Abstract
Background
Falls in long-term care are common. The aim of our study was to explore how medication use is associated with incidence of falls, related consequences, and all-cause mortality among long-term care residents.
Methods
Five hundred thirty two long-term care residents aged 65 years or older participated in this longitudinal cohort study in 2018–2021. Data on medication use were retrieved from medical records. Polypharmacy was defined as use of 5–10 medications and excessive polypharmacy as use of > 10 medications. The numbers of falls, injuries, fractures, and hospitalizations were collected from medical records over 12 months following baseline assessment. Participants were followed for three years for mortality. All analysis were adjusted for age, sex, Charlson Comorbidity Index, Clinical dementia rating, and mobility.
Results
A total of 606 falls occurred during the follow-up. Falls increased significantly with the number of medications used. Fall rate was 0.84/person-years (pyrs) (95% CI 0.56 to 1.13) for the non-polypharmacy group, 1.13/pyrs (95% CI 1.01 to 1.26) for the polypharmacy group, and 1.84/pyrs (95% CI 1.60 to 2.09) for the excessive polypharmacy group. Incidence rate ratio for falls was 1.73 (95% CI 1.44 to 2.10) for opioids, 1.48 (95% CI 1.23 to 1.78) for anticholinergic medication, 0.93 (95% CI 0.70 to 1.25) for psychotropics, and 0.91 (95% CI 0.77 to 1.08) for Alzheimer medication. The three-year follow-up showed significant differences in mortality between the groups, the lowest survival rate (25%) being in the excessive polypharmacy group.
Conclusion
Polypharmacy, opioid and anticholinergic medication use predicted incidence of falls in long-term care. The use of more than 10 medications predicted all-cause mortality. Special attention should be paid to both number and type of medications when prescribing in long-term care.
Similar content being viewed by others
Background
Half of long-term care residents fall annually, a proportion that is two to three times that of community-dwelling people [1]. Polypharmacy and several drug classes, such as psychotropics, opioids, and anticholinergics, have been shown to expose older adults to the risk of falls [2,3,4,5]. Recent studies have suggested that polypharmacy is also associated with all-cause mortality [6, 7].
A nationwide study from Korea found that in home-dwelling older adults an incrementally higher number of daily prescribed medications was associated with increasingly higher risk for mortality [6], whereas in the Newcastle 85 + study each additional medication prescribed was associated with a 3% increased risk of mortality [7].
Older adults living in long-term care are prone to polypharmacy due to several symptoms and multimorbidity [8,9,10]. Despite it being very common, polypharmacy lacks a universal definition [10]. The prevalence of polypharmacy varies between 10 and 90% according to the definition used and the age group and healthcare setting of the study [11]. The prevalence of polypharmacy in long-term care, defined as the use of 5 or more medications in the European SHELTER Study in 2012, was 50%, and for excessive polypharmacy, defined as the use of 10 or more medications, 24% [12]. A systematic review from 2015 found that 91%, 74%, and 65% of residents in long-term care facilities were taking more than 5, 9, and 10 medications, respectively [9].
Although the associations of medication use and polypharmacy with falls and mortality in long-term care have been studied extensively, evidence on the number of medications that currently predict adverse outcomes, including falls, is inconclusive [13]. A recent Australian prospective cohort study found that the optimal polypharmacy cut-point for predicting falls was 8.5 regularly used medications, whereas for mortality it was 9.5 and for all-cause and for fall-related hospitalizations 11.5 and 9.5 regularly used medications, respectively [13]. Some studies suggest that the use of two or more fall risk-increasing drugs could be an independent risk factor for falls instead of polypharmacy [14], whereas others have found polypharmacy to be an independent risk factor even after adjustments for fall risk-increasing drugs [15]. It has also been debated that maybe we should stop counting medications to define polypharmacy and concentrate more on identifying polypharmacy with unnecessary medications, defined as a medication having no indication, being ineffective, and/or a therapeutic duplication [16].
Previous research thus indicates that both polypharmacy and different medication classes can affect fall risk, injuries, fractures, hospitalizations and mortality in older adults, but the risk factors for falls in long-term care may differ from those in the population at large, and the association between falls, polypharmacy, and types of medications used may differ accordingly [17, 18].
The aim of this study was therefore not just to explore how polypharmacy, defined by the number of medications used is associated with the incidence of falls and related consequences in long-term care, but also to examine specific fall risk-increasing drugs and their association with falls, in order to broaden the existing evidence. Another aim was to examine the association between medication use and all-cause mortality in frail long-term care population living the last years of their life.
Methods
Study participants
Participants to this longitudinal study concerning nutrition, medications, frailty and falls were recruited from institutional settings in Helsinki in 2017. Altogether 532 volunteer residents were recruited from a random sample of 18 long-term care facilities. Baseline assessments and data collection was performed between February 2018 and August 2018. The participants were followed for 12 months for falls and for three years for mortality. Data on falls was collected in 2019. Mortality data was retrieved from the national registry in 2021.
Measures
Data on demographic factors, such as sex, age, and diagnoses, were collected from medical records. The Charlson Comorbidity Index [19] was calculated to assess each resident’s burden of comorbidity. Assessments were performed by trained study nurses and a geriatrician (HMR). The Barthel Index [20] was used to evaluate physical functioning. Mobility was assessed by one item in the 15D questionnaire [21] and categorized as follows: 1) I am able to walk normally (without difficulty) indoors, outdoors, and on stairs, 2) I am able to walk without difficulty indoors, but outdoors and/or on stairs I have slight difficulties, 3) I am able to walk without help indoors (with or without an appliance), but outdoors and/or on stairs only with considerable difficulty or with help from others, 4) I am able to walk indoors only with help from others, or 5) I am completely bedridden and unable to move about. Short Physical Performance Battery (SPPB) was performed to evaluate lower extremity function and mobility [22].
Phenotypic frailty status was defined by using modified Fried criteria [23], i.e. four criteria as follows: (1) unintentional weight loss was based on weight loss of ≥ 5% in the preceding year, (2) physical weakness was based on self-reported or care-staff evaluation of difficulty in carrying a bag of groceries, (3) exhaustion was based on self-reported or care-staff evaluation of low energy during the preceding four weeks, and (4) physical inactivity was based on the response to the question: “Do you/does the resident exercise regularly weekly?” A negative response meant physical inactivity. The sum of fulfilled criteria classified the person as “not frail” (no criteria), “pre-frail” (1–2 criteria), or “frail” (3–4 criteria).
To assess the severity of cognitive impairment, Mini-Mental State Examination (MMSE) [24] and Clinical Dementia Rating (CDR) [25] were performed.
Data on medication use were retrieved from medical records on the assessment day. All regularly used medications were noted. Combination products were considered as one medication. We defined non-polypharmacy as the use of < 5 medications, polypharmacy as the use of 5–10 medications, and excessive polypharmacy as the use of > 10 medications. Anticholinergic Risk Scale (ARS) was used to assess each medication’s anticholinergic potential. The ARS list contains 49 medications with anticholinergic properties [26]. Medications were classified using the Anatomical Therapeutic Chemical classification system [27]. Psychotropic medications included antipsychotics (N05A), antidepressants (N06A), anxiolytics (N05B), and hypnotics and sedatives (N05C). The use of Alzheimer medication (N06D) included cholinesterase inhibitors (N06DA) and/or memantine (N06DX01). Opioids (N02A) included both weak and strong opioids.
The primary outcome measure was the fall rate per person-year. Data on number of falls, injuries, fractures, and hospitalizations were collected from medical records during the 12-month follow-up. Falls were dated in the medical records, in the date of the event, as in long-term care facilities nurses write a report in the medical record on each resident every 8 h, before the end of each shift, where they report falls, injuries, fractures, and hospitalizations. The falls are also recorded in ‘Haipro’ patient safety report system. Mortality was retrieved from central records on March 31, 2021.
This study was performed to explore the relationship between nutrition, medications, frailty, dementia, neuropsychiatric symptoms and falls. The sample size calculation was performed to show about 10% difference in mortality between those who are malnourished and those not (with a power 80%, 5% type 1 error). We calculated that the size of about 550 could show clinically meaningful differences in many of our outcome measures.
Statistics
The descriptive statistics were presented as means with standard deviation (SD), as medians with interquartile range (IQR), or as counts with percentages. Statistical significance for the hypothesis of linearity across categories of regularly used medication levels was evaluated by using the Cochran-Armitage (Chi-squared) test for trend, ordered logistic regression model, Cuzick test, and an analysis of variance with an appropriate contrast. The number and incidence rate of falls were calculated assuming a Poisson distribution. Models included age, sex, Charlson Comorbidity Index, CDR, and mobility as covariates. A possible non-linear relationship between incidence of falls and regularly used medication was assessed by using a 3-knot-restricted cubic spline Poisson regression model. Adjusted Kaplan–Meier cumulative survival was estimated using two propensity score-based techniques, stratification and weighting (MMWS, marginal mean weighting through stratification) [28]. MMWS is an extension of propensity score matching that combines propensity score stratification and inverse probability of treatment weighting. Between-group differences in mortality were evaluated using log-rank test-adjusted survival curves. The normality of variables was evaluated graphically and by using the Shapiro–Wilk W test. Stata 17.0 (StataCorp LP, College Station, TX, USA) was used for statistical analyses.
Statement of ethics
The study protocol was approved by the Ethics Committee of the University of Helsinki. Written informed consent was obtained from each participant and in case of significant cognitive decline (CDR 2 or 3) from their closest proxy.
Results
Of 532 residents, 68 used ˂5 medications (non-polypharmacy group), 318 used 5–10 medications (polypharmacy group), and 146 used ˃10 medications (excessive polypharmacy group) (Table 1). The three groups did not differ in baseline demographic characteristics such as age or sex. The mean age across all groups was 85 years, and 80% of the participants were women.
However, the groups differed in the number of comorbidities, function, and mobility. The non-polypharmacy group had the lowest function, mobility, and comorbidity score (p < 0.001). There was also a significant difference in cognition. The non-polypharmacy group had the lowest MMSE (2.7 (mean 5.9)) and highest CDR, indicating more severe cognitive impairment.
The groups also differed significantly in psychotropic, anticholinergic, and Alzheimer medication use, the non-polypharmacy group naturally administered a lower number of each respective medication. No differences emerged in frailty status or neuropsychiatric symptoms. Median points in SPPB were zero in all three groups, but the range was 0–5 for the non-polypharmacy group, 0–10 for the polypharmacy group, and 0–7 for the excessive polypharmacy group.
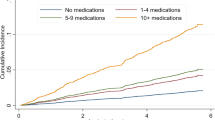
Incidence of falls and fall-related consequences
There was a total of 606 falls during the follow-up year. Altogether 194 residents, 36% of the participants, fell at least once. Falls increased significantly with the number of medications used (p < 0.001) (Fig. 1). Fall rate was 0.84/person-years (pyrs) (95% CI 0.56 to 1.13) for the non-polypharmacy group, 1.13/pyrs (95% CI 1.01 to 1.26) for the polypharmacy group, and 1.84/pyrs (95% CI 1.60 to 2.09) for the excessive polypharmacy group (Table 2). Incidence rate ratio for falls was 1.73 (95% CI 1.44 to 2.10) for opioid use, 1.48 (95% CI 1.23 to 1.78) for anticholinergic medication, 0.93 (95% CI 0.70 to 1.25) for psychotropics, and 0.91 (95% CI 0.77 to 1.08) for Alzheimer medication. All analyses were adjusted for age, sex, Charlson Comorbidity Index, CDR, and mobility as covariates.
There was a total of 121 injuries, 42 hospitalizations, and 20 fractures during the follow-up year. Polypharmacy was associated with injuries (p = 0.008) and hospitalization (p = 0.004) but not with fractures (p = 0.19).
All-cause mortality
The three-year follow-up showed significant differences in mortality between the groups (p = 0.039) (Fig. 2). The survival curves for two groups (< 5 drugs and > 10 drugs) crossed before one year follow-up. At the end of the follow-up, the survival was 29% in the non-polypharmacy group, 42% in the polypharmacy group, and 25% in the excessive polypharmacy group.
Discussion
Polypharmacy was associated with incidence of falls over a one-year follow-up in this long-term care population. Excessive polypharmacy, i.e. the use of over 10 medications, was associated with a significant increase in incidence of falls. Fall risk seemed to be associated to opioid and anticholinergic medication use. Polypharmacy was also associated with fall-related consequences, such as injuries and hospitalization, but not with fractures. The three-year follow-up showed significant differences in all-cause mortality between the different polypharmacy groups, with the lowest survival rate (25%) in the excessive polypharmacy group.
Both polypharmacy (60%) and excessive polypharmacy (27%) were common among our participants. Their prevalence was similar to that in the European SHELTER Study in 2012, where the figure for polypharmacy was 50% and for excessive polypharmacy 23% [12], but markedly lower than in a review from 2015 [9]. A more recent register-based prospective cohort study also found that living in a nursing home seemed to be associated with an increased risk of developing incident polypharmacy and excessive polypharmacy over time [29].
Of our participants, 36% fell at least once during the follow-up year. Regarding the prevalence of falls, the results of our study are in line with the WHO Global Report on Falls, according to which 30–50% of people living in long-term care fall each year [30]. The prevalence of falls is also consistent with other recent findings from long-term care. In an Italian study from 2020, 27% of the residents fell [31], whereas in a Canadian study 56% of their sample fell at least once [32].
Polypharmacy and especially excessive polypharmacy predicted falls in our study. The fall risk rose exponentially when using more than 10 medications. The results are in accord with other recent publications. In a UK study among home-care residents, for every additional drug prescribed the odds of falling increased by 1.06 times [33], whereas among Swedish community-dwelling older adults the number of medications was associated with an increased risk of fall injury in a dose–response fashion and using 10 or more medications was associated with an almost two-fold higher risk [15]. In an Australian study, no optimal cut-point for predicting falls or mortality over two years was identified, but the use of 11.5 regular medications best predicted all-cause hospitalization, whereas the use of 9.5 regular medications best predicted fall-related hospitalization [13].
People with polypharmacy are significantly more likely to be prescribed anticholinergic drugs [34]. There is evidence that use of anticholinergic medications is associated with increased risk of falls [35,36,37]. Also in our study, a significantly increasing trend was observed in the mean number of anticholinergic drugs along with increasing polypharmacy. Although we did not determine the actual anticholinergic burden in this study, the burden is likely to increase as the number of anticholinergics rises. Further, a greater anticholinergic burden has been associated with a higher risk of falls [38].
The highest incidence rate ratio for falls was found for opioid use, whereas the incidence rate ratio for psychotropic use was surprisingly low. The prevalence of psychotropic use has decreased over the last 14 years in long-term care in Helsinki, but at the same time the rates of opioid use have increased [39]. Similar findings have been reported from other countries [40, 41]. This is concerning as the results of our study support earlier findings that opioids seem to have major effect sizes as regards the risk of falls, fall-related injuries, and fractures [5, 42, 43].
The highest survival rate was found in the polypharmacy group (42%), whereas the lowest survival rate was in the excessive polypharmacy group (25%). A previous study has also found excessive polypharmacy to be an indicator of five-year mortality in older persons living at home [44]. In the non-polypharmacy group, the survival rate was 29%. Almost half of the non-polypharmacy group were unable to move, being practically bedridden, showing signs of end of life. Residents with a short life expectancy may have had long-term preventative medications deprescribed, which may explain a lower survival rate in the beginning of the follow up and neutralize a possible association between polypharmacy and mortality [45]. In recent years interventions to decrease polypharmacy and inappropriate prescribing have increasingly been developed. A systematic review from 2020 found that deprescribing in older patients with life‐limiting illness and short life expectancy can improve medication appropriateness and has the potential for enhancement of several clinical outcomes while also being cost-saving [46], while in other more recent studies no differences in mortality, falls or admissions have been reported [47,48,49].
This study has several strengths. All residents were thoroughly assessed by well-trained study nurses and a geriatrician. A large number of well-validated variables was used. The data collection instruments and the methodology used led to high validity of the data. The study sample is representative of long-term care residents in terms of age, sex, mobility, and dementia status. However, the study was conducted in only one city (Helsinki, Finland) so the results may not be generalizable to all long-term care residents worldwide. The sample size can be considered large for a frail, long-term care population since older people with multiple chronic conditions or frailty are often excluded from studies. It is also a significant strength that medication data were retrieved from medical records, thus representing medications actually administered to residents.
The study also has some limitations that should be considered when interpreting the results. As a longitudinal follow-up study, we cannot rule out unknown confounders having an effect on falls or mortality. One limitation is that the medication list was assessed only at baseline. The determinants and participants' medications may change over time, and this could not be taken into account in our study. However, the medications lists in long-term care settings tend to be constant over long periods of time. The same holds true for the determinants of falls. However, the medication lists tend to shorten as the older residents become frailer and more severe in respect to their dementia over time. Thus, even though the medication list is reduced—which may dilute the findings—the baseline medications remain as determinants of falls. When interpreting the association between falls and polypharmacy, we must also consider confounding by indication and confounding by multimorbidity. However, all our analysis were adjusted for age, gender, comorbidities, dementia stage, and mobility. Another limitation is that the information on falls was retrieved from medical records. Previous studies have highlighted that the most reliable method for recording falls is a daily fall diary [50]. Thus, our results might underestimate the number of falls. However, Finnish nurses are well instructed to report all falls and their consequences in their daily records.
Conclusion
Our results indicate the importance of excessive polypharmacy, i.e. the use of more than 10 medications, as an indicator of falls and all-cause mortality in a frail long-term care population. Rather than polypharmacy, excessive polypharmacy might be the optimal risk indicator in long-term care populations. This difference compared with community-dwelling older adults may be due to differences in multimorbidity as well as frailty, mobility and cognitive status. The results also confirm that medication optimizing is not merely linked to the number of medications. The associations found between polypharmacy status, falls, and all-cause mortality call for interventions to ensure optimal medication for older adults. Special attention should be paid to both number and type of medication when prescribing in long-term care. Further research is needed to determine when deprescribing interventions in long term care have an impact on falls, hospitalizations, and mortality.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due but are available from the corresponding author on reasonable request.
Abbreviations
- ARS:
-
Anticholinergic Risk Scale
- CDR:
-
Clinical Dementia Rating
- MMSE:
-
Mini-Mental State Examination
- NPI:
-
Neuropsychiatric Inventory
- SPPB:
-
Short Physical Performance Battery
References
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35 Suppl 2:ii37-ii41. https://doi.org/10.1093/ageing/afl084.
Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc. 2014;62(12):2261–72. https://doi.org/10.1111/jgs.13153.
de Vries M, Seppala LJ, Daams JG, van de Glind EMM, Masud T, van der Velde N, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: I. Cardiovascular Drugs. J Am Med Dir Assoc. 2018 Apr;19(4):371.e1–371.e9. https://doi.org/10.1016/j.jamda.2017.12.013.
Seppala LJ, Wermelink AMAT, de Vries M, Ploegmakers KJ, van de Glind EMM, Daams JG, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: II. Psychotropics J Am Med Dir Assoc. 2018;19:371.e11-371.e17. https://doi.org/10.1016/j.jamda.2017.12.099.
Seppala LJ, van de Glind EMM, Daams JG, Ploegmakers KJ, de Vries M, Wermelink AMAT, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-analysis: III. Others J Am Med Dir Assoc. 2018;19:372.e1-372.e8. https://doi.org/10.1016/j.jamda.2017.12.099.
Chang TI, Park H, Kim DW, Jeon EK, Rhee CM, Kalantar-Zadeh K, et al. Polypharmacy, hospitalization, and mortality risk: a nationwide cohort study. Sci Rep. 2020;10(1):18964. https://doi.org/10.1038/s41598-020-75888-8.
Davies LE, Kingston A, Todd A, Hanratty B. Is polypharmacy associated with mortality in the very old: findings from the Newcastle 85+ Study. Br J Clin Pharmacol. 2022 Jan 3. https://doi.org/10.1111/bcp.15211. Epub ahead of print.
Bronskill SE, Gill SS, Paterson JM, Bell CM, Anderson GM, Rochon PA. Exploring variation in rates of polypharmacy across long term care homes. J Am Med Dir Assoc. 2012;13(3):309.e15-21. https://doi.org/10.1016/j.jamda.2011.07.001.
Jokanovic N, Tan EC, Dooley MJ, Kirkpatrick CM, Bell JS. Prevalence and factors associated with polypharmacy in long-term care facilities: a systematic review. J Am Med Dir Assoc. 2015;16(6):535.e1-12. https://doi.org/10.1016/j.jamda.2015.03.003.
Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med. 2021;12(3):443–52. https://doi.org/10.1007/s41999-021-00479-3.
Khezrian M, McNeil CJ, Murray AD, Myint PK. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf. 2020;11:2042098620933741. https://doi.org/10.1177/2042098620933741.
Onder G, Liperoti R, Fialova D, Topinkova E, Tosato M, Danese P, et al. Polypharmacy in nursing home in Europe: results from the SHELTER study. J Gerontol A Biol Sci Med Sci. 2012;67(6):698–704. https://doi.org/10.1093/gerona/glr233.
Wang KN, Tan ECK, Ilomäki J, Gilmartin-Thomas JFM, Sluggett JK, Cooper T, et al. What is the Best Definition of Polypharmacy for Predicting Falls, Hospitalizations, and Mortality in Long-Term Care Facilities? J Am Med Dir Assoc. 2021;22(2):470–1. https://doi.org/10.1016/j.jamda.2020.10.040.
Zia A, Kamaruzzaman SB, Tan MP. The consumption of two or more fall risk-increasing drugs rather than polypharmacy is associated with falls. Geriatr Gerontol Int. 2017;17(3):463–70. https://doi.org/10.1111/ggi.12741.
Laflamme L, Monárrez-Espino J, Johnell K, Elling B, Möller J. Type, number or both? A population-based matched case-control study on the risk of fall injuries among older people and number of medications beyond fall-inducing drugs. PLoS One. 2015;10(3):e0123390. https://doi.org/10.1371/journal.pone.0123390.
Hanlon JT, Hajjar ER. Isn’t It Time We Stop Counting the Number of Drugs to Define Polypharmacy in This New Era of Deprescribing and What Related Outcomes Should Be Measured? J Am Med Dir Assoc. 2018;19(8):644–5. https://doi.org/10.1016/j.jamda.2018.04.010.
Eriksson S, Gustafson Y, Lundin-Olsson L. Risk factors for falls in people with and without a diagnose of dementia living in residential care facilities: a prospective study. Arch Gerontol Geriatr. 2008;46(3):293–306. https://doi.org/10.1016/j.archger.2007.05.002.
Rapp K, Becker C, Cameron ID, König HH, Büchele G. Epidemiology of falls in residential aged care: analysis of more than 70,000 falls from residents of bavarian nursing homes. Am Med Dir Assoc. 2012;13(2):187.e1-6. https://doi.org/10.1016/j.jamda.2011.06.011.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–83.
Mahoney FI, Barthel DW. Functional evaluation: The Barthel index. Md State Med J. 1965;14:61–5.
Sintonen H. The 15D instrument of health-related quality of life: Properties and applications. Ann Med. 2001;33:328–36.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85-94.
Perttila N, Pitkala K, Kautiainen H, Tilvis R, Strandberg T. Various Diagnostic Measures of Frailty as Predictors for Falls, Weight Change, Quality of Life, and Mortality among Older Finnish Men. J Frailty Aging. 2017;6:188–94. https://doi.org/10.14283/jfa.2017.26.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72.
Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168:508–13.
WHO Collaborating Centre for Drug Statistics Methodology. The Anatomical Therapeutic Chemical Classification System. ATC/DDD Index 2020. Available at: https://www.whocc.no/atc_ddd_index/. Accessed on December 1, 2021.
Linden A. Combining propensity score-based stratification and weighting to improve causal inference in the evaluation of health care interventions. J Eval Clin Pract. 2014;20(6):1065–71. https://doi.org/10.1111/jep.12254.
Morin L, Johnell K, Laroche ML, Fastbom J, Wastesson JW. The epidemiology of polypharmacy in older adults: register-based prospective cohort study. Clin Epidemiol. 2018;10:289–98. https://doi.org/10.2147/CLEP.S153458.
World Health Organization. (2008). WHO global report on falls prevention in older age. World Health Organization. https://apps.who.int/iris/handle/10665/43811.
Castaldo A, Giordano A, Antonelli Incalzi R, Lusignani M. Risk factors associated with accidental falls among Italian nursing home residents: A longitudinal study (FRAILS). Geriatr Nurs. 2020;41(2):75–80. https://doi.org/10.1016/j.gerinurse.2019.06.003.
Cameron EJ, Bowles SK, Marshall EG, Andrew MK. Falls and long-term care: a report from the care by design observational cohort study. BMC Fam Pract. 2018;19(1):73. https://doi.org/10.1186/s12875-018-0741-6.
Izza MAD, Lunt E, Gordon AL, Gladman JRF, Armstrong S, Logan P. Polypharmacy, benzodiazepines, and antidepressants, but not antipsychotics, are associated with increased falls risk in UK care home residents: a prospective multi-centre study. Eur Geriatr Med. 2020;11(6):1043–50. https://doi.org/10.1007/s41999-020-00376-1.
Lee EK, Lee YJ. Prescription patterns of anticholinergic agents and their associated factors in Korean elderly patients with dementia. Int J Clin Pharm. 2013;35:711–8.
Mehdizadeh D, Hale M, Todd O, Zaman H, Marques I, Petty D, et al. Associations Between Anticholinergic Medication Exposure and Adverse Health Outcomes in Older People with Frailty: A Systematic Review and Meta-analysis. Drugs Real World Outcomes. 2021;8(4):431–58. https://doi.org/10.1007/s40801-021-00256-5.
Tan SX, Cameron SC, Sam LM, Eigeland H, Hay K, Eeles E, et al. A delicate balance: Psychotropic polypharmacy and anti-cholinergic use are correlated with fall incidence in Australian inpatients with dementia. Aging Med (Milton). 2021;4(3):193–200. https://doi.org/10.1002/agm2.12175.
Stewart C, Taylor-Rowan M, Soiza RL, Quinn TJ, Loke YK, Myint PK. Anticholinergic burden measures and older people’s falls risk: a systematic prognostic review. Ther Adv Drug Saf. 2021;12:20420986211016644. https://doi.org/10.1177/20420986211016645.
Suehs BT, Caplan EO, Hayden J, Ng DB, Gaddy RR. The Relationship Between Anticholinergic Exposure and Falls, Fractures, and Mortality in Patients with Overactive Bladder. Drugs Aging. 2019;36(10):957–67. https://doi.org/10.1007/s40266-019-00694-5.
Roitto HM, Kautiainen H, Aalto UL, Öhman H, Laurila J, Pitkälä KH. Fourteen-Year Trends in the Use of Psychotropic Medications, Opioids, and Other Sedatives Among Institutionalized Older People in Helsinki. Finland J Am Med Dir Assoc. 2019;20(3):305–11. https://doi.org/10.1016/j.jamda.2018.12.022.
Gerlach LB, Olfson M, Kales HC, Maust DT. Opioids and Other Central Nervous System-Active Polypharmacy in Older Adults in the United States. J Am Geriatr Soc. 2017;65(9):2052–6. https://doi.org/10.1111/jgs.14930.
Gustafsson M, Lövheim H, Sjölander M. Pharmacological Pain Treatment in 2012 and 2017 Among Older People with Major Neurocognitive Disorder. Drugs Aging. 2021;38(11):1017–23. https://doi.org/10.1007/s40266-021-00897-9.
Perttila NM, Öhman H, Strandberg TE, Kautiainen H, Raivio M, Laakkonen ML, et al. Effect of Exercise on Drug-Related Falls Among Persons with Alzheimer’s Disease: A Secondary Analysis of the FINALEX Study. Drugs Aging. 2018;35(11):1017–23. https://doi.org/10.1007/s40266-018-0594-7.
Yoshikawa A, Ramirez G, Smith ML, Foster M, Nabil AK, Jani SN, et al. Opioid Use and the Risk of Falls, Fall Injuries and Fractures among Older Adults: A Systematic Review and Meta-Analysis. J Gerontol A Biol Sci Med Sci. 2020;75(10):1989–95. https://doi.org/10.1093/gerona/glaa038.
Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S. Polypharmacy status as an indicator of mortality in an elderly population. Drugs Aging. 2009;26(12):1039–48.
O’Mahony D, O’Connor MN. Pharmacotherapy at the end-of-life. Age Ageing. 2011;40(4):419–22. https://doi.org/10.1093/ageing/afr059.
Shrestha S, Poudel A, Steadman K, Nissen L. Outcomes of deprescribing interventions in older patients with life-limiting illness and limited life expectancy: A systematic review. Br J Clin Pharmacol. 2020;86(10):1931–45. https://doi.org/10.1111/bcp.14113.
Cateau D, Ballabeni P, Niquille A. Effects of an interprofessional deprescribing intervention in Swiss nursing homes: the Individual Deprescribing Intervention (IDeI) randomised controlled trial. BMC Geriatr. 2021;21(1):655. https://doi.org/10.1186/s12877-021-02465-7.
Kornholt J, Feizi ST, Hansen AS, Laursen JT, Reuther LØ, Petersen TS, et al. Effects of a comprehensive medication review intervention on health-related quality of life and other clinical outcomes in geriatric outpatients with polypharmacy: A pragmatic randomized clinical trial. Br J Clin Pharmacol. 2022;88(7):3360–9. https://doi.org/10.1111/bcp.15287.
Salari P, O'Mahony C, Henrard S, Welsing P, Bhadhuri A, Schur N, et al. Cost-effectiveness of a structured medication review approach for multimorbid older adults: Within-trial analysis of the OPERAM study. PLoS One. 2022;17(4):e0265507. https://doi.org/10.1371/journal.pone.0265507.
Hannan MT, Gagnon MM, Aneja J, Jones RN, Cupples LA, Lipsitz LA, et al. Optimizing the Tracking of Falls in Studies of Older Participants: Comparison of Quarterly Telephone Recall With Monthly Falls Calendars in the MOBILIZE Boston Study. Am J Epidemiol. 2010;171:1031–6.
Funding
Open Access funding provided by University of Helsinki including Helsinki University Central Hospital. The authors did not receive support from any organization for the submitted work. Open access funding provided by University of Helsinki.
Author information
Authors and Affiliations
Contributions
KP is the project leader for the study that generated data for this article. HMR and KS participated in data collection. HK, KP, KS and HMR performed the statistical analysis and drafted the manuscript. All authors took part in the design of the study, as well as read and critically reviewed the drafted manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Participation in the present study was voluntary and data collection took part upon informed written consent. The study protocol was approved by the Ethics Committee of the University of Helsinki. All procedures performed were in accordance with the ethical standards of the Ethics Committee of the University of Helsinki and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Roitto, HM., Aalto, U.L., Öhman, H. et al. Association of medication use with falls and mortality among long-term care residents: a longitudinal cohort study. BMC Geriatr 23, 375 (2023). https://doi.org/10.1186/s12877-023-04096-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04096-6