Abstract
Background
Antimicrobial drug resistance is one of the top ten threats to global health according to the World Health Organization. Urinary tract infections (UTIs) are among the most common bacterial infections and main reason for antibiotic prescription. The incidence of UTIs appears to be high among people living with HIV. We sought to determine the most common UTI pathogens among HIV infected patients and evaluate their susceptibility towards antibiotics.
Methods
We performed a cross-sectional study among HIV-infected patients aged ≥ 18 years presenting at an HIV care specialized clinic with symptoms suggestive of a urethritis. Urine cultures were subjected to antibiotic susceptibility testing according to Clinical Laboratory Standards Institute. The data was analyzed using STATA, we performed Pearson’s Chi-square and Fisher’s exact tests to compare differences between proportions.
Results
Out of the 200 patients, 123 (62%) were female. The median age was 41.9 years (IQR 34.7–49.3). Only 32 (16%) urine cultures showed bacterial growth. Escherichia coli was the most commonly isolated uropathogen (72%), followed by Klebsiella pneumoniae (9%). E. coli was completely resistant to cotrimoxazole and ampicillin; resistance to ciprofloxacin and ceftriaxone was 44% and 35% respectively; 9% to gentamicin; no resistance detected to nitrofurantoin and imipenem.
Conclusions
Our findings are congruent with the Uganda national clinical guidelines which recommends nitrofurantoin as the first line antibiotic for uncomplicated UTI. Significant ciprofloxacin and ceftriaxone resistance was detected. In the era of emerging antibiotic resistance, understanding the local susceptibilities among sub-populations such as HIV infected patients is crucial. Further investigation is needed to address reasons for the low bacterial growth rate observed in the urine cultures.
Similar content being viewed by others
Background
Urinary tract infections (UTIs) are one of the most common bacterial infections globally, with an estimated annual incidence of more than 150 million cases worldwide [1]. UTIs are one of the main reasons for the prescription of antibiotics [2, 3]. They are caused by a variety of uropathogens, most commonly gastrointestinal bacterial flora such as uropathogenic Escherichia coli, Klebsiella pneumoniae, various other Enterobacteriaceae, as well as Staphylococcus saprophyticus [4]. In recent years, studies have shown rising drug resistance patterns in these uropathogens across the globe [5, 6]. World Health Organization (WHO) surveillance data on antimicrobial resistance reveal high levels of resistance to a number of bacterial infections in both high and low-income countries [7]. Furthermore, antimicrobial resistance (AMR) was identified as one of the top ten threats to global health in 2019 that will require focus from health care providers and implementers [8].
Sub-Saharan Africa (SSA), a region with a high burden of infectious diseases, is especially vulnerable to antimicrobial resistance [9]. In South Africa, a study reported suboptimal adherence to national antibiotic prescription guidelines due to a number of factors [10]. These included undocumented diagnosis, unnecessary antibiotic prescription, incorrect dosage, incorrect drug and incorrect duration of therapy [10]. Studies conducted in Uganda revealed that up to 41% of antibiotics were issued over the counter and high antibiotic prescription rates among hospitalized patients with frequently missed doses [11, 12]. Antimicrobial resistance in UTIs to cotrimoxazole, ciprofloxacin, cephalosporins and other antibiotics have been reported in SSA, however the data is limited [13,14,15].
Generally, the incidence of UTIs appears to be high among people living with HIV, especially in those with lower CD4 lymphocyte count [16]. HIV-infected individuals with low CD4 lymphocyte count are often receiving prophylactic cotrimoxazole to prevent opportunistic infections, such as pneumocystis jirovecii pneumonia (PCP) [17]. Cotrimoxazole prophylaxis is not effective in reduction of the incidence of UTIs among HIV-infected individuals with lower CD4 lymphocyte count [16]. In Uganda, the national clinical guidelines for the treatment of UTI were revised, and cotrimoxazole was replaced with nitrofurantoin as a first-line agent for UTIs due to high resistance rates [18, 19].
This study was conducted through the Infectious Diseases Institute (IDI), Makerere University, Uganda and University of Zurich (UZH), Switzerland research collaboration. The study describes findings of a UTI surveillance project implemented in an out-patient HIV clinic of the IDI of the Makerere University College of Health Sciences in Kampala, Uganda. We sought to determine the most common UTI pathogens in the HIV-positive population and evaluate their susceptibility towards commonly prescribed antibiotic agents.
Methods
Study site
The study was conducted between September 2017 and December 2018 in an out-patient HIV clinic at IDI in Kampala, Uganda. It is an urban center of excellence for HIV care and treatment, with over 8000 patients.
Study design and patients
We performed a cross-sectional study among HIV-infected patients aged ≥ 18 years presenting with symptoms suggestive of urethritis. This was defined as showing one or more of the following symptoms; dysuria, urgency, frequency and fever. The patient data was collected as part of routine surveillance at the out-patient HIV-Clinic for a period of 16 months.
Urine sample collection
Patients were instructed on how to provide an adequate midstream urine sample (MSU) by a nurse with the help of a leaflet with visual step-by-step instructions of the procedure. The MSU was then taken to the laboratory at the Department of Medical Microbiology, Makerere University School of Biomedical Sciences within 2 h or within 24 h if refrigerated at 4 °C.
Laboratory procedures
The MSU was subjected to urine dipstick and urine cultures were subjected to antibiotic susceptibility testing according to Clinical Laboratory Standards Institute (CLSI). Sheep Blood and Cystine Lactose Electrolyte Deficient (CLED) agar were used for urinary culture. Cultures were incubated at 35–37 °C and checked for growth after 18–24 h. Agar plates with pure growth > 104 colony forming units (CFU)/ml, or > 105 CFU/ml if two types of pathogens were present, were classified as showing significant growth and used for further identification and sensitivity testing using Müller-Hinton Agar. Plates with no visible colonies were reported as no bacterial growth. Growth results ≥ 102 CFU/ml, but below the threshold for significant growth were reported as insignificant growth. Cultures with more than two types of organisms were reported as mixed growth, suggesting contamination. Drug susceptibility testing (DST) was performed for the following antimicrobial agents, as per the laboratory SOP: ciprofloxacin, cotrimoxazole, nitrofurantoin, ampicillin, ceftazidime, cefuroxime, ceftriaxone, chloramphenicol, gentamicin, imipenem, and nalidixic acid. Sensitivity was evaluated with the Kirby-Bauer disc diffusion method. More details on microbiology are provided in the Additional file 1: Appendix S1.
Patient follow up
In case the cultured uropathogen showed resistance towards the empirically prescribed antibiotic regimen, patients were contacted and asked to report to the clinic. Therapy was then adjusted by the assigned follow-up physician according to the resistance test results.
Data collection
Demographic and clinical characteristics, UTI related information including urine test results was collected using Epidata®. UTI-symptoms and further information about the patients’ medical history were obtained using a standard evaluation form that was filled out by the patients with the support of a nurse.
Statistical analysis
The data was analyzed using STATA version 14.2 (College Station, Texas 77845 USA). Statistics for proportions, means with standard deviations (SD) and medians with interquartile ranges (IQR) were acquired to describe the data. We performed Pearson’s Chi-square and Fisher’s exact tests to compare differences between proportions.
Results
A total of 200 HIV infected patients presenting with symptoms suggestive of UTI were recruited and included in the study. Of these, 123 (61.5%) were female. The median age was 41.9 years (IQR 34.7–49.3); 40.1 years (IQR 33.8–48.7) for females and 43.9 years (IQR 36.7–50.9) for males. The majority of patients presented with dysuria (158, 79.0%). Nearly all the patients (198, 99.0%) reported to be taking cotrimoxazole or dapsone prophylaxis, which was recommended by the Uganda HIV treatment guidelines at the time of the study. The median duration on cotrimoxazole or dapsone prophylaxis in months was 110 (IQR 64–142). 83 (41.2%) patients reported using other antibiotics within the past month, of these 59 (29.5%) were taking antibiotics at the time of recruitment. Almost all the patients, 195 (97.5%) were on antiretroviral treatment (ART) and the median duration on ART in months was 103 (IQR 60–144). Majority of them, 195 (97.5%) had had a viral load test within the past 12 months; of these 175 (87.5%) were undetectable (< 75 copies/ml). Comprehensive details on the baseline characteristics of patients recruited in the study are presented in Table 1.
Out of 200 cultures, only 32 (16.0%) showed bacterial growth. 36 (18.0%) cultures showed mixed bacterial growth, and 132 (66.0%) cultures had no bacterial growth. Escherichia coli was the most commonly isolated uropathogen (71.9%), followed by Klebsiella pneumoniae (9.4%) and Morganella morganii (6.3%). Other isolates included Acinetobacter baumannii, Enterobacter spp, Citrobacter freundii, Providencia spp., Enterococcus spp. and Group B Salmonella.
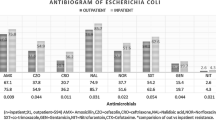
Escherichia coli was completely resistance to ampicillin and cotrimoxazole. Resistance to ciprofloxacin and ceftriaxone was 44.4 and 35.0% respectively; to gentamicin was 9.1%, no resistance was observed to nitrofurantoin and imipenem. Klebsiella pneumoniae was cultured in three cases, all were resistant to cotrimoxazole and ampicillin. One out of two isolates was resistant to ciprofloxacin; one out of three to ceftriaxone, gentamicin and nitrofurantoin; none was resistant to imipenem. Table 2 shows a summary of the resistance profile of the isolated pathogens towards the tested antibiotics.
Table 3 compares culture growth, isolated pathogens and antibiotic resistance with and without recent use of other antibiotics in the past month (with exception of those on cotrimoxazole/dapsone prophylaxis). The antibiotics taken in the month prior to the study or being taken at the time of the study included doxycycline, metronidazole, amoxicillin, cefuroxime, ampicillin, azithromycin, gentamicin, ceftriaxone and chloramphenicol. No statistically significant difference was observed in cultural growth, pathogen distribution and antibiotic resistance between groups of the two groups of patients.
Discussion
This surveillance study describes urinary tract pathogens and their resistance patterns among Ugandan patients living with HIV who presented with symptoms suggestive of a UTI. The most commonly isolated pathogen in our study was Escherichia coli (71.8%). This finding is congruent with other studies conducted in Uganda, Sub-Saharan African countries and other parts of the world. In Uganda, two studies found Escherichia coli to be the responsible pathogen in 57.5% and 50% of culturally confirmed UTI respectively [14, 20]. A study in Ethiopia, reported Escherichia coli in 52.7% of urine cultures [21]. In Europe and North America, Escherichia coli is estimated to be responsible for 60–70% of UTIs [22, 23]. However, there is limited antimicrobial surveillance data for UTI among HIV infected patients in Uganda. Hence a comparison of the resistance profiles of pathogens with other studies conducted locally was not possible.
E. coli, the most isolated uropathogen was completely resistant to ampicillin and cotrimoxazole, as well as significantly resistant to ciprofloxacin and ceftriaxone. Susceptibility was high to nitrofurantoin, imipenem and gentamicin. In Uganda, high resistance in uropathogens to cotrimoxazole, amoxicillin, and nalidixic acid and considerable resistance towards ciprofloxacin has been observed [17]. This resistance pattern is similar to findings in other SSA countries [18]. Another Ugandan study describes high sensitivity towards nitrofurantoin, with similarly low sensitivity towards ciprofloxacin and cotrimoxazole [14]. High resistance towards cotrimoxazole has been described in other studies conducted in Sub-Saharan African countries and could be attributed to the use of cotrimoxazole as prophylaxis against opportunistic infections in HIV-positive patients [14, 17, 24]. It is noteworthy that ampicillin and other beta-lactam antibiotics are widely dispensed over the counter in Uganda without the need of a physician’s prescription [11]. This fact could provide an alternative explanation to the high resistance rates observed. In other patient scenarios, the recommended duration of the antibiotic treatment is cut short due to financial constraints [11, 25]. A study in Uganda reported ciprofloxacin and ceftriaxone as commonly prescribed systemic antibiotics in hospitalized patients [12]. The same study reported that under-administration of prescribed antibiotics was frequent and therefore a concern for loss of efficacy and emergence of antibiotic resistance. In the current Ugandan clinical guidelines, ciprofloxacin is recommended as second line therapy in UTIs [22]. However, this study has demonstrated that ciprofloxacin has been ineffective in inhibiting bacterial growth in vitro. High efficacy of nitrofurantoin and gentamicin has been described in Sub-Saharan African countries [14, 18, 20]. Nitrofurantoin is recommended as the first line agent for uncomplicated UTIs by the Ugandan clinical guidelines and the study results concur with this recommendation [22]. Since gentamicin and imipenem are administered intravenously and are considered as antibiotics reserved for difficult to treat situations, this may limit their dispensation over the counter and overall availability and may provide an explanation of their low resistance rates.
Out of 200 patients, only 32 (16%) cultures had significant bacterial growth. Other studies in Sub-Saharan African countries showed similarly low rates of culture growth [14, 17, 20, 26]. In comparison, studies conducted in other settings such as Europe showed high growth rates of around 80% [27, 28]. Possible explanations for the low growth rate might be found in the high percentage of patients with recent antibiotic consumption (41.5%) and the use of cotrimoxazole or dapsone prophylaxis in almost all patients (99.0%). The consumed antibiotic agents may inhibit in vitro culture growth of bacteria in urine. Other studies have shown such an inhibiting impact of antibiotic intake on urine culture growth [29]. As both groups in this analysis were taking cotrimoxazole/dapsone prophylaxis, additional antibiotic intake may not significantly further alter positive culture growth. Another potential reason for the low rate of bacterial growth on culture might be that some of the patients’ symptoms were not attributed to a UTI. Alternative causes of the described symptoms may be found in sexually transmitted diseases (STI) such as chlamydia or gonococcal urethritis which cannot be diagnosed by standard urine cultures.
The limitations of this study are we included only HIV-infected patients presenting with symptoms suggestive of urethritis. Furthermore, we did not have recent CD4 count results of the patients because CD4 is no longer routinely measured and replaced by viral load count for monitoring purposes of HIV patients. Lastly, we did not collect data on previous hospitalizations of the patients.
Conclusion
Our study found the most isolated pathogen, E. Coli to be completely resistant to cotrimoxazole and ampicillin. Furthermore, significant resistance to ciprofloxacin and ceftriaxone was observed. Susceptibility was high to gentamicin, nitrofurantoin and imipenem. It is noteworthy that majority of urine cultures showed no bacterial growth in symptomatic patients. This is a concern and further studies are needed to address potential reasons behind the observed low growth rate. Finally, in the era of emerging antibiotic resistance, understanding the epidemiology and the local susceptibilities among sub-populations such as HIV infected individuals is crucial. This study is aligned with the WHO global action plan on antimicrobial resistance and provides further information that will contribute to the database on antimicrobial resistance in UTI in Uganda.
Availability of data and materials
All data generated during this study are included in this article. Details of the full data may be accessed through the Corresponding Author, George Abongomera, Department of Public and Global Health, Epidemiology, Biostatistics and Prevention Institute, University of Zurich, Hirschengraben 84, CH 8001 Zurich, Switzerland, Phone: + 41 44 634 49 36, Email: george.abongomera@uzh.ch.
Abbreviations
- AMR:
-
Antimicrobial resistance
- ART:
-
Antiretroviral therapy
- CLED:
-
Cystine Lactose Electrolyte Deficient
- CLSI:
-
Clinical Laboratory Standards Institute
- DST:
-
Drug susceptibility testing
- IDI:
-
Infectious Diseases Institute
- IQR:
-
Interquartile range
- MSU:
-
Midstream urine
- PCP:
-
Pneumocystis jirovecii Pneumonia
- SD:
-
Standard deviations
- SSA:
-
Sub-Saharan Africa
- UTIs:
-
Urinary tract infections
- UZH:
-
University of Zurich
- WHO:
-
World Health Organization
References
Öztürk R, Murt A. Epidemiology of urological infections: a global burden. World J Urol. 2020;38:2669–79.
Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388:1545–602.
Low M, Almog R, Balicer RD, Liberman N, Raz R, Peretz A, et al. Infectious disease burden and antibiotic prescribing in primary care in Israel. Ann Clin Microbiol Antimicrob. 2018;17:26.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13:269–84.
Tandogdu Z, Wagenlehner FM. Global epidemiology of urinary tract infections. Curr Opin Infect Dis. 2016;29:73–9.
Fasugba O, Gardner A, Mitchell BG, Mnatzaganian G. Ciprofloxacin resistance in community- and hospital-acquired Escherichia coli urinary tract infections: a systematic review and meta-analysis of observational studies. BMC Infect Dis. 2015;15:545.
WHO.int. Fact Sheet Antimicrobial Resistance. http://www.who.int/en/news-room/fact-sheets/detail/antimicrobial-resistance. Accessed 12 Nov 2020.
WHO.int. Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. Accessed 12 Nov 2020.
Kariuki S, Dougan G. Antibacterial resistance in sub-Saharan Africa: an underestimated emergency. Ann N Y Acad Sci. 2014;1323:43–55.
Gasson J, Blockman M, Willems B. Antibiotic prescribing practice and adherence to guidelines in primary care in the Cape Town Metro District South Africa. South Afr Med J. 2018;108:304–10.
Mukonzo JK, Namuwenge PM, Okure G, Mwesige B, Namusisi OK, Mukanga D. Over-the-counter suboptimal dispensing of antibiotics in Uganda. J Multidiscip Healthc. 2013;6:303–10.
Kiguba R, Karamagi C, Bird SM. Extensive antibiotic prescription rate among hospitalized patients in Uganda: but with frequent missed-dose days. J Antimicrob Chemother. 2016;71:1697–706.
Tadesse BT, Ashley EA, Ongarello S, Havumaki J, Wijegoonewardena M, González IJ, et al. Antimicrobial resistance in Africa: a systematic review. BMC Infect Dis. 2017;17:616.
Mwaka A, Mayanja-Kizza H, Kigonya E, Kaddu-Mulindwa D. Bacteriuria among adult non-pregnant women attending Mulago hospital assessment centre in Uganda. Afr Health Sci. 2011;11(2):182–9.
Leopold SJ, van Leth F, Tarekegn H, Schultsz C. Antimicrobial drug resistance among clinically relevant bacterial isolates in sub-Saharan Africa: a systematic review. J Antimicrob Chemother. 2014;69:2337–53.
Evans JK, McOwan A, Hillman RJ, Forster GE. Incidence of symptomatic urinary tract infections in HIV seropositive patients and the use of cotrimoxazole as prophylaxis against Pneumocystis carinii pneumonia. Genitourin Med. 1995;71:120–2.
Church JA, Fitzgerald F, Walker AS, Gibb DM, Prendergast AJ. The expanding role of co-trimoxazole in developing countries. Lancet Infect Dis. 2015;15:327–39.
Uganda Clinical Guidelines 2016. http://library.health.go.ug/sites/default/files/resources/Uganda%20Clinical%20Guidelines%202016_FINAL.pdf. Accessed 12 Nov 2020.
Uganda Clinical Guidelines 2012. http://health.go.ug/docs/UCG_2012.pdf. Accessed 12 Nov 2020.
Kabugo D, Kizito S, Ashok DD, Graham KA, Nabimba R, Namunana S, et al. Factors associated with community-acquired urinary tract infections among adults attending assessment centre Mulago Hospital Uganda. Afr Health Sci. 2016;16:1131–42.
Bitew A, Molalign T, Chanie M. Species distribution and antibiotic susceptibility profile of bacterial uropathogens among patients complaining urinary tract infections. BMC Infect Dis. 2017;17:654.
Sader HS, Flamm RK, Jones RN. Frequency of occurrence and antimicrobial susceptibility of Gram-negative bacteremia isolates in patients with urinary tract infection: results from United States and European hospitals (2009–2011). J Chemother. 2014;26:133–8.
Córdoba G, Holm A, Hansen F, Hammerum AM, Bjerrum L. Prevalence of antimicrobial resistant Escherichia coli from patients with suspected urinary tract infection in primary care. Denmark BMC Infectious Diseases. 2017;17:670.
Hamel MJ, Greene C, Chiller T, et al. Does cotrimoxazole prophylaxis for the prevention of HIV-associated opportunistic infections select for resistant pathogens in Kenyan adults? Am J Trop Med Hyg. 2008;79:320–30.
Okeke IN, Lamikanra A, Edelman R. Socioeconomic and behavioral factors leading to acquired bacterial resistance to antibiotics in developing countries. Emerg Infect Dis. 1999;5:18–27.
Kayima JK, Otieno LS, Twahir A, Njenga E. Asymptomatic bacteriuria among diabetics attending Kenyatta National Hospital. East Afr Med J. 1996;73(8):524–6.
Ferry SA, Holm SE, Stenlund H, Lundholm R, Monsen TJ. Clinical and bacteriological outcome of different doses and duration of pivmecillinam compared with placebo therapy of uncomplicated lower urinary tract infection in women: the LUTIW project. Scand J Prim Health Care. 2007;25:49–57.
Schmiemann G, Kniehl E, Gebhardt K, Matejczyk MM, Hummers-Pradier E. The diagnosis of urinary tract infection. Dtsch Arztebl Int. 2010;107(21):361–7.
Gandee L, Hsieh J-T, Sperandio V, Moreira CG, Lai C-H, Zimmern PE. The efficacy of immediate versus delayed antibiotic administration on bacterial growth and biofilm production of selected strains of uropathogenic Escherichia coli and Pseudomonas aeruginosa. Int Braz J Urol Jan-Feb. 2015;41(1):67–77.
Acknowledgements
We thank all the study subjects for their participation and the staff at Infectious Diseases Institute clinic for their dedicated service during this study. We would like to thank Emmanuel Mande, laboratory technologist at Infectious Diseases Institute for his support in clarification of the laboratory procedures in the study.
Funding
The study design, sample collection, analysis, data interpretation and manuscript writing was funded by the Swiss-African Research Cooperation (SARECO) grant from University of Basel. The views expressed in this paper are not necessarily those of SARECO.
Author information
Authors and Affiliations
Contributions
MK and GA contributed to the conducted literature review and contributed towards interpretation and analysis of the results; writing manuscript. JM, HBT, MK and ML contributed substantially towards the proposal writing; supervision of data entry; analysis and interpretation of the data; writing manuscript. BC and JF contributed towards the study design; proposal writing; interpretation of the results; writing the manuscript. JH and AK provided technical advice in proposal writing and editing the manuscript. NE and SH contributed towards study design; interpretation of results and reviewing of the manuscript. The joint first authors MK and GA and last authors JF and BC both contributed equally to this paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The consent waiver of the study was approved and annually renewed by the School of Medicine Research and Ethics Committee, Makerere University Medical School (Reference number 2009–120), and the Uganda National Council for Science and Technology. This is because the information was collected as part of routine surveillance conducted at the infectious diseases clinic when financial resources are available; all the information was analyzed after stripping it of unique personal identifiers.
Consent for publication
Not applicable.
Competing interests
Dr. Fehr reports grants from Gilead Sciences, grants from MSD, grants from VIIV Healthcare, outside the submitted work. Dr. Kälin reports a grant from SARECO, University of Basel; Switzerland, during the conduct of the study. The rest of the authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix S1.
SOP Microbiology.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abongomera, G., Koller, M., Musaazi, J. et al. Spectrum of antibiotic resistance in UTI caused by Escherichia coli among HIV-infected patients in Uganda: a cross-sectional study. BMC Infect Dis 21, 1179 (2021). https://doi.org/10.1186/s12879-021-06865-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06865-3