Abstract
Background
Ireland frequently reports the highest annual Crude Incidence Rates (CIRs) of cryptosporidiosis in the EU, with national CIRs up to ten times the EU average. Accordingly, the current study sought to examine the spatiotemporal trends associated with this potentially severe protozoan infection.
Methods
Overall, 4509 cases of infection from January 2008 to December 2017 were geo-referenced to a Census Small Area (SA), with an ensemble of geo-statistical approaches including seasonal decomposition, Local Moran’s I, and space–time scanning used to elucidate spatiotemporal patterns of infection.
Results
One or more confirmed cases were notified in 3413 of 18,641 Census SAs (18.3%), with highest case numbers occurring in the 0–5-year range (n = 2672, 59.3%). Sporadic cases were more likely male (OR 1.4) and rural (OR 2.4), with outbreak-related cases more likely female (OR 1.4) and urban (OR 1.5). Altogether, 55 space–time clusters (≥ 10 confirmed cases) of sporadic infection were detected, with three “high recurrence” regions identified; no large urban conurbations were present within recurrent clusters.
Conclusions
Spatiotemporal analysis represents an important indicator of infection patterns, enabling targeted epidemiological intervention and surveillance. Presented results may also be used to further understand the sources, pathways, receptors, and thus mechanisms of cryptosporidiosis in Ireland.
Similar content being viewed by others
Introduction
Cryptosporidium is an oocyst-forming protozoan parasite first identified as a causative agent of gastrointestinal infection in the mid-1970s [1]. Cryptosporidiosis is associated with a wide range of symptoms including watery diarrhoea, weight loss, vomiting, abdominal pain, nausea and fever [2]. In the most severe cases, infection may lead to acute dehydration and death, particularly among immuno-compromised individuals, including children aged ≤ 5 years, the elderly (≥ 65) and patients with underlying health conditions (i.e., immunosuppressed) [3]. To date, approximately 40 genetically distinct Cryptosporidium species have been identified, with C. parvum and C. hominis the most frequently confirmed species among cases of human infection [4]. Transmission typically occurs via the faecal-oral route through consumption of contaminated water or food, in addition to direct human-animal contact and exposure to contaminated environments including recreational water [2, 5,6,7]. A previous experimental study of healthy adult volunteers indicated that ingestion of 30 oocysts is sufficient to initiate infection, with a significantly lower threshold dose (≈ 10 oocysts) associated with specific C. hominis and C. parvum strains [5].
Cryptosporidiosis occurs in both rural and urban environments, with several studies indicating that C. hominis is more frequent in urban areas (due to increased rates of person-to-person transmission) while C. parvum predominates in rural areas [7]. Environmental transmission in rural areas represents a particular concern due to the ability of oocysts to survive for prolonged periods in the natural environment (e.g., soil, water) due to temperature buffering and high humidity [8].
Human cryptosporidiosis became a notifiable disease in Ireland on January 1st 2004 under the Infectious Diseases (Amendment) (No. 3) Regulations 2003 (S.I. 707 of 2003). As such, all medical practitioners are required to notify the regional Medical Officer of Health (MOH)/Director of Public Health of all confirmed cases. According to the most recent European Centre for Disease Prevention and Control (ECDC) report, Ireland consistently reports the highest Crude Incidence Rates (CIR) of confirmed cryptosporidiosis infection in the European Union [9]. For example, during 2017 Ireland reported a cryptosporidiosis CIR of 12.0/100,000 residents, compared with an EU mean CIR of 3.2/100,000 (including 15 member states with national notification rates < 1/100,000) [10]. Nationally, cryptosporidiosis represents the most frequently reported protozoan infection, with CIRs having remained relatively consistent over the past decade, ranging from 11.0/100,000 in 2004 to 13.2/100,000 in 2018 [10]. Unlike other gastroenteric infections (e.g., giardiasis), cryptosporidiosis in Ireland is primarily associated with domestic (indigenous) exposure and transmission. For example, 81% (556/629) of confirmed cases during 2018 were identified as sporadic domestic cases, 12% (n = 73) were associated with a recognised cluster/outbreak, while travel-related cases accounted for 7% (n = 43) of the total case number [10]. The largest Irish cryptosporidiosis outbreak to date was attributed to C. hominis and occurred in the west of Ireland during March/April 2007. This was concentrated around Galway city, with at least 242 confirmed cases caused by municipal wastewater ingress to Lough Corrib, a lake employed for public water supply in the region [11]. The economic and human health burden accruing from events like the “Galway outbreak”, recently estimated at approximately €19 million [11] coupled with the high baseline incidence of cryptosporidiosis, create a need for a greater understanding of the sources and transmission routes for the disease.
While several studies have examined the likely routes of exposure to Cryptosporidium spp. in Ireland [e.g., 12,13], few epidemiological investigations of the spatiotemporal dynamics of confirmed cryptosporidiosis infection has been undertaken. This represents a significant knowledge gap with respect to understanding pathogen sources and pathways, particularly in light of the endemic nature of cryptosporidiosis in Ireland. An improved mechanistic understanding of infection occurrence would enable earlier detection, enhanced surveillance, and more focused public-health and healthcare policies. The current study sought to explore the temporal and spatial patterns of domestically acquired (sporadic and outbreak-related) cases of cryptosporidiosis in Ireland via identification of infection clustering. To accurately describe the epidemiological patterns of this important zoonotic parasite, the study integrated several modelling approaches including seasonal decomposition, spatial autocorrelation (Anselin Local Moran’s I), hot-spot analysis (Getis-Ord Gi*) and space–time scanning with a large georeferenced dataset of confirmed cryptosporidiosis cases (n = 4509) over a 10-year period (2008–2017). To the authors’ knowledge, this represents the first spatio-temporal study of its kind in Ireland, which as previously described, exhibits the highest national cryptosporidiosis infection CIRs in the EU.
Methods
Data collection and processing
Irreversibly anonymised cases of cryptosporidiosis reported by regional departments of public health between 1st January 2008 and 31st December 2017 were provided from the national Computerised Infectious Disease Reporting (CIDR) database. Data prior to 2008 were excluded to avoid potential bias being introduced by the large number of cases reported during the 2007 Galway outbreak. All confirmed cases, including patient-specific data fields [age, gender, date of reporting, and case outcome (severity)] were geo-spatially linked to the geographical centroid of their associated Census Small Area (SA) (the smallest administrative unit currently employed for census reporting in Ireland) using the Health Service Executive (HSE) Health Intelligence Unit’s geocoding tools. Sporadic, outbreak-related, and travel-related (non-outbreak) cases were defined and discretized for analyses. Outbreak-related cases are defined as confirmed cases with an attached “CIDR outbreak ID”, used for identifying cases associated with a recognised infection outbreak or cluster. Travel-related cases are specifically categorised for purposes of analytical exclusion or adjustment (i.e., national reporting) and defined as any patient self-reporting travel outside of Ireland within the likely incubation period. Sporadic cases were subsequently delineated via exclusion of the two previous categories from the total case dataset. All case data and analyses were granted full research ethics approval by the Royal College of Physicians of Ireland Research Ethics Committee (RCPI RECSAF_84).
As cryptosporidiosis in Ireland is most prevalent among children ≤ 5 years of age and in rural areas [10], specific analyses were undertaken with respect to case age (≤ 5 years, ≥ 6 years) and land-use classification (rural/urban). The Central Statistics Office (CSO) Census of 2011 and 2016 were used to extract Electoral Division (ED)- and SA-specific human population counts, permitting calculation of cryptosporidiosis incidence rates at both spatial (administrative unit) scales. The CSO’s 14 urban/rural categories were used to classify each spatial unit as rural or urban. Population density and settlement size were employed to verify all classifications. For reporting purposes within the current article, Ireland has been delineated into eight distinct geographical zones (Fig. 1). Zone NE (corresponding to Northern Ireland) is located outside Irish public health legislative jurisdiction and was not included for analyses. Pearsons χ2 test with Yates’ continuity corrections and Fisher’s exact test (where any cell had < 5 cases) were used to test for association between categorical case classifications.
Seasonal decomposition
Seasonal decomposition was carried out using Seasonal and Trend (STL) decomposition via the LOESS (Locally Estimated Scatterplot Smoothing) method on different subsets of the case dataset, e.g., sporadic cases, outbreak-related cases, cases in children ≤ 5 years of age, cases in people ≥ 6 years of age, travel-related cases and cases in urban vs. rural areas. The monthly incidence of infection was calculated for each case sub-category. The STL method decomposes incidence data (Yv) time-series into three separate component series: seasonal variation (Sv), overall trend over time (Tv) and residuals (Rv), whereby the incidence data is equal to the sum of all three trends denoted by [14]:
An additive seasonal decomposition formula was used, as opposed to multiplicative, to remove seasonality (Sv) and trend (Tv) from the overall time-series (Yv) and filter random variation from long-term trends given by the residuals (Rv) so that: Residuals (Rv) = Time series (Yv) − Seasonal trend (Sv) − Trend (Tv).
Spatial autocorrelation
The total number of sporadic cryptosporidiosis cases, sporadic cases in children ≤ 5, people aged ≥ 6 years, and outbreak-related cases were mapped to individual SA centroids. Age-adjusted infection rates within each sub-category were calculated at both SA and ED level, based on 2011/2016 census data. Outbreak-related infection rates were calculated as a proportion of overall cases within each SA and ED. Data aggregation and infection rate calculation were carried out in R statistical software version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria). Anselin Local Moran’s I was employed for spatial autocorrelation.
Anselin Local Moran’s I focuses on the relationship of individual features with nearby features and assigns clusters based on variance assigned to individual spatial units, thus negating the assumption underlying the Global Moran’s I statistic that a single statistic appropriately accounts for clustering and dispersion of the spatial predominance of infection across the entire study area [15]. The Anselin Local Moran’s I statistic is calculated by generating a neighbour list of spatially proximal SAs or EDs and calculating spatial autocorrelation of similar infection rates as a function of distance bands, thus identifying localised clusters which are correlated based on the variance assigned to all individual spatial units [15, 16]. Clusters of high-high (H–H) and low–low (L–L) infection, and outliers of high–low (H–L) and low high (L–H) infection are subsequently identified. Local Moran’s I statistics were calculated using the cluster and analysis tool in ArcGIS version 10.6 (ESRI, Redlands, California) which generates a Moran’s I statistic, z-score and pseudo p-value for each spatial unit. A positive I value is indicative of spatial units with a high or low infection rate, surrounded by SAs or EDs with similarly high or low infection rates. Conversely, a negative I value indicates outliers of infection where an SA or ED with a high rate of infection is surrounded by SAs or EDs with low rates of infection, and vice versa [15].
Hot-spot analysis (Getis-Ord GI*)
Hot-spot analysis was carried out for all sporadic cases, sporadic cases among children ≤ 5, cases ≥ 6 years, and outbreak cases by calculating spatially specific Getis-Ord GI* statistics in ArcGIS. The Getis-Ord Gi* statistic is calculated for each feature (SA or ED) in the dataset, generating a unit-specific z-score and p-value, used to statistically determine significant spatial clustering of features in the dataset [17]. Statistically significant clusters are clusters which have high values surrounded by SAs or EDs with similarly high values, and vice versa [18]. Hot- and cold-spots of infection are determined based on the spatial proximity of high/low values statistically similar to neighbouring features. Compared with Anselin local Moran’s I statistics, clusters based on the Getis-Ord GI* statistic are determined by comparing the sum of local features and their neighbours with the overall sum of all features. Getis-Ord GI* statistics were used to examine whether differing statistical analyses of spatial clustering of infection between spatial units yield varying results. The Getis-Ord GI* statistic is given as [18]:
where χj is the attribute value for feature j, wi,j is the spatial weight between feature i and j, n is equal to the total number of features and:
Space–time scanning
Space–time scanning was undertaken using SaTScan v9.6 software (Kulldorf and Information Management Services, Inc., MA, USA). SaTScan detects spatial clusters of areal units (i.e., SAs/EDs) by imposing an infinite number of overlapping circular (or elliptical) scanning windows of predetermined sizes across a defined geographic area [19]. Temporal clusters were simultaneously assessed using the scan statistic, which includes an infinite number of overlapping cylindrical windows defined by a base (spatial scan statistic) and height (temporal scan statistic) [20].
A discrete Poisson model was employed for space–time scanning to account for the high-resolution spatial scale (n = 18,488 SAs), resulting in high zero/one inflation (i.e., high numbers of SAs with 0 or 1 case). A case threshold of 10 cases (minimum) per cluster was selected to ensure that identified clusters were significant i.e., avoidance of single household clusters. Similarly, a maximum of 10% of population at risk (PAR) was employed concurrently with a maximum cluster radius of 50 kms to account for low case numbers within individual Small Areas. Data were aggregated at a monthly scale, with maximum cluster duration set to 3 months to account for known seasonal variation of cryptosporidiosis in Ireland.
SaTScan analyses produce two primary outputs; a spatial cluster location(s) (cluster centroid and diameter) and descriptive cluster data (start/end dates, total population, number of observed-expected cases, relative risk, and p-value). The authors have developed a novel mapping approach for representing SaTScan results, whereby all significant clusters (p < 0.05) are selected and mapped in ArcGIS (ArcGIS 10.6), with binary cluster location [i.e., Cluster Membership (0/1)] for annual space–time scans summed at the CSO SA scale. The final mapping provides a “cluster recurrence” index ranging from 0 to 10 (i.e., annual absence/presence of cluster over 10-year study period).
Results
Occurrence of cryptosporidiosis infection in the Republic of Ireland (2008–2017)
The dataset comprised 4,633 confirmed cases of cryptosporidiosis from 2008 to 2017, of which 4509 cases (97%) were successfully geo-linked to a distinct spatial unit (SA/ED centroid). Overall, 1964 Electoral Divisions (58% of 3,409), 3413 Small Areas (18.3% of 18,488) and all (26/26) Irish counties were associated with at least one confirmed case. Most cases were associated with children ≤ 5 years (n = 2672, 59.3%) (Fig. 2), with a slightly higher incidence rate reported among males (53%) (Table 1).
As shown (Table 1), sporadic cases were statistically more likely to be male (OR 1.4, 95% CI 1.2, 1.6), ≤ 5 years of age (OR 1.5, 95% CI 1.3, 1.8), and associated with a categorically rural area (OR 2.4, 95% CI 2, 28). Conversely, outbreak-related cases were associated with females (OR 1.4, 95% CI 1.2, 1.7) and urban areas (OR 1.5, 95% CI 1.3, 1.9). Travel-related cases were more likely to be female (OR 1.3, 95% CI 1, 1.6), > 5 years of age (OR 2.4, 95% CI 1.5, 3.1), and resident in an urban conurbation (OR 3.6, 95% CI 2.8, 4.6). Temporal cumulative incidence rates (Fig. 3) indicate a marked annual peak in late spring (n = 1812), with a maximum incidence rate occuring during April (n = 916). Lowest incidence rates were recorded during winter months (n = 493) with the lowest incidence rate being recorded in January (n = 136). Case numbers peaked in 2017 (n = 584).
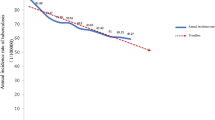
Seasonal decomposition
Seasonal decomposition of sporadic infection over the ten-year study period indicates a clear seasonal peak in mid-spring (April) annually (Fig. 4). Residual trends show a generally consistent annual and long-term trend with a notable peak of infection in April 2016 (Residual: + 56). Outbreak cases exhibit a similar seasonal trend to that of sporadic cases with annual peaks occurring in April, followed by a secondary peak in September. The overall long-term trend in outbreak cases displayed a marked increase during 2011, continuing until 2014. Residuals calculated for outbreak cases point to more variation in 10-year trends with peaks observed during the late winter/early spring months (January to March) of 2011, 2012 and 2017 while late spring/early summer peaks (April to June) were observed in 2013. A peak in outbreak-associated cases was also observed during the winter months (October to November) of 2013.
There was an increasing trend in the number/rate of travel-associated cases with an annual peak occurring in August/September (Fig. 5). The long-term trends varied significantly between delineated age categories with considerably more variation noted among children ≤ 5 years of age (Fig. 6), albeit annual peaks were observed among both age cohorts during April of each year. Residuals again point to a large transmission peak (Residuals: + 22, + 34) within both sporadic and outbreak cohorts during April 2016.
Annual decomposed patterns of infection peaked in April of each year followed by a significantly smaller peak during September in both urban and rural areas (Fig. 7). Calculated residuals point to an infection peak in April 2016 in both urban (+ 18) and rural (+ 38) areas, consistent with trends observed among sporadic and age-delineated infection peaks.
Spatial autocorrelation
A significant H–H cluster of sporadic cases was observed in the midland (M) region, with a large L–L cluster identified along the eastern seaboard (E), surrounding the greater Dublin urban area and commuter belt (Fig. 8a). L–L clusters were also observed in the S and SE regions, spatially proximal to the urban conurbations of Cork, Waterford, and Limerick cities. Smaller H–H clusters of infection were observed in the S, SE and W regions of the country, consistent with an overarching urban/rural pattern. Notable L–L outbreak-related case clusters were observed in the east of the country surrounding Dublin city and in the south surrounding Limerick city (Fig. 8b). Few H–H clusters were associated with outbreak-related cases, however H–H cases identified in the midland region (M) were surrounded by L–H clusters, thus indicating potential neighbouring outliers. H–H and L–L clusters of infection in children ≤ 5 followed a broadly similar spatial pattern to that observed within the sporadic case cohort, due to the large proportion of cases from this cohort comprising the total dataset (Fig. 8c). A large H–H cluster was observed in the M region, with smaller H–H clusters again identified in S, SE and W regions. L–L clusters of infection were also consistent with sporadic case clusters and typically identified around urban areas in the S and SE of the country. The spatial predominance of infection cold spots (L–L) among people age > 5 (Fig. 8d) followed a similar pattern of infection cold spots among sporadic cases and paediatric (≤ 5 years) cases (Fig. 8c). However, the spatial predominance of infection hot spots among this cohort was markedly different to sporadic and ≤ 5-year hot spots, with smaller and more spatially dispersed hot spots identified, primarily in the midlands (region M) and SW regions.
a Sporadic cryptosporidiosis case clusters and outliers determined by Anselin Local Moran’s I clusters b Outbreak-related cryptosporidiosis case clusters and outliers determined by Anselin Local Moran’s I clusters c Sporadic cryptosporidiosis case clusters and outliers among children aged 5 years and younger determined by Anselin Local Moran’s I clusters d Sporadic cryptosporidiosis case clusters and outliers among the cohort of people age 6 years and older determined by Anselin Local Moran’s I clusters
Hot-spot analysis (Getis-Ord GI*)
Getis-Ord GI* analyses identified notable hot spots among sporadic cases in the midlands (M), east and north-east of Galway city, with smaller hot spots also evident in the midlands, south and south-east (M, S and SE) (Fig. 9a). Again, a spatially extensive cold spot was identified in the east of the country (E), encompassing the greater Dublin metropolitan urban area, and in the south and south-east (S and SE) around Waterford, Limerick and Cork cities.
a Sporadic cryptosporidiosis case hot and cold spots determined by Getis-Ord Gi* hot-spot analysis—b Outbreak-related cryptosporidiosis hot and cold spots determined by Getis-Ord Gi* hot-spot analysis—c Sporadic cryptosporidiosis case hot and cold spots among children aged 5 years and younger determined by Getis-Ord Gi* hot-spot analysis—d Sporadic cryptosporidiosis case hot and cold spots among the cohort of people age 6 years and older determined by Getis-Ord Gi* hot-spot analysis
The spatial predominance of hot and cold spots among children ≤ 5 years again followed a similar pattern to clustering of infection among all sporadic cases (Fig. 9c). Large hot spots were observed in the midlands and south (M and S), with a previously identified sporadic infection hot spot in the west (W) demonstrating a significantly more pronounced occurrence among the paediatric subpopulation (NE of Galway city). A large cold spot among children ≤ 5 was also observed in the in the greater Dublin area (E), albeit significantly reduced when compared with that observed among all sporadic infections. The spatial distribution of hot and cold spots of infection among people aged > 5 varied (Fig. 9d), with the spatial distribution of hot and cold spots of sporadic infection and infection in children ≤ 5. One hot spot was identified in the SW region, which was not observed using other statistical methods or among other subcategories of infection.
Space–time scanning
Space–Time clustering recurrence and cluster temporality for sporadic cryptosporidiosis cases are presented in Fig. 10, with results of year-on-year space–time scanning presented in Additional file 1: Appendix 1. Annual space-time clusters of Cryptosporidiosis in Ireland from 2008 to 2017; Appendix 2. Space-time clusters of Cryptosporidiosis in Ireland during 2008. As shown (Fig. 10), three primary hot spots were identified: south-west and east of Limerick city (SW, S, SE), and north-east of Galway city (M). Cold spots are persistent along much of the eastern seaboard, and particularly around the larger urban conurbations of greater Dublin and Cork city, in addition to significant areas of the western coastline. The temporal window for space–time clusters mirrors the general seasonal distribution of cryptosporidiosis infection (Sect. 3.2), with peak cluster identification occurring from March to June and peaking in April.
Significantly lower levels of space–time clustering were found among outbreak-related cases (Fig. 11), with largest hot spots located in western and midland regions (M, W), and a maximum cluster recurrence of 30% (i.e., geographic area included in 3 identified clusters over 10 annual iterations). Two additional space–time clusters were identified to the north-east of Cork city (S) and County Donegal (N). Most (8/9) outbreak-related clusters were observed from March to June, with one cluster occurring during October/November (2013). Cluster index mapping for ≤ 5 year sub-population mirrored that of sporadic cases, with three primary hot spots identified; again, a large area located north-east of Galway city (M), and two “secondary” (i.e., lower cluster recurrence indices) areas located south-west and south-east of Limerick city (SW,S) (Fig. 12). Results for the sub-population > 5 years point to a lower level of clustering, with hot spots located south-west of Limerick city (SW), the Midlands (M) and south-east (SE) (Fig. 13).
Discussion
Occurrence of sporadic and outbreak-associated cryptosporidiosis
Cryptosporidiosis exhibits a relatively wide geographical distribution in Ireland with 58% and 18.3% of Electoral Divisions and Small Areas associated with at least one confirmed case during the study period, respectively. Crude Incidence Rates (CIRs) of infection indicate a moderately increasing trend, ranging from 9.8/100,000 in 2008 to 12.4/100,000 in 2017 [10]. Most (59.3%) sporadic cases were associated with children ≤ 5 years, which concurs with several previous studies [3, 7]. Within the ≤ 5 years cohort, cases were more frequently associated with male children (OR 1.3873), potentially reflecting the tendency of male children to mount weaker immune responses [21], an enhanced susceptibility to environmental exposures via gender-related outdoor activities [22], or a gender-related bias in healthcare-seeking behaviours [23]. Conversely, female children were statistically associated with outbreak-related cryptosporidiosis, potentially reflecting higher levels of direct contact (and subsequent transmission) between parents/family members and female children [24]. A recent small-scale investigation of the regional epidemiology of cryptosporidiosis in County Cork, Ireland, demonstrated moderately increased infection rates among 20–34-year olds, suggesting likely anthroponotic transmission via caregiver contact with infected children [25]. Geographically, most sporadic cases (65.8%) occurred in categorically rural areas (χ2 = 110.493, p < 0.001; Table 1), where approximately 37.3% of the Irish populace reside [26]. A previous Scottish study by Pollock et al. similarly found C. parvum infection was associated with areas characterised by lower human population density and a higher ratio of farms to humans, both indicators of rurality [27]. While the current study represents the first nationwide study of the spatiotemporal epidemiology of cryptosporidiosis in Ireland, this finding was expected, and likely attributable to increased exposure to sources of Cryptosporidium spp. oocysts in rural areas, including farmyard animals [28], direct exposure to contaminated surface waters [29] and the use of groundwater as a drinking water source [6]. Conversely, urban areas exhibited a significantly higher secondary (OR 1.5383) and travel-related (OR 3.5742) case occurrence, likely indicative of C. hominis infections as opposed to the agriculturally (rural) associated C. parvum, however, as Cryptosporidium spp. is not identified within the Irish disease reporting system, this is somewhat speculative.
Seasonal decomposition
Seasonal decomposition points to an overall increasing temporal trend over the ten-year study period (Fig. 4), consistent with previously reported trends in the west of Ireland during 2004–2007 [30]. Specifically, the annual peak found during April is consistent with previously reported regional peaks (March/April) [30], in addition to those reported in Scotland (April/May) [27], likely associated with agricultural cycles in temperate regions i.e. lambing/calving and manure spreading. While not reported in the current study, seasonal patterns may vary among differing Cryptosporidium species; for example, C. hominis is more prevalent during autumn in the UK and New Zealand (increased travel and school/childcare attendance), whereas C. parvum is more typically encountered during spring in Canada, Ireland and The Netherlands [9]. The secondary peak observed among outbreak-related cases during September (Fig. 4) is consistent with the bimodal peaks observed in C. hominis in Scotland in August and October [27], and may reflect the increase in national/international travel and children returning to childcare/school after summer break.
Seasonal decomposition also identified several notable deviations (i.e., residual peaks) from the overarching temporal trend which merit closer investigation, particularly regarding dynamic drivers of exposure/transmission such as extreme weather events [28, 31]. A marked positive residual was identified during April 2016 (Fig. 4), initiating further exploration with respect to dynamic meteorological events, particularly in light of severe flooding experienced across Ireland and the UK [32]. Winter 2015/2016 was characterised by a succession (n = 6) of Atlantic storms across Ireland, resulting in exceptional and widespread flooding with all synoptic weather stations reporting rainfall volumes significantly above their Long-Term Average (LTA) [32]. Recent work by Boudou et al. have shown that excess cases of cryptosporidiosis were widespread during and after the flood period, with areas characterised by the presence of a surface water body exhibiting significantly higher incidence rates (OR 1.363; p < 0.001) [32]. Time-series modelling of the event presented a clear association between rainfall, surface water discharge, groundwater levels and infection incidence, with lagged associations from 16 to 20 weeks particularly strong, thus indicating a link between infection peaks (April 2016) and the flood event which began approximately 18 weeks earlier [32]. Thus, it was concluded that increases in storm water, soil saturation and surface runoff increased pathogen mobility for a significant period, thus exacerbating transmission of cryptosporidiosis both directly (i.e., contaminated ‘raw’ water and food) and indirectly (i.e., long-term soil saturation) [32]. Similarly, a cryptosporidiosis outbreak which occurred during August 2013 in Halle, Germany, began six weeks after the river Saale inundated the floodplain and parts of the city centre [3], thus emphasising the (lagged) impact of local meteorological conditions on the incidence of infection.
Spatial autocorrelation and Hot-Spot analysis
Incorporating a spatial dimension into investigations of infectious disease epidemiology is of primary importance considering the spatial variation of environmental exposure such as land use, local climate, and socioeconomic status, particularly in Ireland which has previously been described as “the perfect storm” with regard to potential gastroenteric infection risk factors [33]. Results of Anselin Local Moran’s I statistics and the Getis Ord GI* statistic provided relatively similar spatial patterns. High incidence (H-Hs) clusters were identified in the Irish Midlands (M), a predominantly rural area with a high level of dependence on pastoral agriculture and “private infrastructure” (e.g., one-off housing with on-site wastewater treatment and domestic water supplies). Several previous studies have documented strong associations between cryptosporidiosis and cattle density [27, 34]. Similarly, a study from central Wisconsin previously found the incidence of endemic diarrhoeal infections significantly higher in areas characterised by elevated septic tank (OR 1.22) and private water supply (OR 6.18) densities among a population-based cohort [35]. Conversely, low incidence (L-L) clusters were primarily located in the vicinity of Ireland’s capital (Dublin) and other relatively large cities (Waterford, Cork, Limerick, Galway), thus likely highlighting the protective effect of urban living within the Irish context, where reduced environmental exposure to pathogen sources coupled with reduced pathogen transport (i.e., treated drinking water supply) may reduce the risk of exposure and subsequent infection [36]. Conversely, recent studies have shown rates of cryptosporidiosis are typically higher in urban areas characterised by elevated human population densities, for example Cohen et al. previously reported that higher population density and above average household sizes were associated with increased odds of reported cases of cryptosporidiosis in Massachusetts [37]. Likewise, Greenwood & Reid have found that most cryptosporidiosis clusters identified across Queensland, Australia from 2001 to 2015 centred on major and regional cities [38].
Both geostatistical techniques suggest a disparity exists with respect to outbreak-related clustering over the 10-year study period, as they relate to clustering of sporadic cases (Figs. 8a, b, 9a, b), with outbreak-related clusters occurring in the north Midlands and “border area”, regions traditionally characterised by relatively low population densities. This merits further investigation within the context of population age structure, household size and domestic water source, along with close monitoring and surveillance by the relevant Departments of Public Health.
Space–Time scanning and cluster recurrence
Space–time scan statistics detect temporally-specific clusters characterised by a significantly higher observed case number than expected (e.g., space–time randomness not present), based on calculated baseline incidence rates [20] with the approach employing a 3-dimensional (cylindrical) scanning window comprising both height (time) and space (geographic area) [19]. Over the past decade, space–time scan statistics have been recognised as a powerful tool for endemic disease surveillance and early outbreak detection [39], however to the authors knowledge, this represents the first time it has been applied to infectious disease incidence in Ireland. A total of 69 space–time clusters (≥ 10 confirmed cases) were identified over the 10-year study period, of which 55 (79.7%) were clusters of sporadic infection, ranging from a minimum of 4 (7.3%) during 2017 to a maximum of 7 (12.7%) during 2009. No statistical association was found between annual sporadic and outbreak-related cluster number during the study period, however development of the “cluster recurrence” index (e.g., Figs. 10, 11, 12, 13) permits identification of discernible spatial and temporal patterns defining the formation of clusters across the decade-long period. Three regions exhibited particularly recurrent space–time clusters of infection, with occurrences during ≥ 8 out of 10 years, namely south-west and east of Limerick city (SW, S, SE), and north-east of Galway city (M), with neither urban conurbation actually located within a high recurrence region. The spatiotemporal frequency of space–time clusters suggests the presence of persistent reservoirs in these areas thus maintaining community and/or transmission pathways [38]. The proximity of large urban centres to each high-recurrence region may potentially reflect relatively narrow transitional zones between urban fabric and populated rural regions i.e., rural commuter belts which remain un-serviced with respect to municipal wastewater treatment and/or drinking supplies. Additionally, all three regions are predominantly underlain by karstified carboniferous limestone aquifers [40] which have previously been associated with the presence of Cryptosporidium spp. in private and small public drinking water supplies [12, 41]. Conversely, the Greater Dublin area, characterised by a large urban commuter belt, spatially extensive consolidated bedrocks and high levels of municipal water and wastewater infrastructure, did not exhibit any space–time clusters over the study period. A significant majority of space–time clusters occurred over the 4-month period May–June, thus mirroring findings from the overall case cohort, and further highlighting the likely association between agricultural cycles and the incidence of infection in temperate regions including Ireland, Scotland and New Zealand [27, 42]. Additionally, Lal et al. have signalled a need to study the effect of spatial and temporal variations in ecological and social risk factors on the incidence of cryptosporidiosis with specific emphasis on the potential for socioeconomic disadvantage to amplify disease risk within populations, e.g., in areas of low educational attainment and lower income levels, which are often associated with rural living [28].
From a public-health surveillance perspective, identification of 55 space–time clusters of sporadic cryptosporidiosis infection over a 10-year period represents a concern, while underscoring the major challenges involved in decreasing the incidence of infection via enhanced surveillance and subsequent intervention. For example, during 2008, a spatially restricted space–time cluster which was identified in the northern Midlands (Cluster 2, Additional file 1: Appendix) was characterised by almost 18 times more cases of infection than would be expected (RR 17.95) over a three-month period (February–April), with several identified space–time clusters occurring over time periods as short as 4 weeks. As such, this level of clustering may suggest the need for new surveillance and/or analytical methods to elucidate hitherto unidentified sources and pathways of infection, and to identify space–time clusters while they exist i.e., real-time or prospective scanning [43].
It is important to note that a lack of species information, and particularly the inability to discern between C. parvum and C. hominis, the two most frequently encountered Cryptosporidium species in Ireland, represents a study limitation. As previously outlined, Pollock et al. found C. parvum infection to be associated with lower population density and higher ratio of farms to humans, indicators of rurality, while C. hominis was more likely to be found in the more urban area of southern Scotland [27]. Speciation would thus permit closer elucidation of sociodemographic influences on rural/urban distribution. Further investigation is required to elucidate potential sources and pathways of infection, with particular regard to livestock densities, climate, hydrogeology and socioeconomic status.
In conclusion, despite mandatory surveillance of cryptosporidiosis due to its communicable disease status in Ireland, it is widely regarded that cryptosporidiosis remains under-reported in Ireland and on a broader European level. The spatiotemporal epidemiology of cryptosporidiosis in Ireland reflects the diverse population and geography of the country, albeit with a markedly higher rate of occurrence in rural areas, likely due to the ubiquity of Cryptosporidium spp. sources (e.g., cattle) and pathways (e.g., karstic limestone bedrocks). The elevated burden among children ≤ 5-years is likely related to both immunological status and specific routes of exposure and warrants further study. The presented study represents a significant advance in efforts to investigate the spatiotemporal epidemiology of cryptosporidiosis with a view to further elucidating pathways of infection to guide public-health interventions through an improved understanding of its spatio-temporal occurrence, clustering mechanisms, levels of recurrence, and associated drivers, pathways, and receptors.
Availability of data and materials
Due to the sensitive nature of the study data, datasets are not publicly available. For further information related to data acquisition, please contact the corresponding author, Dr Paul Hynds (email: Paul.Hynds@tudublin. i.e., phone: 0,838,256,888).
References
Nime FA, Burek JD, Page DL, Holscher MA, Yardley JH. Acute enterocolitis in a human being infected with the protozoan Cryptosporidium. Gastroenterology. 1976;70(4):592–8.
Fayer R, Ungar BL. Cryptosporidium spp. and cryptosporidiosis. Microbiol Rev. 1986;50(4):458.
Chalmers RM, Cacciò S. Towards a consensus on genotyping schemes for surveillance and outbreak investigations of Cryptosporidium, Berlin, June 2016. Eurosurveillance. 2016;21(37):30338.
Feng Y, Ryan UM, Xiao L. Genetic diversity and population structure of Cryptosporidium. Trends Parasitol. 2018;34(11):997–1011.
Chappell CL, Okhuysen PC, Langer-Curry R, Widmer G, Akiyoshi DE, Tanriverdi S, Tzipori S. Cryptosporidium hominis: experimental challenge of healthy adults. Am J Trop Med Hyg. 2006;75(5):851–7.
Chique C, Hynds P, Andrade L, Burke L, Morris D, Ryan MP, O’Dwyer J. Cryptosporidium spp. in groundwater supplies intended for human consumption–a descriptive review of global prevalence, risk factors and knowledge gaps. Water Res. 2020;115726.
Putignani L, Menichella D. Global distribution, public health and clinical impact of the protozoan pathogen Cryptosporidium. Interdisciplinary perspectives on infectious diseases, 2010.
Thompson RA, Koh WH, Clode PL. Cryptosporidium—what is it? Food Waterborne Parasitol. 2016;4:54–61.
European Centre for Disease Prevention and Control. Cryptosporidiosis. In: ECDC. Annual epidemiological report for 2017. Stockholm: ECDC; 2019.
Health Protection Surveillance Centre (HPSC). (2019) Cryptosporidiosis in Ireland, 2018. Dublin, Ireland. https://www.hpsc.ie/a-z/gastroenteric/cryptosporidiosis/publications/epidemiologyofcryptosporidiosisinirelandannualreports/.
Chyzheuskaya A, Cormican M, Srivinas R, O’Donovan D, Prendergast M, O’Donoghue C, Morris D. Economic assessment of waterborne outbreak of cryptosporidiosis. Emerg Infect Dis. 2017;23(10):1650.
Zintl A, Proctor AF, Read C, Dewaal T, Shanaghy N, Fanning S, Mulcahy G. The prevalence of Cryptosporidium species and subtypes in human faecal samples in Ireland. Epidemiol Infect. 2009;137(2):270–7.
Cummins E, Kennedy R, Cormican M. Quantitative risk assessment of Cryptosporidium in tap water in Ireland. Sci Total Environ. 2010;408(4):740-753.12.
Cleveland RB, Cleveland WS, McRae JE, Terpenning I. STL: a seasonal-trend decomposition. J Off Stat. 1990;6(1):3–73.
Anselin L, Syabri I, Smirnov O. Visualizing multivariate spatial correlation with dynamically linked windows. In Proceedings, CSISS Workshop on New Tools for Spatial Data Analysis, Santa Barbara. 2002.
Mao Y, Zhang N, Zhu B, Liu J, He R. A descriptive analysis of the Spatio-temporal distribution of intestinal infectious diseases in China. BMC Infect Dis. 2019;19(1):766.
Guo C, Du Y, Shen SQ, Lao XQ, Qian J, Ou CQ. Spatiotemporal analysis of tuberculosis incidence and its associated factors in mainland China. Epidemiol Infect. 2017;145(12):2510–9.
Varga C, Pearl DL, McEwen SA, Sargeant JM, Pollari F, Guerin MT. Area-level global and local clustering of human Salmonella Enteritidis infection rates in the city of Toronto, Canada, 2007–2009. BMC Infect Dis. 2015;15(1):1–13.
Kulldorff M, Heffernan R, Hartman J, Assunçao R, Mostashari F. A space–time permutation scan statistic for disease outbreak detection. PLoS Med. 2005;2(3):e59.
Linton SL, Jennings JM, Latkin CA, Gomez MB, Mehta SH. Application of space-time scan statistics to describe geographic and temporal clustering of visible drug activity. J Urban Health. 2014;91(5):940–56.
Muenchhoff M, Goulder PJ. Sex differences in pediatric infectious diseases. J Infect Dis. 2014;209(suppl_3):S120–6.
Jarman AF, Long SE, Robertson SE, Nasrin S, Alam NH, McGregor AJ, Levine AC. Sex and gender differences in acute pediatric diarrhea: a secondary analysis of the Dhaka study. J Epidemiol Global Health. 2018;8(1):42–7.
Sarker AR, Sultana M, Mahumud RA, Sheikh N, Van Der Meer R, Morton A. Prevalence and health care–seeking behavior for childhood diarrheal disease in Bangladesh. Global Pediatric Health, 2016;3: 2333794X16680901.
Guerra-Silveira F, Abad-Franch F. Sex bias in infectious disease epidemiology: patterns and processes. PLoS ONE. 2013;8(4):e62390.
O’Leary JK, Blake L, Corcoran D, Elwin K, Chalmers R, Lucey B, Sleator RD. Cryptosporidium spp surveillance and epidemiology in Ireland: a longitudinal cohort study employing duplex real-time PCR based speciation of clinical cases. J Clin Pathol. 2020;73(11):758–61.
Central Statistics Office (CSO). Census of Population, 2016 (Ireland)—Profile 2 Population Distribution and Movements. 2019. https://www.cso.ie/en/releasesandpublications/ep/p-cp2tc/cp2pdm/pd/.
Pollock KGJ, Ternent HE, Mellor DJ, Chalmers RM, Smith HV, Ramsay CN, Innocent GT. Spatial and temporal epidemiology of sporadic human cryptosporidiosis in Scotland. Zoonoses Public Health. 2010;57(7–8):487–92.
Lal A, Hales S, French N, Baker MG. Seasonality in human zoonotic enteric diseases: a systematic review. PLoS ONE. 2012;7(4):e31883.
Hamilton KA, Waso M, Reyneke B, Saeidi N, Levine A, Lalancette C, et al. Cryptosporidium and Giardia in wastewater and surface water environments. J Environ Qual. 2018;47(5):1006–23.
Callaghan M, Cormican M, Prendergast M, Pelly H, Cloughley R, Hanahoe B, O’Donovan D. Temporal and spatial distribution of human cryptosporidiosis in the west of Ireland 2004–2007. Int J Health Geogr. 2009;8(1):1–9.
Britton E, Hales S, Venugopal K, Baker MG. The impact of climate variability and change on cryptosporidiosis and giardiasis rates in New Zealand. J Water Health. 2010;8(3):561–71.
Boudou M, ÓhAiseadha C, Garvey P, O’Dwyer J, Hynds P. Flood hydrometeorology and gastroenteric infection: the Winter 2015–2016 flood event in the Republic of Ireland. J Hydrol. 2021;599:126376.
O’Dwyer J, Hynds PD, Byrne KA, Ryan MP, Adley CC. Development of a hierarchical model for predicting microbiological contamination of private groundwater supplies in a geologically heterogeneous region. Environ Pollut. 2018;237:329–38.
Luffman I, Tran L. Risk factors for E. coli O157 and cryptosporidiosis infection in individuals in the karst valleys of east Tennessee, USA. Geosciences. 2014;4(3):202–18.
Borchardt MA, Chyou PH, DeVries EO, Belongia EA. Septic system density and infectious diarrhea in a defined population of children. Environ Health Perspect. 2003;111(5):742–8.
Lal A, Dobbins T, Bagheri N, Baker MG, French NP, Hales S. Cryptosporidiosis risk in New Zealand children under 5 years old is greatest in areas with high dairy cattle densities. EcoHealth. 2016;13(4):652–60.
Cohen SA, Egorov AI, Jagai JS, Matyas BT, DeMaria A Jr, Chui KK, et al. The SEEDs of two gastrointestinal diseases: socioeconomic, environmental, and demographic factors related to cryptosporidiosis and giardiasis in Massachusetts. Environ Res. 2008;108(2):185–91.
Greenwood KP, Reid SA. Clustering of cryptosporidiosis in Queensland, Australia, is not defined temporally or by spatial diversity. Int J Parasitol. 2020;50(3):209–16.
Tango T, Takahashi K, Kohriyama K. A space–time scan statistic for detecting emerging outbreaks. Biometrics. 2011;67(1):106–15.
Woodcock NH, Strachan RA. Geological history of Britain and Ireland. John Wiley & Sons; 2009.
Darnault CJ, Peng Z, Yu C, Li B, Jacobson AR, Baveye PC. Movement of Cryptosporidium parvum oocysts through soils without preferential pathways: exploratory test. Front Environ Sci. 2017;5:39.
Khan A, Shaik JS, Grigg ME. Genomics and molecular epidemiology of Cryptosporidium species. Acta Trop. 2018;184:1–14.
Jones RC, Liberatore M, Fernandez JR, Gerber SI. Use of a prospective space-time scan statistic to prioritize shigellosis case investigations in an urban jurisdiction. Public Health Rep. 2006;121(2):133–9.
Acknowledgements
The authors would like to acknowledge the CIDR Review Committee for data acquisition and the Royal College of Physicians of Ireland (RCPI) Research Ethics Review Committee. The authors also wish to acknowledge the Irish Research Council (COALESCE Research Programme) and Irish Environmental Protection Agency (STRIVE Research Programme) for provision of research funding.
Funding
This work was funded by the Environmental Protection Agency (EPA) under the STRIVE Research Programme (2018-W-MS-33) and the Irish Research Council under the COALESCE Funding Programme (COALESCE/2019/53).
Author information
Authors and Affiliations
Contributions
MB: Methodology, software, validation, formal analysis, writing, preparation of Figures 1, 2, 3, 4, 5, 6, 7, 10, 11, 12, 13. EC: Preparation of Figs. 8, 9, Writing. CO: resources, data curation, writing—review and editing. PG: resources, data curation, writing—review and editing. PM: resources, data curation, writing—review and editing. JO: Conceptualization, supervision, funding acquisition, writing—review and editing. PH: conceptualization, supervision, funding acquisition, writing—review and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
With the exception of age, gender and minimal clinical data such as date of onset, no personal data, as defined by the Irish Health Research Regulations, were used for this research. The employed anonymisation protocol is considered equivalent to irreversible anonymisation, appropriate for release to academic researchers, as approved by the Irish Data Protection Commissioner, and as such, informed consent was considered unnecessary, as set out in the Research Ethical Approval documents provided by the Royal College of Physicians of Ireland, comprising both data usage and epidemiological methodologies employed. Additionally, the authors can confirm that all methods and analyses have been carried out in accordance with the International Ethical Guidelines for Epidemiological Studies as stipulated in the conditions of the aforementioned project Ethical Approval document.
Consent for publication
All authors consent with study submission for publication.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Appendix 1. Annual space-time clusters of Cryptosporidiosis in Ireland from 2008 to 2017; Appendix 2. Space-time clusters of Cryptosporidiosis in Ireland during 2008.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boudou, M., Cleary, E., ÓhAiseadha, C. et al. Spatiotemporal epidemiology of cryptosporidiosis in the Republic of Ireland, 2008–2017: development of a space–time “cluster recurrence” index. BMC Infect Dis 21, 880 (2021). https://doi.org/10.1186/s12879-021-06598-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06598-3