, et al. The increase of sepsis-related mortality in Italy: a nationwide study, 2003–2015. Eur J Clin Microbiol Infect Dis. 2019;38(9):1701–8.
Strandberg G, Walther S, Agvald Öhman C, et al. Mortality after severe Sepsis and septic shock in Swedish intensive care units 2008-2016-A nationwide observational study. Acta Anaesthesiol Scand. 2020;64(7):967–75.
Sakr Y, Elia C, Mascia L, et al. The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care. 2013;17(2):R50.
Acknowledgements
The authors are most thankful for the Universidad de La Sabana.
Funding
This work was supported by Universidad de la Sabana Grant MEDMSc-70-2023.
Author information
Authors and Affiliations
Contributions
HO, ETQ, MP, AG and FR contributed to the conception and design. HO and ETQ supervised the whole process. HO, ETQ, and FR contributed to data collection. HO analyzed and interpreted the patient data. HO, ETQ and FR wrote major parts of the manuscript. HO, ETQ, MP, AG and FR revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the principles of the current Helsinki Declaration, as well as local, regional, and international regulations pertaining to clinical research, including Colombian Law on Biomedical Research. Ethical approval was obtained from the Medical Ethics Committee of the Universidad de La Sabana (approval number: 450-9Nov2018). Prior to participating in the study, all participants provided written informed consent, and the confidentiality of their data was strictly maintained throughout the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Oliveros, H., Tuta-Quintero, E., Piñeros, M. et al. One-year survival of patients admitted for sepsis to intensive care units in Colombia. BMC Infect Dis 24, 678 (2024). https://doi.org/10.1186/s12879-024-09584-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09584-7