Abstract
Objective
Research the dose–response relationship between overall and certain types of exercise and cognitive function in older adults with Alzheimer's disease and dementia.
Design
Systemic and Bayesian Model-Based Network Meta-Analysis.
Methods
In our study, we analyzed data from randomized controlled trials investigating the effects of different exercises on cognitive outcomes in older adults with AD. We searched the Web of Science, PubMed, Cochrane Central Register of Controlled Trials, and Embase up to November 2023. Using the Cochrane Risk of Bias tool (Rob2) for quality assessment and R software with the MBNMA package for data analysis, we determined standard mean differences (SMDs) and 95% confidence intervals (95%CrI) to evaluate exercise's impact on cognitive function in AD.
Results
Twenty-seven studies with 2,242 AD patients revealed a nonlinear relationship between exercise and cognitive improvement in AD patients. We observed significant cognitive enhancements at an effective exercise dose of up to 1000 METs-min/week (SMDs: 0.535, SD: 0.269, 95% CrI: 0.023 to 1.092). The optimal dose was found to be 650 METs-min/week (SMDs: 0.691, SD: 0.169, 95% CrI: 0.373 to 1.039), with AE (Aerobic exercise) being particularly effective. For AE, the optimal cognitive enhancement dose was determined to be 660 METs-min/week (SMDs: 0.909, SD: 0.219, 95% CrI: 0.495 to 1.362).
Conclusion
Nonlinear dose–response relationship between exercise and cognitive improvement in Alzheimer’s disease, with the optimal AE dose identified at 660 METs-min/week for enhancing cognitive function in AD.
Similar content being viewed by others
Introduction
According to a recent report in 2023, the number of people with Alzheimer's in the United States alone has skyrocketed to 6.75 million and is projected to exceed 13.8 million by 2026 [1]. Alzheimer's dementia has become one of the prominent public health challenges of the twenty-first century [2]. At the same time, the enormous cost of Alzheimer's disease and dementia(AD) puts a huge strain on society and families, with studies showing that [3]: According to estimates made in 2019, the global annual societal cost of dementia was US$131.34 billion for 55.2 million people living with dementia. This equates to a cost of US$23,796 per person with dementia. Out of this amount, direct medical costs amounted to US$213.2 billion (16%), direct social sector costs (including long-term care) to US$448.7 billion (34%), and informal care costs to US$651.4 billion (50%). Moreover, in low- and middle-income countries, family caregivers of people with dementia face high levels of caregiving stress, adverse health effects of long-term care, and difficulties in managing the caregiving process. They also struggle to adapt to life changes and meet their own needs [4].
In the previous study, a comprehensive meta-analysis synthesizing findings from 43 prospective observational studies and 153 randomized controlled trials, Yu et al. established exercise as an effective intervention for preventing AD in older adults [5]. This conclusion is supported by similarities between animal models and human AD, including amyloid-beta deposition and tau protein pathology. Animal studies have further validated exercise's molecular basis for cognitive enhancement in AD, demonstrating its impact on reducing beta-amyloid deposition and improving cerebrovascular function [6, 7]. Additionally, a recent study by Holstein et al. in 'Nature Neuroscience' highlighted that exercise enhances brain health by increasing blood flow and promoting the circulation of cerebrospinal fluid [8]. Collectively, these findings underscore the role of regular exercise in boosting neurotrophic factor expression, exerting anti-inflammatory effects, and improving cognitive function and neuroplasticity.
However, different exercises have different effects on improving cognition in AD. Susana et. al. of the meta-analysis showed that aerobic exercise seems to significantly improve AD patients’ cognition [9]. Although studies have proven that aerobic exercise can improve the cognitive function of AD patients, the results of the network meta-analysis study by Shi et.al showed that resistance exercise was the most effective way to improve the cognitive function of AD patients [10]. In previous dose–response meta-analyses, the effects associated with resistance exercise on healthy older adults had yielded good insights [11, 12]. Additionally, the dose and response network meta of Daniel et. al. opened a new direction in the study of dose–response relationships and confirmed for the first time that the relationship between exercise dose and cognition in older adults was nonlinear and found older adults can achieve clinically meaningful benefits at doses lower than the WHO (724 METs-min per week) [13]. The varying effectiveness of exercise interventions on cognitive function in AD patients may largely be due to differences in exercise dosages. Previous dose–response studies often treated exercises within the same category as equivalent, regardless of their duration (e.g., equating a 40-min session with a 100-min session). Such an approach may overlook the distinct advantages of specific exercise types. For instance, it might ignore the benefits of strength training on bone density and metabolic rate or the cardiovascular benefits inherent to aerobic exercise [12, 14,15,16]. Moreover, the reliance on single-category dose–response modeling has made it challenging to accurately model the effects of different interventions. Additionally, while much of the existing research has focused on mild cognitive impairment a precursor to AD there has been a significant gap in studies specifically exploring the optimal exercise dosage and its impact on cognitive function in AD patients. Our study aims to fill this gap by providing nuanced insights into how different exercise doses can uniquely contribute to health outcomes in AD patients, representing a vital advancement in the field.
In order to fill the gap, our study follows the method used by Daniel et. al. to evaluate exercise intensity using task metabolic equivalents [13]. By utilizing a new dose–response model of network meta-analysis through a classical Bayesian prior theory model in probability [17, 18]. Our research meticulously evaluates existing randomized controlled trials on exercise interventions designed to enhance cognitive functions in AD. It delves into the nuanced, non-linear dynamics between the intensity and volume of exercise and the observed cognitive benefits. The study's core objective is to pinpoint the most effective exercise modalities for AD patients, alongside determining the optimal dosage for maximum cognitive improvement. This investigation is poised to substantially enrich evidence-based guidelines for exercise in managing cognitive symptoms of AD, thereby equipping healthcare professionals with robust data to inform their clinical decisions.
Method
Search strategy
This systematic review and network meta-analysis is registered on the international Prospective Register of Systematic Reviews site as CRD 42023484877, and it was reported following the PRISMA checklist [19]. We conducted a comprehensive literature search across Web of Science, PubMed, Cochrane Central Register of Controlled Trials, and Embase databases up to November 2023. To ensure the search was both thorough and precise, we crafted a strategy using medical subject headings (MeSH) and keyword searches specifically in PubMed, with three authors reviewing for accuracy and completeness. Our search utilized a combination of MeSH terms and synonyms including "Alzheimer”," "Dementia," "Aged," "Older adults," "Aging," "Cognitive impairment," and terms related to exercise such as "Physical Activity," "Exercise," "Training," "Resistance Exercise," and "Aerobic Exercise." We explicitly excluded studies on Mild Cognitive Impairment (MCI) using the term "NOT (MCI, Mild Cognitive Impairment)." Detailed search strategies, including the specific terms, dates, and methodologies employed, are documented in Appendix File 1.
Study selection
We first imported the literature we retrieved into the Endnote 20 software (Clarivate Analytics, Philadelphia, PA, USA) to screen for duplicate articles. We also manually screened for duplicates. Secondly, we excluded animal experiments, conference abstracts, experimental protocols, guidelines, and reports, as well as non-English literature. Finally, we meticulously screened for and excluded reviews and meta-analyses to guarantee that our study exclusively incorporated RCTs. Title/abstract and full-text screening were conducted independently and in duplicate by two investigators (Y.Y/X.F.H), with disagreements resolved by discussion or adjudication by a third author (Yang. Y).
Eligibility criteria
Types of participants
Participants must be diagnosed with AD and meet age criteria for older adults 65 years and older. Secondly, only studies focusing on cognitive impairment in healthy older adults and subjects clinically diagnosed with Mild cognitive impairment (MCI) were excluded. Furthermore, we also excluded studies of cognitive impairment due to other diseases (e.g. Parkinson's, stroke, diabetes, Attention Deficit/Hyperactivity Disorder, Epilepsy, Multiple Sclerosis, Autism, or Schizophrenia, etc.) and to ensure completely that the study looked at populations with AD.
Types of intervention
Previous research exercises had focused on increasing planned, structured activities. However, activities like gardening, daily tasks, household chores, and others with low task metabolic equivalents (METs, used to assess the intensity of exercise) do not result in muscle contraction sufficient to increase the body's calorie demand significantly. Therefore, it is challenging to make reasonable recommendations regarding appropriate exercise doses for AD [20].
In our study, both the intervention and control groups engaged in some form of physical activity. However, to be included in our intervention analysis, studies needed to specify the duration, frequency, and methods of exercise, quantifiable in METs. This research focused exclusively on the impact of exercise on cognitive impairment in AD, omitting studies that incorporated other interventions such as exercise combined with cognitive therapy, gardening, music therapy, or physiotherapy. This exclusion criterion was essential to isolate the cognitive benefits attributable solely to physical exercise. Moreover, the control group received standard care, including daily living guidance and health education, without additional exercise or specific health interventions. A comprehensive definition of the exercise interventions analyzed is available in Appendix File 9.
Types of outcome measures
In our studies, experiments that reported at least one outcome with one of the global cognitive measures were eligible for inclusion. (ex: MMSE [21], ADAS-Cog [22], MoCA [23]).
Types of studies
In order to keep the risk of bias at a low to moderate level, both published and unpublished randomized controlled trials (RCTs) were included in our study, whereas non-randomized controlled studies (cohort studies, pathology-control, cross-sectional studies, etc.) were excluded.
Data extraction3
The data from studies that met the inclusion criteria (Y.Y/X.F.H) were extracted independently by two authors and disagreements were resolved by consensus among the third authors (Yang. Y). For each inclusion study, pertinent data and populated into an Excel spreadsheet. the researcher's name, published year of study, sample size (total/male/female), sex, age, intervention and control description, intervention period/frequency/minutes, cognitive assessment tool, and used transformation formulas for estimating the mean and standard deviation (Appendix file 2) any data that could be used to calculate effect size was extracted (Appendix file 3). The formulas utilized for the calculation of Mean change and SD values were:
According to the guidelines of the Cochrane Handbook, the correlation coefficient (Corr) was set to 0.5 [24]. In addition to meeting the data analysis requirements of the Dose–Response network meta-analysis Package in R, we converted the standard errors (SE). n as sample size [25].
In cases where the required data for dose–response meta-analyses could not be retrieved from published reports, we contacted the authors and requested additional data. In two studies, the authors were able to provide the required data after being contacted [26, 27].
Data setting
First, the interventions were coded in two categories; Category I: the intervention and control groups were coded as "Exercise (PA)" and "Control (CON)". Exercise will be viewed as an overall equivalent (e.g., regardless of aerobic, anaerobic, exercise, etc.), with the aim of analyzing the optimal dose of overall exercise for AD patients. Category II: Interventions will be coded according to their primary form of PA: “Aerobic exercise” (AE), “Mixed exercise” (MIX), "Tai Chi” (TC), “Resistance training” (RT), “Exergame” (EX) and “control” (CON). The aim was to analyze the optimal dose and optimal modality of the different forms of exercise. At the same time, we chose metabolic equivalents of tasks (METs) to define exercise-specific energy expenditure [28]. Because METs provide a standardized way to quantify the intensity of different exercises. By measuring energy expenditure in terms of METs, the intensity of various sports and physical activities can be objectively compared, regardless of the type of activity or the individual performing the activity [29]. Not only, by calculating METs-min consumed per week, our study took into account not only the duration and frequency of exercise (METs-min/week = duration minute × times-pre week × MET value) but also the intensity of exercise, which is critical to assess its impact on health outcomes [20, 30, 31]. Additionally, in order to facilitate the connectivity required for Network Meta-analysis, the intervention intensity was classified into five different groups with weekly controls set at 0,250, 500, 750,1000, and 1250 METs-min and it’s proved in the previous study [32, 33].
Data synthesis
All data analysis was performed in R version 4.0.3 [34]. We used the "MBNMAdose" package to analyze the reticulation dose–response relationship which exercise dose and AD cognition impairment [17, 35]. We used the Emax functional model, restricted cubic spline, non-parametric model, exponential model different fitting metrics for random and fixed effects models to select the best-fitting model for analyzing our study data. such as DIC (deviation information criterion), standard deviation, parameters in the model, and residuals [36]. With the results (Appendix File 5 Table 2), the restricted cubic spline model of the random effects model was found to have a better fit. Therefore, in our study, we opted restricted cubic spline of the random effects model [18, 37, 38]. In addition, to visualize the best functional model fit to our data, we plotted relative line and box plots of the deviation of equivalent exercises from different exercises in Appendix File 5.
At the same time, we checked the data for three key hypotheses of network meta-analysis network connectivity, consistency (Appendix Table 1)., and transitivity (Appendix 4: Figure, 4) [37, 39, 40]. Additionally, because included studies assessed cognitive function using different measurement scales, effect measures were pooled as standardized mean differences (SMDs), SMDs do not rely on the specific units of the original scale and therefore can be used to combine results from studies that use different measurement units and ranges, eliminating interpretation barriers that may arise when using raw score differences directly, meanwhile with 95% credible intervals (95% CrI) to assess the credibility of our estimates [41, 42].
In order to estimate the overall and different exercise doses that resulted in the predicted maximum significant effect referred to as the ‘optimal exercise dose’. We summarized the result of the dose–response relationship by the MCMC model (Markov Chain Monte Carlo Iterations) [3 chains, 20,000 iterations each (first 10,000 discarded), n. thin = 10] of the beta coefficients on the restricted cubic spline curves by “rjags” package in R [43]. We positioned the three nodes at the 10th, 50th, and 90th percentile of the exercise dose to visualize our model-fitting results. The code to reproduce the results presented in this paper can be accessed at the first author's e-mail address.
Risk of bias and quality of evidence
Our study was selected according to the Cochrane (Rob2) criteria [44,45,46]. and packages “robvis” was used to plot the results in R. Three reviewers (Y.Y/X.F.H/Yang. Y) assessed the study, we assessed only five categories of risk of bias, including randomized sequence generation, bias due to deviation from the intended intervention, incomplete data, bias in measurements, and selective bias in reporting results. Disagreements were resolved by the third author. Additionally, we performed sensitivity analyses and excluded high-risk bias studies to determine the robustness of the overall exercise dose–response model [47] (Appendix File 8).
Results
Description of included studies
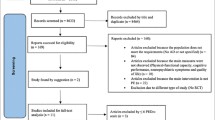
A total of 1962 potentially eligible studies were searched. After removing literature that did not fit my study by title, abstract, etc., we considered 147 studies that were potentially eligible for inclusion and retrieved full-text articles. After deleting duplicates and applying the inclusion criteria, there were 27 RCT studies [26, 27, 48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72] included in this analysis were published between 2006 and 2023 (Fig. 1). Out of the total of 2242 participants, 1210 (54%) were male and 1032 (46%) were female. All patients included in the studies had AD and were aged between 65 and 85 years old. In these studies, the exercise interventions in the 17 studies have AE, 8 studies have Mixed, 3 studies have RT, 3 studies have Taiichi and 2 studies were game-based exercise interventions and we provided Characteristics information for the included study in Table 1. More information about the characteristics of the included studies can be found in Appendix File 3.
Network connectivity
Whether connectivity is met determines the basis of NMA. Lack of connectivity can lead to low statistical power and misleading results when direct comparison is not possible [73]. The analysis confirmed no connectivity deficit in the two networks, ensuring the accuracy of the results (Figs. 2 and 3).
Dose–response relationship
Figure 4 shows there was a nonlinear dose–response relationship between overall exercise dose and cognition up to 1000 METs -min/week (SMDs: 0.535, SD: 0.269, 95%Crl: 0.023 to 1.092), with overall exercise showing a significant increase in cognitive function. Above 1000 METs-min/week, the response to cognitive function was significantly diminished. Meanwhile, the optimal dose of overall exercise was estimated at 650 METs-min/week (SMDs:0.691, SD:0.169, 95%Crl: 0.373 to 1.039) for improving cognitive function with AD.
In Fig. 5, we show the dose–response curves for different types of exercise. Surprisingly, AE, EG, and MIX of maximum dose exceed 1000METs-min/week, however, EG did not appear to be effective in improving cognitive function in AD within the dose range. At the same time, we found an inverted U-shaped relationship between exercise dose and cognition function for AE. The optimal AE dose was found at 660 METs -min/week (SMDs: 0.909, SD:0.219, 95% CrI: 0.495 to 1.362). The improvement of cognition effect was not significant for AE at over 980 METs-min/week (SMDs: 0.729, SD: 0.374, 95%CrI: 0.004 to 1.501). On the other hand, mixed exercise was estimated to be effective at improving cognitive function at a small dose level until 180 METs-min/week (SMDs: 0.324, SD: 0.171, 95%Crl: 0.004 to 0.683). It is worth exploring that RT and TC have not found any dose to improve cognitive function in AD.
Risk of bias and certainty of evidence
Thirteen studies had a low risk of bias, 11 studies had a moderate risk of bias, and 4 studies had a high risk of bias (Fig. 6). Study-level risk of bias assessments are presented in Appendix File 7. Sensitivity analyses that included only studies with a low risk of bias were consistent with the results of the main analysis (Appendix File 7). The overall quality of the evidence was moderate according to the GRADE system. After excluding studies at high risk of bias (Appendix File 8). The optimal dose of the overall exercise was estimated at 760METs-min/week (SMDs: 0.7663, SD: 0.298, 95%CrI: 0.205 to 1.392) in improving cognitive function. The significance of improving cognitive deficits in AD was not significant at above 880METs-week (SMDs: 0.753, SD: 0.3653, 95%CrI: 0.0535 to 1.526).
Discussion
Main findings
Our study is the first to explore the nonlinear relationship between exercise dosage and cognitive function in AD, revealing that exercise positively influences cognitive impairment in AD patients. This systematic review and network meta-analysis encompassed 27 randomized controlled trials, involving 2,242 AD patients. Our findings indicate that aerobic, mixed exercise significantly enhances cognitive functions in AD patients. and that the optimal dose of overall exercise to improve cognitive dysfunction in elderly patients with AD was 650 METs-min/week. This also corresponds to approximately 150 min of moderate-intensity exercise per week or 75 min of vigorous exercises per week. This result could provide a theoretical basis for future pairs of clinical trials and indirectly demonstrate the clinical feasibility implications of our study [74]. In the analysis of the results of different exercise modalities to improve cognitive deficits in AD patients, it was concluded that 660 METs -min/week of aerobic exercise was the optimal dose to improve cognitive function in AD, which is consistent with the results of previous Susana et. al. study [9]. Our study expands upon the research conducted by Susana et al., offering a detailed exploration into the optimal dosage of specific exercise intensities for enhancing cognitive function in AD patients. This investigation delves further into the empirical validity of the findings, aiming to refine and substantiate the recommended exercise protocols for AD patients.
Strengths
There are several key strengths to our study. First, our study's use of metabolic equivalents of task (METs) to assess exercise intensity lies in its simplicity, versatility, and ability to easily compare different activities. METs are relative values of resting metabolic rate, allowing use by people across age, gender, and culture, facilitating the formulation of public health guidelines and public understanding. In addition, METs can quantitatively compare various activity intensities, supporting individuals and health professionals in developing and adjusting exercise plans [28]. Second, our study included a relatively large sample size of AD, and in order to achieve the study aim, our study provided adequate statistical power. Third, we applied the current state of the newest meta-analytical techniques to investigate the dose–response between exercise and the improvement of cognition function in AD. The new method allowed us to determine the effective dose of exercise and the optimal dose of different modalities for cognitive improvement in AD patients. Also, order to WHO recommendations, exercise improves cognitive function in patients with AD, and indirectly proves any level of exercise is better than no exercise [74, 75]. Our research results not only determined that exercise within the effective dose range is 1000 METs-min/week but also identified 650 METs-min/week as the optimal dose to improve cognitive function in AD. The actual recommendations of the WHO (600 ~ 1200METs-min/week) are echoed, and we have confirmed the effectiveness of the WHO through the existing evidence and helped medical staff better understand the strength of the WHO recommendations. Fourth, our study utilizes direct, indirect, and network estimation methods to compare the relative efficacy of various exercise interventions. This comprehensive approach enabled us to identify exercise as the most effective intervention for enhancing cognitive function in AD. We found that all types of exercise evaluated are associated with improvements in overall cognition. However, aerobic exercise has a more significant interaction with overall cognition than other types of exercise. Comparison to previous studies reporting that resistance exercise improves overall cognition in dementia or MCI populations [13, 76], The results of our study indicated that only aerobic exercise was effective in improving cognitive function in patients with AD. This was due to the strict control of inclusion and exclusion criteria, which focused specifically on AD. On the other hand, the study found a weaker dose response of mixed exercise with resistance training to improve cognitive function in patients with AD. This may be the reason why there are too few randomized controlled trials for relevant AD and more randomized controlled trials for AD patients are expected in the future, seeking to prove the effectiveness of mixed exercise versus resistance exercise on cognition in AD.
Limitations
There are several limitations in our study. Firstly, we were unable to conduct a more in-depth statistical analysis of heterogeneity due to the small number of included studies. Instead, we used a risk assessment tool to assess bias. Secondly, we did not thoroughly analyze some potential covariates such as education level, gender, and weight of the elderly, which could contribute to heterogeneity in the study results. Thirdly, we categorized the methods of evaluating cognitive impairment in AD patients into global cognitive impairment evaluation (primarily using scale evaluation) and executive cognitive impairment evaluation methods (assessing working memory, switching, and inhibition). Our primary outcome focused on the global cognitive impairment scale evaluation. Although our study identifying optimal exercise doses for AD patients provides an evidence-based recommendation aimed at promoting cognitive health, its applicability may vary due to global cognitive impairment and executive cognition. Functional impairment varies with different types of cognitive impairment. Individual differences, such as the patient's performance level, disease stage, and specific type of cognitive impairment, all need to be considered to ensure the effectiveness and safety of the exercise program. Therefore, although 650 METs-min/week provides a useful starting point, individualized adjustment of exercise dose and a combination of multimodal interventions may better meet the individual needs of AD patients, thereby maximizing positive effects on cognition and function. Fourth, our study only included English language literature, potentially leading to missing data from researchers in other countries and limiting the generalizability of our results.
Lastly, although metabolic equivalents of exercise (METs) are a widely used metric for assessing exercise intensity, which quantifies the intensity of different exercises in terms of their ratio relative to resting-state energy expenditure, in practice, the application of METs faces several significant limitations [77]. First, the calculation of METs is based on the average resting metabolic rate, without considering individual differences that affect energy expenditure, such as age, gender, weight, and physical condition. This means that the same activity may represent different actual intensities for different individuals. Second, MET values provide a fixed estimate of energy expenditure for an activity but lack the sensitivity to capture subtle changes in activity intensity, especially when distinguishing between high- and low-intensity exercise. In addition, the resting metabolic rate of all individuals is assumed to be a uniform standard (1 MET), ignoring the actual differences in energy expenditure in the resting state between people. METs are also difficult to accurately assess complex exercises or contain multiple levels of intensity, and to accurately measure exercise intensity in everyday settings where specialized measurement equipment is not available. Finally, standard MET values do not apply to individuals with specific health conditions because it does not reflect the unique responses of these individuals to exercises. Therefore, while METs provide a convenient metric for rapid estimation of exercise intensity, to obtain a more accurate and personalized assessment, other methods including heart rate monitoring are recommended, taking into account the individual's specific health status and energy expenditure characteristics.
Clinical implications and directions for future research
Our study not only corroborates previous findings on the efficacy of aerobic exercise in enhancing cognitive function in AD patients but also found a specific dose–response relationship, identifying an optimal aerobic exercise dose of 660 METs-min/week [9]. Furthermore, we established that the overall exercise dose aligns with the World Health Organization's recommended range. By pinpointing effective modalities and dosages for cognitive improvement in AD patients, our research paves the way for future exercise guidelines. In addition, implementing exercise interventions for AD patients presents significant logistical challenges. Effective execution of aerobic exercise programs demands skilled supervision and considerable resources. Comprehensive planning is essential, incorporating policy development, economic considerations, and future research directions [78]. Both government bodies and the private sector must invest in public health policies and infrastructure. This investment should focus on creating safe and accessible exercise venues, alongside professional and public education initiatives to heighten awareness of AD and the advantages of regular exercise. Concurrently, conducting cost-effectiveness analyses can highlight the potential of exercise interventions to reduce the long-term financial burden of AD care. Additionally, financial policies and incentives aimed at promoting investments in exercise programs for the prevention and management of AD are crucial. This multifaceted approach is key to enhancing the feasibility and success of exercise interventions in the AD patient population, ultimately contributing to improved health outcomes and reduced societal costs.
Conclusion
Our study incorporates the latest Bayesian modeling 'MBNMAdose' package to determine the dose–response relationship between different types of exercise and cognitive function in patients with AD. We found that the optimal overall exercise and AE dose. Using these findings, scientifically prescribed exercise can help us better cope with the cognitive function of AD by developing appropriate exercise prescription guidelines. Furthermore, given the limitations of the previously explained meta-analyses and the insufficient number of studies in the existing literature, it is important to interpret the results with caution. In the future, more detailed randomized controlled trials using a randomized group approach with different exercise doses are recommended to obtain more direct evidence on the relative effectiveness of exercise dose and response in different exercise interventions. In addition, the baseline physical tolerances of different AD patients should be fully considered to develop a rational exercise prescription programmer.
Availability of data and materials
If reviewers want to repeat the results of our study data, Please contact the first author by e-mail.
Abbreviations
- RCT:
-
Randomized controlled trials
- AD:
-
Alzheimer's disease and dementia
- PA:
-
Exercise
- SMD:
-
Standardized Mean Difference
- SD:
-
Standard Deviation
- 95%Crl:
-
95% Credible Interval
- AE:
-
Aerobic exercise
- MIX:
-
Mixed exercise
- RT:
-
Resistance training
- TC:
-
Tai chi
- EG:
-
Exergame exercise
- CON:
-
Control group
References
2023 Alzheimer’s disease facts and figures. Alzheimers & Dementia. 2023;19(4):1598–695.
Frankish H, Horton R. Prevention and management of dementia: a priority for public health. Lancet. 2017;390(10113):2614–5.
Wimo A, Seeher K, Cataldi R, Cyhlarova E, Dielemann JL, Frisell O, Guerchet M, Jönsson L, Malaha AK, Nichols E, et al. The worldwide costs of dementia in 2019. Alzheimers & Dementia. 2023;19(7):2865–73.
Kılıç B, Hiçdurmaz D, Ayhan Y, Saka E. Perspectives of Family Caregivers of People With Alzheimer's Disease on Caregiving Experience and Needs: A Qualitative Study. J Psychosoc Nurs Ment Health Serv. 2023;61:1–10.
Yu JT, Xu W, Tan CC, Andrieu S, Suckling J, Evangelou E, Pan A, Zhang C, Jia J, Feng L, et al. Evidence-based prevention of Alzheimer’s disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020;91(11):1201–9.
Norevik CS, Huuha AM, Røsbjørgen RN, Bergersen LH, Jacobsen K, Miguel-dos-Santos R, Tari AR. Exercised blood plasma promotes hippocampal neurogenesis in the Alzheimer's disease rat brain. J Sport Health Sci. 2024;13(2):245–55.
Tari AR, Nauman J, Zisko N, Skjellegrind HK, Bosnes I, Bergh S, Stensvold D, Selbæk G, Wisløff U. Temporal changes in cardiorespiratory fitness and risk of dementia incidence and mortality: a population-based prospective cohort study. The Lancet Public Health. 2019;4(11):e565–74.
Holstein-Ronsbo S, Gan YM, Giannetto MJ, Rasmussen MK, Sigurdsson B, Beinlich FRM, Rose L, Untiet V, Hablitz LM, Kelley DH, et al. Glymphatic influx and clearance are accelerated by neurovascular coupling. Nat Neurosci. 2023;26(6):1042–53.
Lopez-Ortiz S, Valenzuela PL, Seisdedos MM, Morales JS, Vega T, Castillo-Garcia A, Nisticò R, Mercuri NB, Lista S, Lucia A. Exercise interventions in Alzheimer’s disease: A systematic review and meta-analysis of randomized controlled trials. Ageing Res Rev. 2021;72:101479.
Lv S, Wang Q, Liu W, Zhang X, Cui M, Li X, Xu Y. Comparison of various exercise interventions on cognitive function in Alzheimer’s patients: A network meta-analysis. Arch Gerontol Geriatr. 2023;115:105113.
Nicola F, Catherine S. Dose–response relationship of resistance training in older adults: a meta-analysis. Br J Sports Med. 2011;45(3):233–4.
Borde R, Hortobágyi T, Granacher U. Dose–response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med. 2015;45:1693–720.
Gallardo-Gómez D, del Pozo-Cruz J, Noetel M, Álvarez-Barbosa F, Alfonso-Rosa RM, del Pozo CB. Optimal dose and type of exercise to improve cognitive function in older adults: A systematic review and bayesian model-based network meta-analysis of RCTs. Ageing Res Rev. 2022;76:101591.
Chen ML, Wotiz SB, Banks SM, Connors SA, Shi Y. Dose-Response Association of Tai Chi and Cognition among Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021;18(6):3179.
Sanders LMJ, Hortobágyi T, la Bastide-van GS, van der Zee EA, van Heuvelen MJG. Dose-response relationship between exercise and cognitive function in older adults with and without cognitive impairment: A systematic review and meta-analysis. PLoS ONE. 2019;14(1):e0210036.
Shao Z, Hu M, Zhang D, Zeng X, Shu X, Wu X, Kwok TCY, Feng H. Dose-response relationship in non-pharmacological interventions for individuals with mild cognitive impairment: A systematic review and meta-analysis of randomised controlled trials. J Clin Nurs. 2022;31(23–24):3390–401.
Pedder H. MBNMAdose: An R package for incorporating dose-response information into Network Meta-Analysis. In: Evidence Synthesis and Meta-Analysis in R Conference. 2021: 2021.
Mawdsley D, Bennetts M, Dias S, Boucher M, Welton NJ. Model-based network meta-analysis: a framework for evidence synthesis of clinical trial data. CPT: Pharmacometrics syst pharmacol. 2016;5(8):393–401.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81.
Arevalo-Rodriguez I, Smailagic N. i Figuls MR, Ciapponi A, Sanchez-Perez E, Giannakou A, Pedraza OL, Cosp XB, Cullum S: Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. 2015;3:CD010783.
Cano SJ, Posner HB, Moline ML, Hurt SW, Swartz J, Hsu T, Hobart JC. The ADAS-cog in Alzheimer’s disease clinical trials: psychometric evaluation of the sum and its parts. J Neurol Neurosurg Psychiatry. 2010;81(12):1363–8.
Hobson J. The montreal cognitive assessment (MoCA). Occup Med. 2015;65(9):764–5.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. 2008.
Watt JA, Del Giovane C, Jackson D, Turner RM, Tricco AC, Mavridis D, Straus SE, Veroniki A-A. Incorporating dose effects in network bmj. 2022;376:e067003.
Angiolillo A, Leccese D, Ciccotelli S, Di Cesare G, D’Elia K, Aurisano N, Matrone C, Dentizzi C, Di Costanzo A. Effects of Nordic walking in Alzheimer’s disease: A single-blind randomized controlled clinical trial. Heliyon. 2023;9(5):e15865.
Abbas RL, Saab IM, Al-Sharif HK, Naja N, El-Khatib A. Effect of Adding Motorized Cycle Ergometer Over Exercise Training on Balance in Older Adults with Dementia: A Randomized Controlled Trial. Exp Aging Res. 2023;49(2):100–11.
Jetté M, Sidney K, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990;13(8):555–65.
Hills AP, Mokhtar N, Byrne NM. Assessment of physical activity and energy expenditure: an overview of objective measures. Front Nutr. 2014;1:5.
Eijsvogels TM, Thompson PD. Exercise is medicine: at any dose? JAMA. 2015;314(18):1915–6.
Lee I-M. Dose-response relation between physical activity and fitness: even a little is good; more is better. JAMA. 2007;297(19):2137–9.
White IR. Network meta-analysis. Stand Genomic Sci. 2015;15(4):951–85.
Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med. 2013;159(2):130–7.
RDC Team. R: A language and environment for statistical computing. 2010.
Pedder H. MBNMAdose: An R package for dose-response Model-Based Network Meta-Analysis models. 2020.
Wheeler DC, Hickson DA, Waller LA. Assessing local model adequacy in Bayesian hierarchical models using the partitioned deviance information criterion. Comput Stat Data Anal. 2010;54(6):1657–71.
Pedder H, Dias S, Bennetts M, Boucher M, Welton NJ. Modelling time-course relationships with multiple treatments: Model-based network meta-analysis for continuous summary outcomes. Research synthesis methods. 2019;10(2):267–86.
DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–14.
Higgins JPT, Jackson D, Barrett J, Lu G, Ades A, White I. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Research synthesis methods. 2012;3(2):98–110.
Hu D, O’Connor AM, Wang C, Sargeant JM, Winder CB. How to conduct a Bayesian network meta-analysis. Frontiers in veterinary science. 2020;7:271.
Takeshima N, Sozu T, Tajika A, Ogawa Y, Hayasaka Y, Furukawa TA. Which is more generalizable, powerful and interpretable in meta-analyses, mean difference or standardized mean difference? BMC Med Res Methodol. 2014;14(1):1–7.
Hespanhol L, Vallio CS, Costa LM, Saragiotto BT. Understanding and interpreting confidence and credible intervals around effect estimates. Braz J Phys Ther. 2019;23(4):290–301.
Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29(9):1037–57.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d59282.
Minozzi S, Cinquini M, Gianola S, Gonzalez-Lorenzo M, Banzi R. The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. J Clin Epidemiol. 2020;126:37–44.
Minozzi S, Dwan K, Borrelli F, Filippini G. Reliability of the revised Cochrane risk-of-bias tool for randomised trials (RoB2) improved with the use of implementation instruction. J Clin Epidemiol. 2022;141:99–105.
Iyengar S, Greenhouse J. Sensitivity analysis and diagnostics. Handbook of research synthesis and meta-analysis. 2009:417–33.
Lautenschlager NT, Cox KL, Flicker L, Foster JK, Van Bockxmeer FM, Xiao J, Greenop KR, Almeida OP. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA. 2008;300(9):1027–37.
Kwak Y-S, Um S-Y, Son T-G, Kim D-J. Effect of regular exercise on senile dementia patients. Int J Sports Med. 2007;29:471–4.
Kemoun G, Thibaud M, Roumagne N, Carette P, Albinet C, Toussaint L, Paccalin M, Dugué B. Effects of a physical training programme on cognitive function and walking efficiency in elderly persons with dementia. Dement Geriatr Cogn Disord. 2010;29(2):109–14.
Tai S-Y, Hsu C-L, Huang S-W, Ma T-C, Hsieh W-C, Yang Y-H. Effects of multiple training modalities in patients with Alzheimer’s disease: a pilot study. Neuropsychiatr Dis Treat. 2016;12:2843–9.
Holthoff VA, Marschner K, Scharf M, Steding J, Meyer S, Koch R, Donix M. Effects of physical activity training in patients with Alzheimer’s dementia: results of a pilot RCT study. PLoS ONE. 2015;10(4):e0121478.
Bossers WJ, van der Woude LH, Boersma F, Hortobágyi T, Scherder EJ, van Heuvelen MJ. A 9-week aerobic and strength training program improves cognitive and motor function in patients with dementia: a randomized, controlled trial. Am J Geriatr Psychiatry. 2015;23(11):1106–16.
Telenius EW, Engedal K, Bergland A. Effect of a high-intensity exercise program on physical function and mental health in nursing home residents with dementia: an assessor blinded randomized controlled trial. PLoS ONE. 2015;10(5):e0126102.
Yang S-Y, Shan C-L, Qing H, Wang W, Zhu Y, Yin M-M, Machado S, Yuan T-F, Wu T. The effects of aerobic exercise on cognitive function of Alzheimer’s disease patients. CNS Neurol Disord Drug Targets. 2015;14(10):1292–7.
Cancela JM, Ayán C, Varela S, Seijo M. Effects of a long-term aerobic exercise intervention on institutionalized patients with dementia. J Sci Med Sport. 2016;19(4):293–8.
Hoffmann K, Sobol NA, Frederiksen KS, Beyer N, Vogel A, Vestergaard K, Brændgaard H, Gottrup H, Lolk A, Wermuth L. Moderate-to-high intensity physical exercise in patients with Alzheimer’s disease: a randomized controlled trial. J Alzheimers Dis. 2016;50(2):443–53.
Toots A, Littbrand H, Boström G, Hörnsten C, Holmberg H, Lundin-Olsson L, Lindelöf N, Nordström P, Gustafson Y, Rosendahl E. Effects of exercise on cognitive function in older people with dementia: a randomized controlled trial. J Alzheimers Dis. 2017;60(1):323–32.
Lamb SE, Sheehan B, Atherton N, Nichols V, Collins H, Mistry D, Dosanjh S, Slowther AM, Khan I, Petrou S. Dementia And Physical Activity (DAPA) trial of moderate to high intensity exercise training for people with dementia: randomised controlled trial. bmj. 2018;361:k1675.
Venturelli M, Scarsini R, Schena F. Six-month walking program changes cognitive and ADL performance in patients with Alzheimer. Am J Alzheimer’s Dis Other Dem. 2011;26(5):381–8.
Arcoverde C, Deslandes A, Moraes H, Almeida C. Araujo NBd, Vasques PE, Silveira H, Laks J: Treadmill training as an augmentation treatment for Alzheimer’s disease: a pilot randomized controlled study. Arq Neuropsiquiatr. 2014;72:190–6.
Gaitán JM, Boots EA, Dougherty RJ, Oh JM, Ma Y, Edwards DF, Christian BT, Cook DB, Okonkwo OC. Brain glucose metabolism, cognition, and cardiorespiratory fitness following exercise training in adults at risk for Alzheimer’s disease. Brain Plasticity. 2019;5(1):83–95.
Huang N, Li W, Rong X, Champ M, Wei L, Li M, Mu H, Hu Y, Ma Z, Lyu J. Effects of a modified Tai Chi program on older people with mild dementia: a randomized controlled trial. J Alzheimers Dis. 2019;72(3):947–56.
Nyman SR, Ingram W, Sanders J, Thomas PW, Thomas S, Vassallo M, Raftery J, Bibi I, Barrado-Martín Y. Randomised controlled trial of the effect of Tai Chi on postural balance of people with dementia. Clin Interv Aging. 2019;14:2017–29.
Sampaio A, Marques EA, Mota J, Carvalho J. Effects of a multicomponent exercise program in institutionalized elders with Alzheimer’s disease. Dementia. 2019;18(2):417–31.
Liu I-T, Lee W-J, Lin S-Y, Chang S-T, Kao C-L, Cheng Y-Y. Therapeutic effects of exercise training on elderly patients with dementia: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101(5):762–9.
van Santen J, Dröes RM, Twisk JW, Henkemans OAB, van Straten A, Meiland FJ. Effects of exergaming on cognitive and social functioning of people with dementia: a randomized controlled trial. Journal of the American Medical Directors Association. 2020;21(12):1958-1967.e1955.
Liao Y-Y, Chen I-H, Hsu W-C, Tseng H-Y, Wang R-Y. Effect of exergaming versus combined exercise on cognitive function and brain activation in frail older adults: A randomised controlled trial. Ann Phys Rehabil Med. 2021;64(5):101492.
Yu F, Salisbury D, Mathiason MA. Inter-individual differences in the responses to aerobic exercise in Alzheimer’s disease: Findings from the FIT-AD trial. J Sport Health Sci. 2021;10(1):65–72.
Yu F, Vock DM, Zhang L, Salisbury D, Nelson NW, Chow LS, Smith G, Barclay TR, Dysken M, Wyman JF. Cognitive effects of aerobic exercise in Alzheimer’s disease: a pilot randomized controlled trial. J Alzheimers Dis. 2021;80(1):233–44.
Borges-Machado F, Teixeira L, Carvalho J, Ribeiro O. Does Multicomponent Physical Exercise Training Work for Dementia? Exploring the Effects on Cognition, Neuropsychiatric Symptoms, and Quality of Life. J Geriatr Psychiatry Neurol. 2023;36(5):376–85.
Vreugdenhil A, Cannell J, Davies A, Razay G. A community-based exercise programme to improve functional ability in people with Alzheimer’s disease: A randomized controlled trial. Scand J Caring Sci. 2012;26(1):12–9.
Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med. 2017;12:103–11.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput J-P, Chastin S, Chou R. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Larson EB, Wang L, Bowen JD, McCormick WC, Teri L, Crane P, Kukull W. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med. 2006;144(2):73–81.
Huang X, Zhao X, Li B, Cai Y, Zhang S, Wan Q, Yu F. Comparative efficacy of various exercise interventions on cognitive function in patients with mild cognitive impairment or dementia: a systematic review and network meta-analysis. J Sport Health Sci. 2022;11(2):212–23.
Franklin BA, Brinks J, Berra K, Lavie CJ, Gordon NF, Sperling LS. Using metabolic equivalents in clinical practice. Am J Cardiol. 2018;121(3):382–7.
Bynum JP. The long reach of Alzheimer’s disease: patients, practice, and policy. Health Aff. 2014;33(4):534–40.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YY and YY designed the study and revised the manuscript. YY and XFH drafted the manuscript. LZ and YY conducted the database search and data extraction. YY, ZYX and YY conducted the data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12877_2024_5060_MOESM1_ESM.docx
Additional file 1: Appendix 1. Search Strategy. Appendix 2. Transformation formulas for estimating the mean and standard deviation. Appendix 3. Characteristics of the dataset and included studies. Appendix 4. Key Assumptions of Network Meta-Analysis. Appendix 5. Nonlinear function and model fit comparison. Appendix 6. Ranking of the effectiveness of interventions. Appendix 7. Study level Risk of Bias analysis. Appendix 8. Sensitivity analysis including only studies with low risk of bias. Appendix 9. The list of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yuan, Y., Yang, Y., Hu, X. et al. Effective dosage and mode of exercise for enhancing cognitive function in Alzheimer's disease and dementia: a systematic review and Bayesian Model-Based Network Meta-analysis of RCTs. BMC Geriatr 24, 480 (2024). https://doi.org/10.1186/s12877-024-05060-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05060-8