Abstract
Background
Cytomegalovirus (CMV) has high seroprevalence, and its active infection is associated with several adverse prognoses in adult patients with acute respiratory distress syndrome (ARDS). However, the role of active CMV infection in ARDS-associated fibroproliferation is unknown. This study aimed at determining the association between active CMV infection and lung fibroproliferation in adult patients with ARDS.
Methods
We retrospectively reviewed the medical records of all adult patients with ARDS who were admitted to the intensive care unit (ICU) from January 2018 to December 2020 at a national university-affiliated hospital in China. Study subjects were divided into active and non-active CMV infection groups based on CMV DNAemia within a 28-day ICU hospitalization. Lung fibroproliferation was measured using chest high-resolution computed tomography (HRCT) and N-terminal peptide of serum procollagen III (NT-PCP-III) within the first 28 days of ICU admission. Pulmonary fibrosis, clinical features, laboratory findings, treatment measures, and clinical outcomes were compared between the two groups.
Results
Among the 87 ARDS patients included in this study, the incidence of active CMV infection was 16.1% within the 28-day ICU admission period. In logistic regression analyze, active CMV infection was found to be associated with higher pulmonary fibrogenesis, pulmonary fibrosis score, and NT-PCP-III level (P < 0.05). The duration of ICU stay in ARDS patients with active CMV infection was significantly higher than in those without active CMV infection (P < 0.05).
Conclusions
Among adult patients with ARDS, active CMV infection was related to poor clinical outcomes. Active CMV infection was associated with ARDS-associated fibroproliferation. Prophylactic and preemptive use of anti-CMV agents on pulmonary fibrosis should be assessed to determine a consensus therapeutic strategy.
Similar content being viewed by others
Introduction
Cytomegalovirus (CMV) is a latent infection virus that is widespread in the population [1]. CMV may reactivate under certain circumstances, and its hazardous nature has been proven, especially in immunosuppressed patients [2]. However, several studies have found that CMV reactivation also exists in immunocompetent patients with a critical illness [3]. Among those patients, the incidence of CMV reactivation, which is more than 30% is associated with prolonged length of mechanical ventilation, increased duration of hospital stay, and higher mortality [4].
The incidence of acute respiratory distress syndrome (ARDS) in the intensive care unit (ICU) is still higher than 10%, and the case fatality rate is even higher at 40% [5, 6]. Recent studies have shown that the incidence of CMV reactivation in ARDS patients is 22.0–27.3% and is also associated with adverse prognoses [7, 8]. Moreover, pulmonary fibrosis is one of the important reasons for the progressive aggravation of ARDS [9]. At present, in-vivo experiments and clinical research have preliminarily shown that active CMV infection induces pulmonary fibrogenesis, and the fibrogenesis may lead to the decline of pulmonary oxygenation among sepsis patients [10, 11]. However, in ARDS patients, the role of active CMV infection in lung fibroproliferation is not clear. Furthermore, chest high-resolution computed tomography (HRCT) and N-terminal peptide of serum procollagen III (NT-PCP-III) are considered reliable assessment methods for assessing ARDS-associated fibroproliferation [12, 13]. Therefore, this study aimed at investigating the association between active CMV infection and lung fibroproliferation in ARDS patients by chest HRCT and NT-PCP-III.
Methods
Patient screening
We retrospectively reviewed the medical records of all adult patients with ARDS who were admitted to the ICU between January 2018 and December 2020 at the First Affiliated Hospital of Guangzhou Medical University in China. CMV DNAemia was detected using real-time PCR for laboratory diagnosis of active CMV infection [14,15,16]. The study subjects were divided into active CMV infection (≧ 500 copies/mL) and non-active CMV infection groups (< 500 copies/mL) based on CMV DNAemia within a 28-day ICU hospitalization period. HRCT was recorded and NT-PCP-III was detected in the two groups at the set time interval. The Ethics Committees of the First Affiliated Hospital of Guangzhou Medical University approved the study protocol (No. GY-2021-K04).
Data collection
The clinical data of 87 patients, including clinical features, laboratory findings, treatment measures, and clinical outcomes, were extracted from the electronic records by two independent intensivists who subsequently cross-checked their records for data accuracy. Furthermore, disagreements were further adjudicated by a third independent reviewer (an authoritative expert). Finally, all case data were entered into the electronic database for statistical analysis.
Study definitions
The study met all of the following criteria: (1) the diagnostic criteria for ARDS (Berlin definition 2012) [9] within 24 h of ICU admission; (2) age > 18 years; (3) informed consent and retention of blood specimens; (4) chest HRCT was performed with the following intervals: admission to general ward ~ 28 days after ICU entry; (5) chest HRCT was performed ≧ 2 times; (6) interval between two chest HRCTs ≧ 7 days. Any of the following exclusion criteria was sufficient for exclusion: (1) pregnancy or lactation; (2) survival time < 72 h; (3) CMV not detected; (4) antiviral therapy before ICU admission; (5) presence of pulmonary fibrosis on the first chest HRCT.
CMV positive (active CMV infection) load values (CMV DNA) were calibrated to the HCMV World Health Organization Standard and relevant clinical study definitions, defined as a load greater than or equal to 500 copies/mL in plasma [14,15,16]. Included study subjects (87 cases) were tested for CMV at ICU admission, and tested for CMV at least once a week thereafter. Meanwhile, the management of those ARDS patients was strictly based on relevant treatment measures of international consensus [17], including low tidal volume ventilation, inspiratory pressure ventilation, prone positioning, etc.
Assessment of pulmonary fibrosis
Chest HRCT
Chest HRCT was performed in the supine position, and image data acquisition was completed with spiral scanning for the study subjects. All chest HRCT scans were performed at the end of inspiration. Chest HRCT scans were performed from the lung apex to the diaphragmatic crest, slice thickness: 1.25 mm, pitch: 10 mm; scanning conditions were: 120 kV, 250 mA, images were displayed in the matrix: 512 × 512, slice thickness: 1.25 mm, and high spatial resolution reconstruction. All images were taken as lung window (window width 2000 Hu, window position 550 Hu) and mediastinal window (window width 450 Hu, window position 55 Hu). The extent of fibrotic lesions was observed under lung window conditions.
Subsequently, three radiologists read and scored images individually, and the resulting scoring results were averaged. Furthermore, a radiologist judged between ground glass, grid, honeycomb, and solid variants, according to the Fleischner Society definitions for HRCT terminology in the lung [18]. The lungs were divided into three levels according to their anatomical structure in six locations: lung apex to aortic arch level, aortic arch to inferior pulmonary vein level, and inferior pulmonary vein to lung base level. The pattern of signs of pulmonary fibrosis included simple ground-glass opacity, the mixture of ground-glass opacity and grid shadow, simple grid shadow, and honeycomb. We further quantified and defined imaging findings as follows: First, we defined the occurrence of pulmonary fibrosis as ‘1’ and the absence of pulmonary fibrosis as ‘0.’ Second, we referred to Prof. Ellen L Burnham’s method for scoring based on the area occupied by signs of pulmonary fibrosis [12]: the extent of involvement for each pattern was assigned a numerical score, where 0 = no involvement, 1 ≦ 5% involvement/minimal/not normal, 2 = 5–25% involvement, 3 = 26–49% involvement, 4 = 50–75% involvement, and 5 ≧ 75% involvement. Assessment of lung fibroproliferation by chest HRCT was completed within 28 days of ICU admission.
NT-PCP-III
A clinical blood sample resource bank was established at our medical center, and we routinely collected and stored patient blood specimens at regular intervals after admission to the ICU when the patients or their relatives signed the informed consent form. The study was approved by the ethics review board of the First Affiliated Hospital of Guangzhou Medical University.
Serum samples were collected from each ARDS patient at the time of enrollment (Day 1, 28). Refer to a similar approach by the Prof. Xu [19], the method of serum collection: whole blood was collected in procoagulant tubes and centrifuged at 2500 rpm for 10 min, and serum in the supernatant was collected and stored at − 80 °C until detection. Serum levels of NT-PCP-III (Day 1 and Day 28) were measured by enzyme-linked immunosorbent assay (ELISA) (SEA573Hu, USCN, Houston, TX, Lot: L210714899) according to the manufacturer’s instructions.
Study outcomes
The primary outcomes of this study included the chest HRCT and NT-PCP-III differences between active and non-active CMV infection groups. Moreover, we also assessed secondary outcomes between the two groups, including clinical features, laboratory findings, treatment measures, and clinical outcomes.
Statistical analysis
All statistical analyses or charting were performed using SPSS (SPSS Inc., USA, version 25.0) and GraphPad Prism (GraphpadSoftware Inc., USA, version 8.0). Continuous variables were expressed as Mean ± SD or Median (interquartile ranges, IQRs) and were compared with the Wilcoxon rank-sum test. Categorical variables were expressed as counts and percentages and were compared using the Chi-square test or Fisher’s exact test as appropriate. Logistic regression was used to determine the association between active CMV infection and pulmonary fibrosis indicators, including chest HRCT scores and NT-PCP-III level. Correlation coefficients between chest HRCT scores and NT-PCP-III level were calculated using the Spearman correlation coefficient. Additionally, risk factors for active CMV infection were screened with the univariate logistic regression and the variables with a P < 0.05 was considered as the potential risk factors, furthermore, the potential risk factors were imported into the multivariate logistic regression analysis. The regression coefficient (β), odds ratio (OR), and 95% confidence interval (CI) were calculated for establishing the active CMV infection risk model. The predictive value of active CMV infection was evaluated by using the receiver operating characteristic (ROC) curve. Moreover, we further calculated the area under the ROC curve (AUC), specificity, sensitivity, 95% CI, and P-value. The significance threshold was set at a two-sided P < 0.05.
Results
Active CMV infection
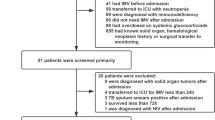
From January 2018 to December 2020, a total of 4261 patients were transferred to the ICU. As shown in Fig. 1, 4174 cases were excluded because of a non-ARDS diagnosis (n = 3987), lack of blood samples or chest HRCT (n = 81), non-CMV detection (n = 69), death within 72 h after ICU admission (n = 23), pregnancy or lactation (n = 7), juveniles (n = 5), and receiving antiviral therapy before ICU entry (n = 2). Eventually, 87 cases were enrolled with complete data for analysis. Furthermore, 14 of 87 cases (16.1%) had active CMV infection; so, the study subjects were divided into an active CMV infection group (n = 14, 16.1%) and a non-active CMV infection group (n = 73, 83.9%).
Patients’ features
The clinical features of 87 patients enrolled in the study are presented in Table 1. The study included 87 cases for statistical analysis, of whom 52 were male (59.8%). The mean age of the study population was 56 ± 16 years. Of the patients, 16 (18.4%) had mild ARDS, 40 (46.0%) had moderate ARDS, and 31 (35.6%) had severe ARDS. The patients’ condition was severe because the scores for APACHE II (median: 19) and SOFA (median: 9) were high. Severe pneumonia (94.3%) is the main cause of ARDS. The main comorbidities were cardiovascular diseases (n = 27, 31.0%), hypertension (n = 25, 28.7%), and diabetes (n = 15, 17.2%). Nevertheless, the differences in those clinical features between the two groups were not significant.
Furthermore, laboratory findings of the study subjects at ICU admission are presented in Table 2. The active CMV infection group showed lower platelet counts [median: 71 vs. 151 (109/L), P = 0.013] and NK cell proportion [median: 4.7 vs. 11.9 (%), P = 0.030] than the non-active CMV infection group. There were, however, no significant differences in other laboratory findings between the two groups.
Pulmonary fibrosis
The association between active CMV infection and lung fibroproliferation is shown in Table 3, Additional file 1: Table S1, and Fig. 2. Pulmonary fibrogenesis [64.3% vs. 34.3% (n), P = 0.035], pulmonary fibrosis score [median: 1 vs. 0 (d), P = 0.031], and NT-PCP-III level (Day 1) [median: 62.3 vs. 36.5 (ng/mL), P = 0.015] in patients with active CMV infection were significantly higher than in those without active CMV infection. The level of NT-PCP-III (Day 28) [median: 61.9 vs. 43.8 (ng/mL), P = 0.317] was high in cases with active CMV infection than in cases with non-active CMV infection, although statistical significance was not reached. In the logistic regression analyses, higher pulmonary fibrogenesis [β: 1.240, OR: 3.456, 95% CI 1.046–11.421, P = 0.042], pulmonary fibrosis score [β: 0.895, OR: 2.447, 95% CI 1.042–5.748, P = 0.040], and NT-PCP-III level (Day 1) [β: 0.018, OR: 1.019, 95% CI 1.001–1.036, P = 0.038] were found to be associated in patients with active CMV infection. Furthermore, the Spearman analysis revealed strong correlation [r = 0.249, P = 0.020] between chest HRCT score and NT-PCP-III (Day 1), as shown in Additional file 1: Table S2.
Treatment measures, complications, and clinical outcomes
It is clear from Table 4 that significantly more patients with active CMV infection underwent blood transfusion [35.7% vs. 11.0% (n), P = 0.049] and antiviral therapy [100% vs. 0% (n), P < 0.001] than patients with non-active CMV infection.
Moreover, compared to the non-active CMV infection group, the number of ARDS patients with septic shock complications [92.9% vs. 58.9% (n), P = 0.034] was higher in the active CMV infection group. Nevertheless, there were no statistically significant differences for other treatment measures and complications between the two groups.
As shown in Additional file 1: Table S3, in the multivariate regression model, platelet [OR: 0.991, 95% CI 0.983–1.000, P = 0.042] and septic shock [OR: 9.097, 95% CI 1.097–75.453, P = 0.041] were independently associated with active CMV infection in ARDS patients. Based on the regression coefficient (β), platelet [β: − 0.009] was an inhibitory factor and septic shock [β: 2.208] was a promotive factor for active CMV infection. We further plotted ROC curves for platelet to assess the active CMV infection predictive value. From Additional file 1: Table S4, it can be seen that the AUC of platelet was 0.711 [Specificity: 88.7%, Sensitivity: 50.0%; 95% CI 0.562–0.860; P = 0.013], so platelet had a moderate predictive value for active CMV infection. The pathogens caused by ARDS is shown in Additional file 1: Table S5, but the differences in those pathogens between the two groups were not significant. And the detection time-point of CMV DNAemia and chest HRCT Scans are shown in Additional file 1: Table S6.
From Table 4, the duration of ICU stay [median: 51 vs. 29 (d), P = 0.035] was significantly higher in the active CMV infection group than in the non-active CMV infection group. Although statistical significance was not reached, the duration of hospital stay [median: 56 vs. 39 (d), P = 0.330], length of invasive mechanical ventilation (IMV) [median: 40 vs. 24 (d), P = 0.072], and the in-hospital mortality rate [14.3% vs. 8.2% (n), P = 0.830] were lower in cases without active CMV infection than in cases with active CMV infection.
Discussion
This study aimed at determining the association between active CMV infection and lung fibroproliferation in adult patients with ARDS. Among adult patients with ARDS, the incidence of active CMV infection was 16.1%. In addition, clinical characteristics, including laboratory findings (lower level of platelet and NK cells), blood transfusion, and septic shock, were related to active CMV infection. Most importantly, further correlation statistical analysis revealed that active CMV infection was associated with pulmonary fibrosis based on chest HRCT and NT-PCP-III. Additionally, active CMV infection was associated with several adverse prognoses.
Active CMV infection is not an uncommon phenomenon in critically ill patients. Our research team’s systematic review and meta-analysis have shown that the incidence of reactivation in immunocompetent patients is up to 31% in critical care settings [4]. In a prospective, multicenter epidemiological study that enrolled 399 patients with ARDS, 271 (68%) cases were CMV seropositive, and reactivation occurred in 74 (27%) of them; so the incidence of active CMV infection was 18.6% [7]. An additional study, which enrolled 123 ARDS patients receiving extracorporeal membrane oxygenation (ECMO), revealed that CMV DNAemia occurred at any level in 22.0% of the patients [8]. Due to the different inclusion and exclusion criteria, diagnostic methods, and specimen detection, the above incidence was slightly different from the results of this study. In particular, the detection methods (time points and monitoring periods) of CMV in different studies may have an effect on the incidence of active CMV infection. The present study was retrospective and could not detect each time point clearly; so, the incidence of active CMV infection may be lower than the real situation. It is also essential to note that our study used blood DNAemia for evaluating active CMV infection, which might underestimate the active CMV infection, combined with a more comprehensive detection of lower respiratory tract specimens.
Previous studies have verified that low-level platelet and NK cells, blood transfusion, and septic shock are associated with active CMV infection [3, 20, 21], consistent with this study's results. The reason behind these associations is related to the direct pathological damage and indirect damage.
The inhibition of platelet and NK cells may be related to the damage caused by CMV infection to the hematopoiesis and immune system [21,22,23]. Specifically, for bone marrow transplantation patients, CMV infection causes delayed platelet recovery [23]. CMV infection can inhibit NK cells through driving adaptive epigenetic diversification with altered signaling and effector function [21, 24]. Moreover, active CMV infection through blood transfusion is a risk in treating patients with a critical illness. A study has indicated that donations from new CMV-IgG-positive donors bear the highest risk for transmitting CMV infections because they contain elevated CMV-DNA levels, a risk factor for active CMV infection [25]. Several studies have found that sepsis is associated with active CMV infection [10, 19, 26, 27]. An in vivo model has shown that inflammatory factors such as lipopolysaccharide (LPS), tumor necrosis factor-alpha (TNF-α), and interleukin-1beta (IL-1β) are associated with sepsis and could activate CMV immediate early genes and promote viral replication [28]. From clinical studies, it has also been speculated that CMV reactivation is associated with multiple inflammatory factors (IL-6 and TNF-α) [29, 30]. There was an interaction between septic shock and active CMV infection. However, there were cases of prolonged mechanical ventilation causeing ventilator-acquired pneumonia clinically, which might also lead to sepsis-related active CMV infection, though no statistically significant difference was reached between these pathogens and active CMV infection. Therefore, the limited sample size and unmeasured confounders were the inadequacies of this study.
Furthermore, our results showed that septic shock and platelet were independent risk factors for active CMV infection and were independent of each other in the study subjects. It was further found that platelet levels had a moderate value for predicting active CMV infection. The mechanisms through which septic shock causes active CMV infection have been described above, and this result was consistent with most of the current studies. Nonetheless, no relevant study is consistent with our results, and the association between CMV and platelet has never been shown before. Platelets are small masses of cytoplasm released from the cytoplasm of mature megakaryocytes in the bone marrow and are extremely important for the body’s hemostatic function. However, the latest view considers that platelets can be an important mediator of immunity and inflammation [31]. In allogeneic bone marrow transplantation recipients, platelet recovery was significantly slower in CMV-positive patients than in CMV-negative patients, the condition may be related to CMV-associated myelosuppression [23]. Evidence for the association between CMV and myelosuppression has been provided from in vitro/vivo studies and clinical studies, those results indicated the direct infection of hematopoietic progenitors and that the supportive microenvironment is infected, thereby compromising its supportive function [32]. Importantly, more patients need to be included for further confirmation of the role of platelets. Meanwhile, it needs to be emphasized that the relatively small sample size in this study opens the possibility for a type II error.
Current treatment protocols for ARDS continue to evolve and be refined; nevertheless, its incidence and case fatality remain high [5, 6]. Pulmonary fibrosis is a common complication of ARDS, and its severity significantly influences clinical outcomes and long-term quality of life in ARDS patients [33]. Multiple factors have been associated with ARDS-associated fibroproliferation, in which viral infection plays an important role, but the role of CMV infection in this is not definite. At present, in vitro results have shown that CMV from latent infection in the lung could undergo reactivation under LPS intervention, and active CMV infection could lead to the development of fibrosis in the lungs of mice [11]. Besides, a clinical study showed that active CMV infection could influence the oxygenation function (PaO2/FiO2) of critically ill patients with sepsis [10]. In summary, we hypothesized that active CMV infection was associated with pulmonary fibrosis leading to low oxygenation levels in ARDS patients; so, we further designed and carried out this study. There is no relevant clinical research consistent with our results, and the association between active CMV infection and lung fibroproliferation in adult patients with ARDS has never been studied before. We found that active CMV infection was associated with ARDS-associated fibroproliferation based on chest HRCT and NT-PCP-III. The active CMV infection group had a lower oxygenation level than the non-active CMV infection group, although statistical differences have not been observed. This revealed that CMV could damage the respiratory barrier, leading to pulmonary fibrosis and subsequently to decreased oxygenation. There is not well-established method to assess CT image of ARDS associated the lung fibrosis, thus in the study, we adapted the scoring system of CT image which is commonly used in evaluation of pulmonary fibrosis which is characterized by honeycombing. In this study, ARDS patients do not show typical honeycombing on HRCT scans. Meanwhile, pulmonary fibrosis once present in HRCT was largely refractory to disappear, so excluded patients with pulmonary fibrosis at the first HRCT scan who had excluded pre-existing pulmonary fibrosis. Moreover, the level of NT-PCP-III (Day 28) was high in cases with active CMV infection than in cases with non-active CMV infection, although statistical significance is not reached. Only 38 patients (6 in active CMV infection group and 32 in non-active group) still stayed in ICU on day 28 and NT-PCP-III were evaluated in these patients. The relatively small sample may be the potential reason for negative correlation between active CMV infection and NT-PCP-III at day 28. Furthermore, antiviral therapy was used in the active CMV infection group which effectively in suppressing the virus and reduced pulmonary fibroproliferation.
In addition, our assessment of pulmonary fibrosis using chest HRCT and NT-PCP-III is clinically feasible; both of these are reliable diagnostic methods or markers for ARDS-associated lung fibroproliferation [12, 13, 34], with the advantages of non-invasiveness and high specificity. Our results also found that chest HRCT score and NT-PCP-III had a strong correlation. Although lung histopathology is the gold standard, performing open lung biopsies in ARDS patients is complicated. Besides, the testing time points for chest HRCT were not consistent, and the endpoints were 28 days after admission to the ICU, and testing samples for NT-PCP-III were sera, which are slightly less sensitive relative to lower respiratory specimens (endotracheal aspirate or bronchoalveolar lavage fluid). Thus, the incidence of pulmonary fibrosis may have been underestimated. Furthermore, the source of fibrosis is also a matter of concern. Studies have shown that CMV infection could lead to epithelial–mesenchymal transition (EMT) in various cells, and continuous EMT is closely related to organ fibrosis [35,36,37]. EMT refers to the biological process in which epithelial cells lose epithelial characteristics and obtain mesenchymal characteristics under some physiological or pathological conditions [38]. EMT is transient and reversible, depending on its biological and functional environment, so preventive or preemptive anti-CMV treatment may benefit ARDS patients. In addition, the current studies have revealed that some patients occurred pulmonary fibrosis after COVID-19 pulmonary infection owing to SARS-CoV-2 infection promoted the occurrence of lung fibroproliferation [39, 40]. Due to the outbreak control requirements of the Chinese government, all patients with confirmed COVID-19 diseases were sent to the specialized infectious disease hospital or department for isolation and treatment. Therefore, no patients with COVID-19 pulmonary infection were included during this study period. Hemopexin (hx) level of pulmonary disease was associated with lung fibroproliferation [41, 42], but the study lacked detection of hx.
Most studies have shown that active CMV infection was associated with several poor clinical outcomes, which is consistent with our results, including prolonged duration of mechanical ventilation, hospitalization and ECMO, and increased complications and mortality [2,3,4, 7, 8, 10, 20, 23, 26,27,28,29,30]. The mechanisms include direct CMV pathogenicity or indirect CMV effects such as CMV-mediated immunosuppression and CMV-mediated lung injury [29, 43]. Moreover, the cause of death in both groups was multiple organ dysfunction syndrome in this study. Furthermore, the main cause of death in the active CMV infection group was multiorgan failure. As a matter of fact, it is very hard to tell the exact attribution to death when the patient is being in the end-stage of ARDS in clinical practice. In most cases, we believe that above conditions may contribute to the death of ARDS patients, the attribution of pulmonary fibroproliferation to death of ARDS patients need to be evaluated in a prospective well controlled study. In addition, the notable role of antiviral therapy in active CMV infection is well established. However, the preemptive and prophylactic application of anti-CMV therapy remains controversial for non-immunosuppressed patients [30, 44, 45], and the role of preemptive and prophylactic anti-CMV therapy in pulmonary fibrosis, which is not clear, should be further investigated in future studies.
This study has several limitations. First, it was a single-center retrospective study, so the time points at which CMV detections and chest HRCT scans were made were difficult to be determined. Therefore, the timing of when CMV was detected relative to admission and relative to HRCT scans might affect assessment of the association between active CMV infection and lung fibroproliferation. Second, only active infection, and not reactivation, could be assessed because of the lack of detection of CMV IgG. Third, the number of patients included was relatively insufficient to comprehensively evaluate the epidemiological characteristics and lung fibroproliferation of CMV for adult patients with ARDS. Fourth, due to the lack of CMV and NT-PCP-III detection in the lower respiratory tract, we could not further assess the association between CMV and NT-PCP-III among ARDS patients. Therefore, a prospective, multicenter study is needed in the future, and more study participants with ARDS should be included. Moreover, the effect of prophylactic and preemptive therapy using anti-CMV agents for pulmonary fibrosis should be evaluated in ARDS patients. Eventually, further assessment of the effect of CMV in the airways of ARDS-associated fibroproliferation markers is urgently needed.
Conclusions
The incidence of active CMV infection was 16.1% in adult patients with ARDS. Active CMV infection was related to adverse clinical outcomes, including prolonged ICU hospitalization. Moreover, active CMV infection was associated with ARDS-associated fibroproliferation based on chest HRCT and NT-PCP-III. Therefore, further evaluation of the prophylactic and preemptive therapy using anti-CMV agents for pulmonary fibrosis should be conducted in the future to identify a consistent treatment strategy.
Availability of data and materials
The datasets generated during and analyzed during the current study are not publicly available due to patients privacy but are available from the corresponding author on reasonable request.
Abbreviations
- CMV:
-
Cytomegalovirus
- ICU:
-
Intensive care unit
- ARDS:
-
Acute respiratory distress syndrome
- HRCT:
-
High-resolution computed tomography
- NT-PCP-III:
-
N-terminal peptide of serum procollagen III
- MV:
-
Mechanical ventilation
- IMV:
-
Invasive mechanical ventilation
- BMI:
-
Body Mass Index
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- SOFA:
-
Sequential Organ Failure Assessment
- qSOFA:
-
Quick Sequential Organ Failure Assessment
- CAP:
-
Community-acquired pneumonia
- HAP:
-
Hospital-acquired pneumonia
- P/F:
-
PaO2/FiO2
- QRT-PCR:
-
Quantitative real-time polymerase chain reaction
- COPD:
-
Chronic obstructive pulmonary disease
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thromboplastin time
- NT-proBNP:
-
N-terminal Pro-B-type Natriuretic Peptide
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine transaminase
- T-BIL:
-
Total bilirubin
- Scr:
-
Serum creatinine
- BUN:
-
Serum urea nitrogen
- Hb:
-
Hemoglobin
- Th:
-
T-helper lymphocytes
- Ts:
-
T-suppressor lymphocytes
- NK:
-
Natural killer
- IL:
-
Interleukin
- TNF:
-
Tumor necrosis factor
- INF:
-
Interferon
- CRRT:
-
Continuous renal replacement therapy
- ECMO:
-
Extracorporeal membrane oxygenation
- AKI:
-
Acute kidney injury
- DIC:
-
Disseminated intravascular coagulation
- AHF:
-
Acute heart failure
- AECOPD:
-
Acute exacerbation of chronic obstructive pulmonary disease
- VFD:
-
Ventilator-free days
- IQRs:
-
Interquartile ranges
- r:
-
Correlation coefficient
- β:
-
Regression coefficient
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the ROC curve
- CI:
-
95% Confidence interval
- LPS:
-
Lipopolysaccharide
- EMT:
-
Epithelial mesenchymal transition
- Hx:
-
Hemopexin
- ETA:
-
Endotracheal aspirates
- G+ :
-
Gram-positive
- G− :
-
Gram-negative
References
Zuhair M, Smit GSA, Wallis G, et al. Estimation of the worldwide seroprevalence of cytomegalovirus: a systematic review and meta-analysis. Rev Med Virol. 2019;29(3):e2034. https://doi.org/10.1002/rmv.2034.
Griffiths P. Burden of disease associated with human cytomegalovirus and prospects for elimination by universal immunisation. Lancet Infect Dis. 2012;12(10):790–8. https://doi.org/10.1016/S1473-3099(12)70197-4.
Al-Omari A, Aljamaan F, Alhazzani W, et al. Cytomegalovirus infection in immunocompetent critically ill adults: literature review. Ann Intensive Care. 2016;6(1):110. https://doi.org/10.1186/s13613-016-0207-8.
Li X, Huang Y, Xu Z, et al. Cytomegalovirus infection and outcome in immunocompetent patients in the intensive care unit: a systematic review and meta-analysis. BMC Infect Dis. 2018;18(1):289. https://doi.org/10.1186/s12879-018-3195-5.
Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800. https://doi.org/10.1001/jama.2016.0291.
Villar J, Blanco J, Kacmarek RM. Current incidence and outcome of the acute respiratory distress syndrome. Curr Opin Crit Care. 2016;22(1):1–6. https://doi.org/10.1097/MCC.0000000000000266.
Ong DSY, Spitoni C, Klein Klouwenberg PMC, et al. Cytomegalovirus reactivation and mortality in patients with acute respiratory distress syndrome. Intensive Care Med. 2016;42(3):333–41. https://doi.org/10.1007/s00134-015-4071-z.
Hraiech S, Bonnardel E, Guervilly C, et al. Herpes simplex virus and cytomegalovirus reactivation among severe ARDS patients under veno-venous ECMO. Ann Intensive Care. 2019;9(1):142. https://doi.org/10.1186/s13613-019-0616-6.
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–33. https://doi.org/10.1001/jama.2012.5669.
Heininger A, Haeberle H, Fischer I, et al. Cytomegalovirus reactivation and associated outcome of critically ill patients with severe sepsis. Crit Care. 2011;15(2):R77. https://doi.org/10.1186/cc10069.
Cook CH, Zhang Y, Sedmak DD, et al. Pulmonary cytomegalovirus reactivation causes pathology in immunocompetent mice. Crit Care Med. 2006;34(3):842–9. https://doi.org/10.1097/01.ccm.0000201876.11059.05.
Burnham EL, Hyzy RC, Paine R 3rd, et al. Detection of fibroproliferation by chest high-resolution CT scan in resolving ARDS. Chest. 2014;146(5):1196–204. https://doi.org/10.1378/chest.13-2708.
Forel JM, Guervilly C, Hraiech S, et al. Type III procollagen is a reliable marker of ARDS-associated lung fibroproliferation. Intensive Care Med. 2015;41(1):1–11. https://doi.org/10.1007/s00134-014-3524-0.
Fryer JF, Heath AB, Anderson R, et al. Collaborative study to evaluate the proposed 1st WHO International Standard for Human Cytomegalovirus (HCMV) for nucleic acid amplification (NAT)-based assays. WHO/BS/10/2138. Geneva: World Health Organization; 2010.
Ljungman P, Boeckh M, Hirsch HH, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. 2017;64(1):87–91. https://doi.org/10.1093/cid/ciw668.
Kotton CN, Kumar D, Caliendo AM, et al. The third international consensus guidelines on the management of cytomegalovirus in solid-organ transplantation. Transplantation. 2018;102(6):900–31. https://doi.org/10.1097/TP.0000000000002191.
Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319(7):698–710. https://doi.org/10.1001/jama.2017.21907.
Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266(1):304–17. https://doi.org/10.1148/radiol.12120628.
Xu Z, Li X, Huang Y, et al. The predictive value of plasma galectin-3 for ARDS severity and clinical outcome. Shock. 2017;47(3):331–6. https://doi.org/10.1097/SHK.0000000000000757.
Zhang Z, Liu X, Sang L, et al. Cytomegalovirus reactivation in immunocompetent mechanical ventilation patients: a prospective observational study. BMC Infect Dis. 2021;21(1):1026. https://doi.org/10.1186/s12879-021-06698-0.
Barnes S, Schilizzi O, Audsley KM, et al. Deciphering the immunological phenomenon of adaptive natural killer (NK) cells and cytomegalovirus (CMV). Int J Mol Sci. 2020;21(22):8864. https://doi.org/10.3390/ijms21228864.
Renzaho A, Podlech J, Kühnapfel B, et al. Cytomegalovirus-associated inhibition of hematopoiesis is preventable by cytoimmunotherapy with antiviral CD8 T Cells. Front Cell Infect Microbiol. 2020;10:138. https://doi.org/10.3389/fcimb.2020.00138.
Verdonck LF, de Gast GC, van Heugten HG, et al. Cytomegalovirus infection causes delayed platelet recovery after bone marrow transplantation. Blood. 1991;78(3):844–8.
Schlums H, Cichocki F, Tesi B, et al. Cytomegalovirus infection drives adaptive epigenetic diversification of NK cells with altered signaling and effector function. Immunity. 2015;42(3):443–56. https://doi.org/10.1016/j.immuni.2015.02.008.
Ziemann M, Thiele T. Transfusion-transmitted CMV infection—current knowledge and future perspectives. Transfus Med. 2017;27(4):238–48. https://doi.org/10.1111/tme.12437.
Imlay H, Dasgupta S, Boeckh M, et al. Risk factors for cytomegalovirus reactivation and association with outcomes in critically ill adults with sepsis: a pooled analysis of prospective studies. J Infect Dis. 2021;223(12):2108–12. https://doi.org/10.1093/infdis/jiaa697.
von Müller L, Klemm A, Weiss M, et al. Active cytomegalovirus infection in patients with septic shock. Emerg Infect Dis. 2006;12(10):1517–22. https://doi.org/10.3201/eid1210.060411.
Cook CH, Trgovcich J, Zimmerman PD, et al. Lipopolysaccharide, tumor necrosis factor alpha, or interleukin-1beta triggers reactivation of latent cytomegalovirus in immunocompetent mice. J Virol. 2006;80(18):9151–8. https://doi.org/10.1128/JVI.00216-06.
Papazian L, Hraiech S, Lehingue S, et al. Cytomegalovirus reactivation in ICU patients. Intensive Care Med. 2016;42(1):28–37. https://doi.org/10.1007/s00134-015-4066-9.
Limaye AP, Stapleton RD, Peng L, et al. Effect of ganciclovir on IL-6 levels among cytomegalovirus-seropositive adults with critical illness: a randomized clinical trial. JAMA. 2017;318(8):731–40. https://doi.org/10.1001/jama.2017.10569.
Koupenova M, Clancy L, Corkrey HA, et al. Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ Res. 2018;122(2):337–51. https://doi.org/10.1161/CIRCRESAHA.117.310795.
Randolph-Habecker J, Iwata M, Torok-Storb B. Cytomegalovirus mediated myelosuppression. J Clin Virol. 2002;25(Suppl 2):S51-56. https://doi.org/10.1016/s1386-6532(02)00092-6.
Herridge MS, Tansey CM, Matté A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–304. https://doi.org/10.1056/NEJMoa1011802.
Hamon A, Scemama U, Bourenne J, et al. Chest CT scan and alveolar procollagen III to predict lung fibroproliferation in acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):42. https://doi.org/10.1186/s13613-019-0516-9.
Shimamura M, Murphy-Ullrich JE, Britt WJ, et al. Human cytomegalovirus induces TGF-β1 activation in renal tubular epithelial cells after epithelial-to-mesenchymal transition. PLoS Pathog. 2010;6(11):e1001170. https://doi.org/10.1371/journal.ppat.1001170.
Teo WH, Chen HP, Huang JC, et al. Human cytomegalovirus infection enhances cell proliferation, migration and upregulation of EMT markers in colorectal cancer-derived stem cell-like cells. Int J Oncol. 2017;51(5):1415–26. https://doi.org/10.3892/ijo.2017.4135.
Cobbs C. Cytomegalovirus is a tumor-associated virus: armed and dangerous. Curr Opin Virol. 2019;39:49–59. https://doi.org/10.1016/j.coviro.2019.08.003.
Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15(3):178–96. https://doi.org/10.1038/nrm3758.
Mylvaganam RJ, Bailey JI, Sznajder JI, et al. Recovering from a pandemic: pulmonary fibrosis after SARS-CoV-2 infection. Eur Respir Rev. 2021;30(162):210194. https://doi.org/10.1183/16000617.0194-2021.
Wendisch D, Dietrich O, Mari T, et al. SARS-CoV-2 infection triggers profibrotic macrophage responses and lung fibrosis. Cell. 2021;184(26):6243-6261.e27. https://doi.org/10.1016/j.cell.2021.11.033.
Buehler PW, Swindle D, Pak DI, et al. Hemopexin dosing improves cardiopulmonary dysfunction in murine sickle cell disease. Free Radic Biol Med. 2021;175:95–107. https://doi.org/10.1016/j.freeradbiomed.2021.08.238.
Aggarwal S, Ahmad I, Lam A, et al. Heme scavenging reduces pulmonary endoplasmic reticulum stress, fibrosis, and emphysema. JCI Insight. 2018;3(21):e120694. https://doi.org/10.1172/jci.insight.120694.
Vergara A, Cilloniz C, Luque N, et al. Detection of human cytomegalovirus in bronchoalveolar lavage of intensive care unit patients. Eur Respir J. 2018;51(2):1701332. https://doi.org/10.1183/13993003.01332-2017.
Cowley NJ, Owen A, Shiels SC, et al. Safety and efficacy of antiviral therapy for prevention of cytomegalovirus reactivation in immunocompetent critically ill patients: a randomized clinical trial. JAMA Intern Med. 2017;177(6):774–83. https://doi.org/10.1001/jamainternmed.2017.0895.
Papazian L, Jaber S, Hraiech S, et al. Preemptive ganciclovir for mechanically ventilated patients with cytomegalovirus reactivation. Ann Intensive Care. 2021;11(1):33. https://doi.org/10.1186/s13613-020-00793-2.
Acknowledgements
Thanks to the Biobank for Respiratory Diseases in the National Clinical Research Center for Respiratory Disease (BRD-NCRCRD, Guangzhou, Southern China). We thank Prof. Xu for guidelines on methods for the extraction of blood samples.
Accordance statement
All methods were performed in accordance with the relevant guidelines and regulations.
Funding
The study was funded by the National Natural Science Foundation of China (Nos. 81970071, 82070084), Science and Technology Program of Guangzhou (No. 202102010366), and Guangzhou Medical University Students Extracurricular Academic Technology Project (Nos. 2020A012, 2021A016).
Author information
Authors and Affiliations
Contributions
ZHZ, YML, and XQL conceived and designed the study; ZHZ, RJL, YBC, JRZ, YXZ, MMX, JQL, JHL, YBH, and YHX collected and aggregated data; ZHZ analyzed the data and wrote the manuscript; YML, XQL, and WQH reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Ethics Committees of the First Affiliated Hospital of Guangzhou Medical University approved the protocol (No. GY-2021-K04), and written informed consent was obtained from the patients or surrogates to retain patient blood samples.
Consent for publication
Not applicable.
Competing interests
None of the authors has any conflict of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Assessment of pulmonary fibrosis by HRCT and NT-PCP-III. Table S2. Correlation analysis of chest HRCT Score and NT-PCP-III. Table S3. Risk factors for active CMV infection. Table S4. Predictive value of platelet on active CMV infection evaluated by ROC. Table S5. Bacterial and fungal species. Table S6. Detection Time-point of CMV DNAemia and Chest HRCT Scans.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Z., Li, R., Chen, Y. et al. Association between active cytomegalovirus infection and lung fibroproliferation in adult patients with acute respiratory distress syndrome: a retrospective study. BMC Infect Dis 22, 788 (2022). https://doi.org/10.1186/s12879-022-07747-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07747-y