Abstract
Background
Falls are a major public health problem affecting millions of older adults each year. Little is known about FRID prescribing behaviors after injurious falls occur. The primary objective of this study was to investigate whether an injurious fall is associated with being prescribed a new FRID.
Methods
We conducted a cross-sectional analysis using data from the National Ambulatory Medical Care Survey (2016). We included visits from patients age ≥ 65 years and classified visits based on presence of an injurious fall. The outcome of interest was prescription of new FRID between those with and without an injurious fall. Multivariable logistic regression weighted for sampling and adjusted for demographics, health history and other medications was used. Age and Alzheimer’s disease were examined as potential effect measure modifiers. Odds ratios and 95% confidence intervals were reported. Bayes factor upper bounds were also reported to quantify whether the data were better predicted by the null hypothesis or the alternative hypothesis.
Results
The sample included 239,016,482 ambulatory care visits. 5,095,734 (2.1%) of the visits were related to an injurious fall. An injurious fall was associated with a non-statistically significant increase in odds of at least one new FRID prescription: adjusted OR = 1.6 (95% CI 0.6, 4.0). However, there was non-statistically significant evidence that the association depended on patient age, with OR = 2.6 (95% CI 0.9, 7.4) for ages 65–74 versus OR = 0.4 (95% CI 0.1, 1.6) for ages ≥ 75. In addition to age, Alzheimer’s disease was also identified as a statistically significant effect measure modifier, but stratum specific estimates were not determined due to small sample sizes.
Conclusions
Ambulatory care visits involving an injurious fall showed a non-statistically significant increase in odds of generating a new FRID prescription, but this association may depend on age.
Similar content being viewed by others
Background
Falls are a major public health problem that affects millions of people in the United States each year. Older adults (specifically those 65 years of age and older) are disproportionately affected, with one out of four older adults experiencing a fall each year according to data from the Centers for Disease Control and Prevention [1]. Approximately 20% of these falls result in a serious injury, most often a fractured or broken bone or a traumatic brain injury (TBI) [1]. Injurious falls initiate a cascading effect that can negatively impact the patient’s physical and mental health. For example, patients experiencing hip fractures often require orthopedic surgery, which puts them at increased short-term risk for infection and bleeding, as well as increased long-term risk for deep venous thrombosis (DVT) and muscle atrophy due to prolonged immobility [2]. In addition, patients often have a fear of falling a second time, which can cause them to be less mobile, therefore compounding the probability of a subsequent fall [1, 3, 4]. The economic costs associated with injurious falls place an enormous burden on the healthcare system. Each year, approximately $50 billion and $754 million is spent on non-fatal and fatal fall injuries, respectively [5].
Numerous risk factors for falls have been elucidated, and they are generally subclassified as extrinsic or intrinsic. Extrinsic factors are related to the physical environment (i.e., dim lighting, improper use of assistive devices, etc.) and are often modifiable. Intrinsic factors are related to patient-specific factors, such as advanced age, history of previous falls, chronic conditions, and the physiologic effects of medication use [1, 5,6,7,8]. More specifically, medications belonging to certain medication classes can independently increase fall risk and are known as fall-risk-increasing drugs (FRIDs).
The CDC implemented a program called Stopping Elderly Accidents, Deaths, & Injuries (STEADI)-Rx that is designed to help pharmacists identify medications of concern [9]. The American Geriatrics Society (AGS) 2019 Updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults (hereafter “Beers Criteria”) created a similar list of medications and medication classes to avoid in patients with a history of falls or fractures [10]. These medication classes include anticonvulsants, antidepressants, antihypertensives, antipsychotics, antispasmodics, benzodiazepines, opioids, and sedative hypnotics [11,12,13]. Polypharmacy, which is generally defined as a medication regimen consisting of five or more medications, is also associated with increased fall risk, with one study estimating a 7% increase in fall risk with every additional medication reported [14].
While FRID classes have been elucidated, little is known about FRID prescribing behaviors after injurious falls occur. The primary objective of this study was to examine prescribing behaviors occurring during a visit for an injurious fall and to investigate whether an injurious fall is associated with being prescribed a new FRID. The secondary objective of this study is to describe the pharmacist’s role in fall prevention. Analyses described herein are based on prescribing behaviors ascertained from the 2016 National Ambulatory Medical Care Survey (NAMCS), which was the most recently available data at the time data analysis was conducted and finalized in April 2021.
Methods
Study population and data source
NAMCS is a nationally representative cross-sectional survey that provides information about the utilization of ambulatory medical care services in the United States. Each participating office-based physician is assigned to a 1-week reporting period randomly, and a systematic random sample of visits is recorded during that timeframe using a computerized form [15]. Data provided by participating physicians include patient characteristics such as demographic information; diagnoses and chronic conditions (including total number of chronic conditions); services ordered or provided; laboratory values; and treatments, including up to 30 medication therapies. NAMCS is a publicly available, deidentified data source. The surveys are administered by the National Center for Health Statistics that is part of the Centers for Disease Control and Prevention (CDC) in the US. The data collected are made publicly available by the CDC along with sampling weights and guidance in applying the weights to obtain nationally representative estimates. A detailed description of NAMCS sampling methodology is available from the National Center for Health Statistics [16]. The study was exempt from Institutional Review Board approval at the University of Kentucky. All methods were performed in accordance with the relevant guidelines and regulations.
Eligibility criteria
For this study, we included visits for patients age 65 years or older, as available lists of potentially inappropriate medications (PIMs) are typically based on this age criterion [9, 10]. Adults less than 65 years of age were excluded.
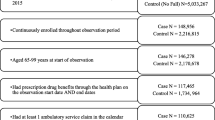
Identification of injurious falls
We created an indicator to identify the presence of injurious falls (Fig. 1). Under the “Injury” section on the NAMCS standard form, the physician selected whether the visit was related to an injury/trauma, overdose/poisoning, or adverse effect of medical/surgical treatment. For visits related to injury/trauma, we then manually selected each injury caused by a fall from the free-text fields for the cause1, cause2, and cause3 variables. We also investigated the “Reason for Visit” section on the NAMCS standard form when the causes of injury were left blank. We identified reasons for visits related to probable falls in older adults (e.g., fracture/dislocation of arm or wrist). Please see additional file 1: Appendix 1 for the values corresponding to injurious falls identified in the cause of injury variables (CAUSE1, CAUSE2, and CAUSE3), as well as the reason for visit variables (RFV1, RFV2, RFV3, RFV4, and RFV5).
Identification of FRIDs and Polypharmacy
The survey data collection form allows up to 30 medications to be reported. The physician indicates whether the medication was new or continued at the time of the visit. The medications are then assigned to up to four therapeutic classes using the Lexicon Plus® database and the Multum classification system [17]. Based on the lists provided by STEADI-Rx and the Beers Criteria, we created new, continued, and new or continued indicator variables for each medication class of concern: anticonvulsants, antidepressants, antihypertensives, antipsychotics, antispasmodics, benzodiazepines, opioids, and sedative hypnotics [9, 10]. New medications were those prescribed at the visit, and continued medications were those already part of the patient’s medication regimen prior to the visit. See additional file 1: Appendix 2 for the Multum therapeutic class codes corresponding to the medication classes of concern.
In addition to the indicator variables for each medication class of concern, we also created an indicator variable to show whether any new, continued, or new or continued FRID belonging to any FRID class listed above was present. We also created continuous variables to indicate the total number of new, continued, and new or continued FRIDs present.
Lastly, we created an indicator variable to identify the presence of poly-FRID. Poly-FRID is defined as a medication regimen consisting of two or more FRIDs and has been shown to be an independent risk factor for falls [18]. For the poly-FRID variable, we only considered continued medications in order to assess medication use prior to the visit.
Covariates (potential confounders)
We conducted a literature review to identify important risk factors for falls [8, 19,20,21]. Figure 2 lists potential confounders (i.e., shared causes of falls and medication use), whether or not they were available in the NAMCS data, and how they were defined if included in the analyses. We included Alzheimer’s disease, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), arthritis, asthma, depression, diabetes mellitus, heart attack/angina, obesity, polypharmacy, and stroke in the multivariable logistic model, based on the minimally sufficient adjustment set identified by the hypothesized causal diagram. Chronic pain, impaired vision, incontinence, insomnia, and orthostatic hypotension were also part of the minimally sufficient adjustment set but were not available from the NAMCS data.
Potential Confounders
Minimal sufficient adjustment set for estimating the total effect of visit for injurious fall on new FRID: Alzheimer’s disease, CKD, COPD, arthritis, asthma, chronic pain, depression, diabetes, heart attack/angina, impaired vision, incontinence, insomnia, obesity, orthostatic hypotension, polypharmacy, stroke. *Chronic pain, impaired vision, incontinence, insomnia, and orthostatic hypotension not available, **CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease
Data Analyses
We applied NAMCS sampling weights to account for complex sampling design and to generate a nationally representative sample of ambulatory care visits for patients 65 years of age or older [16]. Proportions were reported for nominal variables of interest. Continuous variables of interest were described using the mean and standard error (SE). Chi-squared tests were used to compare characteristics between the injurious fall group and the non-fall group, as appropriate. To assess whether new FRID prescriptions were more or less likely between the two groups, multivariable logistic regression was used. Age (65–74 years versus 75 years and older, per NAMCS coding) was examined as a potential effect measure modifier, given the dramatic increase in fall-related mortality rate in persons 75 years of age and older [22]. Adjusted odds ratios (OR) and 95% confidence intervals (95% CI) were reported, with p< 0.05 considered statistically significant. Bayes factor upper bounds were reported to quantify whether the data were better predicted by the null hypothesis or the alternative hypothesis [23]. Alzheimer’s disease was examined as a potential effect measure modifier, as certain medications (i.e., psychotropics with anticholinergic properties) can both exacerbate cognitive impairment and increase the risk for subsequent falls. However, no model estimates are presented due to sparse data [24, 25].
Results
Baseline demographics
A total of 239,016,482 ambulatory care visits occurring among patients 65 years or older were included in the analyses (Table 1). Of those, 5,095,734 (2.1%) visits were related to an injurious fall. The mean (SE) age for the 239,016,482 adults 65 years of age or older represented by study visits was 74.8 (SE 0.2). Non-Hispanic white patients made up 78.1% of the visits. The majority of visits were made by women (55.9%). Prevalence of chronic conditions recorded at the time of the visit was similar between those with and without injurious falls (mean of 2.2 (0.4) versus 2.2 (0.1). Chronic conditions [8, 19,20,21] were also similar between the two groups, with the exception of COPD and Alzheimer’s disease, which were more prevalent in the injurious fall group (see Table 1 below).
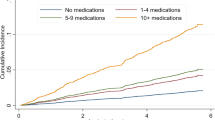
Medication use
Patients experiencing an injurious fall had a non-statistically significant higher mean (SE) number of continued medications (defined as medications in their regimens prior to the visit) than those without falls (5.9 (0.9) versus 4.4 (0.4); p = 0.096). Most (56.8% [95% CI 46.4%, 67.2%]) patients in the injurious fall group had at least one continued FRID as part of their prescription regimen, versus 49.9% [95% CI 44.9%, 54.8%] of patients in the non-fall group. A larger percentage of patients in the injurious fall group experienced polypharmacy (50.2% versus 39.4%; p = 0.145) and poly-FRID (44.9% versus 36.8%; p = 0.228), though these differences were non-statistically significant. In the injurious fall group, antihypertensives were the most often continued FRID medication class (44.9%), followed by opioids (14.3%), antidepressants (13.7%), anticonvulsants (13.1%), sedative hypnotics (10.3%), benzodiazepines (9.0%), antispasmodics (4.4%), and antipsychotics (0.7%). The frequencies were similar in the non-fall group.
Prescribing behaviors at the visit
Antihypertensive medications, newly prescribed at the time of the visit, were significantly more prevalent in the non-fall group compared to the injurious fall group (see Table 2 at the end of the text: 5.7% versus 0.4%; p < 0.001). Newly prescribed anticonvulsants, antipsychotics, and sedative hypnotics were also more frequent in the non-fall group. In contrast, new antidepressants and antispasmodics were more frequently prescribed in the injurious fall group. Of note, no new anticonvulsants, antipsychotics, benzodiazepines, or opioids were prescribed to the injurious fall group and no new opioids were prescribed to the non-fall group. Patients in the injurious fall group were more likely to be prescribed a new FRID compared to the non-fall group (15.6% [CI 2.3%, 28.8%] versus 10.5% [95% CI 8.9%, 12.2%]), although this difference was modest in magnitude and not statistically significant. See Figs. 3 and 4 for most frequently prescribed (any) new and continued FRID classes by group.
In the logistic regression model adjusted for age at visit, polypharmacy, and presence of chronic conditions (cerebrovascular disease, CKD, arthritis, depression, diabetes, coronary artery disease, asthma, COPD, Alzheimer’s disease, osteoporosis, and obesity), an injurious fall was associated with 1.6 times increased odds (95% CI 0.6, 4.0; p = 0.3058 and Bayes factor upper bound = 1.0153) of being prescribed at least one new FRID. See Table 3 below.
The relation of an injurious fall with the odds of being prescribed any new FRID differed by age, though these differences were non-statistically significant. For adults aged 65 to 74 years, an injurious fall was associated with a non-statistically significant 2.6-fold increase in odds (95% CI 0.9, 7.4; p = 0.0687 and Bayes factor upper bound = 1.9996) of being prescribed at least one new FRID. For patients aged 75 years of age or older, an injurious fall was associated with non-statistically significant decreased odds, OR 0.40 (95% CI 0.1, 1.6; p = 0.2220 and Bayes factor upper bound = 1.1010) of being prescribed at least one new FRID. See Table 3 below.
Discussion
In this cross-sectional analysis of a nationally representative sample of ambulatory care visits occurring in the United States among adults age 65 years or older, we observed that an injurious fall showed a non-statistically significant increase in odds of being prescribed any new FRID, but these results differed by age. Patients age 65 to 74 years presenting with an injurious fall were more likely to be prescribed any new FRID, in comparison to patients age 75 years or older, who were less likely to be prescribed any new FRID. Though the results were not statistically significant based on p-values, the Bayes factor upper bound of 1.9996 for adults 65–74 years indicates the alternative hypothesis (meaning there is a difference in likelihood of being prescribed a new FRID between the two groups) is at most twice as likely as the null hypothesis. In addition, the trends in data suggest possible clinical significance. One might reason that an ambulatory care physician’s level of concern is increased in a patient 75 years or older (as opposed to a younger patient 65–74 years) after an injurious fall. It is possible that increasing frailty often seen with advancing age may lead the provider to place greater weight on the risk of a subsequent fall as opposed to the potential benefits of a newly prescribed FRID (such as better blood pressure control with a new antihypertensive medication) in this higher age group. In contrast, providers may be more willing to risk a subsequent fall in the group of younger patients (age 65–74 years) given increased life expectancy and the potential to improve chronic conditions and associated long-term health outcomes.
Out of the entire sample (all visits with patients 65 years or older), new antidepressants and new antispasmodics were the most frequently prescribed FRID medication classes at the visits occurring due to injurious falls. Patients frequently experienced polypharmacy, which was defined as 5 or more continued medications. Poly-FRID, which was defined as 2 or more continued FRID medications, was also frequently experienced by all patients regardless of fall group.
The results from this cross-sectional analysis have concerning implications for health outcomes in older adults, especially considering the frequent prescribing of new antidepressants and antispasmodics, as well as the widespread issue of polypharmacy across both groups. A meta-analysis found that use of antidepressants in older adults was associated with a 1.4 times increased risk of falls after adjusting for potential confounders [12]. Antispasmodics are also widely understood to increase fall risk, especially in elderly patients, due to their depressive effects (dizziness, drowsiness, and hypotension) on the central nervous system [26]. Antihypertensives, anticonvulsants, antipsychotics, antispasmodics, benzodiazepines, opioids, and sedative hypnotics have also been shown to increase fall risk and should therefore be avoided when possible, especially in patients acutely experiencing an injurious fall [11,12,13]. Lastly, a meta-analysis of extant studies suggests that polypharmacy is associated with an increased odds of falling (pooled OR 1.75 [1.27, 2.41]) [13]. In addition, the results from this cross-sectional analysis are similar to a recent systematic review that concluded, with limited evidence, that there is a high prevalence of FRID use among older adults who have experienced a fall-related injury and no reduction in overall FRID use following the fall-related healthcare encounter [27].
While the data suggest concerning implications in some realms, there are also positive trends to be noted. First, opioid prescribing was not higher in the injurious group (which might be anticipated given potential pain from the injuries), suggesting that providers may be considering subsequent fall risk in their prescribing practices. In addition, the significant increase in prescription of antihypertensives in the non-fall group likely reflects appropriate ambulatory care prescribing practices (i.e., management of hypertension and prevention of negative cardiovascular health outcomes); the lower frequency in the injurious fall group suggests providers may be balancing the risk of a subsequent fall with the potential benefit of managing chronic conditions.
Pharmacists are uniquely positioned to implement falls-prevention interventions in the older adult population. As one of the most accessible healthcare providers, pharmacists can 1) assist with comprehensive medication management (CMM); 2) provide patients with appropriate education regarding medications that increase fall risk; and 3) counsel patients on non-pharmacologic tips to decrease fall risk.
The CMM is perhaps one of the most effective ways for pharmacists to serve as a liaison between patients and their other health care providers. It is defined as “a patient centered approach to optimizing medication use and improving patient health outcomes that is delivered by a clinical pharmacist working in collaboration with the patient and other health care providers.” [28] During this process, the pharmacist evaluates each of the patient’s medications (including prescription, over-the-counter, and vitamins/herbal supplements) for appropriateness, safety, and efficacy. When the pharmacist identifies a potential issue, they work with the prescriber(s) to either resolve or mitigate the risk.
CMM has been shown to improve patient experience, provide better care, reduce cost, and to improve the provider experience in a variety of settings [28]. One example of when CMM could be effective in preventing falls is when a patient experiences polypharmacy (or poly-FRID). The pharmacist would first raise awareness to both the patient and prescriber(s) about risks associated with polypharmacy (or poly-FRID), and then make recommendations as to which potentially inappropriate medications (PIMs) should be prioritized for deprescribing efforts. In fact, one study showed that withdrawal of fall-risk-increasing drugs is effective as a single intervention for fall prevention [29]. In addition, CMM could be effective in preventing recurrent falls. In outpatient clinic settings, pharmacists included on interprofessional teams can discourage new FRIDs prescriptions, especially at visits related to injurious falls.
Unfortunately, deprescribing FRIDs is not always a viable option, as the disease state being treated often poses more risk than an injury from a hypothetical fall or there are no reasonable medication alternatives. In this case, patient counseling is essential. During any counseling session with a patient age 65 years or older, the pharmacist should first and foremost ask the patient about his/her history of falls. The pharmacist should then discuss medications that are known to independently increase fall risk. One example of a counseling tip for a new or continued antihypertensive medication would be, “Because this medication lowers your blood pressure, you may feel dizzy and lose your balance when standing or sitting up quickly. Be sure to rise slowly.”
Providing such pharmacologic tips to patients is not the only way to decrease fall risk, however. Pharmacists can also suggest simple, non-medication related tips to prevent falls, such as being physically active and wearing sensible shoes. Pharmacists can also educate patients on modifications to their physical residence – illuminating stairs, removing throw rugs on the floor, and placing a nightlight in the path from the bedroom to the bathroom. Lastly, pharmacists can assist patients in selecting durable medical equipment (DME), like canes or walkers, when appropriate.
Strengths
One strength of this study was the ability to leverage a large, nationally representative dataset to provide estimates of FRID associated with injurious falls. The majority of analyses currently available in the literature include much smaller sample sizes, and the results are not always generalizable to the target population. Another strength of this study was the use of the comprehensive Lexicon Plus® database and the Multum classification system in the classification of FRIDs.
Limitations
Perhaps the major limitation of this study was the low weighted frequency of injurious falls reported in the NAMCS. Further, we note that our results underestimate the true prevalence of injurious falls for several reasons. First, fall injuries are frequently underreported in older adults, with one study concluding that 72% of individuals who received Medicare-reimbursed health care for fall-related injuries failed to report a fall injury when asked [30]. Second, patients with more severe injuries likely sought care at an emergency department, rather than with their primary care provider, and therefore were not captured in this survey. Third, the NAMCS does not include a section for physicians to record whether patients have experienced a fall-related injury within the recent past, and therefore only acute injuries were likely to be recorded. Despite the low percentage of injurious falls, however, significant knowledge can be gleaned from the results of this study, which highlight the pharmacist’s role in fall prevention.
Another limitation was the cross-sectional nature of the analysis, which ruled out the possibility for any longitudinal follow-up and for causal inference. We were further limited in the inability to observe from the NAMCS data discontinued medications or fall history. Lastly, because sampling of visits per physician was not based on age, we may have introduced selection bias by excluding visits for persons less than 65 years of age.
Conclusions
Although our effect estimates were not statistically significant, we observed that adults age 65 to 74 years presenting to their ambulatory care visit for an injurious fall showed a non-statistically significant increase in odds of being prescribed a new FRID than their counterparts. In contrast, adults age 75 years or older showed a non-statistically significant decrease in odds of being prescribed a new FRID than their counterparts. Pharmacists can play an important role in preventing recurrent and first-time falls for all older adults, regardless of age, through CMM and patient counseling (both pharmacologic and non-pharmacologic). More studies are needed to further evaluate prescribing behaviors after a fall.
Availability of data and materials
The datasets analyzed during the current study are available publicly on the Centers for Disease Control and Prevention NAMCS/NHAMCS – Ambulatory Health Care Data Homepage (https://www.cdc.gov/nchs/ahcd/about_ahcd.htm).
Abbreviations
- AGS:
-
American Geriatrics Society
- DVT:
-
Deep venous thrombosis
- CDC:
-
Centers for Disease Control and Prevention
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CMM:
-
Comprehensive medication management
- COPD:
-
Chronic obstructive pulmonary disease
- DME:
-
Durable medical equipment
- FRID(s):
-
Fall-risk-increasing-drug(s)
- IQR:
-
Interquartile range
- NAMCS:
-
National Ambulatory Medical Care Survey
- PIMs:
-
Potentially inappropriate medications
- RFV:
-
Reason for visit
- SE:
-
Standard error
- STEADI-Rx:
-
Stopping Elderly Accidents, Deaths, and Injuries
- TBI:
-
Traumatic brain injury
References
Important Facts about Falls | Home and Recreational Safety | CDC Injury Center. Published February 1, 2019. Accessed June 29, 2020. https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
Terroso M, Rosa N, Torres Marques A, Simoes R. Physical consequences of falls in the elderly: a literature review from 1995 to 2010. Eur Rev Aging Phys Act. 2014;11(1):51–9. https://doi.org/10.1007/s11556-013-0134-8.
Hip Fractures Among Older Adults | Home and Recreational Safety | CDC Injury Center. Published May 2, 2019. Accessed January 26, 2021. https://www.cdc.gov/homeandrecreationalsafety/falls/adulthipfx.html
Kwong LM. Hip fracture and venous thromboembolism in the elderly. J Surg Orthop Adv. 2004;13(3):139–48.
Falls Data | Home and Recreational Safety | CDC Injury Center. Published September 17, 2019. Accessed June 29, 2020. https://www.cdc.gov/homeandrecreationalsafety/falls/fallcost.html
Bueno-Cavanillas A, Padilla-Ruiz F, Jiménez-Moleón JJ, Peinado-Alonso CA, Gálvez-Vargas R. Risk Factors in Falls among the Elderly According to Extrinsic and Intrinsic Precipitating Causes. Eur J Epidemiol. 2000;16(9):849–59.
Callis N. Falls prevention: Identification of predictive fall risk factors. Appl Nurs Res. 2016;29:53–8. https://doi.org/10.1016/j.apnr.2015.05.007.
Paliwal Y, Slattum PW, Ratliff SM. Chronic Health Conditions as a Risk Factor for Falls among the Community-Dwelling US Older Adults: A Zero-Inflated Regression Modeling Approach. Biomed Res Int. 2017;2017:5146378. https://doi.org/10.1155/2017/5146378.
STEADI-Rx | STEADI - Older Adult Fall Prevention | CDC Injury Center. Published August 20, 2020. Accessed August 31, 2020. https://www.cdc.gov/steadi/steadi-rx.html
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults: 2019 AGS BEERS CRITERIA® UPDATE EXPERT PANEL. J Am Geriatr Soc. 2019;67(4):674–94. https://doi.org/10.1111/jgs.15767.
de Vries M, Seppala LJ, Daams JG, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: I. Cardiovascular Drugs. J Am Med Dir Assoc. 2018;19(4):371.e1-371.e9. https://doi.org/10.1016/j.jamda.2017.12.013.
Seppala LJ, Wermelink AMAT, de Vries M, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: II. Psychotropics J Am Med Dir Assoc. 2018;19(4):371.e11-371.e17. https://doi.org/10.1016/j.jamda.2017.12.098.
Seppala LJ, van de Glind EMM, Daams JG, et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-analysis: III. Others J Am Med Dir Assoc. 2018;19(4):372.e1-372.e8. https://doi.org/10.1016/j.jamda.2017.12.099.
Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012;65(9):989–95. https://doi.org/10.1016/j.jclinepi.2012.02.018.
NAMCS/NHAMCS - About the Ambulatory Health Care Surveys. Published September 6, 2019. Accessed November 23, 2020. https://www.cdc.gov/nchs/ahcd/about_ahcd.htm
NAMCS/NHAMCS - Estimation Procedures. Published March 4, 2019. Accessed November 11, 2021. https://www.cdc.gov/nchs/ahcd/ahcd_estimation_procedures.htm
NAMCS/NHAMCS - Ambulatory Care Drug Database System - Search. Accessed November 23, 2020. https://www2.cdc.gov/drugs/applicationnav1.asp
The consumption of two or more fall risk‐increasing drugs rather than polypharmacy is associated with falls - Zia - 2017 - Geriatrics & Gerontology International - Wiley Online Library. Accessed January 18, 2021. https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1111/ggi.12741
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. https://doi.org/10.1016/j.maturitas.2013.02.009.
van Nieuwenhuizen RC, van Dijk N, van Breda FG, et al. Assessing the prevalence of modifiable risk factors in older patients visiting an ED due to a fall using the CAREFALL Triage Instrument. Am J Emerg Med. 2010;28(9):994–1001. https://doi.org/10.1016/j.ajem.2009.06.003.
Sousa LMM, Marques-Vieira CMA, de Caldevilla MNGN, Henriques CMAD, Severino SSP, Caldeira SMA. Risk for falls among community-dwelling older people: systematic literature review. Rev Gaucha Enferm. 2017;37(4): e55030. https://doi.org/10.1590/1983-1447.2016.04.55030.
Fuller GF. Falls in the Elderly AFP. 2000;61(7):2159.
Halsey LG. The reign of the p-value is over: what alternative analyses could we employ to fill the power vacuum? Biol Lett. 2019;15(5):20190174. https://doi.org/10.1098/rsbl.2019.0174.
Palmer JB, Albrecht JS, Park Y, et al. Use of Drugs with Anticholinergic Properties Among Nursing Home Residents with Dementia: A National Analysis of Medicare Beneficiaries from 2007 to 2008. Drugs Aging. 2015;32(1):79–86. https://doi.org/10.1007/s40266-014-0227-8.
Zia A, Kamaruzzaman S, Myint PK, Tan MP. Anticholinergic burden is associated with recurrent and injurious falls in older individuals. Maturitas. 2016;84:32–7. https://doi.org/10.1016/j.maturitas.2015.10.009.
Inappropriate Use of Skeletal Muscle Relaxants in Geriatric Patients. Accessed January 15, 2021. https://www.uspharmacist.com/article/inappropriate-use-of-skeletal-muscle-relaxants-in-geriatric-patients
Hart LA, Phelan EA, Yi JY, Marcum ZA, Gray SL. Use of Fall Risk-Increasing Drugs Around a Fall-Related Injury in Older Adults: A Systematic Review. J Am Geriatr Soc. 2020;68(6):1334–43. https://doi.org/10.1111/jgs.16369.
McFarland MS, Buck M, Armistead L. The Outcomes of Implementing and Integrating Comprehensive Medication Management in Team-Based Care: A Review of the Evidence on Quality, Access and Costs, October 2020. :9.
van der Velde N, Stricker BHC, Pols HAP, van der Cammen TJM. Risk of falls after withdrawal of fall-risk-increasing drugs: a prospective cohort study. Br J Clin Pharmacol. 2007;63(2):232–7. https://doi.org/10.1111/j.1365-2125.2006.02736.x.
Hoffman GJ, Ha J, Alexander NB, Langa KM, Tinetti M, Min LC. Underreporting of fall injuries of older adults: implications for wellness visit fall risk screening. J Am Geriatr Soc. 2018;66(6):1195–200. https://doi.org/10.1111/jgs.15360.
Acknowledgements
Not applicable
Funding
This work was supported by the National Institute on Aging [R01AG054130]. This research did not receive any specific grant from funding agencies in the commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
CRediT Statement. TRE: Conceptualization, Methodology, Software, Formal analysis, Investigation, Writing – Original Draft, Writing – Review & Editing, Visualization. SW: Software, Formal analysis, Investigation. SDK: Software, Formal analysis, Investigation. ELA: Conceptualization, Writing – Review & Editing, Supervision. AKN: Conceptualization, Writing – Review & Editing, Supervision. DCM: Conceptualization, Methodology, Writing – Review & Editing, Supervision. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was exempt from Institutional Review Board approval at the University of Kentucky. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Elliott, T.R., Westneat, S., Karanth, S.D. et al. An evaluation of injurious falls and Fall-Risk-Increasing-Drug (FRID) prescribing in ambulatory care in older adults. BMC Geriatr 22, 190 (2022). https://doi.org/10.1186/s12877-022-02877-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-02877-z