Abstract
Background
This study evaluated the real-world effectiveness and potential cost-effectiveness of a community-based vision care programme for the elderly population aged 60 years or above.
Methods
Data from a total of 8899 subjects participating in a community-based comprehensive vision care programme from 2015 to 2019 were analysed to evaluate the effectiveness of the programme in terms of the prevalence of distance visual impairment (VI), the change in the prevalence of distance VI after refractive error correction, and the types of ocular disorders suspected. Distance VI was defined as a) visual acuity (VA) worse than 6/18 in any eye (worse eye) and b) VA worse than 6/18 in the better eye. The cost-effectiveness from the funder’s perspective was also estimated in terms of cost per distance VI avoided.
Results
Based on the presenting vision of the worse eye, the prevalence of distance VI was 39.1% (3482/8899, 95% CI: 38.1%-40.1%) and reduced to 13.8% (1227/8899, 95% CI: 13.1%-14.5%) based on best-corrected VA. Referenced to the presenting vision of the better eye, the prevalence of distance VI was 17.3% (1539/8899, 95% CI: 16.5%-18.1%) and decreased to 4.2% (373/8899, 95% CI: 3.8%-4.6%) with best optical correction. Uncorrected refractive error was the major cause of presenting distance VI. From the funder’s perspective, the cost per distance VI case prevented was HK$1921 based on VA in the worse eye and HK$3715 based on the better eye.
Conclusion
This community-based programme identified distance VI in the best eye of 17 out of every 100 subjects. With appropriate new or updated distance optical corrections, distance VI was reduced to about 4 in 100 subjects. Visual impairment in the elderly is common even in a relatively affluent city. A model of care which could minimise avoidable distance VI would bring benefits at individual and societal levels.
Similar content being viewed by others
Background
According to the World Health Organization (WHO), the proportion of the global population over 60 years old will increase from 12 to 22% between 2015 and 2050 [1]. Ageing is associated with general functional loss and impairment, including vision [2]. Age-related vision problems and disorders, such as uncorrected refractive error, cataracts, age-related macular degeneration, and diabetic retinopathy, are thus expected to become more common. Poor vision affects daily living activities and quality of life and often results in negative consequences such as poor mental health, falls, and increased dependency [3, 4]. More people are expected to experience visual impairment in a society with an ageing population. There is urgency for healthcare and social systems to prepare for this demographic shift in the future.
From 2019 to 2050, the population of adults aged 60 years or above in Hong Kong (HK) is estimated to increase from 25 to 40% [5]. A 2002 population-based study of 3441 elders aged 60 years or above in the Shatin district, a suburban area of HK, found that 41.3% presented with visual acuity (VA) less than 6/18 in at least one eye [6]. This percentage of visual impairment (VI) dropped to 34.5% when a pinhole was used. In addition, 19.5% of subjects presented with VA less than 6/18 in the better eye. The main causes of VI were uncorrected refractive error, cataract and macular degeneration. Over the ensuing 20 years, public healthcare sector spending has been increasing by around 7% per annum which has ensured modern healthcare services are available to all [7]. All these may contribute to improved access to vision care and prevention of VI. A more recent cross-sectional study conducted between 2016 and 2018 found that the prevalence of VI (i.e. VA worse than 20/60 in the better eye) among HK elderly aged 60 years or above, who were recruited from the FAMILY cohort project, was 9.5% (63/661) and 2.0% (13/661) for presenting vision and best-corrected VA respectively [8]. Similarly, uncorrected refractive error and cataracts were the major causes of VI. However, this study has several features which make a direct comparison with the Shatin study problematic. First, the subjects recruited were aged from between 18 to 90 years. With lower participation from older subjects, this study is likely to underestimate the prevalence rate of VI in the general population. Second, the subjects were recruited from a family cohort with some coming from the same family and this raises the potential of the family clustering effect [8].
The WHO has called for global action to support healthy ageing by formulating evidence-based policies that strengthen the abilities of older persons and align health systems with the needs of older populations [1]. Older people who maintain good vision are more likely to maintain good functioning in activities of daily living, good social function, and independence. They are also more likely to avoid co-morbidities related to poor visual function such as falls and depression [9]. A community-based programme, namely the “Kwai Tsing Signature Project Scheme” (KT programme), was established in 2015 in the Kwai Tsing district in HK with the purpose to provide comprehensive vision care to the elderly residents of the Kwai Tsing district. This provided an opportunity to evaluate the real-world evidence from a community health service in terms of the effectiveness and potential cost-effectiveness of addressing the needs for vision care for an ageing population.
Methods
Community-based programme
This KT programme was launched by the Kwai Tsing District Council, in collaboration with the Kwai Tsing Safety Community and Healthy City Association, and the School of Optometry of The Hong Kong Polytechnic University (PolyU). This programme was publicized over a wide area by the District Council through various channels, such as advertisements and public events. Under the scheme, Kwai Tsing residents aged 50 years or above could apply for a one-off comprehensive vision examination at the Integrative Community Health Centre (ICHC) in Lai King with a co-payment of HK$15 (HK$10 initially during 2015–2017, 1US$ = 7.8HK$) and purchase a pair of single-vision spectacles with a co-payment of HK$75 if indicated (the co-payment was HK$50 initially during 2015–2017). The District Council, with funding from the Home Affairs Bureau of the Hong Kong SAR government, subsidised HK$250 for each examination and HK$550 for a pair of prescription spectacles (the subsidy for spectacles was HK$500 initially during 2015–2017). Those residents who were under the Comprehensive Social Security Assistance (CSSA) Scheme or recipients of fringe benefits for civil servants and their relatives were not eligible for this KT programme. The comprehensive vision examination was conducted by optometrists in the ICHC of PolyU following the routine examination protocol, including history taking, VA measurement and preliminary testing, objective and subjective refraction, external and internal ocular health assessment and additional tests if indicated.
Subjects and data extraction
All subjects who have participated in the KT programme, aged 60 years or above, and with complete examination records were eligible for this study. This study focused on the analysis of the distance visual acuity as distance vision is the usual parameter used in vision standards. The examination rooms were equipped with the Thomson Test Chart (Thomson Software Solutions, UK) which was displayed on a monitor and with the aid of a mirror, calibrated to be viewed at an optical distance of 6 m. In a typical measurement of presenting vision, the subject covered one eye with an occluder and read the letters of the chart until the smallest line they could read. The measurement was repeated for the other eye with a different chart. The results were recorded in Snellen notation.
Subject data were extracted from the electronic record system and included demographic data, entrance distance VA, best-corrected distance VA (BCVA), and the types of suspected ocular disorders. Two broad categories were adopted, namely, VA based on the a) worse eye or b) better eye. For each category, 4 levels of VI were defined (Table 1) [10]. Distance VI was defined as VA less than 6/18, as used by Michon et al. [6]. Suspected ocular disorders were classified into 3 categories: uncorrected refractive error, anterior disorders (e.g. cataract and corneal scars) and posterior disorders (e.g. macular hole, age-related macular degeneration and epiretinal membrane).
Statistical analysis
Descriptive analyses were used to summarise the prevalence of VI with a 95% confidence interval (CI), the changes in the levels of VI after refractive error correction, and the suspected ocular disorders. The difference in the prevalence of VI between males/females and age groups was analysed using the Chi-square test. The SPSS statistical software version 26.0 was used for analyses.
Estimating the cost and cost-effectiveness of the subsidised programme
This part of the analysis estimated the direct cost of the subsidy from such a programme from the funder’s perspective and the cost per distance VI avoided as the immediate effect of receiving the comprehensive vision examination. From the funder’s perspective, the direct subsidised cost of the examination and spectacles for correcting refractive errors was considered. The co-payment from subjects for the examination and the spectacles were also included, but as revenue to the funder. This analysis represents the short-term cost-effectiveness of the programme by considering the immediate benefit from the programme.
Results
From 2015 to 2019, a total of 9149 adults participated in the KT programme. Two hundred and fifty subjects were excluded due to not meeting the aged criterion or incomplete data set, leaving 8899 subjects eligible to be included as subjects for this study. Of those eligible to be subjects, 61.9% (5507/8899) were female participants and 46.7% (4159/8899) were 70 years or above (Table 2).
Prevalence of distance visual impairment
a) Based on the worse eye
The overall prevalence of distance VI was 39.1% (3482/8899, 95% CI: 38.1%-40.1%) based on presenting VA of the worse eye and 13.8% (1227/8899, 95% CI: 13.1%-14.5%) based on BCVA respectively (Table 3). Optical correction reduced the prevalence of moderate distance VI from 33.0% (2937/8899) to 10.4% (925/8899), severe distance VI from 3.7% (329/8899) to 1.4% (125/8899), and blindness from 2.4% (216/8899) to 2.0% (177/8899).
b) Based on the better eye
The overall prevalence of VI was reduced from 17.3% (1539/8899, 95% CI: 16.5%-18.1%) based on presenting VA of the better eye to 4.2% (373/8899, 95% CI: 3.8%-4.6%) with the use of an optical correction (Table 3). Optical correction reduced the prevalence of moderate distance VI from 16.6% (1480/8899) to 4.0% (359/8899), severe distance VI from 0.6% (49/8899) to 0.1% (11/8899), and blindness from 0.1% (10/8899) to 0.03% (3/8899).
Comparison by sex and age group
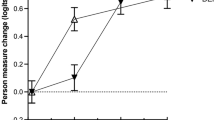
There was more distance VI in older age groups. Based on the worse eye, the prevalence of VI in the “60–64” group was 22.5% (407/1813) and for the “75 or above” group, it was 62.1% (1306/2104) (Table 4). Based on the better eye, the prevalence of VI increased from 8.4% (152/1813) to 32.9% (693/2104) from the increased age groups.
Among subjects with distance VI based on the worse eye, the proportion of correctable vision from any VI to no VI was significantly higher in the younger age group than in the older groups, reduced from 79.6% (324/407) in the 60–64 aged group to 50.0% (653/1306) in the 75 or above aged group (P-value < 0.001, Table 5). When the distance VI was defined based on the better eye, 92.1% (140/152) VI can be correctable in the aged group 60–64 and 64.1% (444/693) in the aged group 75 or above.
Suspected ocular disorders among uncorrectable distance visual impairment
Suspected ocular disorders were classified into anterior and posterior types. Among 3482 subjects with distance VI based on worse eye, 2255 had a correctable refractive error. The remaining were still visually impaired in at least one eye after refractive error correction, including 612 subjects with anterior disorders only, 235 with posterior disorders only, 146 with both anterior and posterior disorders and 234 subjects with unknown causes (Table 6).
Cost-effectiveness of the subsidised programme
From the funder’s perspective, the total cost of subsidising the vision examination was HK$2,091,265 ((HK$250-HK$15)*8899) and the total cost of subsidising the glasses was HK$2,240,323 ((HK$550-HK$75)*8899*53%) (around 53% required new prescription glasses), giving a total of HK$4,331,588. After refractive error correction (Table 3), a total number of 2255 subjects improved from any distance VI to no VI using a) VA based on the worse eye and a total of 1166 subjects using b) VA based on the better eye. Therefore, the cost per distance VI avoided from this community-based programme was estimated to be HK$1921 (US$246) based on the worse eye and HK$3715 (US$476) based on the better eye from the funder’s perspective (Table 7).
Discussion
This study evaluated the effectiveness and potential cost-effectiveness of a community-based programme to detect and address the vision problems of an elderly population resident in one district in Hong Kong. The results provide real-world evidence which could inform service planning for vision care for the wider elderly population.
This government-funded programme was initiated by a district council and was widely publicized in the relevant district. The participating elders represent those who would normally respond to public health initiatives in their community. This programme required a very low co-payment for the examination and a pair of glasses, so the financial barrier was minimal. Although the subjects might not be representative of the whole elderly population in HK, we are confident that they represented the more connected and health-conscious group. From this programme, a relatively high prevalence of distance VI was found. About 17 out of every 100 elders had distance VI (based on the better eye). With refractive error correction, distance VI improved to no VI in 76% of these cases. This significant drop suggests that a majority of the elders with distance VI benefited from this type of community-based programme and particularly so for the groups with moderate to severe VI and the younger aged groups. Results from another study of people aged 60 years and above in another part of HK indicated a 78.9% reduction in VI after optical correction [8].
The prevalence of distance VI (based on the worse eye) from this programme was similar to one population-based study conducted in another district (Shatin) 20 years ago which reported a 41.3% prevalence of VI with VA worse than 6/18 in at least one eye [6]. It is worth noting that the sampling methods were different. The Shatin study was a population-based study that used cluster sampling while convenient sampling was used in our study. Although the sampling methods were different, both studies ended up with a similar demographic profile of subjects (mean age: ~ 70 years, female/male ratio: 6:4). It is worth noting that a pinhole measurement instead of a subjective refraction was used in the Shatin study. The prevalence of VI was reduced from 41.3% to 34.5% using pinhole VA, a 16.5% relative reduction in the VI. The pinhole reduces the influence of spherical aberration and diffractive effects of media opacities. An improvement in VA with a pinhole does not imply a refractive error [11]. The pinhole acuity may also be several letters worse than the subjective BCVA [12].
Among the 1227 subjects who were still visually impaired after refractive error correction, the common suspected ocular disorders were anterior eye disorders including cataracts, pterygium, corneal degenerations and dystrophies, and posterior eye disorders including age-related macular degeneration, myopic maculopathy, epiretinal membrane, diabetic retinopathy, glaucoma and macular hole. These cases were advised to seek medical attention through the usual channels consistent with local practice.
One limitation of this study was that no data was collected on individual socioeconomic status, knowledge about ageing and vision problems, or other health data. Consequently, we were not able to perform further data analysis to determine the factors associated with VI. Moreover, the scheme excluded applicants receiving CSSA and fringe benefits (such as civil servants). This could result in a selection bias and underestimation of the prevalence of VI if the excluded groups were associated with a higher risk of VI. Besides these limitations, other limitations had been mentioned in previously published studies. For example, in defining VI, only central visual acuity was used although it is accepted that visual field integrity is an important element of visual performance. This problem is often faced by people with glaucoma, whereby progressive visual field loss and constriction may not be associated with a concurrent drop in VA [13]. It is possible that some of our subjects could have good central vision but constricted visual fields. Near vision is also an important element in enabling activities of daily living, but near VI was not considered in this study. In the majority of the cases, near vision can also be improved with near optical correction if the distance vision is correctable and therefore avoiding near VI. However, a more detailed study will be helpful to investigate issues related to near vision for the elderly population. As activities of daily living become increasingly centred on small portable screens, near vision performance is becoming more important to the quality of life.
This is a large-scale community-based programme providing vision care to over 8000 elders. From the funder’s perspective, we estimated the direct cost of such a subsidised programme and associated immediate benefit in terms of avoiding distance VI by refractive error correction during the comprehensive vision examination. We estimated that it costs between HK$1921 and HK$3715 to prevent one distance VI case. This represents the short-term cost-effectiveness of such a subsidised programme versus no subsidy, and provides a quantifiable basis to consider whether or not to provide subsidised vision care for the elderly. Future research should look holistically at the societal level and the cost–benefit of minimizing VI in the ageing population. This future research could further consider the impact of VI on elders’ quality of life and comprehensive costs across a lifetime, such as the cost of health services and social care services, social welfare payment, and the cost of caregivers depending on the perspective. A previous study estimated that the global cost of establishing and operating educational and refractive care facilities to deal with VI resulting from uncorrected refractive error was far below the global loss in productivity associated with that VI [14]. Another study reported that a dilated eye evaluation was cost-effective when compared to no screening [15].
Elders can benefit from such a community-based programme which could potentially result in better daily physical function, quality of life and independence by avoiding VI. Recent systematic reviews and meta-analyses found that VI was significantly associated with cognitive impairment in cross-sectional and longitudinal studies [16, 17]. In a longitudinal cohort study, it was found that worse visual acuity at baseline was associated with greater declines in language and memory domains of cognitive function [18]. Although the causality between the VI and cognitive impairment remains to be investigated, the value of screening elders for visual impairment and optimizing their vision could potentially contribute to the prevention of cognitive decline.
Conclusions
The prevalence of distance VI was relatively high among older people in HK. The main cause was uncorrected refractive errors. Having access to regular vision care and affordable prescription spectacles would reduce the prevalence of VI and associated risks.
Availability of data and materials
The dataset analyzed for during the current study is not publicly available as the service recipients’ data is protected by the Personal Data (Privacy) Ordinance and ethical approval on the use of the data was restricted to the approved research proposal only. Please contact the corresponding author if there are any queries regarding the dataset.
Abbreviations
- VI:
-
Visual Impairment
- VA:
-
Visual Acuity
- WHO:
-
World Health Organization
- HK:
-
Hong Kong
- KT:
-
Kwai Tsing
- PolyU:
-
The Hong Kong Polytechnic University
- ICHC:
-
The Integrative Community Health Centre
- CSSA:
-
The Comprehensive Social Security Assistance
References
World Health Organization. Ageing and health 2018 [Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 26 July 2021
Miller DB, O’Callaghan JP. Aging, stress and the hippocampus. Ageing Res Rev. 2005;4(2):123–40.
Wang CW, Chan CLW, Chi I. Overview of quality of life research in older people with visual impairment. Adv Aging Res. 2014;3:79–94.
Wang X, Lamoureux E, Zheng Y, Ang M, Wong TY, Luo N. Health burden associated with visual impairment in Singapore: the Singapore epidemiology of eye disease study. Ophthalmology. 2014;121(9):1837–42.
Census and Statistics Department, The Government of the Hong Kong Special Administrative Region. Hong Kong Population projections 2020-2069 2020 [Available from: https://www.censtatd.gov.hk/en/data/stat_report/product/B1120015/att/B1120015082020XXXXB0100.pdf. Accessed 26 July 2021
Michon JJ, Lau J, Chan WS, Ellwein LB. Prevalence of visual impairment, blindness, and cataract surgery in the Hong Kong elderly. Br J Ophthalmol. 2002;86(2):133–9.
Healthcare spending to rise 13%: news.gov.hk; 2018 [Available from: https://www.news.gov.hk/eng/2018/02/20180228/20180228_104540_809.html. Accessed 11 Aug 2022
You QS, Choy BKN, Chan JCH, Ng ALK, Shih KRC, Cheung JJC, et al. Prevalence and causes of visual impairment and blindness among adult Chinese in Hong Kong - the Hong Kong eye study. Ophthal Epidemiol. 2020;27(5):354–63.
World Health Organization. World report on vision 2019 [Available from: https://www.who.int/news-room/detail/08-10-2019-who-launches-first-world-report-on-vision. Accessed 27 July 2021
World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th revision. Fifth Edition 2016. Chapter VII. Diseases of the eye and adnexa. H54 Visual Impairment including blindness (binocular or monocular) 2016 [Available from: https://apps.who.int/iris/handle/10665/246208. Accessed 28 July 2021
Schiefer U, Kraus C, Baumbach P, Ungewiss J, Michels R. Refractive errors. Deutsches Arzteblatt Int. 2016;113(41):693–702.
Sun JK, Aiello LP, Cavallerano JD, Stockman M, Miller KM, Qin H, et al. Visual acuity testing using autorefraction or pinhole occluder compared with a manual protocol refraction in individuals with diabetes. Ophthalmology. 2011;118(3):537–42.
Rulli E, Quaranta L, Riva I, Poli D, Hollander L, Galli F, et al. Visual field loss and vision-related quality of life in the Italian primary open angle glaucoma study. Sci Rep. 2018;8(1):619.
Fricke TR, Holden BA, Wilson DA, Schlenther G, Naidoo KS, Resnikoff S, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 2012;90(10):728–38.
Rein DB, Wittenborn JS, Zhang X, Hoerger TJ, Zhang P, Klein BE, et al. The cost-effectiveness of Welcome to Medicare visual acuity screening and a possible alternative welcome to medicare eye evaluation among persons without diagnosed diabetes mellitus. Arch Ophthalmol. 2012;130(5):607–14.
Nagarajan N, Assi L, Varadaraj V, Motaghi M, Sun Y, Couser E, et al. Vision impairment and cognitive decline among older adults: a systematic review. BMJ Open. 2022;12(1):e047929.
Vu TA, Fenwick EK, Gan ATL, Man REK, Tan BKJ, Gupta P, et al. The bidirectional relationship between vision and cognition a systematic review and meta-analysis. Ophthalmology. 2021;128(7):981–92.
Varadaraj V, Munoz B, Deal JA, An Y, Albert MS, Resnick SM, et al. Association of vision impairment with cognitive decline across multiple domains in older adults. JAMA Netw Open. 2021;4(7):e2117416.
Acknowledgements
We thank Mr Chow Yick Hay, Kwai Tsing Safety Community and Healthy City Association, for initiating this vision care programme and for supporting our study. Maurice Yap was supported by the KB Woo Family Endowed Professorship in Optometry during the study period.
Funding
The project received no direct funding.
Author information
Authors and Affiliations
Contributions
SCY, TKL, YLLL and YYT contributed to the design of the work, acquisition, analysis and interpretation of data, and drafted the work; RS contributed to the acquisition of the data and revise the paper critically for important intellectual content. JL contributed to the design of the study, interpretation of data, and revised the work critically for important intellectual content; MY contributed to the conception and design of the study and revised the work critically for important intellectual content. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the Human Subjects Ethics Sub-committee of The Hong Kong Polytechnic University (HSEARS20200320001).
All participants signed the written informed consent form when they participated in this Kwai Tsing Project.
The research has been performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, S.C., Law, T.K., Leung, Y.L.L. et al. An evaluation of a community-based vision care programme for the elderly. BMC Geriatr 22, 711 (2022). https://doi.org/10.1186/s12877-022-03399-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03399-4