Abstract
Background
Tuberculosis is a serious public health problem worldwide. It is the leading cause of death amongst people living with HIV, and default from tuberculosis (TB) treatment in people living with HIV increases the probability of death. The aim of this study was to estimate the survival probability of people living with HIV who default treatment for TB compared to those who complete the treatment.
Methods
This was a longitudinal cohort study of people living with HIV, from June 2007 to December 2013 with two components: a retrospective (for those who started tuberculosis treatment before 2013 for whom failure (death) or censoring occurred before 2013), and prospective (those who started tuberculosis treatment at any time between 2007 and June 2013 and for whom death or censoring occurred after the beginning of 2013), at two referral hospitals for people living with HIV (Correia Picanço Hospital - HCP and at Hospital Universitário Oswaldo Cruz – HUOC), in Recife/PE. A total of 317 patients who initiated TB treatment were studied. Default from TB treatment was defined as any patient who failed to attend their pre-booked return appointment at the health center for more than 30 consecutive days, in accordance with Brazilian Ministry of Health recommendations.
Results
From a cohort of 2372 people living with HIV we analyzed 317 patients who had initiated TB treatment. The incidence of death was 5.6 deaths per 100 persons per year (CI 95% 4.5 to 7.08). Independent factors associated with death: default from TB treatment 3.65 HR (95% CI 2.28 to 5.83); CD4 < 200 cells/mm3 2.39 HR (95% CI 1.44 to 3.96); extrapulmonary tuberculosis 1.56 HR (95% CI 0.93 to 2.63); smoking 2.28 HR (95% CI 1.33 to 3.89); alcohol light 0.13 HR (95% CI 0.03 to 0.56).
Conclusion
The probability of death in people living with HIV who default TB treatment is approximately four times greater when compared to those who do not default from treatment.
Similar content being viewed by others
Background
Tuberculosis (TB) is a serious public health problem worldwide [1–3], and is the leading cause of morbidity and mortality in people living with HIV [4–7], who are 21 to 34 times more likely to develop TB when compared to those without HIV [2]. The pulmonary and extrapulmonary forms of tuberculosis are the most common opportunistic infections in people living with HIV [8, 9]. The interaction between Mycobacterium tuberculosis and HIV can cause elevation of viral load and decrease of CD4 + T lymphocytes count, leading to accelerated decline in the immune function and decreased survival [10] People living with HIV have been considered as being more likely to have unfavorable treatment outcomes of TB treatment, due to the complexity of the management of co-infection and to behavioral factors of this population [11]. Although almost all patients who receive TB treatment are cured, those living with HIV and undergoing concomitant treatment for HIV infection and TB present a number of challenges, amongst which are: the long duration of therapy, the dosing frequency, the potential complex drug interaction and toxicity of the two therapies [1, 12–14]. Therefore, numerous factors may influence the risk of defaulting TB treatment and death in HIV-infected individuals. Some authors found an association between defaulting from TB treatment and male sex, smoking, lymphocyte CD4 count <200 cells per mm3, low salaries, alcohol use, previous default from TB treatment, age of 35–49 years old, illiteracy and previous treatment for TB [15–18] Tuberculosis is the leading cause of death in people living with HIV, causing a great impact on the survival of this population. In turn, default from treatment features amongst the leading causes of TB treatment failure in people living with HIV, and may therefore be associated with a higher mortality rate within this group [7, 15, 19]. This aim of this study was to compare the survival probability of people living with HIV who defaulted treatment for TB with those who did not default treatment.
Methods
This study is nested in the AIDS Cohort of the state of Pernambuco (Cohort AIDS-PE), a clinical cohort that has collected information of more than 2300 patients with HIV/AIDS attending two reference centers for the care of HIV/AIDS patients in Recife, Brazil. The study design was a longitudinal cohort with two components: retrospective, (June 2007 to December 2012) and prospective (January 2013 to December 2013). As we started this investigation in the beginning of 2013, people living with HIV who started tuberculosis treatment before 2013 and for whom failure (death) or censoring occurred before 2013, the study was retrospective. For those who started tuberculosis treatment at any time between June 2007 and June 2013 and for whom death or censoring occurred after the beginning of 2013, the study was prospective. The same selection procedures were used in the retrospective and prospective arm of the study. Patients attending two reference centers for the treatment of HIV (Hospital Correia Picanço and Hospital Universitário Oswaldo Cruz) were enrolled in the study at the time they were notified to the Surveillance System for Infectious Diseases (SINAN/MS) as having tuberculosis. Registering the case in the SINAN/MS is a prerequisite for initiation of TB treatment. They were then invited to participate in the study and after reading and signing the Informed Consent (IC) forms, they were interviewed by previously trained staff using a standardized questionnaire. Recruitment loss ocurred when the patient was notified to the Surveillance System for Infectious Diseases (SINAN/MS) as having tuberculosis but was not included in the study. Recruitment loss occurred in the retrospective arm (n = 182) as well as in the prospective (n = 10).
The study population consisted of people living with HIV aged 18 and over who had initiated treatment for TB. In our study TB cases were considered as those diagnosed of TB by the attending physician (according to the Ministry of Health of Brazil guidelines, that is based on clinical findings, direct investigation of Acid-fast bacillus –AFB -smear and culture for M.tb).and notified to the (SINAN/MS). Default from TB treatment was defined as any patient who failed to attend their pre-booked return appointment at the health center for more than 30 consecutive days. The study excluded individuals who presented any change in the diagnosis of TB during follow-up, those with multidrug-resistant TB (MDR-TB) and pregnant women. The response variable of the study was the occurrence of all-cause mortality. Information on the occurrence of death was obtained from medical records and from the Mortality Information System, ascertained through record linkage. Death registration is compulsory in Brazil. There is no burial without a death certificate and the death certificate is the source of information to the mortality system. The Mortality Information System is a national and sub-national electronic system with all routine mortality data coded to International Coding Disease. Registration of deaths is managed by the Ministry of Health in Brazil.
The main exposure was the default from treatment for TB. Patients were classified as defaulters or non defaulters. Defaulters were further classified according to the moment in which default ocurred (first quarter: meaning the first three months after the start of tuberculosis treatment and the second quarter meaning four to six months after the start of tuberculosis treatment).
Co-variables were grouped into six categories: biological variables (gender and age); variables related to habits and lifestyle (smoking and drinking); socioeconomic factors (income, place of residence and marital status); clinical variables (body mass index [BMI] and anemia); HIV-related variables (presence of opportunistic infection, AIDS case, CD4 count and antiretroviral therapy [ART]); variables related to tuberculosis (place of treatment, form of TB and previous treatment). Amongst the lifestyle variables, smoking was considered as the habit of cigarette smoking and categorized as: non-smokers (those who had never smoked during their lifetime); former smokers (those who had given up smoking at least six months prior to enrolling on the study); smokers (those who were smoking at the time of enrollment or had stopped smoking during the previous six months). Alcohol consumption was regarded as consuming alcoholic beverages and categorized as: abstainer (has never drunk or drinks less than 8 units/year); light drinker (drinks twice a week, at maximum, not exceeding 10 units/month); moderate drinker (drinks at least 3 or 4 times per week, exceeding 5 units/day); heavy drinker (undergoing treatment for alcoholism). The CD4+ count was considered as that observed at the time of initiating TB treatment and categorized as: greater than or equal to 200 cells/mm3 and less than 200 cells/mm3. The clinical form of TB was defined as the organ or tissue affected by the disease and categorized as: pulmonary TB (disease restricted to the lungs); extrapulmonary TB (when the disease involved organs other than the lungs); disseminated TB (involvement of two non-contiguous sites).
Statistical analysis
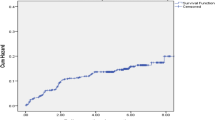
For the data analysis, we considered the alpha level = 5% and a confidence interval (CI) of 95%. In the survival analysis, the Kaplan-Meier method was used to compare the probability of survival between those who defaulted from tuberculosis treatment and those who did not and the median survival time, and the log-rank test to test the statistical significance of the difference between the curves and compare survival curves. The death rate was expressed in person/years; time was measured since the start of tuberculosis treatment until death or failure. The semi-parametric regression Cox model was adopted to identify factors associated with survival time, in which the hazard ratio [HR] was used as the measurement of association. The association between default from tuberculosis treatment and death was adjusted for confounding factors. Deaths were identified by pairing individuals from the cohort during the follow-up period and the Mortality Information System of Pernambuco (SIM-PE), using the probabilistic linkage program RecLink III [20]. For the statistical analysis in the survival model we used STATA 12.0. The data entry and double entry validation were performed in parallel with data collection, and the database was managed by the SQL Server 2000 (Microsoft), using GeneXus software (version 7.5).
Ethical considerations
The study was approved by the Research Ethics Committee at HUOC/PROCAPE/UPE on 02/07/2014, Report n°: 706. 132/CAAE: 30621114.8.0000.5192 and by the Ethics Committee of the Universidade Federal de Pernambuco, registered in the National System on Research Ethics (SISNEP) FR-067 159/CAAE-0004.1.172.106-05/REGISTRATION CEP/Health Sciences Center/Universidade Federal de Pernambuco (UFPE) Report n° 254/05 and funded by the Ministry of Health and Ministry of Science and Technology - CNPq/MS-SCTIE-DECIT (Case 10567/2006-0).
Results
Out of 512 people living with HIV who initiated tuberculosis treatment, 317 were included in the study. Losses occurred because of: recruitment loss (n = 182, retrospective arm = 170 and prospective arm = 12), change in diagnosis (n = 5), not signing informed consent forms (n = 5) and loss to followup (n = 3). Of the 317 patients studied, 91 (28.7%) defaulted treatment for TB, while 226 (70.9%) did not (Fig. 1). A total of 59 individuals underwent further treatment for TB during follow-up, and contributed more than once to the cohort, thus resulting in a total of 375 treatment episodes for the entire cohort. From amongst these, there were 111defaults from TB treatment (29.6%) (Table 1), 47 (42.7%) during the first three months after the start of TB treatment and 63 (57.3%) between the fourth and sixth month after the start of TB treatment; the date of default of one patient was not recorded. From the 317 patients studied, 75 (23.6%) deaths were recorded during the study period. (Table 1) In the first year of follow-up there were 14 deaths (18.6%), in the second there were 25 (33.3%) and in the third year 36 (48%). Amongst the cases of death, 36 (48%) occurred in the group that did not default TB treatment, 20 (26.7%) in the group that defaulted treatment in the first quarter and 19 (25.3%) in the group that defaulted treatment in the second quarter. In the group that did not default treatment, 38.9% of the deaths occurred within two years of initiating treatment for TB, while the percentages of death for those who defaulted treatment in the first and second quarter were, respectively, 70% and 57.9%. (Table 2) The death rate amongst patients who defaulted TB treatment was 14.4 deaths per 100 person/years (95% CI: 10.5 to 19.7) and among patients who did not default treatment 3.4 deaths per 100 person/years (95% CI: 2.46 to 4.72) (Fig. 2). The probability of death for patients who defaulted treatment was 3.91 times greater (95% CI: 2.48 to 6.17) when compared to those who did not default treatment. Moreover, the probability of death was higher in those who defaulted from treatment early (Fig. 2).
In the univariate analysis, the following variables were significantly associated with death: age (30–49 years) (Table 3), heavy/dependent alcohol consumption and smoking (Table 4), a CD4 count <200 cells/mm3 (Table 5). In addition to treatment default, a CD4 count <200 cells/mm3, smoking, extrapulmonary TB and alcohol consumption all remained in the final model. (Table 6) Information on sputum smear was not available for 16.3% of the TB treatments; for those with available information, the percentage of TB treatments which had started with a positive sputum smear was 14.0%. Mortality was higher among those with a negative sputum smear (HR = 2.1, 95%-CI = 0.9–4.7, p = 0.075) than in those with a positive result. The probability of death was greater for defaulters in the the group with positive sputum smear (HR = 2.38, 95%-CI = 0.53–10.79), though it did not reach statistical significance; in the group with negative (HR = 3.74, 95%-CI = 1.88–7.46) and among those who did not have the sputum smear performed (HR = 3.30, 95%-CI = 1.63–6.67). We compared the group of patients not enrolled because they were not contactable by the researchers (n = 182) with the group of patients included in the study (n = 317) in relation to sex, age and default rate. The two groups were similar in relation to age and sex but the default rate was higher among those enrolled in the study.
Discussion
The probability of death amongst people living with HIV who defaulted treatment for TB was almost four times greater than in those who did not. In addition, there was an independent association of death and CD4 count <200 cells/mm3, extrapulmonary TB and smoking. Light alcohol consumption was found to be a protective factor for death.
The study of risk factors for the default from TB treatment was well documented in a study by Maruza 2011, but there are few studies that have focused on the association between treatment default and death [18, 19, 21]. Moreover, we were unable to identify in the literature other studies that have addressed this topic in people living with HIV. In the present study we observed that the highest frequency of defaulting treatment occurred during the first quarter, which corroborates the work of several authors [16, 19, 21]. It is possible that patients present with some clinical improvement during this initial phase of treatment, and therefore the default rate is higher [16, 22]. However, early default is compatible with a lower chance of curing TB, with the risk of death being higher in the group of patients who defaulted treatment earlier (Q1) [21]. In the present study, deaths occurred at different moments in time (36% after 2 years), suggesting that the deaths may have occurred either due to the progression of TB or by the impact of a more prolonged duration of TB on the progression of HIV infection. Persistent infections, such as TB, may increase the patient’s viral load, which leads to a compromised immune function, lowering survival rates and increasing the chance of transmitting the HIV virus [10]. A high viral load may lead to a decrease in the CD4 count, through different mechanisms: accelerating cell loss induced by lysis of the virus or by destroying both healthy and infected cells, or even triggering apoptosis (cell death) of both healthy and infected cells [23]. In the present study it was observed that patients with a CD4 count of less than 200cells/mm3 presented a more than two-fold probability of death. This finding is in accordance with that described by other authors [13, 15, 24, 25] The CD4 cell count is a strong predictor for the progression of Human Immunodeficiency Virus - HIV [26] and patient survival. [27] Individuals with extrapulmonary TB presented a higher probability of death (borderline significance), which is in agreement with other studies. [28, 29] This association was explained by Kingkaew as being due to a delay in diagnosing this form of TB, for which there is a need to conduct more sophisticated tests in order to complete the diagnosis, which may delay initiation of treatment and thus jeopardize patient survival [29]. In the present study, it was observed that smoking presented a two-fold increase in the probability of death. This association has also been described by other authors [30, 31] and is attributed to a change in the structure and functioning of the lungs, as well as a decrease in immunity at both local and systemic levels [31]. Contrary to many studies, we found that light alcohol consumption was a protective factor for death, which is contrary to the findings of other studies that indicate an independent association between alcohol consumption and death [18, 32]. Perhaps light alcohol consumption encountered in our study as a protective factor for death signifies that light alcohol consumption is only a marker for improved conditions of health, and that this status in itself is a protective factor for death. The probability of death was higher in patients who were not using HAART but the difference did not reach statistical significance (p = 0.351), differing from a previou paper of our group [33]. It should be emphasized that most of the patients (81.1%) were using HAART. This study presented some limitations: the recruitment of patients to the study was uneven in the two reference services. Approximately two thirds of the study population was selected from Hospital Correia Picanço. This was due to logistical issues, as the fieldwork team was larger in this hospital. However, we do not believe that it may have nfluenced the association between treatment default and death. Another limitation was the exclusion of 192 patients for loss of recruitment, i.e., patients who started treatment for TB but were not included in the study. However, the exclusion of potentially eligible individuals was not due to any specific criterion and therefore it is unlikely that their absence distorted our results. In fact, for those patients (recruitment loss) it was possible to retrieve some information either from the SINAN or from the dataset of the Cohort AIDS PE and thus to compare patients enrolled and patients eligible but not enrolled. The two groups were similar in relation to age and sex but the default rate was higher among those enrolled in the study (data not shown). Although the default rate may have been overestimated we have no reason to think the association between default from TB treatment and death would differ in the two groups. As only 14.01% of the TB treatments started with a positive sputum smear, there may have been some misdiagnosis, i.e., some individuals without TB may have been classified as with TB However, it should be emphasized that professionals from both reference services have extensive experience in the diagnosis and treatment of tuberculosis, patients were followed until the end of tuberculosis treatment and patients for whom there was a change in the diagnosis of tuberculosis were excluded. The probability of death was greater for defaulters in the group with a positive, negative, or not performed sputum smear.
Conclusion
The present study demonstrated an association between treatment default and death, with a higher probability of death when treatment was defaulted at an early stage. It is necessary to conduct further studies in order to assess the manner in which defaulting TB treatment affects the dynamics of the CD4 count over time, and the resulting effects of this dynamic on death. It would also be appropriate to compare the deaths that occur as a direct consequence of TB (TB death) with those that occur due to the impact of TB on the development of HIV/AIDS.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- ART:
-
Antiretroviral therapy
- BMI:
-
Body mass index
- CD4:
-
Count linfocits T CD4
- CI:
-
Confidence interval
- CNPq:
-
Conselho Nacional de Desenvolvimento Científico e Tecnológico
- DST:
-
Sexually transmitted disease
- HCP:
-
Hospital Correia Picanço
- HIV:
-
Human Immunodeficiency virus
- HR:
-
Hazard ratio
- HUOC:
-
Hospital Univesitário Oswaldo Cruz
- IC:
-
Inform Consent
- MDR-TB:
-
Multidrug-resistant TB
- MS:
-
Ministry of Health
- PE:
-
Pernambuco
- PLHIV:
-
Peolpe living with HIV
- PROCAPE:
-
Pronto Socorro Cardiológico de PE
- RECLINK:
-
Probabilistic linkage program
- SIM:
-
Mortality information system
- SISNEP:
-
National system on research ethics
- STATA:
-
Data analysis and statistical software
- TB:
-
Tuberculosis
- UFPE:
-
Universidade Federal de Pernambuco
- UNESCO:
-
United Nations Educational, Scientific and Cultural Organization
- UPE:
-
Universidade de Pernambuco
References
World Health Organization. Global tuberculosis report 2014. Geneva: WHO; 2014.
World Health Organization. WHO news release. Saudi Med J. 2013;34(11):1205–7.
World Health Organization. Global tuberculosis report 2013. Geneva: WHO; 2013.
Schmaltz CAS, Santoro-Lopes G, Lourenço MC, Morgado MG, Velasque LDS, Rolla VC. Factors impacting early mortality in tuberculosis/HIV patients: differences between subjects naïve to and previously started on HAART. PLoS One. 2012;7(9):e45704.
Naidoo P, Peltzer K, Louw J, Matseke G, Mchunu G, Tushana B. Predictors of tuberculosis (TB) and antiretroviral (ARV) medication non-adherence in public primary care patients in South Africa: a cross sectional study. BMC Public Health. 2013;13:396.
Yuen CM, Weyenga HO, Kim AA, Malika T, Muttai H, Katana A, et al. Comparison of trends in tuberculosis incidence among adults living with HIV and adults without HIV - Kenya, 1998–2012. PLoS One. 2014;9(6):e99880.
Domingos M, Caiaffa W, Colosimo E. Mortality, TB/HIV co-infection, and treatment dropout: predictors of tuberculosis prognosis in Recife, Pernambuco State, Brazil. Cad Saúde Pública. 2008;24(4):887–96.
Geldmacher C, Ngwenyama N, Schuetz A, Petrovas C, Reither K, Heeregrave EJ, et al. Preferential infection and depletion of Mycobacterium tuberculosisspecific CD4 T cells after HIV-1 infection. J Exp Med. 2010;207(13):2869–81.
Ministério da Saúde Brasil.Secretária -Executiva.Subsecretaria de Assuntos Administrativos Coordenaçào Geral de Documentação e Informação, Editorial C de G, organizadores. Ministério da Saúde. Secretária Executiva. Recomendações para o Manejo da co-infecção TB-HIV em Serviços de Atenção Especializada a pessoas vivendo com HIV/Aids. Ministério da Saúde. Secretaria-Executiva – Brasília. MS. 2013.
Lawn SD. AIDS in Africa: the impact of coinfections on the pathogenesis of HIV-1 infection. J Infect. 2004;48:1–12.
Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim Epidemiológico Especial Tuberculose. Brasil - MS, 2012. v.43.
Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Global Report 2013.
Grinsztejn B, Veloso V, Friedman R, Moreira R, Luz P, Campos D, et al. Early mortality and cause of deaths in patients using HAART in Brazil and the United States. AIDS. 2013;23(16):2107–14.
Rodrigues AM, Scatena M, Helena S, Vendramini F, Marin SR, Canini S, et al. Avaliação do acesso ao tratamento de tuberculose por coinfectados ou não pelo vírus da imunodeficiência humana. Rev Esc Enferm USP. 2012;46(5):1163–9.
Maruza M, Albuquerque MFPM, Coimbra I, Moura LV, Montarroyos UR, Miranda Filho DB, et al. Risk factors for default from tuberculosis treatment in HIV-infected individuals in the state of Pernambuco, Brazil: a prospective cohort study. BMC Infect Dis. 2011;11:351.
Muture B, Keraka M, Kimuu P, Karibu E, Ombeka V, Oguya F. Factors associated with default from treatment among tuberculosis patients in Nairobi province, Kenya: a case control study. BMC Public Health. 2011;11(696):1–10.
Zhang Q, Gaafer M, El Bayoumy I. Determinants of default from pulmonary tuberculosis treatment in Kuwait. Sci World J. 2014;14:672825.
Albuquerque M, Ximenes R, Silva N, Souza W, Dantas A, Dantas O, et al. Factors associated with treatment failure, dropout, and death in a cohort of tuberculosis patients in Recife, Pernambuco State, Brazil. Cad Saúde Pública. 2007;23(7):1573–82.
Vree M, Huong NT, Duong BD, Sy DN, Van LN, Co NV, et al. Mortality and failure among tuberculosis patients who did not complete treatment in Vietnam: a cohort study. BMC Public Health. 2007;7:134.
Medina, Claudia & Rochel, Kenneth. RecLink III – Relacionamento Probabilístico de Registros. Versão 3.1.6.3160. 2007.
Alobu I, Oshi SN, Oshi DC, Ukwaja KN. Risk factors of treatment default and death among tuberculosis patients in a resource-limited setting. Asian Pac J Trop Med. 2014;7:977–84.
Kaona FAD, Tuba M, Siziya S, Sikaona L. An assessment of factors contributing to treatment adherence and knowledge of TB transmission among patients on TB treatment. BMC Public Health. 2004;4:68.
Lawn SD, Butera ST, Folks TM. Contribution of immune activation to the pathogenesis and transmission of human immunodeficiency virus type 1 infection. Clin Microbiol Rev. 2001;14(4):753–77.
Karo B, Haas W, Kollan C, Gunsenheimer-Bartmeyer B, Hamouda O, Fiebig L. Tuberculosis among people living with HIV/AIDS in the German ClinSurv HIV Cohort: long-term incidence and risk factors. BMC Infect Dis. 2014;14(1):1–12.
Lawn SD, Myer L, Bekker L-G, Wood R. Burden of tuberculosis in an antiretroviral treatment programme in sub-Saharan Africa: impact on treatment outcomes and implications for tuberculosis control. AIDS. 2006;20:1605–12.
Hoffman J, Van Griensven J, Colebunders R, McKellar M. Role of the CD4 count in HIV management. HIV Ther. 2010;4(1):27–39.
Langford SE, Ananworanich J, Cooper DA. Predictors of disease progression in HIV infection: a review. AIDS Res Ther. 2007;4(11):1–14.
Oshi DC, Oshi SN, Alobu I, Ukwaja KN. Profile, outcomes, and determinants of unsuccessful tuberculosis treatment outcomes among HIV-infected tuberculosis patients in a Nigerian State. 2015. p. 2014.
Kingkaew N, Sangtong B, Amnuaiphon W, Jongpaibulpatana J, Mankatittham W, Akksilp S, et al. HIV-associated extrapulmonary tuberculosis in Thailand: epidemiology and risk factors for death. Int J Infect Dis. 2009;13(6):722–9.
Reed GW, Choi H, Lee SY, Lee M, Kim Y, Park H, et al. Impact of diabetes and smoking on mortality in tuberculosis. PLoS One. 2013;8(2):e58044.
Jee S, Golub J, Jo J, Park I, Ohrr H, Samet J. Smoking and risk of tuberculosis incidence, mortality, and recurrence in South Korean men and women. Am J Epidemiol. 2009;170(12):1478–85.
Volkmann T, Moonan PK, Miramontes R, Oeltmann JE. Tuberculosis and excess alcohol use in the United States. Int J Tuberc Lung Dis. 2015;19(1):111–119.
Maruza M, Albuquerque MFPM, Braga MC, Barbosa MTS, Byington R, Coimbra I, et al. Survival of HIV-infected patients after starting tuberculosis treatment: a prospective cohort study. Int J Tuberc Lung Dis. 2012;16:618–24.
Acknowledgements
None.
Funding
This research was funded by Ministério da Saúde/Programa DST/AIDS/UNESCO (CSV 182/06 - Projeto “Estudo Clínico-Epidemiológico da co-infecção HIV/Tuberculose em Recife”). The authors received partial support from the Conselho Nacional de Desenvolvimento Científico e Tecnológico - CNPq (Scholarship 305934/2012-0 to H.R.L., 308818/2013-0 to R.A.A.X., 236603/2012-4 to D.B.M.F. and 308491/2013-0 to M.F.P.M.).
Availability of data and materials
We do not wish to share the data at this moment because it is being used for other analysis. The data may be provided upon request.
Authors’ contributions
RGC, RAAX, MM and IC gave substantial contributions to the conception or design of the work, interpretation of data, drafting and revising the work; MFPMA, DBMF, HRL, and URM contributed to the design of the work, acquisition and interpretation of the data and revising it critically; URM and RGC conducted the data analysis; all authors approved the final version to be published.
Competing interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee at HUOC/PROCAPE/UPE on 02/07/2014, Report n°: 706. 132/CAAE: 30621114.8.0000.5192 and by the Ethics Committee of the Universidade Federal de Pernambuco, registered in the National System on Research Ethics (SISNEP) FR-067 159/CAAE-0004.1.172.106-05/REGISTRATION CEP/Health Sciences Center/Universidade Federal de Pernambuco (UFPE). Partipants provided written informed consente.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cunha, R., Maruza, M., Montarroyos, U. et al. Survival of people living with HIV who defaulted from tuberculosis treatment in a cohort, Recife, Brazil. BMC Infect Dis 17, 137 (2017). https://doi.org/10.1186/s12879-016-2127-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-016-2127-5