Abstract
Background
Hemorrhagic varicella (HV) is a particular form of chicken pox.,with high mortality in adults. This form of the disease is rare, to date, approximately 4 cases have been reported. Occasional cases of HV have been documented in adults with hematologic disorders or other diseases. While there is one reported case of simultaneous reactivation of cytomegalovirus in an adult with chickenpox, there is a lack of information regarding changes in liver function indicators for such patients. This is unfortunate, as CMV reactivation can further exacerbate liver failure and increase mortality. In this report, we present a case of hemorrhagic varicella reactivation with cytomegalovirus and provide some relevant discussions.
Case presentation
We present the case of a 25-year-old male with HV, who had a history of nephrotic syndrome generally controlled with orally administered prednisone at a dosage of 50 mg per day for two months. The patient arrived at the emergency room with complaints of abdominal pain and the presence of hemorrhagic vesicles on his body for the past 3 days. Despite medical evaluation, a clear diagnosis was not immediately determined. Upon admission, the leukocyte count was recorded as 20.96 × 109/L on the first day, leading to the initiation of broad-spectrum antibiotic treatment. Despite the general interpretation that a positive IgG and a negative IgM indicate a previous infection, the patient’s extraordinarily elevated IgG levels, coupled with a markedly increased CMV DNA quantification, prompted us to suspect a reactivation of the CMV virus. In light of these findings, we opted for the intravenous administration of ganciclovir as part of the treatment strategy. Unfortunately,,the patient succumbed to rapidly worsening symptoms and passed away. Within one week of the patient’s demise, chickenpox gradually developed in the medical staff who had been in contact with him. In such instances, we speculate that the patient’s diagnosis should be classified as a rare case of hemorrhagic varicella.
Conclusion
Swift identification and timely administration of suitable treatment for adult HV are imperative to enhance prognosis.
Similar content being viewed by others
Background
Hemorrhagic varicella (HV) is a rare and potentially life-threatening condition that can arise concurrently with various conditions, including immunodeficiency syndrome, hematologic malignancy, and autoimmune disease [1]. Despite its potential severity, adult hemorrhagic varicella is frequently overlooked due to its low incidence rate, with only four reported cases in the English literature [2,3,4]. This rarity may result in the omission of this disease from the differential diagnosis when evaluating patient symptoms, potentially leading to delayed and inaccurate diagnoses, and adverse outcomes. To address this, it is imperative to raise awareness of this condition.
Cytomegalovirus (CMV)belongs to the ubiquitous herpes family. Following primary infection, CMV establishes latency but can be reactivated by various triggers. Reactivation may occur due to a range of stimuli or conditions, including immunocompromising states, drug eruptions [5], administration of immunosuppressants, HIV infection, and septic shock.
The reactivation of CMV and the infection of Varicella Zoster Virus (VZV) is linked to a poor prognosis, leading to the development of conditions such as pneumonia, colitis, hepatitis, or encephalitis. This case report aims to elaborate on the clinical features of the reactivation of HV and CMV, thereby raising awareness among healthcare professionals.
Case presentation
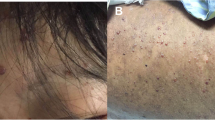
A 25-year-old Chinese male patient visited the emergency department (ED) with a 3 d history of countless hemorrhagic vesicles on his trunk and limbs and abdominal pain (Fig. 1A and B). Three days prior, the patient had developed abdominal pain and blood vesicles all over his body. He visited a local hospital and was given abdominal radiography showed no obstruction. After the examination, he had been treated with lactose and glycerin 1 d prior to his ED visit. However, the above symptoms did not alleviate.
A and B: In comparison between the conditions on day 1 and day 3 of hospitalization, there was a rapid increase in lesions on the patient’s face, accompanied by a noticeable deterioration in consciousness. C and D: In comparison between day 1 and day 3 of hospitalization, the hemorrhagic vesicles on the patient’s trunk not only increased but also exhibited surrounding purpura
The patient had a history of nephrotic syndrome and received orally administered prednisone, 50 mg per day for two months. The patient denied the history of varicella patients contaction, and never received VZV vaccination. There was no family history of severe chickenpox.
During physical examination in the ED, the patients vital signs were measured: Body temperature (36.7℃), blood pressure (140/90mmHg), heart rate (64 bpm), and respiratory rate (20 breaths/min). The patient had dry mouth with a size of approximately 3 mm\(\times 3\)mm ulcer, and enlarged and erythematous tonsis. Hemorrhagic vesicles covered her faces, and the remainder of his body was studded with countless vesicles and papules, including nearly confluent vesicles on his genital organ and the inguinal region. The vesicles were filled with bright red blood or clear fluid; only a few were crusted. An abdominal examination revealed tenderness and rebound pain localized to the lower right half of the abdomen. Cardiac and pulmonary examination findings were normal. No specific findings were observed in the remaining physical examination. A laboratory examination was performed once the patient was admitted our hospital. Due to changes in the condition, some indicators were rechecked on the third day (Tables 1 and 2).
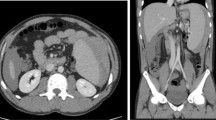
The patient’s head computed tomography (CT) was normal. Abdominal CT was performed due to persistent abdominal pain and it showed silty gallstones in the gallbladder. Chest CT suggested bilateral lung inflammation. At the 10th hour of hospitalization, given the significant increase in the patient’s WBC count, broad-spectrum antibiotics were administered. However, 1 d later, the patient exhibited worsening hemorrhagic ulceration in the oral mucosa compared to the initial presentation. The number of hemorrhagic varicella on the trunk increased, gradually affecting both lower limbs. A large area of ecchymosis, approximately 4 × 7 cm in size, appeared at the blood collection point on the left elbow joint flexion side. Concurrently, the patient developed hematuria, and a single episode of bright red stool was observed (Fig. 1C and D). Laboratory tests revealed disseminated intravascular coagulation, sepsis, hemorrhagic shock, and acute liver failure (Table 2). Unfortunately, high-throughput gene testing targeting pathogenic microorganisms could not be completed due to hemolysis in the patient’s blood sample.
Due to the potential for multiple organ failure, the patient was admitted to the Department of Infectious Disease Intensive Care Unit (ICU) on the 3d of hospitalization and received intravenous treatment with broad-spectrum antibiotics and ganciclovir at 250 mg per day. As his neurological and hepatic conditions progressively deteriorated, he required endotracheal intubation on the 3rd day of hospitalization, along with bedside continuous renal replacement therapy (CRRT). However, acyclovir combined with gamma globulin (recommended for severe chickenpox) was not administered. The assay was not performed due to the lack of availability of the test. Additionally, the patient’s immune system might have been weakened after long-term oral steroid use, rendering him more susceptible to infection.
During the ICU admission, the patient’s coagulation worsened, and infection indicator levels increased. The patient’s condition rapidly deteriorated. On the 4th day of hospitalization, the patient experienced cardiopulmonary arrest due to DIC and succumbed to the illness. On the 11th day after contact with the patient, some ICU physicians and the ED nurses who had been in contact with the patient exhibited symptoms such as vesicles, papules throughout the body, and high fever. All of they had not been vaccinated against the disease The diagnosis of chickenpox of them was made by infectious disease specialists or dermatologists based on the typical presentation of the rash. All of them were subsequently diagnosed with chickenpox. None of them reported any contact history with other varicella patients. Following the patient’s demise, we initiated an extensive discussion about the case across the entire hospital. Based on the characteristics of the patient’s symptoms, it can be clinically confirmed that the patient died from hemorrhagic varicella combined with cytomegalovirus infection.
Discussion and conclusions
HV, a rare condition linked to uncontrolled VZV infection, is characterized by hemorrhagic vesicles surrounded by purpura and subconjunctival hemorrhage [6]. Older age and a compromised immune system are the most significant risk factors associated with the severity of varicella disease [7]. HV is less commonly known to occur in adults, and to date, only a few cases in adults have been reported. For instance, Benchat et al. documented a case of varicella in adult, however, the patient’s ecchymosis in skin and visceral hemorrhage were not typical [8].
CMV belongs to herpes family. After primary infection, latency of CMV is established, but it may be reactivated with some triggers, including immunocompromising condition, drug eruption, immunosuppressant administration, HIV infection and septic shock [9]. Additionally, reactivation of CMV with VZV is associated with poor prognosis. Only Akira et al. described a case of simultaneous reactivation of cytomegalovirus in an adult patient with varicella, however, there was a lack of description regarding the changes in liver function indicators in the patient [10].
Hemorrhagic manifestations and multiorgan failure are severe complications that can arise in the context of autoimmune diseases. During the patient’s hospitalization, we placed particular emphasis on ruling out the possibility of an autoimmune disease, as detailed in the Table 3. The patient’s autoantibodies associated with autoimmune diseases and HIV antibodies tested negative, leading us to exclude the diagnosis of an autoimmune condition.
Our patient presented a challenging case of chickenpox, exhibiting an unusually extensive cutaneous manifestation characterized by the rapid progression of hemorrhagic vesicles and accompanying visceral complications. Notably, a significant number of medical staff from various departments, who had been in direct contact with the patient, contracted chickenpox within a short period. Remarkably, all affected individuals denied any history of exposure to other chickenpox patients. The patient’s initial manifestation of abdominal pain led to a misdiagnosis, aligning with Wong et al.‘s findings, where they reported cases of severe varicella presenting with abdominal pain. The authors emphasized the consideration of varicella in the differential diagnosis of abdominal pain, particularly in immunocompromised patients, especially when the etiology is not readily apparent [11].
The poor prognosis of this patient can be attributed to several factors. Firstly, the patient’s long-term immunocompromised state resulted from the oral administration of prednisolone, specifically 50 mg per day, aimed at managing nephrotic syndrome for a duration of at least two months. And the use of prednisone can be a factor in the reactivation of a CMV reactivation and the hemorrhagic transformation of the vesicular lesion. Secondly, the concomitant CMV reactivation exacerbated the situation, leading to severe hepatitis, deterioration in coagulation function, and a decline in platelet count [12]. Thirdly, the patient’s serum analysis revealed markedly elevated levels of PCT and IL-6, which are suggestive of a sepsis condition potentially triggered by the reactivation of CMV and concurrent infection with VZV. This septicemia could be identified as the primary cause of the patient’s demise. It is pertinent to note that the notable escalation in AST and ALT levels, with AST levels exceeding those of ALT, could be indicative of heart failure. This is corroborated by the marked elevation of troponin and BNP, which are reliable indicators of cardiac injury and heart failure, respectively. This suggests that the elevated AST and ALT levels may not be exclusively a consequence of liver failure induced by CMV infection. Additionally, the observed increase in these enzymes could also be associated with muscle breakdown, further complicating the interpretation of these laboratory findings. Ganciclovir stands as the preferred treatment for CMV [13] and has demonstrated effectiveness against VZV [14]. espite the intravenous administration of 0.25 g of ganciclovir per day starting on the third day of hospitalization, the treatment’s efficacy remained suboptimal. This could be attributed to the premature initiation of antiviral drugs and a potentially insufficient duration of treatment.
The current standard therapeutic regimen for HV involves early active antiviral treatment and symptomatic support, which holds significant importance in improving prognosis, particularly for immunocompromised patients (Table 4). Acyclovir is the preferred antiviral therapy for VZV infection, with an oral bioavailability ranging from 15-30% [15]. In severe VZV infections, intravenous injection becomes necessary. Combining acyclovir with gamma globulin is considered safe and effective [16]. For patients with prolonged steroid use and severe chickenpox, the question of whether to continue steroid treatment remains controversial. Traditional textbooks consider chickenpox a relative contraindication for steroids. Some studies indicate that steroids may hinder the phagocytosis of reticuloendothelial cells, reduce antibody production, and promote VZV proliferation, leading to extensive damage to vascular endothelium and a subsequent imbalance in the coagulation and fibrinolysis systems [17]. However, other studies have suggested that physiological maintenance of steroids can avoid iatrogenic adrenal insufficiency [18].
In conclusion, HV is a severe form of varicella that often manifests in immunocompromised populations, posing a potential fatality risk if treatment is delayed. Patients may present with abdominal pain symptoms, prompting visits to the ED. Emergency medicine physicians should be mindful that unexplained abdominal pain may be attributed to chickenpox. Reactivation of VZV with CMV can intensify liver failure, heightening the risk of mortality. Early initiation of antiviral treatment and immunoglobulin therapy has proven efficacy. Additionally, if deemed necessary, medical staff should consider vaccination against chickenpox.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
- HV:
-
Hemorrhagic varicella
- CMV:
-
Cytomegalovirus
- VZV:
-
Varicella Zoster Virus
- ED:
-
Emergency Department
- WBC:
-
White blood cell
- RBC:
-
Red blood cell
- INR:
-
International standard ratio
- APTT:
-
Activated partial thromboplastin time
- FBI:
-
Fibrinogen
- PCT:
-
Procalcitonin
- CRP:
-
C-reaction protein
- CREA:
-
Creatinine
- ALB:
-
Albumin
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate amino transferase
- CT:
-
Computed tomography
- ICU:
-
Intensive Care Unit
- CRRT:
-
Continuous renal replacement therapy
References
Hirose M, Gilio AE, Ferronato AE, Ragazzi SL. The impact of varicella vaccination on varicella-related hospitalization rates: global data review. Rev Paul Pediatr. 2016;34(3):359–66.
Abzug MJ, Cotton MF. Severe chickenpox after intranasal use of corticosteroids. J Pediatr. 1993;123(4):577–9.
Magi E. Severe varicella in an immunocompromised adult presenting with abdominal pain. West J Med. 2000;173(6):376–7.
Nee PA, Edrich PJ. Chickenpox pneumonia: case report and literature review. J Accid Emerg Med. 1999;16(2):147–50.
Asano Y, Kagawa H, Kano Y, Shiohara T. Cytomegalovirus disease during severe drug eruptions: report of 2 cases and retrospective study of 18 patients with drug-induced hypersensitivity syndrome. Arch Dermatol. 2009;145(9):1030–6.
Widgren K, Persson Berg L, Mörner A, Lindquist L, Tegnell A, Giesecke J, Studahl M. Severe chickenpox disease and seroprevalence in Sweden - implications for general vaccination. Int J Infect Dis. 2021;111:92–8.
Ho BC, Tai DY. Severe adult chickenpox infection requiring intensive care. Ann Acad Med Singap. 2004;33(1):84–8.
Benchat L, Mernissi FZ. Severe varicella in adult. Pan Afr Med J. 2013;16:98.
Naendrup JH, Garcia Borrega J, Eichenauer DA, Shimabukuro-Vornhagen A, Kochanek M, Böll B. Reactivation of EBV and CMV in severe COVID-19-Epiphenomena or trigger of hyperinflammation in need of treatment? A large Case Series of critically ill patients. J Intensive Care Med. 2022;37(9):1152–8.
Kasuya A, Kaneko Y, Enomoto N, Suda T, Tokura Y. Simultaneous reactivation of cytomegalovirus in an adult patient with varicella. J Dermatol. 2015;42(6):658–9.
Wong JW, Chin JM, Schlueter RJ. Shingles in pregnancy: an elusive case of Left Upper Quadrant Abdominal Pain. Hawaii J Med Public Health. 2018;77(8):179–82.
Haidar G, Boeckh M, Singh N. Cytomegalovirus infection in solid organ and hematopoietic cell transplantation: state of the evidence. J Infect Dis. 2020;221(Suppl 1):S23–31.
Kotton CN. Prevention, diagnosis and therapy. Am J Transpl. 2013;13(Suppl 3):24–40. quiz 40.
Collet A, Baes D, Mambie A, Hembert K, Boulle C, Gana I, Lemaire X. VZV meningoencephalitis treated with ganciclovir. Med Mal Infect. 2020;50(5):444–5.
Nair AB, Attimarad M, Al-Dhubiab BE, Wadhwa J, Harsha S, Ahmed M. Enhanced oral bioavailability of acyclovir by inclusion complex using hydroxypropyl-β-cyclodextrin. Drug Deliv. 2014;21(7):540–7.
Cvjetković D, Jovanović J, Hrnjaković-Cvjetković I. [Primary varicella-zoster virus infection–current knowledge, diagnostic and therapeutic approaches]. Med Pregl. 2000;53(5–6):272–6.
Grossi O, Généreau T. [Glucocorticoids and… infections, doping, surgery, sexuality]. Rev Med Interne. 2013;34(5):269–78.
Vandewalle J, Libert C. Glucocorticoids in Sepsis: to be or not to be. Front Immunol. 2020;11:1318.
Acknowledgements
We thank for technical support of the Guangdong Second Provincial General Hospital.
Funding
This research was supported by Guangdong Second Provincial General Hospital In-hospital Fund (3D-A2021001). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Shi SM and Zheng RC contributed to manuscript writing and editing, and data collection; Xu JR and Li ZH contributed to the revision of the manuscript; Cai XX contributed to data analysis; Zhou XX contributed to conceptualization; Wen J contributed to supervision; all authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient’s father for publication of this case report.
Consent for publication
Written informed consent for the publication of case-ralated details was obtained from the wife of the patient described in this report. Copies of the document are available for inspection upon request to the corresponding authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, SM., Li, ZH., Xu, JR. et al. An adult with hemorrhagic varicella co-infects with cytomegalovirus: a case report. BMC Infect Dis 24, 691 (2024). https://doi.org/10.1186/s12879-024-09383-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09383-0