Abstract
Liver injury with marked elevation of aspartate aminotransferase enzyme (AST) is commonly observed in dengue infection. To understand the pathogenesis of this liver damage, we compared the plasma levels of hepatic specific, centrilobular predominant enzymes (glutamate dehydrogenase, GLDH; glutathione S transferase-α, αGST), periportal enriched 4-hydroxyphenylpyruvate dioxygenase (HPPD), periportal predominant arginase-1 (ARG-1), and other non-specific biomarkers (paraoxonase-1, PON-1) in patients with different outcomes of dengue infection. This hospital-based study enrolled 87 adult dengue patients, stratified into three groups based on plasma AST levels (< 80, 80–400, > 400 U/L) in a 1:1:1 ratio (n = 40, n = 40, n = 40, respectively. The new liver enzymes in the blood samples from the 4th to 6th days of their illness were measured by commercial enzyme-linked immunosorbent assay (ELISA) or colorimetric kits. Based on the diagnosis at discharge days, our patients were classified as 40 (46%) dengue without warning signs (D), 35 (40.2%) dengue with warning signs (DWS), and 11 (12.6%) severe dengue (SD) with either shock (two patients) or AST level over 1000 U/L (nine patients), using the 2009 WHO classification. The group of high AST (> 400 U/L) also had higher ALT, GLDH, ARG-1, and HPPD than the other groups, while the high (> 400 U/L) and moderate (80–400 U/L) AST groups had higher ALT, αGST, ARG-1, and HPPD than the low AST group (< 80 U/L). There was a good correlation between AST, alanine aminotransferase enzyme (ALT), and the new liver biomarkers such as GLDH, αGST, ARG-1, and HPPD. Our findings suggest that dengue-induced liver damage initiates predominantly in the centrilobular area toward the portal area during the dengue progression. Moreover, these new biomarkers should be investigated further to explain the pathogenesis of dengue and to validate their prognostic utility.
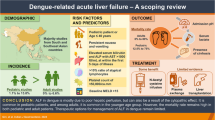
Key messages
Arginase-1, α-glutathione S transferase, and 4-hydroxyphenylpyruvate dioxygenase levels were significantly associated with dengue severity and can serve as good prognostic predictors for liver injury.
Our findings suggest that dengue-induced liver damage initiates predominantly in the centrilobular area toward the portal area during the dengue progression.
Similar content being viewed by others
Introduction
Dengue is currently prevalent in 125 countries worldwide, with two-fifths of the world’s population at risk, and affects approximately 100 million people every year [1]. This number is estimated to increase in the near and distant future due to the suitability of climate and environment [2]. The spectrum of dengue infection ranges from an asymptomatic condition to a severe disease [3, 4]. The 2009 World Health Organization (WHO) guidelines classify dengue infection severity into three main groups including dengue without warning signs (D), dengue with warning signs (DWS), and severe dengue (SD) based on clinical manifestations (vomiting, abdominal pain, hemorrhage), organ dysfunction (liver, renal, coagulation disorders) or shock (related to vascular permeability) [3].
Organ involvement has often been considered in dengue patients. Particularly, hepatic dysfunction is a well-recognized complication of this condition, with elevated AST and ALT occurring in 86% and 46%, respectively [5, 6]. Liver dysfunction is attributed to apoptosis of hepatocytes, hypoperfusion, and hypoxic damage of liver cells due to plasma leakage, oxidative stress, or immune-mediated liver injury [7,8,9].
Acute dengue infection can lead to varying degrees of liver damage (LD) that can be detected from the elevation of transaminases, hepatomegaly, jaundice, and even acute liver failure with hepatic encephalopathy. Acute liver failure can be fatal, especially if it presents in patients with coagulation disorders, renal dysfunction, and metabolic derangements [10,11,12,13,14]. Liver involvement with extremely high transaminases can fully resolve as the acute infection recovers [12]. A major chunk (65–97%) of dengue patients with hepatic derangement has the maximum rise in hepatic aspartate aminotransferase (AST) and alanine aminotransferase (ALT) at convalescence (days 7–10) [15, 16].
The liver dysfunction in dengue is measured in terms of the rise in AST levels, where higher values are associated with a more severe condition, development of complications, and prolonged stay in the hospital. Elevation of AST is therefore considered a prognostic marker and marker for severity classification [6, 17, 18]. Indeed, our previous systematic review and meta-analysis found a significant association between AST and SD [19]. LD biomarkers such as glutamate dehydrogenase (GLDH), glutathione S transferase-α (αGST), arginase-1 (ARG-1), paraoxonase-1 (PON-1), and 4-hydroxyphenylpyruvate dioxygenase (HPPD) have been recently investigated in numerous liver involvement, especially in drug-induced hepatic impairment. Previous studies report that GLDH [20,21,22] and αGST [23, 24] are mainly present in the hepatic centrilobular area, HPPD, also known as F-protein, is expressed in all hepatocytes and enriches in the periportal region [22, 23, 25, 26], while ARG-1 is highly found in the portal area [26,27,28].
We, therefore, conducted this study to assess these new markers of LD in Dengue patients and to explore the characteristics of hepatic zonal damage in dengue infection.
Methods
Ethical statement
This case-control study was performed on adult dengue patients in the Hospital for Tropical Diseases of Ho Chi Minh City, Vietnam. The study was approved by the institutional review board of the Hospital for Tropical Diseases of Ho Chi Minh City (ID: 1104/QD-BVND). Written informed consent was obtained from each patient upon enrollment. All the methods followed the relevant approved regulations, guidelines, and declaration of Helsinki.
Participants’ enrollment
We enrolled all dengue patients presenting to our setting between October 2015 and December 2016 on days 4 to 6 of dengue illness based on either a positive dengue IgM or non-structural protein 1 (NS1).
All hospitalized dengue cases during the study period were eligible for selection and were then stratified into three groups of equal size based on their plasma AST levels: less than 80 U/L, 80–400 U/L, and greater than 400 U/L (Fig. 1). All included patients satisfied the 2009 WHO criteria for dengue diagnosis [3] and were positive for dengue IgM or NS1. Accordingly, patient severity was classified at both admission and discharge. Patients were recruited from normal wards for dengue-infected patients or from the ICU if they were transferred due to shock. However, patients with shock at enrollment were excluded, as AST levels can be elevated in individuals with hypoperfusion [6, 17, 18]. Non-laboratory-confirmed cases were also excluded.
Sample collection
A venous blood sample was collected in EDTA tubes on the 4th – 6th day of illness. Plasma was separated by centrifugation at 1000 × g for 10 min and was stored at -20° until used for the enzyme testing.
Dengue confirmation
All cases were diagnosed as dengue patients if they had positive results for either dengue NS1 protein on the 1st – 4th day or IgM against dengue virus on the 6th day of illness (in case they were negative for NS1) using SD BIOLINE Dengue Duo Strip Kit (Standard Diagnostic Inc., Korea).
Liver enzymes and liver span measurement
Plasma αGST level was measured by sandwich ELISA using (GS41 2kit, Oxford Biomedical Research, Inc., USA), which does not cross-react with mu, theta or pi variants. HPPD was detected by the sandwich ELISA kit (ABIN419893 2kit) produced by Abbiotec™ (USA). ARG-1 was also quantified using the ELISA kit (EH1274, FineTest Biotech Co. Montgomery, TX, The Netherlands). Colorimetric assays were applied to quantify GLDH (ab102527 kit, Abcam Inc.), and PON-1 (Paraoxonase Enzyme Activity Assay Kit, Baran Medikal) according to the manufacturer’s instructions. Liver spans were measured using ultrasound.
Statistical analysis
The skewness and kurtosis tests were used to test the normal distribution of continuous variables. Frequencies and percentages were used to describe categorical variables. The Chi-squared test (or Fisher’s exact test, as appropriate) was used for categorical data. Student’s t-test (one-way ANOVA test for > 2 groups comparisons) was used for normally distributed continuous variables while the Kruskal-Wallis H test was used for continuous non-normally distributed variables. The correlation was analyzed using the Spearman-rank test. Data were analyzed using MedCalc version 14.8.1 and RStudio software version 3.2.4. The data for patients and the R script can be obtained from the authors. Results were considered statistically significant with p < 0.05.
Results
Patients’ characteristics
A total of 87 dengue adult patients were enrolled into three equal groups based on plasma AST levels (< 80, 80–400, > 400 U/l), where 29 patients were equally allocated to each group. In our sample, we had 50 (57.5%) dengue (D) cases, 29 (33.3%), dengue with a warning sign (DWS), and 8 (9.2%) severe dengue cases (SD) with AST > 1000 U/L according to the 2009 WHO severity classification (Fig. 1). The median (IQR) age was 24 (18–34), and the median (IQR) duration of fever was 5 (5–6) days.
At discharge, there were 2 (2.3%) cases with shock (DS), 10 cases without shock but with AST > 1000 U/L (11.5%, included 2 progressing cases), 35 cases of dengue with warning signs (DWS) (40.2%, includes 6 progressing cases) and 40 cases (46%) dengue (D).
The median (IQR) of variables of the study population were described as ALT 91 (34–290) U/L, GLDH 4.01 (2.83–5.42) U/L, αGST 10.19 (6.92–14.56) ng/mL, ARG-1 101.18 (70.43-181.75) ng/mL, PON-1 9.99 (6.77–13.76) U/L and HPPD 827.05 (600.28-1056.53) ng/mL.
Characteristics and value of biomarkers of three AST groups
The group of moderate AST (80–400 U/L) was older than the others (median age was 32 vs. 22 and 23) (p = 0.01). BMI differences existed among the high, moderate, and low groups of AST (p = 0.03) with higher BMI in the moderate and high AST groups than in the low AST group. The group of high AST (> 400 U/L) had also higher ALT, GLDH, ARG-1, and HPPD than the other groups while the high (> 400 U/L) and moderated (80–400 U/L) AST group had higher ALT, αGST, ARG-1, and HPPD than the low AST group (< 80 U/L). The values of PON were not different between the three groups (Table 1).
Our co-efficient correlation analysis revealed significant correlations among GLDH with αGST (p = 0.002), ARG-1 (p = 0.01), and HPPD (p < 0.001); among αGST with ARG-1 (p = 0.001), HPPD (p < 0.001) and minimal platelets count (p = 0.003) and among ARG-1 with HPPD (p < 0.001). We also found a correlation between PON-1 and liver span. Moreover, there were significant correlations among AST and each of ALT (p < 0.001), GLDH (p = 0.003), αGST (p < 0.001), ARG-1 (p < 0.001), HPPD (p < 0.001), minimal platelets count (p < 0.001), and liver span (p = 0.047) while ALT was also significantly correlated with GLDH (p = 0.009), αGST (p < 0.001), ARG-1 (p < 0.001), HPPD (p < 0.001), and minimal platelets count (p < 0.001), but not with liver span (Fig. 2).
A Correlation matrix of different liver enzymes with each other and with the liver span, as well as minimal platelets, count. Abbreviations; AST = Aspartate transaminase, ALT = Alanine transaminase, HPPD = 4-Hydroxyphenylpyruvate dioxygenase, PON-1 = Paraoxonase-1, GLDH = Glutamate Dehydrogenase, ARG-1 = Arginase-1, αGST = Glutathione S Transferase-α. Correlation findings by Spearman-rank test. Significant correlations are in bold. Patients’ number = 87 for all variables
Discussion
In our study, we found that the group with AST > 400 U/L had higher ALT, GLDH, αGST, ARG-1, and HPPD. Interestingly, our findings suggest that dengue-induced liver damage is initiated predominantly in the centrilobular area toward the portal area during the dengue progression. This progression is against the direction of blood supply which follows from portal veins and hepatic arteries draining in central veins, at centrilobular zones.
Additionally, despite a remarkably uniform anatomical structure consisting of hexagon-shaped lobules, liver parenchyma is heterogeneous in terms of cell types and functional origination. Key liver metabolic enzymes are expressed differently within different (periportal, midzonal, or centrilobular) zones on the long porto-central axis of the hepatic lobules, a phenomenon termed metabolic zonation [22, 29, 30]. ARG-1 and HPPD are associated with severe dengue, which can be attributed to the predominant of these enzymes in the periportal zones of the hepatic lobules [31]. Also, ALT and AST have a pan-lobular distribution but more predominantly in periportal areas [22, 23]. Subsequently, periportal zones are more affected in severe cases. However, a specific periportal enzyme (like ARG-1, HPPD) may better prognose the severity of liver injury than other enzymes that show less prominence in the periportal area compared to the centrilobular area, like AST and ALT.
The exact etiology of this direction in liver injury progression is still unknown but it can be attributed to many factors. It can be suggested that this track and sequence of liver damage is due to the dependence of the centrilobular area on the hepatic veins with lower oxygen gradient, unlike the periportal area on the hepatic arteries [29], making centrilobular areas more liable for injury and damage which suggest, in part, a hypoxemic injury. Subsequently, dengue infection can affect the vascular supply to the liver with vascular leakage and endothelial damage [32]. This may lead to increased oxygen free radicals and mediators which finally cause tissue damage [33].
Furthermore, the centrilobular zone of the liver is considered a vulnerable zone in many cases such as hypoxia, toxins, metabolic disorders, drugs, and inflammatory conditions. This is due to the low oxygen concentration and enzymes as described. The centrilobular zone is assumed to be the first affected zone in viral hepatitis and autoimmune hepatitis [34,35,36,37]. Also, the centrilobular zone has a higher activity of Kupffer cells than the periportal zone, although it is more numerous in the periportal zone [22]. Notably, the Kupffer cell is one of the main target cells in dengue infection, which may explain the liability of damage in the centrilobular zone in dengue [32].
Indeed, Kuo et al. suggest that dengue may cause a hepatic injury and transaminase rise akin to that in patients with conventional viral hepatitis [38]. Further, Chen et al. revealed a strong correlation between hepatic cellular infiltration and T-cell activation in immunocompetent mice infected with dengue. Moreover, they also found that the kinetics of hepatic enzyme elevation correlated with that of T-cell activation and suggested a relationship between the elevation of liver enzymes and T-cell infiltration [39].
Similarly, biopsy specimens from dead DSS patients reveal various forms of liver injury with hepatocellular necrosis, Kupffer cell (KC) hyperplasia and destruction, microvesicular steatosis, and a pauci-cellular inflammatory infiltrate being the most common histological features [6, 40,41,42,43,44,45]. Hepatocellular necrosis varies from mild focal necrosis with Councilman bodies to severe submassive and massive necrosis affecting all zones of the hepatic lobules. Interestingly, in dengue cases with mild liver injury, lesions are mainly observed at mid-zonal and centrilobular areas [42, 43, 46].
Moreover, dengue virus was often isolated from Kupffer cells, endothelial cells, and hepatocytes at injured sites [41, 47,48,49], suggesting a direct effect of dengue virus-induced hepatocellular necrosis. Also, Seneviratnea et al. show that the dengue virus is capable of replicating in hepatocytes and KC and dysregulated host immune responses may have a significant causative role in the LD. In contrast to the plasma ALT, GLDH had a 10-fold greater magnitude and persisted longer. Moreover, serum GLDH is more liver-specific than transaminases and is not substantially affected by skeletal muscle damage [50, 51].
The HPPD was a more sensitive and specific biomarker of LD than AST and revealed a close correlation with the histological assessment of LD [52]. Similarly, αGST was found in a high concentration in centrilobular cells and hence is more sensitive to LD in this liver metabolic zone [51]. In addition, the fold increase of αGST is more than serum transaminases but less than GLDH [53]. Akin to ALT, the activity of GLDH rises with the LD severity [50, 54]. Larger ranges of some GLDH and HPPD should be considered in observation studies and differentiate the severity of LD.
Ashamiss et al. suggested ARG-1 as a highly liver-specific biomarker with a higher specificity compared to other liver enzymes [55]. Our previous systematic review and meta-analysis disclosed an association between thrombocytopenia and dengue severity [19], following the WHO recommendation of using low platelets count as a warning sign in dengue [3].
This study had three limitations. Firstly, the reversal correlation between minimum platelet count and AST, ALT, αGST, and HPPD may be due to the independent associations of both platelet count and liver enzymes with disease severity, by various systemic mechanisms [6, 56,57,58]. However, platelets may play important local specific effects on liver injury. Platelets recruited to the liver, on the one hand, increased platelet destruction. On the other hand, they can form clots and extravasated platelet aggregation leading to hepatic microcirculatory dysfunction and worsening hepatic hypoperfusion. Moreover, activated platelets can exaggerate hepatocellular necrosis by releasing mediators such as serotonin or by promoting the accumulation of other inflammatory cells in the liver, including T-lymphocytes [59, 60]. Secondly, sampling methods may not be ideal since blood samples were taken at a single timepoint from day 4 to 6, while different liver enzymes have different peaks after injury. The sample size of this study may limit the generalizability of our findings. Moreover, this study may pose some concerns about information bias because some patients were more closely monitored in the ICU. Hence, adverse events were more likely to be readily spotted. However, this study followed the same methodology of previous projects that aimed at investigating similar exposures and outcomes [5, 61, 62]. Thirdly, there might be cross-reactivities among IgM in dengue and other flavivirus infections that potentially affect the accuracy of dengue classification [63]. However, we did not merely rely on IgM, but also other clinical and sub-clinical criteria for the diagnosis. Due to the above limitations, all studies conducted to date, including ours, should not be used for outcome prediction. Subsequently, it is not in our capacity to draw firm conclusions about the predictability of our findings.
Conclusions
By studying 87 dengue cases, we found a significant correlation between AST, ALT, and the new liver biomarkers, including GLDH, αGST, ARG-1, and HPPD. Our findings suggest a possible progression of dengue-induced liver damage starting in the centrilobular area (where GLDH and αGST are predominantly found) and moving towards the periportal area (where HPPD and ARG-1 are primarily located) during the disease. Moreover, HPPD, ARG-1, GLDH, and αGST could potentially serve as good markers of dengue severity. However, further validation with larger studies and the development of predictive models incorporating these novel biomarkers is crucial for healthcare providers, enabling them to predict patient outcomes and make informed decisions in dengue management.
Data availability
The data used in this manuscript can be provided upon request from the corresponding author.
Abbreviations
- αGST:
-
Glutathione S Transferase-α
- ALT:
-
Alanine Aminotransferase Enzyme
- ARG-1:
-
Arginase-1
- AST:
-
Aspartate Aminotransferase Enzyme
- D:
-
Dengue without warning signs
- DWS:
-
Dengue with Warning Signs
- EDTA:
-
Ethylenediaminetetraacetic Acid
- ELISA:
-
Enzyme-Linked Immunosorbent Assay
- GLDH:
-
Glutamate Dehydrogenase
- HPPD:
-
4-Hydroxyphenylpyruvate Dioxygenase
- ICU:
-
Intensive Care Unit
- KC:
-
Kuffer Cell
- LD:
-
• Liver Damage
- LQAS:
-
Lot Quality Assurance Sampling
- NS-1:
-
Non-Structural protein 1
- PON-1:
-
Paraoxonase-1
- SD:
-
Severe Dengue
- WHO:
-
World Health Organization
References
Zeng Z, Zhan J, Chen L, Chen H, Cheng S. Global, regional, and national dengue burden from 1990 to 2017: a systematic analysis based on the global burden of disease study 2017. EClinicalMedicine. 2021;32:100712. https://doi.org/10.1016/j.eclinm.2020.100712.
Messina JP, Brady OJ, Pigott DM, Golding N, Kraemer MU, Scott TW, et al. The many projected futures of dengue. Nat Rev Microbiol. 2015;13(4):230–9. https://doi.org/10.1038/nrmicro3430.
Dengue W. Guidelines for diagnosis, treatment. Prevention and Control Geneva: World Health Organization; 2009.
Kamel MG, Nam NT, Han NHB, El-Shabouny AE, Makram AM, Abd-Elhay FA, et al. Post-dengue acute disseminated encephalomyelitis: a case report and meta-analysis. PLoS Negl Trop Dis. 2017;11(6):e0005715. https://doi.org/10.1371/journal.pntd.0005715.
Lee LK, Gan VC, Lee VJ, Tan AS, Leo YS, Lye DC. Clinical relevance and discriminatory value of elevated liver aminotransferase levels for dengue severity. PLoS Negl Trop Dis. 2012;6(6):e1676. https://doi.org/10.1371/journal.pntd.0001676.
Seneviratne SL, Malavige GN, de Silva HJ. Pathogenesis of liver involvement during dengue viral infections. Trans R Soc Trop Med Hyg. 2006;100(7):608–14. https://doi.org/10.1016/j.trstmh.2005.10.007.
Diamond MS, Edgil D, Roberts TG, Lu B, Harris E. Infection of human cells by dengue virus is modulated by different cell types and viral strains. J Virol. 2000;74(17):7814–23.
Martina BE, Koraka P, Osterhaus AD. Dengue virus pathogenesis: an integrated view. Clin Microbiol Rev. 2009;22(4):564–81. https://doi.org/10.1128/CMR.00035-09.
Gil L, Martinez G, Tapanes R, Castro O, Gonzalez D, Bernardo L, et al. Oxidative stress in adult dengue patients. Am J Trop Med Hyg. 2004;71(5):652–7.
Wiwanitkit V. Liver dysfunction in Dengue infection: an analysis of the previously published Thai cases. J Ayub Med Coll Abbottabad. 2007;19(1):10–2.
Malavige G, Ranatunga P, Jayaratne S, Wijesiriwardana B, Seneviratne S, Karunatilaka D. Dengue viral infections as a cause of encephalopathy. Ind J Med Microbiol. 2007;25(2):143.
Hien TT, Vinh NN, Hien PTD, Chinh NT, Simmons C, Wills B. Liver involvement associated with dengue infection in adults in Vietnam. Am J Trop Med Hyg. 2010;83(4):774–80.
Sedhain A, Adhikari S, Regmi S, Chaudhari S, Shah M, Shrestha B. Fulminant hepatic failure due to dengue. Kathmandu Univ Med J. 2012;9(2):73–5.
Itha S, Kashyap R, Krishnani N, Saraswat VA, Choudhuri G, Aggarwal R. Profile of liver involvement in dengue virus infection. Natl Med J India. 2005;18(3):127–30.
Souza LJ, Alves JG, Nogueira RM, Gicovate Neto C, Bastos DA, Siqueira EW, et al. Aminotransferase changes and acute hepatitis in patients with dengue fever: analysis of 1,585 cases. Braz J Infect Dis. 2004;8(2):156–63. https://doi.org/10.1590/s1413-86702004000200006.
Lee VJ, Lye DC, Sun Y, Fernandez G, Ong A, Leo YS. Predictive value of simple clinical and laboratory variables for dengue hemorrhagic fever in adults. J Clin Virol. 2008;42(1):34–9. https://doi.org/10.1016/j.jcv.2007.12.017.
Rangani M, Trivedi D, Patel K, Patel R. Study of Dengue Fever with Outcome Analysis in patients with normal and abnormal liver function tests. Indian Practitioner. 2016;69(9):11–6.
Uchadadia S, Ghodke B, Bhuta K, Kejriwal A, Ghanekar J. Degree of impairment of liver function in Dengue Fever correlates to the severity of its complications. 2015.
Huy NT, Van Giang T, Thuy DH, Kikuchi M, Hien TT, Zamora J, et al. Factors associated with dengue shock syndrome: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2013;7(9):e2412. https://doi.org/10.1371/journal.pntd.0002412.
Van Waes L, Lieber CS. Glutamate dehydrogenase: a reliable marker of liver cell necrosis in the alcoholic. Br Med J. 1977;2(6101):1508–10. https://doi.org/10.1136/bmj.2.6101.1508.
Racine-Samson L, Scoazec JY, D’Errico A, Fiorentino M, Christa L, Moreau A, et al. The metabolic organization of the adult human liver: a comparative study of normal, fibrotic, and cirrhotic liver tissue. Hepatology (Baltimore MD). 1996;24(1):104–13. https://doi.org/10.1002/hep.510240118.
Gebhardt R. Metabolic zonation of the liver: regulation and implications for liver function. Pharmacol Ther. 1992;53(3):275–354. https://doi.org/10.1016/0163-7258(92)90055-5.
Beckett GJ, Foster GR, Hussey AJ, Oliveira DB, Donovan JW, Prescott LF, et al. Plasma glutathione S-transferase and F protein are more sensitive than alanine aminotransferase as markers of Paracetamol (acetaminophen)-induced liver damage. Clin Chem. 1989;35(11):2186–9.
Beckett GJ, Chapman BJ, Dyson EH, Hayes JD. Plasma glutathione S-transferase measurements after Paracetamol overdose: evidence for early hepatocellular damage. Gut. 1985;26(1):26–31. https://doi.org/10.1136/gut.26.1.26.
Fagerberg L, Hallstrom BM, Oksvold P, Kampf C, Djureinovic D, Odeberg J, et al. Mol Cell proteomics: MCP. 2014;13(2):397–406. https://doi.org/10.1074/mcp.M113.035600. Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics.
Desert R, Rohart F, Canal F, Sicard M, Desille M, Renaud S, et al. Human hepatocellular carcinomas with a periportal phenotype have the lowest potential for early recurrence after curative resection. Hepatology (Baltimore MD). 2017;66(5):1502–18. https://doi.org/10.1002/hep.29254.
Zeng QL, Yang B, Sun HQ, Feng GH, Jin L, Zou ZS, et al. Myeloid-derived suppressor cells are associated with viral persistence and downregulation of TCR zeta chain expression on CD8(+) T cells in chronic hepatitis C patients. Mol Cells. 2014;37(1):66–73. https://doi.org/10.14348/molcells.2014.2282.
Sekine S, Ogawa R, McManus MT, Kanai Y, Hebrok M. Dicer is required for proper liver zonation. J Pathol. 2009;219(3):365–72. https://doi.org/10.1002/path.2606.
Kietzmann T. Metabolic zonation of the liver: the oxygen gradient revisited. Redox Biol. 2017;11:622–30. https://doi.org/10.1016/j.redox.2017.01.012.
Halpern KB, Shenhav R, Matcovitch-Natan O, Toth B, Lemze D, Golan M, et al. Single-cell spatial reconstruction reveals global division of labour in the mammalian liver. Nature. 2017;542(7641):352–6. https://doi.org/10.1038/nature21065.
Bailey WJ, Holder D, Patel H, Devlin P, Gonzalez RJ, Hamilton V, et al. A performance evaluation of three drug-induced liver injury biomarkers in the rat: alpha-glutathione S-transferase, arginase 1, and 4-hydroxyphenyl-pyruvate dioxygenase. Toxicol Sci. 2012;130(2):229–44. https://doi.org/10.1093/toxsci/kfs243.
Paessler S, Walker DH. Pathogenesis of the viral hemorrhagic fevers. Annu Rev Pathol. 2013;8:411–40. https://doi.org/10.1146/annurev-pathol-020712-164041.
Ebert EC. Hypoxic liver injury. Mayo Clin Proc. 2006;81(9):1232-6. https://doi.org/10.4065/81.9.1232.
Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, Gudat F, et al. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22(6):696–9. https://doi.org/10.1016/0168-8278(95)80226-6.
Kudryavtseva MV, Sakuta GA, Skorina AD, Stein GI, Emelyanov AV, Kudryavtsev BN. Quantitative analysis of glycogen content in hepatocytes of portal and central lobule zones of normal human liver and in patients with chronic hepatitis of different etiology. Tissue Cell. 1996;28(3):279–85. https://doi.org/10.1016/s0040-8166(96)80015-2.
Nguyen Canh H, Harada K, Ouchi H, Sato Y, Tsuneyama K, Kage M, et al. Acute presentation of autoimmune hepatitis: a multicentre study with detailed histological evaluation in a large cohort of patients. J Clin Pathol. 2017;70(11):961–9. https://doi.org/10.1136/jclinpath-2016-204271.
Hofer H, Oesterreicher C, Wrba F, Ferenci P, Penner E. Centrilobular necrosis in autoimmune hepatitis: a histological feature associated with acute clinical presentation. J Clin Pathol. 2006;59(3):246–9. https://doi.org/10.1136/jcp.2005.029348.
Kuo CH, Tai DI, Chang-Chien CS, Lan CK, Chiou SS, Liaw YF. Liver biochemical tests and dengue fever. Am J Trop Med Hyg. 1992;47(3):265–70. https://doi.org/10.4269/ajtmh.1992.47.265.
Chen HC, Lai SY, Sung JM, Lee SH, Lin YC, Wang WK, et al. Lymphocyte activation and hepatic cellular infiltration in immunocompetent mice infected by dengue virus. J Med Virol. 2004;73(3):419–31. https://doi.org/10.1002/jmv.20108.
Bhamarapravati N. Hemostatic defects in dengue hemorrhagic fever. Rev Infect Dis. 1989;11 Suppl 4(Supplement_4):S826-9. https://doi.org/10.1093/clinids/11.supplement_4.s826.
Huerre MR, Lan NT, Marianneau P, Hue NB, Khun H, Hung NT, et al. Liver histopathology and biological correlates in five cases of fatal dengue fever in Vietnamese children. Virchows Arch. 2001;438(2):107–15. https://doi.org/10.1007/s004280000329.
Bhamarapravati N, Tuchinda P, Boonyapaknavik V. Pathology of Thailand haemorrhagic fever: a study of 100 autopsy cases. Ann Trop Med Parasitol. 1967;61(4):500–10. https://doi.org/10.1080/00034983.1967.11686519.
de Macedo FC, Nicol AF, Cooper LD, Yearsley M, Pires AR, Nuovo GJ. Histologic, viral, and molecular correlates of dengue fever infection of the liver using highly sensitive immunohistochemistry. Diagn Mol Pathology: Am J Surg Pathol part B. 2006;15(4):223–8. https://doi.org/10.1097/01.pdm.0000213462.60645.cd.
Aye KS, Charngkaew K, Win N, Wai KZ, Moe K, Punyadee N, et al. Pathologic highlights of dengue hemorrhagic fever in 13 autopsy cases from Myanmar. Hum Pathol. 2014;45(6):1221–33. https://doi.org/10.1016/j.humpath.2014.01.022.
Kularatne SA, Imbulpitiya IV, Abeysekera RA, Waduge RN, Rajapakse RP, Weerakoon KG. Extensive haemorrhagic necrosis of liver is an unpredictable fatal complication in dengue infection: a postmortem study. BMC Infect Dis. 2014;14(1):141. https://doi.org/10.1186/1471-2334-14-141.
Fernando S, Wijewickrama A, Gomes L, Punchihewa CT, Madusanka SD, Dissanayake H, et al. Patterns and causes of liver involvement in acute dengue infection. BMC Infect Dis. 2016;16(1):319. https://doi.org/10.1186/s12879-016-1656-2.
Rosen L, Khin MM, Tin U. Recovery of virus from the liver of children with fatal dengue: reflections on the pathogenesis of the disease and its possible analogy with that of yellow fever. Res Virol. 1989;140:351–60.
Rosen L, Drouet MT, Deubel V. Detection of dengue virus RNA by reverse transcription-polymerase chain reaction in the liver and lymphoid organs but not in the brain in fatal human infection. Am J Trop Med Hyg. 1999;61(5):720–4. https://doi.org/10.4269/ajtmh.1999.61.720.
Jessie K, Fong MY, Devi S, Lam SK, Wong KT. Localization of dengue virus in naturally infected human tissues, by immunohistochemistry and in situ hybridization. J Infect Dis. 2004;189(8):1411–8. https://doi.org/10.1086/383043.
O’brien P, Slaughter M, Polley S, Kramer K. Advantages of glutamate dehydrogenase as a blood biomarker of acute hepatic injury in rats. Lab Anim. 2002;36(3):313–21.
Ozer J, Ratner M, Shaw M, Bailey W, Schomaker S. The current state of serum biomarkers of hepatotoxicity. Toxicology. 2008;245(3):194–205. https://doi.org/10.1016/j.tox.2007.11.021.
Foster GR, Goldin RD, Oliveira DB. Serum F protein: a new sensitive and specific test of hepatocellular damage. Clin Chim Acta. 1989;184(1):85–92. https://doi.org/10.1016/0009-8981(89)90259-3.
Giffen PS, Pick CR, Price MA, Williams A, York MJ. Alpha-glutathione S-transferase in the assessment of hepatotoxicity–its diagnostic utility in comparison with other recognized markers in the Wistar Han rat. Toxicol Pathol. 2002;30(3):365–72. https://doi.org/10.1080/01926230252929945.
Giffen PS, Turton J, Andrews CM, Barrett P, Clarke CJ, Fung KW, et al. Markers of experimental acute inflammation in the Wistar Han rat with particular reference to haptoglobin and C-reactive protein. Arch Toxicol. 2003;77(7):392–402. https://doi.org/10.1007/s00204-003-0458-7.
Ashamiss F, Wierzbicki Z, Chrzanowska A, Scibior D, Pacholczyk M, Kosieradzki M, et al. Clinical significance of arginase after liver transplantation. Ann Transplant. 2003;9(3):58–60.
Zapata JC, Cox D, Salvato MS. The role of platelets in the pathogenesis of viral hemorrhagic fevers. PLoS Negl Trop Dis. 2014;8(6):e2858. https://doi.org/10.1371/journal.pntd.0002858.
Ojha A, Nandi D, Batra H, Singhal R, Annarapu GK, Bhattacharyya S, et al. Platelet activation determines the severity of thrombocytopenia in dengue infection. Sci Rep. 2017;7:41697. https://doi.org/10.1038/srep41697.
Dissanayake HA, Seneviratne SL. Liver involvement in dengue viral infections. Rev Med Virol. 2018;28(2):e1971. https://doi.org/10.1002/rmv.1971.
Nowatari T, Murata S, Fukunaga K, Ohkohchi N. Role of platelets in chronic liver disease and acute liver injury. Hepatol Research: Official J Japan Soc Hepatol. 2014;44(2):165–72. https://doi.org/10.1111/hepr.12205.
Tajima H, Ohta T, Miyashita T, Nakanuma S, Matoba M, Miyata T, et al. Oxaliplatin-based chemotherapy induces extravasated platelet aggregation in the liver. Mol Clin Oncol. 2015;3(3):555–8. https://doi.org/10.3892/mco.2015.512.
Ayaz F, Furrukh M. Assessment of Severity of Dengue Fever by Deranged Alanine aminotransferase levels. Cureus. 2020;12(9):e10539. https://doi.org/10.7759/cureus.10539.
Parkash O, Almas A, Jafri SM, Hamid S, Akhtar J, Alishah H. Severity of acute hepatitis and its outcome in patients with dengue fever in a tertiary care hospital Karachi, Pakistan (South Asia). BMC Gastroenterol. 2010;10(1):43. https://doi.org/10.1186/1471-230X-10-43.
Rathore APS, St John AL. Cross-reactive immunity among flaviviruses. Front Immunol. 2020;11:334. https://doi.org/10.3389/fimmu.2020.00334.
Acknowledgements
We thank Dr. Abdelrahman Tarek Mohammed, Faculty of Medicine, Al-Azhar University, Cairo, Egypt (Email: abdelrahmant.mohammed@azhar.edu.eg), for his early contribution to the writing of an earlier version of this study.
Funding
This work was supported in part by a “Grant-in-Aid for Scientific Research (B)” (16H05844, 2016–2019 for Nguyen Tien Huy) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan and by the Japan Initiative for Global Research Network on Infectious Diseases (J-GRID) for Kenji Hirayama. The funders had no role in the study design, data collection and analysis, publication decision, or manuscript preparation. The open access fees are covered by the Egyptian Knowledge Bank for Dr. Abdelrahman M Makram.
Author information
Authors and Affiliations
Contributions
N.T.C.H., P.T.L.H., N.V.V.C., and N.T.H. were responsible for the idea and study design. N.T.C.H., P.T.L.H., N.P.H., N.T.T., N.T.V., and N.V.V.C. collected the data and performed the experiments. N.T.C.H., P.T.L.H., M.G.K., A.M.M., C.V.K., K.H., and N.T.H. analyzed the data and interpreted it. N.T.C.H., P.T.L.H., C.V.K., M.G.K., A.M.M., R.E., A.E., K.H., and N.T.H. wrote the manuscript. All authors reviewed the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Ethical approval
The study was approved by the institutional review board of the Hospital for Tropical Diseases of Ho Chi Minh City (ID: 1104/QD-BVND). All procedures performed in this study followed the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Written informed consent was obtained from each patient upon enrollment.
Consent to publish
All authors reviewed the manuscript and approved the final version before publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huong, N.T.C., Hai, N.P., Van Khanh, C. et al. New biomarkers for liver involvement by dengue infection in adult Vietnamese patients: a case-control study. BMC Infect Dis 24, 800 (2024). https://doi.org/10.1186/s12879-024-09527-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09527-2