Abstract
Background
Different treatment options are discussed for geriatric odontoid fracture. The aim of this study was to compare the treatment options for geriatric odontoid fractures.
Methods
Included were patients with the following criteria: age ≥ 65 years, identification of seniors at risk (ISAR score ≥ 2), and odontoid fracture type A/B according to Eysel and Roosen. Three groups were compared: conservative treatment, surgical therapy with ventral screw osteosynthesis or dorsal instrumentation. At a follow-up examination, the range of motion and the trabecular bone fracture healing rate were evaluated. Furthermore, demographic patient data, neurological status, length of stay at the hospital and at the intensive care unit (ICU) as well as the duration of surgery and occurring complications were analyzed.
Results
A total of 72 patients were included and 43 patients could be re-examined (range: 2.7 ± 2.1 months). Patients with dorsal instrumentation had a better rotation. Other directions of motion were not significantly different. The trabecular bone fracture healing rate was 78.6%. The patients with dorsal instrumentation were hospitalized significantly longer; however, their duration at the ICU was shortest. There was no significant difference in complications.
Conclusion
Geriatric patients with odontoid fracture require individual treatment planning. Dorsal instrumentation may offer some advantages.
Similar content being viewed by others
Background
Due to demographic changes, the number of geriatric trauma patients is constantly increasing [1]. Geriatric patients, having a worse general condition and a corresponding increased need for extensive care, can be identified by using the seniors at risk (ISAR) score [2,3,4] upon admission to the hospital. In these geriatric patients, odontoid fractures are the most common, comprising more than 50% of fractures of the cervical spine [5].
In contrast to odontoid fractures in young patients, these injuries in the geriatric population are mainly caused by minor trauma and falls at home [6]. The poor bone quality of the geriatric population together with pre-existing conditions such as osteopenia and osteoporosis are one of the main reasons for occurrence of this fracture [7].
In 1974, Anderson and D’Alonzo established a classification system for odontoid fractures according to fracture morphology [8]: type I fractures affect the tip of the odontoid, type II fractures affect the base of the odontoid, and in type III fractures, the corpus of the axis is affected. Around 19 years later, type II odontoid fractures according to Anderson and D’Alonzo were subclassified by Eysel and Roosen for association with different treatment options (Fig. 1): type A is a horizontal fracture (Fig. 1A) that can be treated with ventral screw osteosynthesis; type B is a fracture line from ventrocranial to dorsocaudal (Fig. 1B) that can be treated like type A; type C is a fracture line from ventrocaudal to dorsocranial (Fig. 1C) that can be treated with dorsal instrumentation of C1 and C2 [9,10,11]. Whereas the ventral screw osteosynthesis could only be applied in type A and type B fractures due to an increased risk for a ventral dislocation of the odontoid, the dorsal instrumentation, may be applicable in all fracture types according to Eysel and Roosen [12].
Surgical treatment by different surgical approaches as well as conservative treatment may be associated with various complications and high mortality rates, especially in patients with reduced general condition [13,14,15,16,17,18,19,20].
The aim of the present study was to compare clinical and radiological outcome as well as peri-operative data and complications for geriatric patients with type A and B odontoid fractures according to Eysel and Roosen following conservative treatment vs. operative treatment by ventral vs. dorsal stabilization.
Methods
The present study was approved by the local ethics commission in charge (Ethics Committee of the State Medical Association Rhineland-Palatinate, Mainz, Germany). All patients who met the following criteria were included in this retrospective single-center cohort study: (i) age of 65 years or older, (ii) ISAR [2, 3] score of 2 or higher, (iii) fracture of the odontoid type A or B according to Eysel and Roosen [9], and (iv) treatment between January 2012 and December 2017. To obtain a homogeneous patient population, we excluded non-geriatric patients as well as patients suffering from other C2 fractures.
Clinical evaluation
The demographic data as well as the prehospital and treatment data of the patients were documented as a standard procedure. Data on pre-existing conditions, trauma mechanism, Glasgow Coma Scale (GCS), ISAR score and neurological status were collected for all patients. The ISAR score can be used to assess the need for assistance among geriatric patients. From a score of 2, there is a significant need for additional assistance for the geriatric patients [2,3,4]. The duration of hospital stay, the duration of stay at the intensive care unit (ICU), and the duration of surgery were registered.
Conservative and surgical treatment
All patients underwent a clinical and neurological examination as well as a computer tomography (CT) scan of the cervical spine on the day of admission to the hospital. Further treatment was mainly based on the recommendations given by Eysel and Roosen [9]. However, the decision on treatment was influenced by dislocation and instability [10] of the odontoid fracture. With increasing instability and dislocation, dorsal instrumentation was performed. Dorsal surgical therapy was performed especially in cases of dislocation of more than two millimeters. Otherwise, ventral screw osteosynthesis was performed. Conservative treatment was performed on patients in whom there was no dislocation.
Conservative treatment
The cervical spine was immobilized for 6 weeks in a soft or rigid collar. Regular clinical controls were performed to evaluate the skin under the collar and the patient’s condition.
Surgical treatment
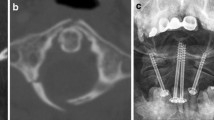
Two different surgical procedures were used to stabilize the fracture. In both surgical procedures, the reduction was performed as a closed procedure. The ventral operative treatment was carried out via a standard Smith–Robinson approach at the upper cervical spine [21]. Two guide wires were inserted into the odontoid from ventrocaudal to craniodorsal. The guide wires were subsequently overscrewed with cannulated screws (Fig. 2A, B, C). The dorsal operative treatment was performed via a median approach. Dorsal instrumentation was performed according to Harms et al. [22] (Fig. 3A, B, C) with a Mountaineer OCT Spinal System (DePuy Spine Inc., Raynham, MA, USA).
A first control CT scan was performed before discharge from the hospital for all patients, regardless of the treatment regime, to detect possible secondary dislocation and to control implant placement in surgical cases. A second control CT scan 6 weeks after the initial trauma was recommended to detect possible secondary dislocation as well as trabecular bone fracture healing rate.
Outcome analysis
The main endpoints of the present study were (1) the range of motion of the cervical spine at the follow–up examination and (2) the trabecular bone fracture healing rate, detected by CT scans at the follow-up examination.
A routine follow–up examination of patients took place after 6 weeks. All motions were performed in a medically controlled manner. The gross mobility of the cervical spine (extension/flexion, rotation, lateral bending) was recorded by the examining physician in all patients. The following three–step range–of–motion score (ROMS) was used to classify range of motion: range of motion was scored as “0” in patients without any mobility in the cervical spine, “1” in patients with limited mobility, and “2” in patients with almost free mobility. Although range-of-motion measurement devices (e.g. goniometer) are promising, their practicability is questionable [23]. Some degrees of exercise make no noticeable clinical difference to patients. Thus, only gross ROMS was assessed to describe the patient’s cervical spine motion.
Pain and other post-treatment complications were recorded. Routine CT imaging 6 weeks after the cervical spine injury was analyzed. Secondary dislocation, implant failure and the trabecular bone fracture healing rate was assessed. Bone healing was defined by the detection of trabecular bone across the fracture line.
Complication analysis
For all patients, every complication was recorded and classified according to Dindo et al. [24]: Grade I is defined as any deviation from a normal treatment process, Grade II includes deviations that could be managed by additional pharmacological therapy, Grade III includes complications that had to be treated with a surgical intervention, and Grade IV describes all life–threatening complications. The death of a patient is classified as Grade V.
Statistical data analysis
The data were tested for normality distribution with the Anderson–Darling and D’Agostino and Pearson test (age and ISAR score). If a normal distribution was found, a one–way ANOVA was performed comparing the three treatment groups. If the normality test failed, the Kruskal–Wallis test with multiple comparisons was performed. In comparing two groups, the Mann–Whitney U–test was performed if distribution was not considered normal. The Fisher´s exact test was applied to the testing of bivariate or categorical data. In all significance tests for differences and associations, a p–value < 0.05 was considered to indicate statistical significance. Statistical data analysis was performed using GraphPad Prism (Version 8.2.1, San Diego, CA, USA).
Results
Patient characteristics
In the period between January 2012 and December 2017, a total of 72 patients (40 female, 32 male) were included in this study. The mean age was 83.2 ± 7.5 years (range: 65–100 years). The mean ISAR score was 2.6 ± 0.8 (range: 2–5). Between the examined groups (conservative treatment, ventral surgery, and dorsal surgery), there was no significant differences regarding the distribution of patient age, gender or ISAR score. Therefore, the groups were categorized as comparable.
The main injury mechanism was fall from a low height (< 2 m, n = 68; 94.4%). Two patients (2.8%) fell from a great height (≥ 2 m). Another two patients (2.8%) were involved in a traffic accident. The mean GCS upon admission was 14.6 ± 1.3 (range: 8–15).
Concomitant injuries were present in 40 patients (55.6%). The most frequent concomitant injuries were scalp laceration (n = 17; 23.6%), fracture of the nasal bone (n = 11; 15.3%), and craniocerebral trauma (n = 7; 9.7%) with accompanying intracranial hemorrhage in 5 cases. In 3 patients (4.2%), an additional injury to the spine was diagnosed.
Treatment
The number of patients in the different treatment groups is shown in Table 1. A total of 19 patients (26.4%) were treated conservatively (conservative treatment). There were no crossovers to surgical therapy. Surgical stabilization of the fracture was performed in 53 patients (73.6%). A ventral approach with screw osteosynthesis of the fractured odontoid was performed in 35 patients (48.6%; ventral surgery). In 18 patients (25.0%), surgery was performed using a dorsal approach (dorsal surgery). In two patients, a halo fixator was applied as emergency treatment until final surgical treatment could be performed.
The duration of surgery in patients from the dorsal surgery group (169.1 ± 58.7 min; range: 86–315 min) was significantly longer than in patients from the ventral surgery group (51.5 ± 32.1 min; range: 23–181 min; p < 0.0001; Fig. 4A, Table 2).
Overall, the patients were hospitalized for 13.9 ± 11.0 days (range: 2–73 days). Patients from the dorsal surgery group were hospitalized for 22.5 ± 17.2 days (range: 8–73 day), which is significantly longer than patients in the ventral surgery group (12.0 ± 4.3 days; range: 5–23 days; p = 0.0162). However, hospitalization was shortest for the conservative treatment group (9.4 ± 7.7 days; range: 2–30 days; Fig. 4B, Table 2).
Patients from the ventral surgery group were treated in the ICU for a mean of 11.0 ± 8.0 days (n = 4; range: 6–23 days). Mean treatment time in the ICU for patients from the dorsal surgery group (3.0 ± 1.6 days; n = 5, range: 1–5 days; Fig. 4C, Table 2) was significantly shorter (p = 0.0444). Patients from the conservative treatment group spent, on average, 13.3 ± 12.0 days (n = 4; range: 4–30 days) in the ICU.
The cervical spine was immobilized in 60 patients (83.3%). Table 3 illustrates the type of immobilization and application time.
Functional and clinical outcome
A total of 43 patients were re–examined (follow–up rate: 59.7%). The mean follow-up time was 2.7 ± 2.1 months (range: 1–9 months). Patients from all groups were re–examined (conservative treatment: n = 9; ventral surgery: n = 22; dorsal surgery: n = 12). Between the follow–up groups, there were no significant differences between the age, gender and ISAR score distributions.
The ROMS distribution of all followed-up patients in the three treatment groups are shown in Fig. 5. Patients with a complete loss of cervical spine mobility towards all directions are rare and were only found in the conservative treatment group (Fig. 5A) as well as in the ventral surgery group (Fig. 5B). In this cohort, full cervical spine mobility was preserved best after dorsal surgery (Fig. 5C).
For reclination and inclination, the mean ROMS in the conservative treatment group was 1.1 ± 0.6. In the ventral vs. dorsal surgery group, mean ROMS for reclination and inclination was 1.5 ± 0.7 vs. 1.5 ± 0.9, respectively. Comparing the surgically and conservatively treated patients, there was no significant difference (p = 0.3299). There was also no significant difference when comparing the ventral and dorsal operative groups (p = 0.9995).
For rotation, the mean ROMS in the conservative treatment group was 1.2 ± 0.7. In the ventral vs. dorsal surgery group, mean ROMS for rotation was 1.3 ± 0.6 vs. 1.9 ± 0.3, respectively. Comparing the surgically and conservatively treated patients, there was no significant difference (p = 0.9148). When comparing the ventral and dorsal operative groups, there was a significant difference (p = 0.0267).
For lateral bending, the mean ROMS in the conservative treatment group was 1.1 ± 0.8. In the ventral vs. dorsal surgery group, mean ROMS for lateral bending was 1.3 ± 0.7 vs. 1.7 ± 0.6, respectively. Comparing the surgically and conservatively treated patients, there was no significant difference (p = 0.9915). There was also no significant difference when comparing the ventral and dorsal operative groups (p = 0.1765).
At the follow-up examination, no patient from the conservative treatment group suffered from pain. In the surgical groups, 19.0% vs. 16.7% (ventral surgery vs. dorsal surgery) of patients complained of pain. The only clinical complication that occurred during the follow-up treatment was an unsteady gait. This complication was most frequent in patients undergoing dorsal surgery, at 16.7%. This unsteady gait was less frequent in the other two groups at 11.1% (conservative treatment) and 4.8% (ventral surgery). There were no significant differences between the results for the three groups (p = 0.5444).
Radiological outcome
The trabecular bone fracture healing rate was 78.6% of patients at follow–up. The conservative group had the lowest trabecular bone fracture healing rate (72.7%). There was no significant difference when comparing trabecular bone fracture healing rate of conservative versus operative group (p = 0.378, odds ratio = 2.2, CI: 0.505–10.2).
The trabecular bone fracture healing rate occurred in 79.2% of patients in the ventral surgery group. The highest rate of trabecular bone fracture healing occurred in the dorsal surgery group (94.2%). There was no significant difference when comparing ventral and dorsal surgery group with trabecular bone fracture healing rate (p = 0.373, odds ratio = 4.2, CI: 0.561–52.29).
Screw loosening occurred only in 2 patients from the ventral surgery group. Secondary dislocation of the fracture occurred in 6 patients (2 with conservative treatment and 4 with ventral surgery).
Complications
A total of 46 patients (63.9%) had no recorded complications. The remaining 26 patients (36.1%) had a total of 34 complications. There was no significant difference between the three treatment groups in terms of numbers and grade of complications according to Dindo et al. (Table 4; Fig. 6; conservative treatment: n = 8, 50.0%; ventral surgery: n = 13, 37.1%; dorsal surgery: n = 12, 66.7%). Delirium occurred most frequently in patients in the conservative treatment group (n = 3; 15.8%) and in patients from the dorsal surgery group (n = 3; 16.7%). Pneumonia occurred most frequently in patients of the ventral surgery group (n = 3; 8.6%). Loss of reduction occurred in patients of the ventral surgery (n = 4; 11.4%) and conservative treatment (n = 2, 10.5%) groups.
Discussion
The treatment options for odontoid fracture in geriatric patients are a subject of controversy in the current literature [13, 20, 25, 26]. There are no clear instructions for further therapy, especially for type A and B fractures according to Eysel and Roosen [27,28,29]. These fractures could be addressed by a ventral stabilization as well as by a dorsal stabilization.
The findings of the current study confirm that the individual treatment methods have different advantages and disadvantages. For each individual geriatric patient entering the emergency room with an odontoid fracture, these treatment advantages and disadvantages should be weighed against each other, and an individual treatment plan should be constructed. The evidence from our study shows that dorsal surgical treatment may be preferable, especially in geriatric patients with a type A or B odontoid fractures according to Eysel and Roosen.
The goals in the treatment of geriatric patients differ from those of adults. The focus in geriatric patients is on maintaining independence in the activities of daily life [30]. The present study showed a trend toward dorsal surgical therapy. Patients had secure fixation with dorsal instrumentation and thus primary stability. The geriatric patients with dorsal instrumentation showed a tendency towards a better functional outcome with better mobility of the cervical spine (ROMS). This high primary stability in the fracture area allows especially the geriatric patients to achieve early autonomy [30]. Treatment by dorsal instrumentation involves fixation of the upper cervical spine and is safe and stable [20, 31, 32], especially in comparison to ventral screw osteosynthesis, which is susceptible to screw dislocation [33], and in comparison to conservative treatment, in which external fixation creates only minimal immobilization, and secondary dislocation of the odontoid fracture often occurs [12].
Especially in geriatric patients, the mobility of the cervical spine during the follow-up examination is another clinically relevant parameter and a main endpoint of the study when evaluating the different treatment methods. Most studies describe an advantage of mobility in ventral screw osteosynthesis since no mobile segments of the upper cervical spine are fixed [26, 34]. For patients with dorsal instrumentation, a considerable restriction of rotation is often described [35]. However, in the current study, rotation was less restricted following dorsal instrumentation. No significant differences were found towards inclination, reclination and lateral bending. The good mobility of the cervical spine from the dorsal surgery group patients was most likely due to non-executed immobilization. Patients from the ventral surgery and conservative treatment groups were immobilized in the cervical spine for up to 6 weeks. Patients from the dorsal group were able to move the cervical spine directly and without immobilization and could thus be physiotherapeutically exercised. Whether this rotation in the three groups is equalized in the long term must be analyzed in further studies.The complication rate of dorsal surgery patients was not significantly higher compared to the other groups, despite the invasiveness of the surgical approach. Even the length of stay in the ICU was significantly shorter than ventral surgery patients. Postoperative unsteady gait was not significantly increased. Postoperative pain was described equally in both surgically treated groups, most likely due to the short follow-up phase. Post-operative pain after cervical spine surgery only decreases noticeably after 3 to 12 months [36]. In a systematic review of a total of 1233 geriatric patients with type II odontoid fracture according to Anderson and D’Alonzo, Schröder et al. found no significant difference in the number of complications between surgical and conservative treatment or between the various surgical treatment options [37]. White et al. reported similar results regarding complications in a systematic review of the literature [38].
A disadvantage for patients in the dorsal surgery group is that the duration of surgery was significantly longer. However, the shorter length of stay of the geriatric patients at the ICU compensated for the longer duration of surgery. Patients from the conservative treatment group and ventral surgery group were treated in the ICU due to respiratory and swallowing problems.
Overall, the long hospitalization time of geriatric patients with high ISAR score is due to early complex rehabilitation already starting in the hospital. The longer hospitalization time of patients from the dorsal surgery group is most likely due to extended clinical control and wound healing. Experience shows that wounds from dorsal cervical spine surgery often shows prolonged wound healing. Furthermore, wound infections occur more frequently [5]. This was also shown in our study.
Limitations
The present study is limited by the retrospective monocentric study design. The decision on the allocation to one of the treatment paths was based on the current recommendations but was also influenced by the patient`s medical condition. Thus, a biased choice of treatment options could not be excluded. Further studies should investigate whether patients with a lower level of dislocation also benefit from dorsal surgery. In addition, only a small group of patients was examined, which limits the significance of the present work.
Some parameters such as the intraoperative blood loss were not documented in a standardized manner at the time of the study and could thus not be analyzed. According to the literature, the follow-up period of almost 3 months is only suitable to make a first statement about a possible trabecular bone fracture healing in the geriatric population [39]. Furthermore, it should be noted that in the present geriatric patient population with a mean age of 83 years and an ISAR score of 2.6, long-term outcome is not expected [40]. Especially since these patients have a high risk of death [41].
Apart from these limitations, the data of the present study suggests that geriatric patients with a type A or B odontoid fracture according to Eysel and Roosen may benefit from a surgical treatment with a dorsal instrumentation. This finding is supported by other recent studies [20, 42]. However, all treatment options have to be weighed up against each other in every individual patient since each of the different treatment option has special disadvantages.
Conclusions
In summary, geriatric patients with odontoid fracture type A and B according to Eysel and Roosen represent a major challenge for hospitals and the healthcare system. The treatment and surgical therapy should be chosen on an individual basis according to the patient’s condition and the fracture morphology. The findings show that the range of motion, the complications and the trabecular bone healing rate do not correlate with the different treatment strategies (conservative treatment, ventral surgery, and dorsal surgery). Altogether, dorsal instrumentation may have advantages over conservative therapy and ventral screw osteosynthesis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computer tomography
- GCS:
-
Glasgow Coma Scale
- ICU:
-
Intensive care unit
- ISAR:
-
Identification of seniors at risk
- ROMS:
-
Range of motion score
References
Smith HE, Kerr SM, Fehlings MG, Chapman J, Maltenfort M, Zavlasky J, et al. Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a model system spine injury tertiary referral center. J Spinal Disord Tech. 2010;23(8):501–5.
Warburton RN, Parke B, Church W, McCusker J. Identification of seniors at risk: process evaluation of a screening and referral program for patients aged > or =75 in a community hospital emergency department. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2004;17(6):339–48.
Barlow DR, Higgins BT, Ozanne EM, Tosteson AN, Pearson AM. Cost effectiveness of operative versus non-operative treatment of geriatric type-II odontoid fracture. Spine (Phila Pa 1976). 2016;41(7):610–7.
Galvin R, Gilleit Y, Wallace E, Cousins G, Bolmer M, Rainer T, et al. Adverse outcomes in older adults attending emergency departments: a systematic review and meta-analysis of the Identification of Seniors At Risk (ISAR) screening tool. Age Ageing. 2016;46(2):179–86.
Osterhoff G, Schnake K, Scheyerer MJ, Ullrich BW, Hartmann F, Franck A, et al. Recommendations for diagnosis and treatment of odontoid fractures in geriatric patients. Z Orthop Unfall. 2020;158(6):647–56. https://doi.org/10.1055/a-0989-2791.
Müller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8(5):360–5.
Watanabe M, Sakai D, Yamamoto Y, Sato M, Mochida J. Upper cervical spine injuries: age-specific clinical features. J Orthop Sci. 2010;15(4):485–92.
Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56(8):1663–74.
Eysel P, Roosen K. Ventral or dorsal spondylodesis in dens basal fracture–a new classification for choice of surgical approach. Zentralbl Neurochir. 1993;54(4):159–65.
Liao S, Jung MK, Hörnig L, Grützner PA, Kreinest M. Injuries of the upper cervical spine-how can instability be identified? Int Orthop. 2020;44(7):1239–53.
Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5(2):123–9.
Meyer C, Oppermann J, Meermeyer I, Eysel P, Muller LP, Stein G. Management and outcome of type II fractures of the odontoid process. Unfallchirurg. 2018;121(5):397–402.
Chapman J, Smith JS, Kopjar B, Vaccaro AR, Arnold P, Shaffrey CI, et al. The AOSpine North America geriatric odontoid fracture mortality study: a retrospective review of mortality outcomes for operative versus nonoperative treatment of 322 patients with long-term follow-up. Spine (Phila Pa 1976). 2013;38(13):1098–104.
Di Paolo A, Piccirilli M, Pescatori L, Santoro A, D’Elia A. Single institute experience on 108 consecutive cases of type II odontoid fractures: surgery versus conservative treatment. Turk Neurosurg. 2014;24(6):891–6.
Fan L, Ou D, Huang X, Pang M, Chen XX, Yang B, et al. Surgery vs conservative treatment for type II and III odontoid fractures in a geriatric population: a meta-analysis. Medicine (Baltimore). 2019;98(44): e10281.
Huang DG, Zhang XL, Hao DJ, He BR, Wang XD, Liu TJ. The healing rate of type II odontoid fractures treated with posterior atlantoaxial screw-rod fixation: a retrospective review of 77 patients. J Am Acad Orthop Surg. 2019;27(5):e242–8.
Vaccaro AR, Kepler CK, Kopjar B, Chapman J, Shaffrey C, Arnold P, et al. Functional and quality-of-life outcomes in geriatric patients with type-II dens fracture. J Bone Joint Surg. 2013;95(8):729–35.
Aquila F, Tacconi L, Baldo S. Type II fractures in older adults: can they be treated conservatively?: A single-center experience and review of the literature. World Neurosurg. 2018;118:e938–45.
Gembruch O, Lemonas E, Ahmadipour Y, Sure U, El Hindy N, Dodel R, et al. Treatment of odontoid type II fractures in octogenarians: balancing two different treatment strategies. Neurospine. 2019;16(2):360–7.
Wagner SC, Schroeder GD, Kepler CK, Schupper AJ, Kandziora F, Vialle EN, et al. Controversies in the Management of Geriatric Odontoid Fractures. J Orthop Trauma. 2017;31(Suppl 4):S44–8.
Cauchoix J, Binet JP. Anterior surgical approaches to the spine. Ann R Coll Surg Engl. 1957;21(4):234–43.
Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001;26(22):2467–71.
Jordan K. Assessment of published reliability studies for cervical spine range-of-motion measurement tools. J Manipulative Physiol Ther. 2000;23(3):180–95.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Gornet ME, Kelly MP. Fractures of the axis: a review of pediatric, adult, and geriatric injuries. Curr Rev Musculoskelet Med. 2016;9(4):505–12.
Platzer P, Thalhammer G, Oberleitner G, Schuster R, Vécsei V, Gaebler C. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am. 2007;89(8):1716–22.
Unfallchirurgie DGf. Verletzungen der oberen Halswirbelsäule. DGU Leitlinie 012–011 2018. Available from: https://www.awmf.org/uploads/tx_szleitlinien/012-011l_S1_Verletzungen-der-oberen-HWS_2018-09.pdf. Accessed 5 May 2019.
Ryken TC, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, et al. Management of isolated fractures of the axis in adults. Neurosurgery. 2013;72(Suppl 2):132–50.
Iyer S, Hurlbert RJ, Albert TJ. Management of odontoid fractures in the elderly: a review of the literature and an evidence-based treatment algorithm. Neurosurgery. 2018;82(4):419–30.
Rommens PM. Paradigm shift in geriatric fracture treatment. Eur J Trauma Emerg Surg. 2019;45(2):181–9.
De Bonis P, Iaccarino C, Musio A, Martucci A, De Iure F, Donati R, et al. Functional Outcome of Elderly Patients Treated for Odontoid Fracture: A Multicenter Study. Spine (Phila Pa 1976). 2019;44(13):951–8.
Maciejczak A, Wolan-Nieroda A, Jabłońska-Sudoł K. Comparison of fusion rates between rod-based laminar claw hook and posterior cervical screw constructs in Type II odontoid fractures. Injury. 2015;46(7):1304–10.
Evaniew N, Yarascavitch B, Madden K, Ghert M, Drew B, Bhandari M, et al. Atlantoaxial instability in acute odontoid fractures is associated with nonunion and mortality. Spine J. 2015;15(5):910–7.
Patterson JT, Theologis AA, Sing D, Tay B. Anterior versus posterior approaches for odontoid fracture stabilization in patients older than 65 years: 30-day morbidity and mortality in a National Database. Clin Spine Surg. 2017;30(8):E1033–8.
Vetter S. Cervical spine injuries in the elderly patient. Chirurg. 2019;90(10):782–90.
Pugely AJ, Bedard NA, Kalakoti P, Hendrickson NR, Shillingford JN, Laratta JL, et al. Opioid use following cervical spine surgery: trends and factors associated with long-term use. Spine J. 2018;18(11):1974–81.
Schroeder GD, Kepler CK, Kurd MF, Paul JT, Rubenstein RN, Harrop JS, et al. A systematic review of the treatment of geriatric type II odontoid fractures. Neurosurgery. 2015;77(Suppl 4):S6-14.
White AP, Hashimoto R, Norvell DC, Vaccaro AR. Morbidity and mortality related to odontoid fracture surgery in the elderly population. Spine (Phila Pa 1976). 2010;35(9 Suppl):S146-57.
Lewis E, Liew S, Dowrick A. Risk factors for non-union in the non-operative management of type II dens fractures. ANZ J Surg. 2011;81(9):604–7.
Theou O, Campbell S, Malone ML, Rockwood K. Older adults in the Emergency Department with Frailty. Clin Geriatr Med. 2018;34(3):369–86.
Vaupel JW, Manton KG, Stallard E. The impact of heterogeneity in individual frailty on the dynamics of mortality. Demography. 1979;16(3):439–54.
Scholz M, Kandziora F, Hildebrand F, Kobbe P. Injuries of the upper cervical spine : Update on diagnostics and management. Unfallchirurg. 2017;120(8):683–700.
Acknowledgements
None.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Contributions
M.K.J.: Methodology (equal); data curation (equal); funding acquisition (equal); supervision (equal), conceptualization (equal); investigation (equal); writing – original draft (equal); review and editing (equal). P.R.: Methodology (equal); data curation (equal); supervision (equal); conceptualization (equal); investigation (equal); writing – original draft (equal), review and editing (equal). L.H.: Methodology (equal); data curation (equal); funding acquisition (equal); supervision (equal); conceptualization (equal); investigation (equal); writing – original draft (equal), review and editing (equal). P.A.G.: Methodology (equal); supervision (equal); conceptualization (equal); investigation (equal); writing – original draft (equal); review and editing (equal). M.K.: Methodology (equal); data curation (equal), funding acquisition (equal), supervision (equal), conceptualization (equal); investigation (equal); writing – original draft (equal), review and editing (equal).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the local ethics commission in charge (Ethics Committee of the State Medical Association Rhineland-Palatinate, Mainz, Germany, ID: 837.156.16). Informed consent was obtained from all subjects. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jung, M.K., Hörnig, L., Raisch, P. et al. Odontoid fracture in geriatric patients — analysis of complications and outcome following conservative treatment vs. ventral and dorsal surgery. BMC Geriatr 23, 748 (2023). https://doi.org/10.1186/s12877-023-04472-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04472-2