Abstract
Background
Cervical cancer is caused by oncogenic human papillomaviruses (HR-HPV) and is common among Kenyan women. Identification of factors that increase HR-HPV persistence is critically important. Kenyan women exposed to aflatoxin have an increased risk of HR-HPV detection in cervical specimens. This analysis was performed to examine associations between aflatoxin and HR-HPV persistence.
Methods
Kenyan women were enrolled in a prospective study. The analytical cohort for this analysis included 67 HIV-uninfected women (mean age 34 years) who completed at least two of three annual study visits and had an available blood sample. Plasma aflatoxin was detected using ultra-high pressure liquid chromatography (UHPLC)-isotope dilution mass spectrometry. Annual cervical swabs were tested for HPV (Roche Linear Array). Ordinal logistic regression models were fitted to examine associations of aflatoxin and HPV persistence.
Results
Aflatoxin was detected in 59.7% of women and was associated with higher risk of persistent detection of any HPV type (OR = 3.03, 95%CI = 1.08–8.55, P = 0.036), HR-HPV types (OR = 3.63, 95%CI = 1.30-10.13, P = 0.014), and HR-HPV types not included in the 9-valent HPV vaccine (OR = 4.46, 95%CI = 1.13–17.58, P = 0.032).
Conclusions
Aflatoxin detection was associated with increased risk of HR-HPV persistence in Kenyan women. Further studies, including mechanistic studies are needed to determine if aflatoxin synergistically interacts with HR-HPV to increase cervical cancer risk.
Similar content being viewed by others
Introduction
Cervical cancer is a common malignancy among Kenyan women [1,2,3]. The incidence rate of cervical cancer in Kenya is 31.3 per 100,000 women per year and the mortality rate is 25 per 100,000 women per year, figures considerably higher than those in wealthy countries [4, 5]. Oncogenic types of human papillomaviruses (“high-risk”, or HR-HPV) are the causative agents of cervical cancer. However, only a small percentage of women infected with HR-HPV will develop cancer, indicating the importance of cofactors associated with HR-HPV persistence that contribute to the occurrence of cervical cancer [6]. Women with persistent infection with oncogenic HPV are at significantly higher risk of cervical cancer [7]. HIV infection is one cofactor that imparts a higher likelihood of HR-HPV persistence [2, 8, 9]. HR-HPV detection and persistence are also prevalent among Kenyan women who are not HIV-infected [10, 11].
Dietary aflatoxin may be another risk factor for HR-HPV persistence that is additive with HIV infection. Aflatoxin is a potent carcinogen and immunosuppressive agent produced by certain strains of Aspergillus, a mold that infects corn crops [12,13,14]. Large percentages of people living in sub-Saharan African countries are exposed to aflatoxin. We previously showed in a cross-sectional analysis that plasma aflatoxin biomarkers were detected among 57% of HIV-uninfected Kenyan women enrolled in a prospective study of HPV epidemiology and associated with cervical detection of A9 HPV types [15]. An additional analysis was performed using longitudinal data from this cohort to examine associations between plasma aflatoxin detection and cervical HR-HPV persistence.
Methods
Study population
Kenyan women were enrolled from September 2015 to October 2016 at the Academic Model Providing Access to Healthcare (AMPATH) Cervical Cancer Screening Program (CCSP) at Moi Teaching and Referral Hospital in Eldoret, Kenya [16]. They were participants in a prospective cohort study investigating biological, behavioral, and environmental risk factors for oncogenic HPV persistence, a part of the East African Consortium for Human Papillomavirus and Cervical Cancer in Women Living with HIV/AIDS [16]. Details of study enrollment procedures have been previously published [11]. Briefly, women aged 18 to 60 years living within 30 km of Eldoret presenting for screening at the CCSP were asked to participate in the study if they had a normal visual inspection with acetic acid (VIA) of the uterine cervix that day.
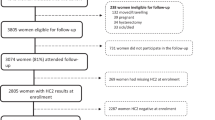
A total of 223 women consented to participation and enrolled in the study, including 116 HIV-infected and 107 HIV-uninfected women. Plasma obtained at enrollment was available for 87 of 107 HIV-uninfected women, but no plasma sample was available for the HIV-infected women. Of the 87 HIV-uninfected women with available plasma, 67 women had at least two adequate cervical swab samples (based on beta globin testing) obtained at enrollment and at 12- or/and 24-month follow-up visits. These 67 women represented the analytical cohort for this post-hoc analysis.
Interview and questionnaire
Structured face-to-face interviews of the participants by trained researchers were conducted at enrollment to capture social, behavioral, and biological information, including age, marital status, educational level, home ownership, walking distance to the local clinic, number of lifetime sexual partners, and age of first sex [11].
Cervical swab and plasma sample collection
A cervical swab for HPV testing was collected by a nurse or physician as part of the inspection for cervical cancer screening. Swabs were placed in standard transport media and frozen at -80 °C in the AMPATH Reference Laboratory. Plasma was collected and frozen at -20 °C at the same laboratory.
HPV testing
Cervical specimens were transported on dry ice to the Kenya Medical Research Institute-University of Massachusetts Medical School (KEMRI-UMMS) Laboratory for processing, DNA extraction, and subsequent genotyping [11]. The Roche Linear Array was used to determine HPV types (Roche Molecular Systems, Inc., Branchburg, NJ, USA) as previously described [17]. HPV 16-positive, negative, and human beta-globin (used to assess specimen adequacy) controls provided by the manufacturer were tested with each batch of samples.
HPV types were grouped into “high-risk” (HR-HPV) and “low-risk” (LR-HPV) based on the designation in the Roche Linear Array instructions, or HR-HPV types as designated by the International Agency for the Research on Cancer (IARC) [18]. HPV types were further grouped into A9 and A7 types and into other groups [19]. The specific HPV types included in each group are detailed in Results.
Aflatoxin-albumin adduct (AFB1-lys) detection in plasma samples
Plasma aflatoxin B1-lysine (AFB1-lys) was measured at the Department of Environmental Health and Engineering of the Johns Hopkins Bloomberg School of Public Health, using a minor variation of the method reported by McCoy and colleagues [15, 20]. Briefly, plasma (150 µL) was spiked with an internal standard (0.5 ng AFB1-d4-lysine in 100 µL), combined with Pronase (EMD Millipore, Billerica MA, USA) protease solution (3.25 mg in 0.5 mL phosphate-buffered saline), and incubated for 18 h at 37 °C. Solid-phase extraction–processed samples (Oasis MAX columns; Waters, Milford, MA, USA) were analyzed with ultra-high pressure liquid chromatography (UHPLC)-isotope dilution mass spectrometry on a ThermoFisher Scientific (San Jose, CA, USA) system composed of a Vanquish UHPLC and a TSQ Quantis triple quadrupole mass spectrometer in positive electrospray ionization mode [21, 22].
Persistent HPV detection
Type-specific HPV testing results obtained from the enrollment, 12-month and 24-month cervical samples were combined to determine the detection category of each specific HPV type for each woman. Three categories of HPV detection were determined: No detection, Incident Detection, and Persistent Detection. To be included, two or three of a participant’s cervical samples (Enrollment, 12-month, or 24-month) had to be available; one of the three samples could be missing. The type-specific HPV detection categories were defined as follows: (I) No detection: No detection for the specific HPV type at any of the three time-points; (II) Incident detection: One sample positive for detection of a specific HPV type, but other samples were negative for that type; (III) Persistent detection: Two samples taken one year apart, or two years apart were positive for detection of a specific HPV type. The third sample could be negative for that type (or missing).
At the level of study participants, a woman’s HPV detection status was defined as the highest level of HPV detection category in the descending order of “Persistent detection,” “Incident detection,” and “No detection” among her type-specific HPV detection episodes within a combined group of specific HPV types. For example, a woman is classified as at the status of persistent detection in HR-HPV if any type-specific “persistence detection” episode is identified among the HR-HPV types. The subsequent analysis of HPV detection was conducted at the level of participant.
Statistical analysis
Demographic and behavioral characteristics of participants at enrollment (age, marital status, educational level, home ownership, walking distance to health care of ⩾60 min, number of lifetime sex partners, and age of first sex) were summarized by descriptive statistics and compared between women with and without detectable plasma AFB1-lys using t-tests, chi-square tests, or Wilcoxon rank sum tests. Frequencies and percentages of HPV detections (“No detection”, “Incident detection” and “Persistent detection”) in women were compared between those with and without detectable plasma AFB1-lys using chi-square tests or Fisher’s exact tests. Plasma AFB1-lys concentration (pg/uL) were summarized in mean, standard deviation (std), median and interquartile range (IQR) and compared among women with different HPV detection status using Wilcoxon rank sum tests. In addition, ordinal logistic regression models were fitted to examine associations of HPV detection (persistent detection vs. incident detection vs. no detection) with plasma aflatoxin detection, controlling for demographic and behavioral characteristics of the women as confounders. The proportional odds assumption was examined for each fitted ordinal logistic regression model to ensure validity of the model. All analyses were performed using SAS Version 9.4 (Cary, NC).
Results
Overall characteristics of participants and aflatoxin (AFB1-lys) detection
The median age (IQR) at enrollment of 67 participants with an available plasma sample and valid HPV testing results was 34.0 (30.0, 38.0) years (range 21 to 46 years) (Table 1). Of 67 women, 27 (40.3%) had no detection of AFB1-lys in plasma, and 40 women (59.7%) had AFB1-lys detected (Table 1). Women with and without detectable plasma AFB1-lys were not significantly different in age, being married, having more than secondary school education, home ownership, living at a walking distance to health care of ≥ 60 min, number of lifetime sex partners, or age of first sex (Table 1).
A total of 87 women in the original cohort had plasma samples tested for AFB1-lys, including 67 women consisting of the analytical cohort and 20 women who did not complete at least two study visits. Comparisons between the 67 women in this analytical cohort and the 20 women who did not complete at least two visits were conducted with respect to the demographics/behavioral characteristics and plasma AFB1-lys detection/concentration. No significant differences in these variables were found between the two groups of women (data not shown).
Association of plasma AFB1-lys detection with persistent HPV detection
Frequencies and percentages of HPV detections (“no detection”, “incident detection” and “persistent detection”) in women with and without plasma AFB1-lys detection and mean (STD) and median (IQR) of plasma AFB1-lys concentration (pg/uL) among women with different HPV detections are shown in Table 2. There was a trend of significantly increasing plasma AFB1-lys concentrations among women who had no detection, incident detection, or persistent detection for any HPV type (p = 0.036), HR-HPV types (p = 0.020), and HR-HPV types not included in the 9 valent HPV vaccine (p = 0.017) (Table 2). Similar trends in increasing plasma AFB1-lys concentrations were observed for some other groups of HPV types, however, these were not significant (Table 2).
In addition, compared with women without detectable plasma AFB1-lys, women with detectable plasma AFB1-lys demonstrated significantly higher percentages of detection for any HPV type (22.5% vs. 11.1% for persistent detection and 55.0% vs. 37.0% for incident detection, p = 0.043) and HR-HPV type (22.5% vs. 7.4% for persistent detection and 45.0% vs. 29.6% for incident detection, p = 0.038). Similar patterns of HPV detections between women with and without detectable plasma AFB1-lys were found for all other HPV combination types except for LR-HPV types. However, these were not statistically significant, possibly due to small sample sizes.
A total of 13 episodes of type-specific persistent HPV detections occurred in 12 women (Table 3). Among these episodes, 12 were HR-HPV types, including 10 episodes that occurred in 9 of 40 women with detectable plasma AFB1-lys, and 2 episodes occurring in 2 of 27 women without detectable plasma AFB1-lys (Table 3). HPV 18 was the most frequently detected persistent type (3 episodes), all occurring in women with detectable plasma AFB1-lys (Table 3). The overall distribution of HPV types detected in the cohort of women is shown in Supplemental Table 1.
Ordinal logistic regression analysis revealed that detectable plasma AFB1-lys was associated with a higher risk of persistent detection for any HPV type (OR = 3.03, 95%CI = 1.08–8.55, P = 0.036), HR-HPV types (OR = 3.63, 95%CI = 1.30-10.13, P = 0.014), and HR-HPV types not included in the 9 valent HPV vaccine (OR = 4.46, 95%CI = 1.13–17.58, P = 0.032) after adjustment for established and suspected confounders (Table 4). The proportional odds assumption was validated for each ordinal logistic regression model. There was no statistically significant association of detectable plasma AFB1-lys with persistent detection of sub-groups of HR-HPV types, for HR-HPV types included in the 9 valent HPV vaccine, and for low-risk (LR) HPV types (Supplemental Table 2).
Discussion
In this longitudinal study, women with detectable aflatoxin biomarkers in plasma had a higher risk of persistent detection of oncogenic cervical HPV. Although only a small percentage of HPV-infected women will eventually develop cervical cancer, women with persistent detection of HR-HPV are at the highest risk for this malignancy [23, 24]. Aflatoxins are mycotoxins produced by certain Aspergillus species during growth or after harvesting of corn and several other crops [25]. These compounds are classified by the International Agency for Research on Cancer (IARC) as class I carcinogens [26]. In addition, aflatoxins are potent immunosuppressive agents [27,28,29,30]. Exposure to aflatoxins contributes heavily to the worldwide burden of hepatocellular carcinoma, but the contribution of aflatoxin exposure to other cancers is unknown [31, 32]. This study revealed an association between aflatoxin exposure and persistent HR-HPV detection, the major risk factor for cervical cancer.
A previous cross-sectional study showed significant associations between plasma aflatoxin biomarkers and detection of A9 HPV types in cervical samples among HIV-uninfected Kenyan women [15]. The current analysis employed a subset of the original cohort with the longitudinal follow-up data on HPV testing, disclosing the relationship of aflatoxins with persistent detections of HR-HPV, and raising the possibility that aflatoxin could be a contributing factor to cervical cancer. We are not aware of other studies describing an association of aflatoxin with HPV persistence, cervical dysplasia, or cancer.
It is possible that HR-HPV types and dietary aflatoxin act synergistically in increasing the risk of cervical cancer in Kenyan women. While aflatoxins are established in the etiology of liver cancer, it is possible that aflatoxins may play a role in other human cancers. Aflatoxins have been detected in many tissues including cervical tissue and could potentially act directly on cervical cells in the carcinogenic process, but this hypothesis has not been studied [33]. It is also possible the immunosuppression caused by aflatoxin could lead to poor immune control of oncogenic HPV infections, leading to persistence [30]. These hypotheses need to be further investigated. From a public health perspective, it is important to investigate the possible interaction between aflatoxin exposure and persistent HPV infection in the etiology, pathogenesis, and prevention of cervical cancer and its precursor lesions in large epidemiological studies, especially in developing countries. In addition, there is a need for mechanistic and in-vitro data to support the biologic plausibility of the association of aflatoxin with HR-HPV persistence, because the evidence presented here is strictly epidemiological.
Aflatoxin exposure is widespread in many sub-Saharan African countries, largely due to consumption of contaminated corn, the major source of daily calories for many people, especially for poor families [34,35,36]. Leroy et al., showed higher serum aflatoxin levels from adult Kenyan women associated with lower household socio-economic status [37]. Women with the lowest socio-economic status also have the lowest rates of cervical cancer screening, and therefore bear the highest burden of cervical cancer [38, 39]. Aflatoxin, as a potential environmental risk factor of cervical cancer, demands more recognition for public health emphasis. Numerous strategies to reduce aflatoxin exposure have been proposed and many of these methods are being studied in efforts to mitigate the harmful effects of these compounds [40,41,42].
Some limitations of the present study include a modest sample size, as not all women initially analyzed for the association of aflatoxin detection and HR-HPV detection continued in the longitudinal study. However, our analysis showed that there were no significant differences in demographic/behavioral characteristics and plasma AFB1-lys detection/concentration between the women who remained in the original study and included in this analysis compared to those who did not continue in the original study. Another potential limitation is that dietary factors that modulate immune functions were not included as potential confounders in our data analysis, which could possibly distort the findings of the present study. For example, malnourishment may contribute to suppressed immunity and render such women more susceptible to the toxic effects of aflatoxin, and thus, more prone to persistent HPV infection [34, 43]. In addition, the results of our study may be subject to multiple comparisons due to a relatively large number of the models presented. However, this is unlikely because all exposure and outcome variables included in the constructed models were carefully selected in terms of the findings of previous studies and biological relevance. Furthermore, model overfitting may occur in the fitted multivariable ordinal logistic regression models due to the number of variables fitted in the model and the small sample size of the analytical cohort, which may impact the generalizability of the current results on a larger population. However, comparisons of the corresponding model estimates of the current analysis and those obtained from a previous analysis based on the original study cohort demonstrated generally consistent results on associations of persistent HPV detection with participants’ characteristics, indicating the validity of the reported multivariable models [11]. Another potential limitation relates to the question of low-level HPV persistence vs. type-specific reinfection. While it is impossible to be certain, many studies provide evidence that redetection of a specific HPV type among women is more likely to represent low-level persistence rather than reinfection [44,45,46,47] (Malagon et al.: Human papillomavirus intermittence and risk factors associated with first detections and redetections in the Ludwig-McGill cohort study of adult women, unpublished). The identity of sequences of the long-control region (LCR) from specific HPV types that were redetected after a period of non-detection has also provided evidence that low-level persistence occurs, rather than type-specific infection [45, 46].
In summary, detection of plasma aflatoxin biomarkers was associated with increased persistence of oncogenic HPV types, in cervical samples from HIV-uninfected Kenyan women. Further studies are needed to determine if exposure to aflatoxin interacts with HPV infection to modulate the risk of cervical cancer in Kenya and other developing countries. In addition, studies are underway to examine associations of aflatoxin exposure and HR-HPV infection on occurrence of cervical dysplasia in a cohort of HIV-infected sub-Saharan women, as HIV infection increases susceptibility to cervical cancer.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author (Dr. Brown and the additional authors) upon reasonable request and with permission of AMPATH.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:398–424.
Stelzle D, Tanaka LF, Lee KK, et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet Glob Health. 2020;9:161–9.
Mwenda V, Mburu W, Bor JP, et al. Cervical cancer programme, Kenya, 2011–2020: lessons to guide elimination as a public health problem. Ecancermedicalscience. 2022;16:1442.
Organization WH. Cervical cancer Kenya 2021 country profile. Available at: https://www.who.int/publications/m/item/cervical-cancer-ken-country-profile-2021.
Brower V. AIDS-related cancers increase in Africa. J Natl Cancer Inst. 2011;103:918–9.
Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide.[see comment]. J Pathol. 1999;189:12–9.
Kjaer SK, Frederiksen K, Munk C, Iftner T. Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: role of persistence. J Natl Cancer Inst. 2010;102:1478–88.
Stelzle D, Tanaka LF, Lee KK, et al. Estimates of the global burden of cervical cancer associated with HIV. The lancet global health. 2021;9:e161–e9.
Liu G, Sharma M, Tan N, Barnabas RV. HIV-positive women have higher risk of human papilloma virus infection, precancerous lesions, and cervical cancer. AIDS. 2018;32:795–808.
Ermel A, Tonui P, Titus M, et al. A cross-sectional analysis of factors associated with detection of oncogenic human papillomavirus in human immunodeficiency virus-infected and uninfected kenyan women. BMC Infect Dis. 2019;19:352.
Tong Y, Tonui P, Ermel A, et al. Persistence of oncogenic and non-oncogenic human papillomavirus is associated with human immunodeficiency virus infection in kenyan women. SAGE Open Med. 2020;8:2050312120945138.
Gong YY, Wilson S, Mwatha JK, et al. Aflatoxin exposure may contribute to chronic hepatomegaly in kenyan school children. Environ Health Perspect. 2012;120:893–6.
Seetha A, Monyo ES, Tsusaka TW, et al. Aflatoxin-lysine adducts in blood serum of the malawian rural population and aflatoxin contamination in foods (groundnuts, maize) in the corresponding areas. Mycotoxin Res. 2018;34:195–204.
Watson S, Moore SE, Darboe MK, et al. Impaired growth in rural gambian infants exposed to aflatoxin: a prospective cohort study. BMC Public Health. 2018;18:1247.
Zhang J, Orang’o O, Tonui P, et al. Detection and concentration of plasma aflatoxin is associated with detection of oncogenic human papillomavirus in Kenyan women. Open Forum Infect Dis. 2019;6(9):ofz354. https://doi.org/10.1093/ofid/ofz354.
Tong Y, Orang’o E, Nakalembe M, et al. The East Africa Consortium for human papillomavirus and cervical cancer in women living with HIV/AIDS. Ann Med. 2022;54:1202–11.
Brown DR, Shew ML, Qadadri B, et al. A longitudinal study of genital human papillomavirus infection in a cohort of closely followed adolescent women. J Infect Dis. 2005;191:182–92.
WHO. Human papillomaviruses. IARC Working Group on the evaluation of carcinogenic risks to humans. IARC Monogr. 2007;90:1–636.
Munoz N, Bosch FX, de Sanjose S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–27.
McCoy LF, Scholl PF, Sutcliffe AE, et al. Human aflatoxin albumin adducts quantitatively compared by ELISA, HPLC with fluorescence detection, and HPLC with isotope dilution mass spectrometry. Cancer Epidemiol Biomarkers Prev. 2008;17:1653–7.
Smith JW, Kroker-Lobos MF, Lazo M, et al. Aflatoxin and viral hepatitis exposures in Guatemala: molecular biomarkers reveal a unique profile of risk factors in a region of high liver cancer incidence. PLoS ONE. 2017;12:e0189255.
Groopman JD, Egner PA, Schulze KJ, et al. Aflatoxin exposure during the first 1000 days of life in rural South Asia assessed by aflatoxin B(1)-lysine albumin biomarkers. Food Chem Toxicol. 2014;74:184–9.
Koshiol J, Lindsay L, Pimenta JM, Poole C, Jenkins D, Smith JS. Persistent human papillomavirus infection and cervical neoplasia: a systematic review and meta-analysis. Am J Epidemiol. 2008;168:123–37.
Stensen S, Kjaer SK, Jensen SM, et al. Factors associated with type-specific persistence of high-risk human papillomavirus infection: a population-based study. Int J Cancer. 2016;138:361–8.
Bennett JW, Klich M. Mycotoxins Clin Microbiol Rev. 2003;16:497–516.
Wild CP, Gong YY. Mycotoxins and human disease: a largely ignored global health issue. Carcinogenesis. 2010;31:71–82.
Turner PC, Moore SE, Hall AJ, Prentice AM, Wild CP. Modification of immune function through exposure to dietary aflatoxin in gambian children. Environ Health Perspect. 2003;111:217–20.
Meissonnier GM, Pinton P, Laffitte J, et al. Immunotoxicity of aflatoxin B1: impairment of the cell-mediated response to vaccine antigen and modulation of cytokine expression. Toxicol Appl Pharmacol. 2008;231:142–9.
Jolly PE. Aflatoxin: does it contribute to an increase in HIV viral load? Future Microbiol. 2014;9:121–4.
Shirani K, Zanjani BR, Mahmoudi M, et al. Immunotoxicity of aflatoxin M1: as a potent suppressor of innate and acquired immune systems in a subacute study. J Sci Food Agric. 2018;98:5884–92.
Chu YJ, Yang HI, Wu HC, et al. Aflatoxin B1 exposure increases the risk of hepatocellular carcinoma associated with hepatitis C virus infection or alcohol consumption. Eur J Cancer. 2018;94:37–46.
Rushing BR, Selim MI. Aflatoxin B1: a review on metabolism, toxicity, occurrence in food, occupational exposure, and detoxification methods. Food Chem Toxicol. 2019;124:81–100.
Carvajal M, Berumen J, Guardado-Estrada M. The presence of aflatoxin B(1)-FAPY adduct and human papilloma virus in cervical smears from cancer patients in Mexico. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2012;29:258–68.
Williams JH, Phillips TD, Jolly PE, Stiles JK, Jolly CM, Aggarwal D. Human aflatoxicosis in developing countries: a review of toxicology, exposure, potential health consequences, and interventions. Am J Clin Nutr. 2004;80:1106–22.
Wagacha JM, Muthomi JW. Mycotoxin problem in Africa: current status, implications to food safety and health and possible management strategies. Int J Food Microbiol. 2008;124:1–12.
Gnonlonfin GJ, Hell K, Adjovi Y, et al. A review on aflatoxin contamination and its implications in the developing world: a sub-saharan african perspective. Crit Rev Food Sci Nutr. 2013;53:349–65.
Leroy JL, Wang JS, Jones K. Serum aflatoxin B(1)-lysine adduct level in adult women from Eastern Province in Kenya depends on household socio-economic status: a cross sectional study. Soc Sci Med. 2015;146:104–10.
Ba DM, Ssentongo P, Musa J, et al. Prevalence and determinants of cervical cancer screening in five sub-saharan african countries: a population-based study. Cancer Epidemiol. 2021;72:101930.
Chirwa GC. Explaining socioeconomic inequality in cervical cancer screening uptake in Malawi. BMC Public Health. 2022;22:1376.
Groopman JD, Kensler TW, Wild CP. Protective interventions to prevent aflatoxin-induced carcinogenesis in developing countries. Annu Rev Public Health. 2008;29:187–203.
Peles F, Sipos P, Kovacs S, Gyori Z, Pocsi I, Pusztahelyi T. Biological control and mitigation of aflatoxin contamination in commodities. Toxins (Basel). 2021;13(2):104. https://doi.org/10.3390/toxins13020104.
Sipos P, Peles F, Brasso DL, et al. Physical and chemical methods for reduction in aflatoxin content of feed and food. Toxins (Basel). 2021;13(3):204. https://doi.org/10.3390/toxins13030204.
Saeed F, Nadeem M, Ahmed R, Nadeem M, Arshad M, Ullah A. Studying the impact of nutritional immunology underlying the modulation of immune responses by nutritional compounds – a review. Food and Agricultural Immunology. 2016;27:205–29.
Gravitt PE. Evidence and impact of human papillomavirus latency. Open Virol J. 2012;6:198–203.
Weaver B, Shew M, Qadadri B, et al. Low-level persistence of human papillomavirus 16 DNA in a cohort of closely followed adolescent women. J Med Virol. 2011;83:1362–9.
Ermel A, Shew ML, Imburgia TM, et al. Redetection of human papillomavirus type 16 infections of the cervix in mid-adult life. Papillomavirus Res. 2018;5:75–9.
Paul P, Hammer A, Rositch AF, et al. Rates of New Human Papillomavirus Detection and loss of detection in Middle-aged women by recent and past sexual behavior. J Infect Dis. 2021;223:1423–32.
Acknowledgements
We thank the nurses at the Cervical Cancer Screening Program at Moi Referral and Teaching Hospital for their hard work, kindness, and attention to detail.
Funding
National Cancer Institute, United States, 1U54CA190151-01, and National Cancer Institute, United States, P30 CA082709.
Author information
Authors and Affiliations
Contributions
YT contributed to conceptualization, methodology, data curation, formal analysis, validation, writing (original, review and editing).PT contributed to study supervision, investigation, writing (review and editing). OO contributed to funding acquisition, project administration, and writing (review and editing). JZ contributed to funding acquisition, writing (review and editing). TM contributed to investigation (performance of laboratory tests).KM contributed to study supervision and writing (review and editing).JG contributed to methodology, formal analysis, resources, and writing (review and editing). JS contributed to investigation (performance of laboratory tests).EM contributed to investigation (performance of laboratory tests).AE contributed to study supervision, and writing (review and editing). PL contributed to funding acquisition, project administration, and writing (review and editing). DB contributed to funding acquisition, project administration, conceptualization, methodology, study supervision, writing (original draft, review and editing). The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Study approval was granted from the local review board at Moi Teaching and Referral Hospital (MTRH) and Moi University, Eldoret, Kenya, the Kenya Medical Research Institute’s Scientific and Ethics Review Unit (KEMRI-SERU) and the Institutional Review Board of Indiana University. All participants provided written informed consent, either in Swahili or English, for participation in the study and for use of clinical specimens. All study procedures were performed in accordance with relevant guidelines and regulations outlined by the Ethics Review Boards indicated above.
Consent for publication
Not applicable.
Competing interests
Dr. Brown currently receives research funding and has received royalties and consulting fees in the past from Merck and Co., Inc. Dr. Brown serves on the Scientific Advisory Board for PDS, Inc.The other Authors do not possess any potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Frequency of HPV detections among women at the enrollment, 12-month and 24-month visits.
Additional file 2: Supplemental Table 2.
Ordinal logistic regression analyses of IARC HR-HPV, A9 HPV, Non-HPV 16 A9, A7 HPV, Non-HPV 18 A7, and LR-HPV detection (persistent detection vs. incidence detection vs. no detection) with plasma AFB1-lys detection, and demographic/behavioral characteristics of women.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tong, Y., Tonui, P., Orang’o, O. et al. Association of plasma aflatoxin with persistent detection of oncogenic human papillomaviruses in cervical samples from Kenyan women enrolled in a longitudinal study. BMC Infect Dis 23, 377 (2023). https://doi.org/10.1186/s12879-023-08323-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08323-8