Abstract
Background
The comparative clinical outcomes between prediabetes and type 2 diabetes mellitus (T2DM) in older adults with AMI in the era of newer-generation drug-eluting stents (DES) are limited. We investigated the 2-year clinical outcomes of these patients.
Methods
A total of 5492 AMI patients aged ≥65 years were classified into three groups according to their glycemic status: normoglycemia (group A: 1193), prediabetes (group B: 1696), and T2DM (group C: 2603). The primary outcome was the occurrence of major adverse cardiac events (MACE), defined as all-cause death, recurrent myocardial infarction (Re-MI), and any repeat revascularization. The secondary outcome was stent thrombosis (ST).
Results
The primary and secondary outcomes cumulative incidences were similar between the prediabetes and T2DM groups. In both the prediabetes and T2DM groups, the cumulative incidences of MACE (adjusted hazard ratio [aHR]: 1.373; p = 0.020 and aHR: 1.479; p = 0.002, respectively) and all-cause death or MI (aHR: 1.436; p = 0.022 and aHR: 1.647; p = 0.001, respectively) were significantly higher than those in the normoglycemia group. Additionally, the cumulative incidence of all-cause death in the T2DM group was significantly higher than that in the normoglycemia group (aHR, 1.666; p = 0.003).
Conclusions
In this retrospective study, despite the 2-year clinical outcomes of the patients with prediabetes and T2DM in the older adults were worse than those in the normoglycemia group; they were similar between the prediabetes and T2DM groups. Hence, comparable treatment strategies should be strengthened between prediabetes and T2DM in older adults with AMI.
Trial registration
Retrospectively registered.
Similar content being viewed by others
Background
The prevalence of diabetes mellitus (DM) is growing rapidly. The number of DM cases is expected to reach 642 million by 2040 worldwide [1]. Of those aged 65 years and above, an estimated 22–33% had diabetes [2,3,4] or more than 20% had impaired glucose regulation [5]. There are numerous complex factors involved in diabetes in older adults, including decreased physical activity [6], defective beta-cell adaptation to insulin resistance [7], and decrease in endogenous estrogen and testosterone concentrations, which are believed to negatively affect glucose hemostasis [8]. Diabetes in older adults is associated with higher mortality [4], which is known to be associated with a higher risk of myocardial infarction (MI) [4, 9]. However, the prognostic implications of prediabetes in older adults remain incompletely characterized. Prediabetes comprises impaired fasting glucose (IFG) and impaired glucose tolerance (IGT), as determined by oral glucose tolerance test (OGTT) and glycated hemoglobin (HbA1c) [10]. George et al. [11] showed that IGT (hazard ratio [HR]: 1.54, 95% CI: 1.06–2.24; P = 0.024) independently predicted major adverse cardiac event (MACE)-free survival in 768 patients with acute MI (AMI). Yang et al. [12] demonstrated that fasting plasma glucose (FPG) levels were associated with a higher risk of in-hospital mortality in 1854 elderly (aged ≥65 years) patients with AMI. According to more recent reports [13, 14], patients with prediabetes had worse outcomes compared to those with normoglycemia and comparable to those with type 2 DM (T2DM). In the study by Kim et al. [14], old age (≥ 65 years) was a significant independent predictor of all-cause death (P < 0.001). However, in the Preiss et al. study [15], glycemic measures were not predictive of cardiovascular events. Another study suggested that patients with prediabetes and normoglycemia had similar 1-year mortality rates (adjusted odds ratio: 0.90; 95% CI: 0.66–1.24) in their 8795 high-risk non-ST-segment elevation myocardial infarction (NSTEMI) patients [16]. Kim et al. [17] showed that stent generation could be regarded as an important determinant of MACE. Hence, to clarify the comparative clinical outcomes between prediabetes and T2DM in older adults and to reflect contemporary trends of percutaneous coronary intervention (PCI), we compared the 2-year clinical outcomes between prediabetes and T2DM in older adults with AMI who underwent successful implantation of newer-generation drug-eluting stents (DES).
Methods
Study design and population
In this retrospective cohort study, patients with diabetes were confined to T2DM based on a previous study [18] that also included patients from the Korea AMI Registry (KAMIR) [19]. KAMIR is a nationwide, prospective, observational online registry in South Korea since November 2005 to evaluate the current epidemiology and major clinical outcomes of patients with AMI. Eligible patients were aged ≥18 years at the time of hospital admission, a more than 50 high-volume university or teaching hospitals for primary PCI and onsite cardiac surgery participated in this registry. Details of the registry can be found on the KAMIR website (http://www.kamir.or.kr). The definition of older adults is controversial. In general, a person is considered old if his or her civil age is ≥60 or 65 years [20]. Additionally, based on the Consensus Development Conference on Diabetes and Older Adults (defined as those aged ≥65 years) in February 2012 convened by the American Diabetes Association (ADA) [4], we defined the cut-off value of older adults aged ≥65 years in our study. Hence, a total of 10,138 AMI patients aged ≥65 years who were aged ≥30 years at the onset of diabetes, and who underwent successful newer-generation DES implantation from January 2006 to June 2015 in the KAMIR were evaluated. Patients who had the following conditions were excluded: (1) incomplete laboratory results including unidentified results of blood hemoglobin (Hb) A1c and blood glucose (n = 4109; 40.5%); or (2) lost to follow-up (n = 537; 5.3%). After exclusion, 5492 AMI patients who underwent successful newer-generation DESs were included. The types of newer-generation DESs used are listed in Table 1. The patients were classified into normoglycemia (group A, n = 1193 [21.7%]), prediabetes (group B, n = 1696 [30.9%]), and T2DM (group C, n = 2603 [47.4%]) groups (Fig. 1). The study protocol was approved by the ethics committee at each participating center and the Chonnam National University Hospital Institutional Review Board (IRB) ethics committee (CNUH-2011-172), according to the ethical guidelines of the 1975 Declaration of Helsinki. Informed written consent was obtained from all patients prior to inclusion in the study. All 5492 patients completed a 2-year clinical follow-up, and any information concerning adverse events that occurred during the follow-up period was monitored at the outpatient clinic, by phone calls, or by reviewing their charts at each participating center. Moreover, all clinical events were evaluated by an independent event adjudication committee [19].
Percutaneous coronary intervention procedure and medical treatment
Based on the known standard techniques [21], diagnostic coronary angiography and percutaneous coronary intervention (PCI) were performed. The loading doses of antiplatelet agents were as follows: aspirin 200–300 mg with clopidogrel 300–600 mg, ticagrelor 180 mg, or prasugrel 60 mg. All patients were asked to take dual antiplatelet therapy (DAPT) for at least 12 months after PCI. Based on previous reports [22, 23], triple antiplatelet therapy (aspirin + clopidogrel + cilostazol [100 mg twice daily]) was used. The use of DAPT or TAPT was left at the discretion of individual operators.
Study definitions and clinical outcomes
Glycemic levels of the included patients were determined based on glycosylated hemoglobin (HbA1c), FPG, and random plasma glucose (RPG) levels of the patients at the index hospitalization, as well as their medical history. According to the ADA clinical practice recommendations [10], normoglycemia was defined as HbA1c < 5.7% and FPG < 100 mg/dL (5.6 mmol/L), prediabetes as HbA1c 5.7–6.4%, and FPG 100–125 mg/dL (5.6–6.9 mmol/L), and T2DM was defined as either known diabetes for which patients received insulin or antidiabetic treatment, or newly diagnosed diabetes defined as a HbA1c level ≥ 6.5%, FPG ≥ 126 mg/dL (7.0 mmol/L), and/or RPG ≥ 200 mg/dL (11.1 mmol/L). Additionally, if there were some discrepancies between the HbA1c levels and those of FPG or RPG, we prioritized the level of HbA1c. AMI was defined according to the current guidelines [24,25,26,27]. A successful PCI was defined as residual stenosis < 30% and thrombolysis in myocardial infarction (TIMI) grade 3 flow for the infarct-related artery (IRA) after the procedure. The primary PCI strategy was performed based on the current guidelines [24, 26]. Early invasive treatment strategy of the patients with non-ST-segment elevation MI (NSTEMI) was defined as a PCI within 24 h after admission [27]. In this study, the primary outcome was the occurrence of major adverse cardiac events (MACE). All-cause death, recurrent myocardial infarction (Re-MI), or any coronary repeat revascularization were included in the MACE. All-cause death was defined as cardiac death (CD) or non-CD. Composites of target lesion revascularization (TLR), target vessel revascularization (TVR), and non-TVR were included in any repeat revascularization. The definitions of Re-MI, TLR, TVR, and non-TVR were included in our previous publication [28]. The secondary outcome was the occurrence of definite or probable stent thrombosis (ST) [29].
Statistical analysis
For continuous variables, the data were expressed as the mean ± standard deviation. The differences among the three groups were evaluated using analysis of variance or the Jonckheere-Terpstra test, while a post-hoc analysis of the two groups was performed using the Hochberg test or the Dunnett T3 test. For categorical variables, intergroup differences were analyzed using the χ2 test or Fisher’s exact test, as appropriate, and data were expressed as counts and percentages. We tested all variables with p < 0.1, among the three glycemic groups, which were included in the univariate analysis. After univariate analysis, all variables in the univariate analysis (p < 0.05) were entered into the multivariate Cox regression analysis. These variables included the following: age, male sex, left ventricular ejection fraction (LVEF), systolic blood pressure (SBP), STEMI, cardiogenic shock, cardiopulmonary resuscitation (CPR) on admission, Killip class III/IV, dyslipidemia, previous MI, previous cerebrovascular accidents (CVA), peak creatine kinase myocardial band (CK-MB), N-terminal pro-brain natriuretic peptide (NT-ProBNP), serum creatinine, estimated glomerular filtration rate (eGFR), total cholesterol, high-density lipoprotein (HDL)-cholesterol, low-density lipoprotein (LDL)-cholesterol, clopidogrel, ticagrelor, beta-blocker, angiotensin-converting enzyme inhibitor (ACEI), angiotensin receptor blocker (ARB), lipid-lowering agent, single-vessel disease, more than three diseased vessels, American College of Cardiology/American Heart Association (ACC/AHA) type B2/C lesions, pre-PCI TIMI flow grade 2/3, and mean the number of deployed stents per patient. Various clinical outcomes were estimated using the Kaplan-Meier method, and intergroup differences were compared using the log-rank test. For all analyses, two-sided values of p < 0.05, were considered statistically significant. All statistical analyses were performed using SPSS version 20 (IBM, Armonk, NY, USA).
Results
Baseline characteristics
Baseline characteristics of the study population are shown in Table 1. The mean value of the LVEF was more than 50%, which was the highest in the prediabetes group (group B). The normoglycemia group (group A) included the oldest mean patient age of all groups and most men. Group A had the highest number of PCI within 24 h, Killip class I, single-vessel disease, and the highest prescription rates of ticagrelor, prasugrel, and ACEI. Moreover, the mean blood levels of HDL-cholesterol and eGFR were the highest in group A. Group B had the highest numbers of NSTEMI, current smokers, pre-PCI TIMI flow grade 0/1, and the use of intravascular ultrasound; the highest peak CK-MB, total cholesterol, and LDL-cholesterol. The T2DM group (group C) had the highest number of NSTEMI, Killip class III, dyslipidemia, previous MI, PCI, CABG, heart failure, and CVA; more than three diseased vessels; and pre-PCI TIMI flow grade 2/3; the highest mean values of BMI, SBP, NT-ProBNP, serum creatinine, and triglycerides; the highest prescription rates of clopidogrel, cilostazole, ARB, and calcium channel blocker. However, the types of IRA and the number of treated vessels were not significantly different among the three groups (group A vs. B vs. C).
Clinical outcomes
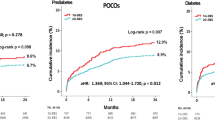
Table 2 and Fig. 2 a-2 g show the cumulative incidences of major clinical outcomes during the 2-year follow-up period. After adjustment, the cumulative incidence of MACE (Fig. 2a) was significantly higher in group B (adjusted HR [aHR], 1.373; 95% confidence interval [CI], 1.051–1.795; p = 0.020) and in group C (aHR, 1.479; 95% CI, 1.149–1.904; p = 0.002) than in group A (Fig. 2a). However, the cumulative incidence of MACE between groups B and C were similar (aHR: 1.112, 95% CI: 0.911–1.259; p = 0.297). The cumulative incidence of all-cause death or MI (Fig. 2e) was also significantly higher in group B (aHR: 1.436, 95% CI: 1.052–1.961; p = 0.022) and in group C (aHR: 1.647, 95% CI: 1.231–2.205; p = 0.001) than in group A. However, the cumulative incidence of all-cause death or MI between groups B and C was similar (aHR: 1.170; 95% CI; 0.932–1.470; p = 0.176). Additionally, the cumulative incidence of all-cause death (Fig. 2b, aHR: 1.666; 95% CI: 1.193–2.327; p = 0.003) was significantly higher in group C than in group A. However, the cumulative incidence of ST (Fig. 2g, was not significantly different among the three glycemic groups. Moreover, the cumulative incidences of all-cause death (Fig. 2b, aHR: 1.232, 95% CI: 0.945–1.608; p = 0.124), CD (Fig. 2c, aHR: 1.108, 95% CI: 0.813–1.510; p = 0.518), Re-MI (Fig. 2d, aHR: 1.127, 95% CI: 0.730–1.737; p = 0.590), and repeat revascularization (Fig. 2f, aHR: 1.018; 95% CI: 0.716–1.449; p = 0.920) were not significantly different between groups B and C. Table 3 shows independent predictors for MACE at 2 years. Age, male sex, decreased LVEF (< 40%), STEMI, cardiogenic shock, CPR on admission, Killip class III/IV, NT-ProBNP, decreased eGFR (< 60 mL/min/1.73m2), ticagrelor, ß-blocker, ACEI, ARB, lipid-lowering agent, multivessel disease, and ACC/AHA type B2/C lesions were significant independent predictors of MACE in our study.
Kaplan-Meier analysis for the MACE (a), all-cause death (b), cardiac death (c), Re-MI (d), All-cause death or MI (e), any repeat revascularization (f), and stent thrombosis (g) during a 2-year follow-up period. MACE major adverse cardiac events, Re-MI recurrent myocardial infarction, T2DM type 2 diabetes mellitus
Discussion
The main findings of this study are as follows: (1) The cumulative incidences of MACE, all-cause death, CD, Re-MI, all-cause death or MI, and any repeat revascularization between groups B (prediabetes) and C (T2DM) were not significantly different. (2) The cumulative incidence of ST was not significantly different among the three glycemic groups; (3) The cumulative incidences of MACE and all-cause death or MI in groups B and C were significantly higher than those in group A (normoglycemia); (4) the cumulative incidence of all-cause death in group C was significantly higher than that in group A; (5) Age, male sex, decreased LVEF, STEMI, cardiogenic shock, CPR on admission, Killip class III/IV, NT-ProBNP, decreased eGFR, ticagrelor, ß-blocker, ACEI, ARB, lipid-lowering agent, multivessel disease, and ACC/AHA type B2/C lesions were significant independent predictors for MACE.
In normal aging, there is a 2 mg/dL/decade rise in FPG [30], older adults have a higher chance of developing diabetes than younger adults [31, 32]. A meta-analysis reported that the pooled incidence of diabetes was 47.4, 45.5, and 70.4 per 1000 person-years among subjects with IFG, IGT, and IFG + IGT respectively [33]. Moreover, although prediabetes is regarded as an intermediate metabolic state from normoglycemia to DM [34], a higher absolute risk of complications was reported in older adults with diabetes than in younger adults [4, 35], and prediabetes is related to macrovascular complications that are recognized in individuals with overt DM [34, 36]. Therefore, without any intervention, prediabetes often progresses to DM and is associated with an increased risk of cardiovascular mortality [37]. However, the prognostic implications of prediabetes in older adults are less well understood. Hence, in this study, we compared the 2-year major clinical outcomes between the prediabetes and T2DM groups in older adults with AMI. In our study, the cumulative incidences of primary and secondary outcomes were not significantly different between the prediabetes and T2DM groups. Both the prediabetes and T2DM groups showed worse clinical outcomes than those in the normoglycemia group. Our results are consistent with the findings from recent reports [13, 14, 38]. In our study, MACE occurred in 8.0 and 10.2% of patients with normoglycemia and with prediabetes (aHR: 1.373, 95% CI: 1.051–1.795; p = 0.020), and this result was similar to that reported by Chattopadhyay et al. [39] In their 1056 MI survivals [39], the HR for MACE between patients with or without prediabetes was 1.43 (95% CI: 1.03–1.98; p = 0.033). In our study, the cumulative incidences of all-cause death, CD, and Re-MI were not significantly different between normoglycemia and prediabetes. However, the net outcome (the cumulative incidence of all-cause death or MI) was significantly higher in the prediabetes group than in the normoglycemia group (aHR: 1.436; 95% CI: 1.052–1.961; p = 0.022) (Table 2). This higher cumulative incidence of all-cause death or MI in the prediabetes group was related to a higher cumulative incidence of MACEs in this group. A possible explanation for these results may be related to hyperglycemia itself [40]. Patients with T2DM have a risk of death two times that of individuals without diabetes [41]. In our study, although the aHR for all-cause death was less than two times, the aHR for all-cause death was significantly higher in the T2DM group than in the normoglycemia group (aHR: 1.666; 95% CI: 1.193–2.327; p = 0.003). Other possible pathological mechanisms related to the worse clinical outcomes of hyperglycemia in patients with AMI include elevated levels of free fatty acids (which may cause cardiac arrhythmia), insulin resistance, impaired myocardial glucose utilization, microvascular dysfunction, and vascular inflammation [42, 43].
Chronically elevated blood glucose leads to pan-vascular damage, which could present in the prediabetes state, and its severity is associated with the onset of hyperglycemia [44, 45]. As a result, the time delay for hyperglycemia to reach the currently defined cut-off levels for the diagnosis of DM and intervention may cause vascular damage to advance and become irreversible [46]. Hence, in the case of older adults with prediabetes, the more intensive treatment of significant risk factors for MACE follows the same or similar guidelines established for patients with T2DM, and a diabetes screening for these patients (≥ 65 years) to identify those with prediabetes or T2DM may be beneficial. In the Steno-2 trial, intensified intervention including multiple risk factors reduced the risk of cardiovascular events by 50% among patients with T2DM [47]. From these points of view, our findings emphasize that the long-term prognosis of older adults with prediabetes is worse than that of normoglycemia, and a prediabetes group is an important group for cardiologists [48]. However, in this retrospective cohort, patients in the normoglycemia group had a relatively low-risk (e.g., highest number of PCI within 24 h, Killip class I, and single-vessel disease, and the largest diameter of a deployed stent) than those included in the prediabetes or T2DM groups. Therefore, although we attempted to adjust the various variables through multivariate analysis, we speculate that these different baseline characteristics may play an important role in explaining the relatively low MACE and all-cause death or MI rate in the normoglycemia group. There has been some data as to clinical outcomes between prediabetes and T2DM [49]. Moreover, it is well known about older age is a strong predictor of mortality in AMI patients receiving newer generation DES [50]. Importantly, hyperglycemia including prediabetes and T2DM in older AMI patients showed worse 2-year clinical outcomes than those in the normoglycemia group in this study. Moreover, the primary outcome between the prediabetes and T2DM groups was not significantly different. Hence, prediabetes in older AMI patients is not a benign condition. Our results suggest that it is important for interventional cardiologists to screen for and mange prediabetes in order to reduce the incidence of MACE in older AMI patients. In addition to lifestyle modifications, closer follow-ups and intensified medical treatment are needed to reduce the risk of developing DM and secondarily prevent clinically apparent coronary artery disease [13].
Despite the relatively higher prevalence of prediabetes and DM in older adults, older individuals and/or those with multiple comorbidities have often been excluded from randomized controlled trials [51, 52]. Even though the size of the study population may be insufficient to provide a firm conclusion, more than 50 community and teaching hospitals in South Korea participated in this nationwide registry analysis. Moreover, previous studies [31, 34, 37, 39,40,41,42, 46, 47] were not confined to patients with AMI who received newer-generation DESs. Hence, our findings that the long-term prognosis of older adults with prediabetes is worse than that of normoglycemia, and individuals at prediabetes state are an important group to cardiologists [48] in the era of newer-generation DES.
This study has some limitations. First, because our study was performed based on registry data, there may have been some under-reporting and/or missing data. Second, in the study, glycemic status was determined by the HbA1c, FPG, and RPG levels of the patients at the index hospitalization, as well as their medical history. To determine glycemic status more accurately, other diagnostic tests for diabetes, including OGTTs, are needed for a finer classification. However, this information was not included in the registry data. Therefore, this is a major shortcoming of this study. Third, the duration and type of antidiabetic treatment are major determinants of PCI in patients with prediabetes or diabetes. However, we did not precisely know the adherence or non-adherence rate of enrolled patients to antidiabetic drugs during the follow-up period, owing to the limitations of the registry study. Moreover, the lack of information concerning the duration of T2DM before enrollment and the degree of glycemic control of the participants during the follow-up period might constitute an additional bias in this study. Fourth, the 2-year follow-up period of this study was relatively short for determining the long-term major clinical outcomes, and multivariable analysis was performed to strengthen our results, and some variables not included in the KAMIR may have affected the study outcomes. Finally, in this study, South Korean patients alone were enrolled; careful caution is needed to interpret the current results, especially among other ethnicities in different parts of the world.
Conclusions
In conclusion, in this retrospective study, regarding the cumulative incidences of MACE and all-cause death or MI, the 2-year clinical outcomes of the patients with prediabetes and T2DM in older adults were worse than those in normoglycemia patients in the era of newer-generation DES. However, the primary and secondary clinical outcomes were similar between the prediabetes and T2DM groups in older adults. Hence, more aggressive efforts should be made to reduce MACE and all-cause death or MI in older adults with prediabetes. However, to confirm these results, further large-scale and long-term follow-up studies are needed.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- AMI:
-
Acute myocardial infarction
- KAMIR:
-
Korea AMI registry
- PCI:
-
Percutaneous coronary intervention
- T2DM:
-
Type 2 diabetes mellitus
- MACE:
-
Major adverse cardiac events
- DES:
-
Drug-eluting stent
- Re-MI:
-
Recurrent myocardial infarction;
- LVEF:
-
Left ventricular ejection fraction
- eGFR:
-
Estimated glomerular filtration rate
- HbA1c:
-
Hemoglobin A1c
References
Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50.
Selvin E, Parrinello CM, Sacks DB, et al. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med. 2014;160:517–25.
Sinclair A, Morley JE, Rodriguez-Mañas L, et al. Diabetes mellitus in older people: position statement on behalf of the International Association of Gerontology and Geriatrics (IAGG), the European diabetes working Party for Older People (EDWPOP), and the international task force of experts in diabetes. J Am Med Dir Assoc. 2012;13:497–502.
Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care. 2012;35:2650–64.
Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–101.
Schernthaner G, Schernthaner-Reiter MH. Diabetes in the older patient: heterogeneity requires individualisation of therapeutic strategies. Diabetologia. 2018;61:1503–16.
Lee PG, Halter JB. The pathophysiology of hyperglycemia in older adults: clinical considerations. Diabetes Care. 2017;40:444–52.
Mauvais-Jarvis F, Manson JE, Stevenson JC, et al. Menopausal hormone therapy and type 2 diabetes prevention: evidence, mechanisms, and clinical implications. Endocr Rev. 2017;38:173–88.
Bauduceau B, Le Floch JP, Halimi S, et al. Cardiovascular complications over 5 years and their association with survival in the GERODIAB cohort of elderly French patients with type 2 diabetes. Diabetes Care. 2018;41:156–62.
American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2016;39(Suppl 1):S13–22.
George A, Bhatia RT, Buchanan GL, et al. Impaired glucose tolerance or newly diagnosed diabetes mellitus diagnosed during admission adversely affects prognosis after myocardial infarction: an observational study. PLoS One. 2015;10:e0142045.
Yang SW, Zhou YJ, Nie XM, et al. Effect of abnormal fasting plasma glucose level on all-cause mortality in older patients with acute myocardial infarction: results from the Beijing elderly acute myocardial infarction study (BEAMIS). Mayo Clinic Proc. 2011;86:94–104.
Kok MM, von Birgelen C, Sattar N, et al. Prediabetes and its impact on clinical outcome after coronary intervention in a broad patient population. EuroIntervention. 2018;14:e1049–56.
Kim YH, Her AY, Jeong MH, et al. Effect of statin treatment in patients with acute myocardial infarction with prediabetes and type 2 diabetes mellitus: a retrospective observational registry study. Medicine. 2021;100:e24733.
Preiss D, Thomas LE, Sun JL, et al. Predictors of cardiovascular events in a contemporary population with impaired glucose tolerance: an observational analysis of the Nateglinide and valsartan in impaired glucose tolerance outcomes research (NAVIGATOR) trial. BMJ Open. 2012;2:e001925.
Giraldez RR, Clare RM, Lopes RD, et al. Prevalence and clinical outcomes of undiagnosed diabetes mellitus and prediabetes among patients with high-risk non-ST-segment elevation acute coronary syndrome. Am Heart J. 2013;165:918–925.e912.
Kim YH, Her AY, Jeong MH, et al. Impact of stent generation on 2-year clinical outcomes in ST-segment elevation myocardial infarction patients with multivessel disease who underwent culprit-only or multivessel percutaneous coronary intervention. Catheter Cardiovasc Interv. 2020;95:E40–55.
Lee SA, Cho SJ, Jeong MH, et al. Hypoglycemia at admission in patients with acute myocardial infarction predicts a higher 30-day mortality in patients with poorly controlled type 2 diabetes than in well-controlled patients. Diabetes Care. 2014;37:2366–73.
Kim JH, Chae SC, Oh DJ, et al. Multicenter cohort study of acute myocardial infarction in Korea - interim analysis of the Korea acute myocardial infarction registry-National Institutes of Health registry. Circ J. 2016;80:1427–36.
Keller I, Makipaa A, Kalenscher T, Kalache A. Global Survey on Geriatrics in the Medical Curriculum, Geneva, World Health organization, 2002. http://www.who.int/ageing/projects/en/alc global survery tegeme.pdf.
Grech ED. ABC of interventional cardiology: percutaneous coronary intervention. II: the procedure. BMJ. 2003;326:1137–40.
Chen KY, Rha SW, Li YJ, et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation. 2009;119:3207–14.
Gao W, Zhang Q, Ge H, et al. Efficacy and safety of triple antiplatelet therapy in obese patients undergoing stent implantation. Angiology. 2013;64:554–8.
Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77.
Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the Management of Acute Coronary Syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:267–315.
O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;61:e78–e140.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the Management of Patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;64:e139–228.
Kim YH, Her AY, Jeong MH, et al. Impact of renin-angiotensin system inhibitors on long-term clinical outcomes in patients with acute myocardial infarction treated with successful percutaneous coronary intervention with drug-eluting stents: comparison between STEMI and NSTEMI. Atherosclerosis. 2019;280:166–73.
Bundhun PK, Wu ZJ, Chen MH. Is there any significant difference in stent thrombosis between Sirolimus and paclitaxel eluting stents?: a systematic review and Meta-analysis of randomized controlled trials. Medicine. 2016;95:e2651.
Milanesi A, Weinreb JE. Diabetes in the elderly. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dungan K, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc. Copyright ©; 2000. p. 2000–21.
Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30:753–9.
Perreault L, Pan Q, Mather KJ, et al. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the diabetes prevention program outcomes study. Lancet. 2012;379:2243–51.
Morris DH, Khunti K, Achana F, et al. Progression rates from HbA1c 6.0-6.4% and other prediabetes definitions to type 2 diabetes: a meta-analysis. Diabetologia. 2013;56:1489–93.
DeFronzo RA, Abdul-Ghani M. Assessment and treatment of cardiovascular risk in prediabetes: impaired glucose tolerance and impaired fasting glucose. Am J Cardiol. 2011;108:3b–24b.
Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016;4:537–47.
Tabák AG, Herder C, Rathmann W, et al. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–90.
Huang Y, Cai X, Mai W, et al. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016;355:i5953.
von Birgelen C, Kok MM, Sattar N, et al. "silent" diabetes and clinical outcome after treatment with contemporary drug-eluting stents: the BIO-RESORT silent diabetes study. JACC Cardiovasc Interv. 2018;11:448–59.
Chattopadhyay S, George A, John J, et al. Pre-diabetes mellitus newly diagnosed after myocardial infarction adversely affects prognosis in patients without known diabetes. Diab Vasc Dis Res. 2019;16:489–97.
Deedwania PC, Ahmed MI, Feller MA, et al. Impact of diabetes mellitus on outcomes in patients with acute myocardial infarction and systolic heart failure. Eur J Heart Fail. 2011;13:551–9.
Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Oliver MF. Metabolic causes and prevention of ventricular fibrillation during acute coronary syndromes. Am J Med. 2002;112:305–11.
Aljada A, Friedman J, Ghanim H, et al. Glucose ingestion induces an increase in intranuclear nuclear factor kappaB, a fall in cellular inhibitor kappaB, and an increase in tumor necrosis factor alpha messenger RNA by mononuclear cells in healthy human subjects. Metabolism. 2006;55:1177–85.
Goldberg RB. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab. 2009;94:3171–82.
Semenkovich CF. We know more than we can tell about diabetes and vascular disease: the 2016 Edwin Bierman award lecture. Diabetes. 2017;66:1735–41.
Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med. 2008;358:2630–3.
Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–93.
Carris NW, Magness RR, Labovitz AJ. Prevention of diabetes mellitus in patients with Prediabetes. Am J Cardiol. 2019;123:507–12.
Kim YH, Her AY, Jeong MH, et al. Comparative effect of statin intensity between prediabetes and type 2 diabetes mellitus after implanting newer-generation drug-eluting stents in Korean acute myocardial infarction patients: a retrospective observational study. BMC Cardiovasc Disord. 2021;21:386.
Taniwaki M, Stefanini GG, Räber L, et al. Predictors of adverse events among patients undergoing primary percutaneous coronary intervention: insights from a pooled analysis of the COMFORTABLE AMI and EXAMINATION trials. EuroIntervention. 2015;11:391–8.
Cruz-Jentoft AJ, Carpena-Ruiz M, Montero-Errasquín B, et al. Exclusion of older adults from ongoing clinical trials about type 2 diabetes mellitus. J Am Geriatr Soc. 2013;61:734–8.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK prospective diabetes study (UKPDS) Group. Lancet. 1998;352:837–53.
Acknowledgments
Korea Acute Myocardial infarction Registry (KAMIR) investigators.
Myung Ho Jeong, MD, Youngkeun Ahn, MD, Sung Chul Chae, MD, Jong Hyun Kim, MD, Seung-Ho Hur, MD, Young Jo Kim, MD, In Whan Seong, MD, Donghoon Choi, MD, Jei Keon Chae, MD, Taek Jong Hong, MD, Jae Young Rhew, MD, Doo-Il Kim, MD, In-Ho Chae, MD, Junghan Yoon, MD, Bon-Kwon Koo, MD, Byung-Ok Kim, MD, Myoung Yong Lee, MD, Kee-Sik Kim, MD, Jin-Yong Hwang, MD, Myeong Chan Cho, MD, Seok Kyu Oh, MD, Nae-Hee Lee, MD, Kyoung Tae Jeong, MD, Seung-Jea Tahk, MD, Jang-Ho Bae, MD, Seung-Woon Rha, MD, Keum-Soo Park, MD, Chong Jin Kim, MD, Kyoo-Rok Han, MD, Tae Hoon Ahn, MD, Moo-Hyun Kim, MD, Ki Bae Seung, MD, Wook Sung Chung, MD, Ju-Young Yang, MD, Chong Yun Rhim, MD, Hyeon-Cheol Gwon, MD, Seong-Wook Park, MD, Young-Youp Koh, MD, Seung Jae Joo, MD, Soo-Joong Kim, MD, Dong Kyu Jin, MD, Jin Man Cho, MD, Sang-Wook Kim, MD, Jeong Kyung Kim, MD, Tae Ik Kim, MD, Deug Young Nah, MD, Si Hoon Park, MD, Sang Hyun Lee, MD, Seung Uk Lee, MD, Hang-Jae Chung, MD, Jang-Hyun Cho, MD, Seung Won Jin, MD, Myeong-Ki Hong, MD, Yangsoo Jang, MD, Jeong Gwan Cho, MD, Hyo-Soo Kim, MD and Seung-Jung Park, MD.
Funding
This research was supported by a fund (2016-ER6304–02) by Research of Korea Centers for Disease Control and Prevention. The funders had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Y.H.K. and A.-Y.H. researched data and wrote the manuscript. Y.H.K., A.-Y.H., B.-K.K., J.-S.K., S.-H.P., B.G.K., S.K., M.-K.H., and Y.J. contributed to study design. M.H.J., B.-K.K., S.-J.H., S.K., C.-M.A., J.-S.K., Y.-G.K., D.C., M.-K.H., and Y.J. contributed to the collection research data. Y.H.K. A.-Y.H., B.-.KK., J.-S.K., Y.-G.K., D.C., M.-K.H., and Y.J. contributed to provide intellectual inputs for the discussion. Y.H.K., A.-Y.H., S.-J.H., and S.K. contributed to data analysis and edited the manuscript. Y.H.K., M.H.J., D.C., M.-K.H., and Y.J. contributed to provide supervisor role during the full processes of manuscript submitting and editing. All authors have read and approved the manuscript, and all authors take full responsibility for this work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of each participating center and the Chonnam National University Hospital Institutional Review Board ethics committee (CNUH-2011-172) according to the ethical guideline of the Declaration of Helsinki. Written informed consent was obtained from all patients prior to inclusion in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, Y.H., Her, AY., Jeong, M.H. et al. Outcomes between prediabetes and type 2 diabetes mellitus in older adults with acute myocardial infarction in the era of newer-generation drug-eluting stents: a retrospective observational study. BMC Geriatr 21, 653 (2021). https://doi.org/10.1186/s12877-021-02601-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-021-02601-3