Abstract
Introduction
Approximately 20 years have passed since we reported our results of histologically proven cytomegalovirus (CMV) pneumonia in non-immunocompromised ICU patients. Even if there are more recent reports suggesting that CMV may worsen the outcomes for ICU patients, there is no definite answer to this question: is CMV a potential pathogen for ICU patients or is it simply a bystander?
Methods
We will describe the pathophysiology of active CMV infection and the most recent insights concerning the epidemiological aspects of these reactivations.
Major findings
Cytomegalovirus can be pathogenic by a direct organ insult (such as for the lung), by decreasing host defences against other microorganisms and/or by enhancing the body’s inflammatory response (as in acute respiratory distress syndrome). The incidence of active CMV infection is dependent on the diagnostic method used. Using the most sophisticated available biological tools, the incidence can reach 15–20 % of ICU patients (20–40 % in ICU patients with positive CMV serology). In adequately powered cohorts of patients, active CMV infection appears to be associated with worse outcomes for mechanically ventilated ICU patients.
Discussion
There is no absolute direct proof of a negative impact of active CMV infection on the health outcomes of mechanically ventilated patients. Prospective randomized trials are lacking. Future trials should examine the potential benefits for health outcomes of using antiviral treatments. Such treatments could be prophylactic, pre-emptive or used only when there is an end-organ disease.
Conclusion
Cytomegalovirus infection may affect health outcomes for ICU patients. Additional prospective trials are necessary to confirm this hypothesis.
Similar content being viewed by others
Introduction
Primary infection due to cytomegalovirus (CMV) is generally asymptomatic or characterized by the presence of non-specific signs and symptoms. Previous infection is confirmed by the presence of CMV-specific IgG responses. Approximately 60–80 % of immunocompetent adults are human CMV seropositive [1, 2]. Following primary infection, CMV remains quiescent in monocytes and macrophages in multiple organs, a state defined as latency. As with other herpesviridae, this harbouring of latent CMV makes this affected population at risk for reactivation, especially during critical illness. Primary infection or reinfection with a different strain of CMV during the ICU stay is theoretically possible (blood products) but is unlikely due to leucoreduction processes. While the potential for CMV reactivation in ICU patients is now acknowledged, much controversy remains over its pathogenicity. Indeed, CMV could be pathogenic or simply an associated sign reflecting the severity of underlying disease.
Several mechanisms have been proposed to explain how CMV reactivation could cause injury. The first is a direct cytopathologic effect from the reactivated virus injuring organs that harboured the virus such as during CMV pneumonia [3–5]. The second mechanism is an immunopathological effect, in which damage to tissues is caused by the excessive immune response to the virus such as that hypothesised in ARDS patients [6]. The third mechanism is related to an alteration of patients’ immune defences, rendering them more susceptible to fungal and bacterial infections [7–10]. However, CMV reactivation could only be an indicator of immune compromise and illness severity not necessitating diagnostic procedures and treatment.
Why we did this study
As with many things in medicine, our story began with an unexpected observation, which occurred during the controversy between intensive care practitioners who maintained the use of a protected specimen brush (PSB) for the diagnosis of bacteriological ventilator-associated pneumonia (VAP) and those who preferred the use of tracheal aspirates (TA) (as we did). This was the reason why we designed a study evaluating the diagnostic performance of several microbiological sampling techniques such as PSB, bronchoalveolar lavage (BAL), TA and protected telescopic catheter for the diagnosis of VAP [11]. The gold standard was lung histology and lung culture following pneumonectomy. Our work has had two major consequences. First, our surgical colleagues became convinced that performing an open-lung biopsy (OLB) was feasible at the bedside, in the ICU, in mechanically ventilated patients. It was why we started to perform OLBs at the bedside [5]. The second consequence was that our pathologist colleagues reported that in some instances they did not identify any sign of bacterial pneumonia but found typical signs of CMV pneumonia that were confirmed using specific immunological markers. After a dubitative period, we decided to extend the use of OLBs, especially with the aim to identify authentic histological CMV pneumonia [4].
Methods and major findings of our study
During a 5-year period, autopsies were performed in patients who died while they presented a clinical picture of VAP with negative microbiological cultures (BAL, PSB, TA). In some patients who had an unexplained worsening of their respiratory status while under invasive mechanical ventilation, an OLB was performed. Immunocompromised patients were excluded from the study. We defined ventilator-associated CMV pneumonia as the association of a mechanical ventilation duration exceeding 7 days with the presence of histopathological signs of CMV pneumonia (e.g., identification of large cells with large nuclei containing a basophilic or eosinophilic inclusion surrounded by a light halo). Sixty autopsies and 26 OLBs were performed during the study period. On the basis of our criteria, 25 cases of CMV pneumonia were identified during this 5-year period (17 autopsies, 8 OLB). Histological studies were done 10–40 days following ICU admission. Interestingly, no bacteria were identified by lung cultures in 88 % of the cases (n = 22), with CMV being the sole identified pathogen.
Shell-vial cultures (done on BAL, blood and urine samples) were performed prior to histologies in some patients. Their sensitivity was poor, however, and failed to exceed approximately 50 %. This was before the antigenaemia and PCR era.
Concerning the reason for ICU admission, only 6 of the 25 patients were admitted following surgery for a cancer diagnosis. Four patients were admitted following a scheduled cardiac or vascular surgery, and the three remaining surgical patients had an emergent surgery for a peritonitis. Regarding the medical causes for ICU admission, five COPD patients were admitted for acute respiratory failure. A neurological cause was observed in five patients. The remaining two medical patients presented with myocarditis for the first one and with pulmonary embolism for the second one. Interestingly, 19 of these 25 patients received blood products prior to histology. At the time, leucodepletion of blood products was not as efficient as it is today, so primary infection was possible in some cases. Indeed, 5 of the 18 patients tested were IgG negative for CMV. Moreover, the potential immunomodulatory effects of a blood transfusion could have favoured CMV reactivation. This is still a matter of debate and a potential area of investigation.
The clinical pictures of these patients were diverse. Our ICU patients presented a febrile ARDS picture with a degree of hepatic dysfunction in 10 patients, an elevated creatininaemia in 10 patients and mononucleosis in only three patients. Evidence of CMV infection of the retina was never found, and in only one case did a colonic biopsy reveal histologic hallmarks of CMV infection.
We concluded by asking an important question: Is CMV infection of the lung a clinically significant process justifying specific antiviral therapy? Approximately 20 years later, the debate remains open. We will try to depict the main advances regarding the comprehension of the mechanisms and consequences of CMV reactivation in ICU patients for the last 20 years.
Pathophysiology of CMV infection
Because many studies have reported an association between the presence of sepsis and CMV infection [12–15], some investigations have been conducted to elucidate the possible mechanisms of this association. Tumour necrosis factor (TNF) is probably involved in CMV reactivation after sepsis from a bacterial origin [13, 16]. It has been shown that TNF-α is able to directly stimulate immediate early (IE) CMV gene expression [17]. However, no clear relationship has been discovered between the severity scores recorded at admission and the risk of developing CMV infection, nor regarding production of TNF-α plasma levels and the risk of CMV reactivation. Other mechanisms might be involved in CMV reactivation. A certain degree of immune deficiency, for instance, has been reported in critically ill patients early during the ICU stay as a result of the underlying disease and/or the treatment [18, 19]. During this period, one’s immune function against infection may be impaired. Studies of severely immunocompromised patients have suggested that T cell immunity is crucial in the control of CMV replication [20]. In a group of 31 CMV-seropositive non-immunosuppressed surgical and trauma ICU patients, the enumeration of CMV pp65 and immediate-early (IE)-1-specific interferon (IFN)-γ CD8+ and CD4+ T cells was performed by flow cytometry for intracellular cytokine staining [21]. The levels of these cells in peripheral blood have been shown to correlate with protection from active CMV infection. In that study, active CMV infection occurred in 17 out of 31 patients. Undetectable levels of pp65 and IE-1-specific IFN-γ CD8+ and CD4+ T cell subsets were observed in 10 patients who developed active CMV infection and in one who did not (at a median of 2 days following ICU admission). Peak CMV DNA loads in both TA and plasma were substantially higher in patients with undetectable IFN-γ T cell responses than in patients with detectable responses [21]. Taken together, these data suggest that T cell response might be involved in at least some CMV reactivation. However, in another study using different immunological methods, active CMV infection was reported in septic shock patients despite detectable levels of CMV-specific IFN-γ-producing CD4+ T cell precursors in blood, suggesting that CMV reactivation is not primarily triggered by T cell immunosuppression [22]. CMV-specific T cell immunity (CD4+) was also conserved in most critically ill surgical/trauma patients experiencing CMV reactivation [23]. In animal models [24], natural killer (NK) cells may at least partially compensate for the absence of adaptive T cell immunity. There is also some evidence of the crucial role of NK cells in keeping herpesviruses latent in humans [25]. In a recent study done in ICU patients, the function of NK cells was altered regarding INF-γ production just before the occurrence of reactivation [26]. This latter result suggests that in the context of global and major lymphopenia observed in ICU patients, dysfunction in NK cells may be involved in CMV reactivation. It has also been recently shown in non-ICU patients that CMV infections are associated with a redistribution of NK cell subsets in the peripheral blood, with expansion of unconventional “memory” NKG2C+NK cells that exhibit impaired effector functions [27]. CMV is also involved in the impaired function of dendritic cells [28]. All of these factors could explain the increase in nosocomial infections observed in patients presenting with active CMV infection [7, 9]. Regarding the pro-inflammatory properties of CMV, it has been shown in a study of upmost importance [13] that CMV can enhance the progression of post-aggressive lung fibrosis. Indeed, using a mice model of caecal ligation and puncture, Cook et al. showed that CMV reactivation was associated with a dramatic increase in lung fibrosis [13]. In summary (Fig. 1), impaired immune defences encourage CMV replication. CMV might also alter immune defences against infections (favouring the occurrence of nosocomial infections in critically ill patients) and enhance compartmentalized pro-inflammatory responses (exacerbating lung inflammation).
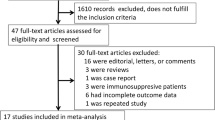
Incidence, diagnosis and risk factors of CMV infection in non-immunocompromised ICU patients
The incidence of CMV infection in non-immunocompromised ICU patients has been assessed in many studies and reviewed in some meta-analyses [29–32]. The incidence is influenced by many factors including the types of patient populations studied and their serologic status on admission, as well as the microbiological tools used to diagnose CMV and the type (blood, TA) and frequencies of sampling. Studies including only seropositive patients have generally shown higher rates of reactivation (Table 1). This is illustrated by a major study involving only seropositive patients who presented with a large variety of critical illnesses such as sepsis, cardiac failure, burns and trauma [32]. These patients were monitored three times a week using quantitative plasma CMV PCR [32]. The authors reported that one-third of the patients presented with a positive viraemia. Twenty per cent of the patients had viraemia greater than 1000 copies/mL. Interestingly, the median time to the first detection of viraemia was 12 days, with a range of 3–57 days [32]. The duration of viraemia was quite long, reaching a median of 17 days (ranging from 2 to 45 days) [32]. Using antigenaemia for the diagnosis, our group reported that the incidence of CMV reactivation was 16.1 % in non-immunocompromised mechanically ventilated ICU patients from a medical ICU [7]. It has been suggested that CMV PCR, when performed on TA, is a more sensitive technique than when performed in blood samples [15]. In this latter study, it was shown that lung reactivation was observed earlier compared with reactivation in the blood (median 14 and 24 days, respectively). Compared with herpes simplex virus (HSV) reactivation, CMV reactivation in respiratory samples exhibits a lower incidence and occurred later in the course of the ICU stay [15]. Co-infections of HSV/CMV have also been reported in as high as 27 % of CMV reactivations in a recent study [29], but there is no information regarding the potential synergistic deleterious impact of this co-infection on outcomes. In a more recent investigation, 49 % of the patients with CMV reactivation also reactivated HHV-6 [33]. The impact on outcome was synergistic between the two viruses. Indeed, the patients with co-reactivation of both HHV-6 and CMV had the greatest risk for death or continued hospitalization by day 30.
The incidence of CMV reactivation is also dependent on the method of diagnosing CMV infection. Three methods have been used: viral cultures, antigenaemia, and PCR. Culture-based techniques (conventional and shell-vial cultures) are considered outmoded because they are time-consuming and lack sensitivity. The antigenaemia assay is a technique based on direct detection of the CMV protein pp65 using monoclonal antibodies. It is sensitive, specific and quantitative. However, this technique is more labour-intensive than the PCR assays, which are now extensively used given their high sensitivity and rapid turnover time. Many diagnostic kits from different manufacturers are commercially available and sometimes PCR is performed by the hospital laboratories. However, a World Health Organization international standard was recently adopted and this allows one to use a conversion factor for expressing the results in international units per millilitre (and not in copies per millilitre). This standardization allows one to adequately compare quantitative PCR when using different diagnostic kits. It is important to underline that no specific threshold for the diagnosis has been identified in either blood or respiratory samples from ICU patients.
Concerning CMV reactivation in ICU patients, there are no specific clinical signs. It is fundamental to highlight that the clinical picture is totally different from CMV infection in HIV patients. The lung is the major organ involved in active CMV infection with end-organ disease. However, there is no radiological specificity as shown in Fig. 2 [34]. Interstitial pneumonia is very uncommon. In some instances, a discrete cholestasis or cytolysis with increased levels of hepatic enzymes are observed. Colitis is rarely observed [35], and only a few cases of retinitis have been reported. Haemophagocytic syndrome can also be associated with CMV infection [36]. In this context, bone marrow examination is useful in establishing the diagnosis.
Lung radiological aspects associated with CMV reactivation. a Interstitial and alveolar infiltrates in an ARDS patient under veno-venous ECMO with a positive PCR (BAL and blood). b Predominantly left lung infiltrates in a patient with histological signs of CMV pneumonia. c Pleural effusion, alveolar condensation and ground-glass opacifications of the right upper lobe in a patient with a positive PCR (BAL and blood). d Bilateral pleural effusion without lung infiltrates in a patient with a positive PCR (BAL and blood). There was no clinical sign of active CMV infection
It is truly difficult to identify associated risk factors for developing CMV reactivation other than admission to an ICU and mechanical ventilation. Active CMV infections have been reported in medical and surgical patients as well as trauma patients. Age is not recognized as a risk factor, and any evidence of an association between CMV infection and gender has been inconsistent [37]. Sepsis, blood transfusions, corticosteroids and ARDS have also been found to be associated with the risk of CMV reactivation [7, 37]. Interestingly, severity scores on ICU admission or on inclusion are generally not recognized as being associated with the occurrence of CMV reactivation except in a meta-analysis of 13 studies [7, 15, 30, 32]. This lack of association between severity scores on ICU admission and CMV reactivation suggests that factors other than severity of the underlying disease and the number and extent of organ dysfunctions are major risk factors. More studies are needed to identify factors that could predict the risk of developing a CMV reactivation. Immunologic predisposition could be responsible for CMV reactivation and warrants further study in particular.
Impact of CMV infection on the outcome of ICU patients
The impact of CMV infection is a matter of continuing debate. Indeed, there has been no clear demonstration of a definite relationship between the development of CMV infection and deleterious consequences regarding morbidity (duration of mechanical ventilation, duration of ICU or hospital stay) and/or mortality. For many intensivists, CMV reactivation is one of the hallmarks of the severity of an underlying disease i.e. it represents more of a symptom than an illness per se. For other intensivists, CMV is thought to be directly responsible for organ disease such as pneumonia [4, 5, 34] and colitis [35]. However, by modulating immune function and anti-inflammatory response, CMV might be responsible for the occurrence of bacterial superinfection and/or the aggravation of inflammatory processes such as ARDS. Epidemiological studies have generally documented a strong association between the occurrence of CMV reactivation and a prolonged duration of mechanical ventilation. In a matched cohort study [9], 40 antigenaemia-positive patients were matched to 40 controls. Patients with CMV had a significantly longer duration of mechanical ventilation (35 ± 27 days vs. 24 ± 20 days, respectively; p < 0.03) and a longer ICU stay. Interestingly, there was also a higher rate of nosocomial infections in the CMV group [9]. This important study alerted us regarding the deleterious impact of CMV infection on outcomes [9]. CMV infection might be directly responsible for an increased duration of mechanical ventilation (lung infection), which is a risk factor for the development of nosocomial infections. In addition, CMV infection might alter immune function, which would also increase the risk for acquiring nosocomial infections. However, these two mechanisms might be associated. In a series of 120 patients from medical, trauma, burn, cardiac and surgical ICUs, CMV viraemia assessed by PCR was independently associated with hospitalization or death by day 30 [32]. Furthermore, in 242 mechanically ventilated medical ICU patients [7], active CMV infection was associated with an increased duration of mechanical ventilation in survivors presenting with an active CMV infection (median 27 days) relative to controls (median 10 days). The number of ventilator-free days and alive by day 60 was also dramatically reduced when patients developed a CMV infection (median 0 days compared with 34 days for the controls) [7]. It was also reported that the rate of nosocomial infections was higher in the CMV group [7], and the difference remained even when ventilator-associated pneumonia and bacteraemia were considered separately [7]. In contrast, two recent epidemiological studies [38, 39] found no association between serological status regarding CMV and outcomes in a non-selected ICU population or in all-cause ARDS patients. However, in a particular subgroup of ARDS patients presenting with septic shock, results showed an association between the CMV serological status and the number of ventilator-free days to day 28 [39]. Other epidemiological studies and some meta-analyses have looked more specifically at the effects of CMV infection on mortality. In particular, three recent meta-analyses have suggested that there is a strong relationship between the presence of an active CMV infection and mortality, with an odds ratio of approximately 2 [29–31]. In a matched cohort study [9], in which patients were matched on age, gender, SAPS II score and reason for admission, the authors reported that ICU mortality was substantially higher in patients presenting with positive antigenaemia (50 %) compared with controls (28 %, p < 0.02). Mortality at day 60 was also higher in patients with a positive PCR in non-immunocompromised ICU patients (55 % vs. 20 %, p = 0.01) [29]. In another series of 86 patients who presented with severe sepsis, although reporting a longer duration of ICU and hospital stays and a prolonged duration of mechanical ventilation when active CMV infection was diagnosed, the authors [15] did not report any increase in mortality related to CMV.
Current situation regarding the pathogenicity of CMV
At the present time, there is no definitive proof of CMV pathogenicity. Arguments suggesting that CMV is pathogenic have come from epidemiological studies and from reports on specific subsets of ICU patients such as ARDS patients who exhibited histological and immunological hallmarks of CMV pneumonia or colitis. Twenty years later, we are still waiting for randomised controlled trials designed to test whether specific antiviral therapies can decrease morbidity and/or mortality. To the best our knowledge, three prospective studies are ongoing that are evaluating a prophylactic or pre-emptive treatment with ganciclovir/valganciclovir/acyclovir. However, only one of these randomised controlled trials aims to evaluate the effectiveness of an antiviral therapy in improving outcomes. Indeed, the main objective of the PTH study (Pre-emptive Treatment for Herpesviridae) is to show that ganciclovir can increase the number of days alive and free of mechanical ventilation to day 60 in patients presenting a reactivation evaluated by blood CMV PCR (NCT02152358). Only non-immunocompromised patients receiving at least 96 h of mechanical ventilation are included. In the CCCC study (Cytomegalovirus Control in Critical Care), seropositive patients receiving at least 24 h of mechanical ventilation are included (NCT01503918). Time-to-reactivation of CMV is the main object of analysis. In the GRAIL study (Study of Ganciclovir/Valganciclovir for Prevention of Cytomegalovirus Reactivation in Acute Injury of the Lung and Respiratory Failure), CMV-seropositive ALI/ARDS patients with severe sepsis or trauma (NCT01335932) are included. The main objective is to study the course of interleukin-6. However, even if the interventional studies show negative results, an etiologic role of CMV is not excluded. Indeed, observed clinical study end points will be influenced by both the effectiveness of the antiviral drug to prevent or to treat CMV reactivation as well as by any negative side effects caused by the antiviral drugs. Furthermore, especially in the trials testing prophylactic treatment, about 60–80 % of the patients will be unnecessarily exposed to antiviral treatment, as CMV does not reactivate in the majority of patients even without receiving prophylaxis. The likelihood of a successful prophylactic approach will largely depend on the ability to improve the selection of patients who are going to reactivate CMV during their ICU stay.
Finally, as only one ongoing randomised controlled trial (PTH) evaluates if CMV treatment is able to improve the outcome, there is the need for additional interventional trials designed to assess if CMV is pathogenic for ICU patients. While waiting for the results of these studies, a screening of CMV reactivation using repeated PCR should focus on mechanically ventilated patients seropositive for CMV on admission. Additional studies are also needed to identify which specific ICU patients have the highest risk for developing active CMV infections.
If the results of the ongoing and future studies suggest that CMV is pathogenic, future trials should investigate the mechanisms causing CMV pathogenicity (direct, indirect or both) and the predisposing immunologic conditions associated with the development of a CMV reactivation. Indeed, one can easily imagine that immune-active drugs could be effective in decreasing the incidence of reactivation and/or the immune system alterations related to CMV reactivation.
To treat or not to treat?
Pending the results of the ongoing and future trials, we recommend the use of a curative antiviral treatment (principally ganciclovir) when there is a CMV reactivation (positive antigenaemia and/or PCR) associated with clinical signs of infection (primarily lung infiltrates) and the presence of risk factors (Fig. 3). Pre-emptive treatment (CMV reactivation without clinical signs of infection) could be discussed in certain circumstances following an assessment of the risk–benefit balance (patients with impaired host defences) [40]. In this context, unless viral load is very high (greater than 10,000 copies/mL), trends in viral load may be more useful than a given value.
There are few antiviral drugs currently available for use against CMV. All of these therapies are associated with side effects, which can worsen the outcomes for ICU patients. The toxicities of ganciclovir, foscarnet and cidofovir are well known. Ganciclovir’s toxicity is mainly related to its haematological side effects (mainly neutropenia, thrombocytopenia and sometimes anaemia). The toxicity of foscarnet is essentially renal. Some disturbances to electrolytes have also been observed in patients receiving foscarnet (regular monitoring of calcium, magnesium, phosphate and potassium is required). Nephrotoxicity is also a significant side effect when using cidofovir. Ganciclovir so far appears to be the least toxic and is currently the leading choice among these agents. The oral formulation of valganciclovir precludes its early use during critical illness when many patients have ileus and unreliable intestinal absorption. By targeting the DNA polymerase, all of these drugs can cause the emergence of drug-resistant strains.
Conclusions
Active CMV infection is observed in 15–20 % of ICU patients (20–40 % in ICU patients with positive CMV serology). Although observed in epidemiological studies, there is no definite proof that CMV worsens the outcome of mechanically ventilated patients. Prospective randomized trials are needed to elucidate this point further.
References
Chiche L, Forel JM, Papazian L (2011) The role of viruses in nosocomial pneumonia. Curr Opin Infect Dis 24:152–156
Gkrania-Klotsas E, Langenberg C, Sharp SJ, Luben R, Khaw KT, Wareham NJ (2012) Higher immunoglobulin G antibody levels against cytomegalovirus are associated with incident ischemic heart disease in the population-based EPIC-Norfolk cohort. J Infect Dis 206:1897–1903
Barry SM, Johnson MA, Janossy G (2000) Cytopathology or immunopathology? The puzzle of cytomegalovirus pneumonitis revisited. Bone Marrow Transplant 26:591–597
Papazian L, Fraisse A, Garbe L, Zandotti C, Thomas P, Saux P, Pierrin G, Gouin F (1996) Cytomegalovirus. An unexpected cause of ventilator-associated pneumonia. Anesthesiology 84:280–287
Papazian L, Thomas P, Bregeon F, Garbe L, Zandotti C, Saux P, Gaillat F, Drancourt M, Auffray JP, Gouin F (1998) Open-lung biopsy in patients with acute respiratory distress syndrome. Anesthesiology 88:935–944
Grundy JE, Shanley JD, Griffiths PD (1987) Is cytomegalovirus interstitial pneumonitis in transplant recipients an immunopathological condition? Lancet 2:996–999
Chiche L, Forel JM, Roch A, Guervilly C, Pauly V, Allardet-Servent J, Gainnier M, Zandotti C, Papazian L (2009) Active cytomegalovirus infection is common in mechanically ventilated medical intensive care unit patients. Crit Care Med 37:1850–1857
Cook CH, Martin LC, Yenchar JK, Lahm MC, McGuinness B, Davies EA, Ferguson RM (2003) Occult herpes family viral infections are endemic in critically ill surgical patients. Crit Care Med 31:1923–1929
Jaber S, Chanques G, Borry J, Souche B, Verdier R, Perrigault PF, Eledjam JJ (2005) Cytomegalovirus infection in critically ill patients: associated factors and consequences. Chest 127:233–241
Walton AH, Muenzer JT, Rasche D, Boomer JS, Sato B, Brownstein BH, Pachot A, Brooks TL, Deych E, Shannon WD, Green JM, Storch GA, Hotchkiss RS (2014) Reactivation of multiple viruses in patients with sepsis. PLoS One 9:e98819
Papazian L, Thomas P, Garbe L, Guignon I, Thirion X, Charrel J, Bollet C, Fuentes P, Gouin F (1995) Bronchoscopic or blind sampling techniques for the diagnosis of ventilator-associated pneumonia. Am J Respir Crit Care Med 152:1982–1991
Brenner T, Rosenhagen C, Hornig I, Schmidt K, Lichtenstern C, Mieth M, Bruckner T, Martin E, Schnitzler P, Hofer S, Weigand MA (2012) Viral infections in septic shock (VISS-trial)-crosslinks between inflammation and immunosuppression. J Surg Res 176:571–582
Cook CH, Trgovcich J, Zimmerman PD, Zhang Y, Sedmak DD (2006) Lipopolysaccharide, tumor necrosis factor alpha, or interleukin-1beta triggers reactivation of latent cytomegalovirus in immunocompetent mice. J Virol 80:9151–9158
Florescu DF, Kalil AC (2011) Cytomegalovirus infections in non-immunocompromised and immunocompromised patients in the intensive care unit. Infect Disord Drug Targets 11:354–364
Heininger A, Haeberle H, Fischer I, Beck R, Riessen R, Rohde F, Meisner C, Jahn G, Koenigsrainer A, Unertl K, Hamprecht K (2011) Cytomegalovirus reactivation and associated outcome of critically ill patients with severe sepsis. Crit Care 15:R77
Docke WD, Prosch S, Fietze E, Kimel V, Zuckermann H, Klug C, Syrbe U, Kruger DH, von Baehr R, Volk HD (1994) Cytomegalovirus reactivation and tumour necrosis factor. Lancet 343:268–269
Hummel M, Abecassis MM (2002) A model for reactivation of CMV from latency. J Clin Virol 25(Suppl 2):S123–S136
Hotchkiss RS, Coopersmith CM, McDunn JE, Ferguson TA (2009) The sepsis seesaw: tilting toward immunosuppression. Nat Med 15:496–497
Hotchkiss RS, Monneret G, Payen D (2013) Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol 13:862–874
Boeckh M, Murphy WJ, Peggs KS (2015) Recent advances in cytomegalovirus: an update on pharmacologic and cellular therapies. Biol Blood Marrow Transplant 21:24–29
Clari MA, Aguilar G, Benet I, Belda J, Gimenez E, Bravo D, Carbonell JA, Henao L, Navarro D (2013) Evaluation of cytomegalovirus (CMV)-specific T-cell immunity for the assessment of the risk of active CMV infection in non-immunosuppressed surgical and trauma intensive care unit patients. J Med Virol 85:1802–1810
Chilet M, Aguilar G, Benet I, Belda J, Tormo N, Carbonell JA, Clari MA, Costa E, Navarro D (2010) Virological and immunological features of active cytomegalovirus infection in nonimmunosuppressed patients in a surgical and trauma intensive care unit. J Med Virol 82:1384–1391
von Muller L, Klemm A, Durmus N, Weiss M, Suger-Wiedeck H, Schneider M, Hampl W, Mertens T (2007) Cellular immunity and active human cytomegalovirus infection in patients with septic shock. J Infect Dis 196:1288–1295
Arase H, Mocarski ES, Campbell AE, Hill AB, Lanier LL (2002) Direct recognition of cytomegalovirus by activating and inhibitory NK cell receptors. Science 296:1323–1326
Biron CA, Byron KS, Sullivan JL (1989) Severe herpesvirus infections in an adolescent without natural killer cells. N Engl J Med 320:1731–1735
Chiche L, Forel JM, Thomas G, Farnarier C, Cognet C, Guervilly C, Zandotti C, Vely F, Roch A, Vivier E, Papazian L (2012) Interferon-gamma production by natural killer cells and cytomegalovirus in critically ill patients. Crit Care Med 40:3162–3169
Min-Oo G, Lanier LL (2014) Cytomegalovirus generates long-lived antigen-specific NK cells with diminished bystander activation to heterologous infection. J Exp Med 211:2669–2680
Avdic S, McSharry BP, Slobedman B (2014) Modulation of dendritic cell functions by viral IL-10 encoded by human cytomegalovirus. Front Microbiol 5:337
Coisel Y, Bousbia S, Forel JM, Hraiech S, Lascola B, Roch A, Zandotti C, Million M, Jaber S, Raoult D, Papazian L (2012) Cytomegalovirus and herpes simplex virus effect on the prognosis of mechanically ventilated patients suspected to have ventilator-associated pneumonia. PLoS One 7:e51340
Kalil AC, Florescu DF (2009) Prevalence and mortality associated with cytomegalovirus infection in nonimmunosuppressed patients in the intensive care unit. Crit Care Med 37:2350–2358
Kalil AC, Florescu DF (2011) Is cytomegalovirus reactivation increasing the mortality of patients with severe sepsis? Crit Care 15:138
Limaye AP, Kirby KA, Rubenfeld GD, Leisenring WM, Bulger EM, Neff MJ, Gibran NS, Huang ML, Santo Hayes TK, Corey L, Boeckh M (2008) Cytomegalovirus reactivation in critically ill immunocompetent patients. JAMA 300:413–422
Lopez Roa P, Hill JA, Kirby KA, Leisenring WM, Huang ML, Santo TK, Jerome KR, Boeckh M, Limaye AP (2015) Coreactivation of human herpesvirus 6 and cytomegalovirus is associated with worse clinical outcome in critically ill adults. Crit Care Med 43:1415–1422
Papazian L, Doddoli C, Chetaille B, Gernez Y, Thirion X, Roch A, Donati Y, Bonnety M, Zandotti C, Thomas P (2007) A contributive result of open-lung biopsy improves survival in acute respiratory distress syndrome patients. Crit Care Med 35:755–762
Siciliano RF, Castelli JB, Randi BA, Vieira RD, Strabelli TM (2014) Cytomegalovirus colitis in immunocompetent critically ill patients. Int J Infect Dis 20:71–73
Fisman DN (2000) Hemophagocytic syndromes and infection. Emerg Infect Dis 6:601–608
Osawa R, Singh N (2009) Cytomegalovirus infection in critically ill patients: a systematic review. Crit Care 13:R68
De Vlieger G, Meersseman W, Lagrou K, Wouters P, Wilmer A, Peetermans WE, Van den Berghe G, Van Wijngaerden E (2012) Cytomegalovirus serostatus and outcome in nonimmunocompromised critically ill patients. Crit Care Med 40:36–42
Ong DS, Klein Klouwenberg PM, Verduyn Lunel FM, Spitoni C, Frencken JF, Dekker HA, Schultz MJ, Bonten MJ, Cremer OL (2015) Cytomegalovirus seroprevalence as a risk factor for poor outcome in acute respiratory distress syndrome. Crit Care Med 43:394–400
Forel JM, Martin-Loeches I, Luyt CE (2014) Treating HSV and CMV reactivations in critically ill patients who are not immunocompromised: pro. Intensive Care Med 40:1945–1949
Domart Y, Trouillet JL, Fagon JY, Chastre J, Brun-Vezinet F, Gibert C (1990) Incidence and morbidity of cytomegaloviral infection in patients with mediastinitis following cardiac surgery. Chest 97:18–22
Stephan F, Meharzi D, Ricci S, Fajac A, Clergue F, Bernaudin JF (1996) Evaluation by polymerase chain reaction of cytomegalovirus reactivation in intensive care patients under mechanical ventilation. Intensive Care Med 22:1244–1249
Kutza AS, Muhl E, Hackstein H, Kirchner H, Bein G (1998) High incidence of active cytomegalovirus infection among septic patients. Clin Infect Dis 26:1076–1082
Cook CH, Yenchar JK, Kraner TO, Davies EA, Ferguson RM (1998) Occult herpes family viruses may increase mortality in critically ill surgical patients. Am J Surg 176:357–360
Heininger A, Jahn G, Engel C, Notheisen T, Unertl K, Hamprecht K (2001) Human cytomegalovirus infections in nonimmunosuppressed critically ill patients. Crit Care Med 29:541–547
Desachy A, Ranger-Rogez S, Francois B, Venot C, Traccard I, Gastinne H, Denis F, Vignon P (2001) Reactivation of human herpesvirus type 6 in multiple organ failure syndrome. Clin Infect Dis 32:197–203
Razonable RR, Fanning C, Brown RA, Espy MJ, Rivero A, Wilson J, Kremers W, Smith TF, Paya CV (2002) Selective reactivation of human herpesvirus 6 variant a occurs in critically ill immunocompetent hosts. J Infect Dis 185:110–113
von Muller L, Klemm A, Weiss M, Schneider M, Suger-Wiedeck H, Durmus N, Hampl W, Mertens T (2006) Active cytomegalovirus infection in patients with septic shock. Emerg Infect Dis 12:1517–1522
Ziemann M, Sedemund-Adib B, Reiland P, Schmucker P, Hennig H (2008) Increased mortality in long-term intensive care patients with active cytomegalovirus infection. Crit Care Med 36:3145–3150
Bordes J, Gaillard T, Maslin J, Esnault P, Goutorbe P, Brisou P (2011) Cytomegalovirus infection monitored by quantitative real-time PCR in critically ill patients. Crit Care 15:412
Frantzeskaki FG, Karampi ES, Kottaridi C, Alepaki M, Routsi C, Tzanela M, Vassiliadi DA, Douka E, Tsaousi S, Gennimata V, Ilias I, Nikitas N, Armaganidis A, Karakitsos P, Papaevangelou V, Dimopoulou I (2015) Cytomegalovirus reactivation in a general, nonimmunosuppressed intensive care unit population: incidence, risk factors, associations with organ dysfunction, and inflammatory biomarkers. J Crit Care 30:276–281
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Financial support
No financial support.
Rights and permissions
About this article
Cite this article
Papazian, L., Hraiech, S., Lehingue, S. et al. Cytomegalovirus reactivation in ICU patients. Intensive Care Med 42, 28–37 (2016). https://doi.org/10.1007/s00134-015-4066-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4066-9