Abstract
Background
Neuroimaging-biomarkers of Mild Cognitive Impairment (MCI) allow an early diagnosis in preclinical stages of Alzheimer’s disease (AD). The goal in this paper was to review of biomarkers for Mild Cognitive Impairment (MCI) and Alzheimer’s disease (AD), with emphasis on neuroimaging biomarkers.
Methods
A systematic review was conducted from existing literature that draws on markers and evidence for new measurement techniques of neuroimaging in AD, MCI and non-demented subjects. Selection criteria included: 1) age ≥ 60 years; 2) diagnosis of AD according to NIAAA criteria, 3) diagnosis of MCI according to NIAAA criteria with a confirmed progression to AD assessed by clinical follow-up, and 4) acceptable clinical measures of cognitive impairment, disability, quality of life, and global clinical assessments.
Results
Seventy-two articles were included in the review. With the development of new radioligands of neuroimaging, today it is possible to measure different aspects of AD neuropathology, early diagnosis of MCI and AD become probable from preclinical stage of AD to AD dementia and non-AD dementia.
Conclusions
The panel of noninvasive neuroimaging-biomarkers reviewed provides a set methods to measure brain structural and functional pathophysiological changes in vivo, which are closely associated with preclinical AD, MCI and non-AD dementia. The dynamic measures of these imaging biomarkers are used to predict the disease progression in the early stages and improve the assessment of therapeutic efficacy in these diseases in future clinical trials.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Alzheimer’s disease (AD) is the most common age-related neurodegenerative disease, characterized by progressive cognitive decline, accounts for 50–75 % of the global dementia population, with a greater proportion in the higher age ranges [1].
Clinicians and researchers have recently updated the AD diagnostic criteria for use in clinical practice and research [2]. Biomarkers (e.g., CSF protein levels, neuroimaging) may be used to rule out other causes of dementia (e.g., vascular) and to support the AD diagnosis in cases with unclear or atypical presentations. Attempts to diagnose AD at an earlier stage have led to the appearance of new medical terminologies such as pre-clinical AD, prodromal AD or mild cognitive impairment (MCI). Recently, new criteria for diagnosis of MCI in clinical and research settings have been published [3, 4].
In this context neuroimaging and fluid biomarkers for amyloid deposition and hippocampal atrophy can be measured more than 10 years before the onset of dementia [5, 6]. The application of these markers could enhance the specificity of clinical diagnosis and improve the prediction of the disease progression. The objective in this paper was to review of biomarkers for Mild Cognitive Impairment (MCI) and AD, with emphasis on neuroimaging biomarkers.
Methods
The search strategy and analysis was informed by: the study’s aims, previous systematic reviews using qualitative data, and best practice recommendations in the research literature [7, 8]. Literature searches were conducted over MEDLINE (2000 to June 2015) and Pubmed (2000 to June 2015), using the OVID search interface. The searches were limited to human studies in English language including potential Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) biomarkers.
Study selection
A single reviewer examined the abstracts retrieved by the electronic search in order to identify articles that met the inclusion criteria and to be fully reviewed.
Inclusion criteria: 1) age ≥ 60 years; 2) diagnosis of AD according to the National Institute on Aging-Alzheimer’s Association (NIAAA) criteria [2], 3) diagnosis of MCI according to NIAAA criteria [4] with a confirmed progression to AD assessed by clinical follow-up, and 4) acceptable clinical measures of cognitive impairment, disability, quality of life, and global clinical assessments.
Exclusion criteria: 1) no English editing (as we lacked resources for translation), 2) diagnosis of non-AD dementia, and 3) MCI not progressed in AD.
Data extraction
In total, 2243 articles, reports and reviews were identified. After reviewing abstracts, 425 were excluded on the basis of the aforementioned inclusion/exclusion criteria and the removal of duplicates (n. 1595). A further 151 were excluded after more in-depth examination (on the basis of the same inclusion/exclusion criteria). Thus, 72 published studies were eligible for the current review (Fig. 1).
Data extraction followed a number of stages. After preliminary categorisation, categories were divided among the authors according to expertise. Each category was reviewed in depth by at least one author and the lead author:
-
Potential structural neuroimaging biomarkers
-
Functional neuroimaging biomarkers
Co-authors provided a detailed summary of each study including its strengths and weaknesses, as well as an overall appraisal of the category [9, 10]. Quality of study reporting was assessed using the Standards for the Reporting of Diagnostic accuracy studies in dementia (STARDdem) [11].
Results and discussions
Potential structural neuroimaging biomarkers
Structural MRI (sMRI)
Medial temporal and hippocampal atrophy were the most common structural MRI (sMRI) markers of progression to AD [12, 13]. The 3-dimensional patterns of cerebral atrophy progression over multiple serial MRI were consistent with neurofibrillary pathological staging scheme in AD, showing that the earliest changes in the anterior medial temporal lobe and fusiform gyrus occur at least 3 years before conversion to AD [14]. However, one study showed that both baseline enthorhinal volume and its slope of decline, but not initial hippocampal size and its rate of decline, were independent predictors of incident AD [15].
Molecular biomarkers of neuronal injury that are present in advance of atrophy offer a complementary target for sMRI [16]. Model-based magnetization transfer (mMT) imaging could improve classification of subjects with early AD and MCI compared with magnetization transfer ratio (MTR) [17].
Individual biomarkers, such as white matter hyperintensities (WMH), cerebral volume, hippocampal volume, entorhinal cortex thickness, ventricle volume, and CSF markers had limited predictive value for cognitive decline [18]. Combination of sMRI and plasma biomarkers, such as whole genome single nucleotide polymorphism data, tocopherols and tocotrienols, or CSF total tau, phosphorylated tau (p-tau) and Aβ42: amyloid-β42 (Aβ42) could enhance the accurancy of differentiating subjects with AD and MCI from cognitively normal subjects [19–21]. Annual ventricular volume changes in serial sMRI were related to concurrent change on general cognitive and functional indices in amnestic MCI (aMCI) and AD, and were influenced by Apolipoprotein E (ApoE) genotype [22]. The combination of imaging and CSF biomarkers could improve the conversion prediction from MCI to AD [21, 23–25] and time to develop dementia in subjects with MCI and amyloid pathology [26]. Baseline fludeoxyglucose (FDG) Positron Emission Tomography (PET) added the greatest prognostic information compared with baseline clinical testing [24], but marginally predicted longitudinal cognitive decline [25]. Baseline sMRI was slightly better predictor of future clinical/functional decline than CSF t-tau/Aβ42 [21]. MRI imaging might be a more practical clinical biomarker for early detection of AD [27]. Multiple MRI markers of underlying dementia pathologies improve the ability to identify patients with prodromal dementia over a single MRI marker [28]. The areas of hypoperfusion in patients with asymmetric cortical degenerative syndromes measured by single-photon emission computed tomography (SPECT) were larger than the corresponding atrophic regions showed by sMRI [29]. The combination of both was useful in identifying the regional structural and functional cerebral abnormalities.
The mild or severe atropy in sMRI with severe decline in parietal regional Cerebral blood flow (CBF) on SPECT could distinguish AD from FTD and VaD patients [30]. The most common non-AD dementia is vascular dementia (VaD) with considerable overlap with AD pathology. VaD results from cerebrovascular and cardiovascular disorders. Non-significant vascular lesions on structre brain imaging result in overdiagnosis of VaD [31]. A significantly higher allele frequency of ApoEε4 in AD patients was found than these with VaD in a community population [32]. The increase of WMH in deep white matter, but not WMH in periventricular white matter on MRI scans indicates 86 % classification accuracy [33]. MRI measure of infarcts, a vascular brain injury, were significantly related to medial-temporal and cerebral atropy in VaD but not in AD patients with 71 % sensitivity and 76 % specificity [34]. The combination of MRI and SPECT could differentiate VaD with sensitivity 88 %, specificity 75 % and FTD with sensitivity 73 %, specificity 78 % respectively, and enhance specificity of AD diagnosis by CSF biomarkers from 71 to 93 % [35].
Diffusion MRI
The diffusion tensor imaging (DTI) metrics including fractional anisotropy (FA), mean diffusivity, axial diffusivity and radial diffusivity (RA), can assess the connectivity between brain regions [36–38]. Both vascular and AD degenerative process have different region-specific structural injury patterns of cerebral white matter [39]. The combination of mean tanscallosal prefrontal FA and the Fazekas score in volume by T2-weighted measures could differentiate VaD from AD with 87.5 % accuracy, 100 % specifity and 93 % sensitivity [40].
The reduced FA and RA values in patients with AD than in patients with MCI suggested that the brain DTI was useful to confirm clinical manifestation of AD but not in the detection of MCI [41]. White matter microstructural changes identified with DTI derived FA doesn’t appear as a significant predictor of cognition [42]. In another study, it was shown that high WMH predict progression from normal to MCI, but not progression from MCI to dementia [43]. Conversely, the brain parenchymal fraction (BPF) which showed whole-brain atrophy, did not predict conversion from normal to MCI but predicted conversion to dementia [43]. In a study, it was shown that posterior periventricular and corpus callosum extension of WMH associated with MCI and AD indicate involvement of strategic white matter bundles that may contribute to the cognitive deficits [44]. Increased amyloid burden, as measured with florbetapir PET imaging, was associated with changes in weighted structural connectome metrics independent of brain region [45]. The decrease of FA and the mode of anisotropy in intracortically projecting fiber tracts of MCI-AD and AD subjects suggested early axonal degeneration in intracortical projecting fiber tracts [46]. To assess the decrease of the cingulum fibers using DTI-derived FA could help early diagnosis of AD [47]. The hippocampal apparent diffusion coefficients were higher in MCI and AD subjects than in controls [48]. The elevated apparent diffusion coefficients in hippocampus may indicate early pre-clinical AD.
Functional neuroimaging biomarkers
PET imaging for metabolism status
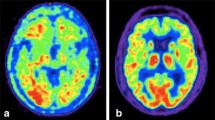
A study showed that 30 min was enough foroptimal FDG accumulation for AD PET scan, especially for the early stage of AD [49]. Bilateral temporoparietal hypometabolism on [18 F] fludeoxyglucose-positron emission tomography (FDG-PET) could differentiate AD dementia from VaD dementia with leukoaraiosis [50]. (18)FDG-PET showed FDG uptake reductions in AD related brain regions in cognitively normal individual with ApoEε4 genotype and subjective cognitive complaint [51], or a maternal history of AD [52]. Compared with nonconverters, converters of MCI patients had lower FDG uptake in the right temporoparietal contex [53]. Hypometabolism in brain regions may be related to ongoing pathologies and to reduced neuronal input in remote but functionally connected regions [54]. MCI patients who did not develop dementia after 2 years showed even higher uptake in the basal forebrain than those who developed dementia [55]. Longitudinal changes in individual subjects in the spatial pattern of brain glucose metabolism measured with (18)F-FDG PET showed correlations with the cognitive decline of AD and MCI [56, 57].
The combination C-labeled Pittsburgh Compound-B ([(11)C]PIB) and FDG track molecular changes could show different stages of AD. Increased [(11)C]PIB images of binding potential was found in MCI patients and progressive decrease of FDG uptake was only observed in AD patients [58]. The hypoperfusion patterns showed by arterial spin labeling MRI and hypometabolism patterns showed by FDG-PET could provide largely overlapping information of fuctional deficits in affected areas of AD [59]. Regional cerebral blood flow measured by [11C]dihydrotetrabenazine (DTBZ)-PET also provided similar information in assessment of regional cerebral metabolic deficits in mild dementia and MCI with FDG-PET, and exhibited a mild decrease in sensitivity [60]. Preclinical and clinical studies have shown that the use of PET imaging for tracking neuroinflammatory changes seems to have a promising role in AD and other central nervous system (CNS) pathologies [61, 62]. Translocator protein (TSPO) radioligands [11C](R)-PK11195, [11C]DAA1106 and [11C]PBR28 suggest the increased expression of TSPO by activated microglia in AD patients [62].
The radioligand 11C-deuterium-L-deprenyl ([11C]-DED) showed the highest binding among PIB in MCI individuals, that suggests the reactive astrocytosis occurs at the early stages of AD [63]. Activation of cytosolic phospholipase A2 (cPLA2) and secretory phospholipase A2 (sPLA2) after microglia-derived inflammatory cytokines bind astrocytic cytokine receptors results in the hydrolysis of membrane phospholipids, liberating arachidonic acid (AA) [64]. A common single nucleotide polymorphism (rs6971) in exon 4 of the TSPO gene has been identified as the key determinant of affinity with second generation TSPO radioligands [11C]DAA1106 and [11C]PBR28 [65]. Cerebral blood flow, which is reduced in AD, highly influences monoamine oxidase B (MAO-B) binding that seems to increase with age in almost all brain regions (with the exception of the cingulate gyrus) in healthy human subjects [62]. PET neuroinflammation imaging may, alternately, be more useful in monitoring the responsivity to anti-inflammatory therapies in AD.
PET imaging for amyloid load
Amyloid accumulation evidenced by florbetapir PET may be a potential marker of preclinical AD. Cognitively normal subjects with florbetapir uptake increase in brain were associated with worse globe cognitive performance [66]. [(11)C]PIB data showed expected differences among subjects of control, MCI and AD [67–69] and identified subjects with significant annual increases in amyloid load across the subject groups [67]. Longitudinal studies showed that PET Aβpositive subjects of cognitively normal, MCI and AD subjects had greater cognitive and global deterioration than Aβnegative subjects [70, 71] and Aβpositive subjects of MCI had higher risk for conversion to AD than Aβnegative subjects [71, 72]. Florbetapir PET measurements showed that 76 % AD, 38 % MCI, and 14 % cognitively normal subjects was amyloid positive [73]. The global cortex standardized uptake value ratio of Florbetapir could differentiate AD and MCI from healthy normal controls with high specificity and sensitivity [74]. Amyloid deposition has already slowed or ceased when dementia occurs [75]. Combination baseline sMRI and (18)F-florbetaben (FBB) uptake values did not improve predictive accuracy of MCI conversion to AD [76]. CSF Aβ42 did not always become abnormal prior to fibrillar Aβ accumulation early in the course of disease [77]. 2-(1-{6-[(2-fluorine 18-labeled fluoroethyl)methylamino]-2-napthyl}ethylidene) malononitrile ([(18)F]FDDNP) provides a measure of both amyloid and tau. [(18)F]FDDNP could predict future cognitive decline and conversion of MCI to AD [78].
PET radioligands of tau protein
In the amyloid cascade hypothesis, although tau pathology is considered secondary to Aβpathology, the post-mortem classification of AD cases into pathological subtypes with distinct clinical characteristics is determined by the localization and distribution of tau pathology in the brain [79, 80]. Abnormal burden of tau species can accurately predict disease severity and the rate of cognitive decline [79, 80]. The recent progress in tau protein ligands makes tau PET imaging a potential biomarker. Radioligands [18 F]-T807 and [18 F]-T808 used in human brain images with different pharmacokinetic characteristics were the most selective compounds for filamentous tau, and the level of selective binding with tau was 27-fold higher than that of Aβ [81, 82]. A phenyl/pyridinyl-butadienyl-benzothiazoles/benzothiazolium (PBB) showed the greatest specificity for tau in vivo PET imaging of tau transgenic mouse models, and [(11)C]PBB3 patterns were consistent with the spreading of tau pathology with AD progression and non-AD tauopathy corticobasal syndrome in a clinical PET study [83].
fMRI and SPECT
A set of medial prefrontal and temporo-parietal regions, such as the posterior cingulate and hippocampus, are referred to as the default-mode network (DMN), which is most active at rest and deactivated during cognitive tasks. Amyloid deposition in AD brains is most obvious in brain areas of the default network. Functional MRI showed that the DMN exhibits both reduced functional connectivity and impaired task-induced deactivation in AD, mild cognitive impairment (MCI) and pre-MCI [84–89].
Subjects with aMCI showed decreased DMN activity in memory function related brain regions, such as left medial temporal lobe before atrophy was detectable by sMRI [86]. Based on a multi-modal imaging approach, including FDG-PET and sMRI and diffusion-weighted MRI results, AD patients revealed decreased structural and functional connections, corresponding consistent reduction of metabolic activity and atrophy within DMN [90]. The disrupted connectivity in AD turns the high metabolic activity of DMN into hypometabolism [84]. A 2- to 3- year follow-up study revealed that functional connectivity indices could predict conversion of MCI to AD [91]. Education, a factor in cognitively demanding tasks, reduces AD risk by reducing neuronal activity and Aβ generation within the default network [92]. It was observed that in the earliest phase of MCI the individuals exhibited significantly greater hippocampal activation than controls even if two group without difference in hippocampal or entorhinal volumes [93]. Longitudinal fMRI in cognitively normal elderly participants reveals that subjects with the highest hippocampal activation at baseline and the greatest loss of hippocampal activation demonstrated more rapid cognition decline [94]. Compensatory efforts as a result of preclinical pathological changes in learning and memory tasks induce enhanced brain activity in some areas in the initial targets of AD, and these changes may precede the diagnosis of AD by 30 years [95]. Neuronal activity stimulates aerobic glycolysis and increases Aβ production and secretion into the interstitial fluid (ISF). The degree of Aβ aggregation and plaque deposition is directly proportional to ISF Aβ concentrations in vivo [96]. Factors including elevated endogenous neuronal activity may accelerate the Aβ deposition process. Cognitively normal ApoEε4 carriers show elevated resting-state activity in the default network and increased hippocampal activation in fMRI during a memory-encoding task compared to non-carriers [97]. Cerebral perfusion abnormalities were evident in AD progression. CBF was a more sensitive parameter than cerebral blood volume for perfusion normalities and appeared before the latter in the progression of AD [98]. A reduced CBF of the left posterior cingulated gyrus [99], bilateral prefrontal and frontal, and left parietal [100], and right parietal and hippocampal regions [101] evidenced by SPECT could predict the conversion of MCI to AD at least 2 years before clinical AD. But low parietal and medial temporal flow using SPECT demonstrated limited utility in predicting MCI conversion to AD [102]. Semi-quantitative circumferential-profile analysis of brain SPECT showed that AD patients have more significant reductions in the posterior temporo-parietal regions, and white matter VaD patients have greater reducutions in the frontal brain regions [103].
Combination the pattern of hypoperfusion and the severity of memory deficits could predict the risk of progression to AD in MCI subjects with a sensitivity and specificity [102, 104].
Regional CBF measured by Arterial spin-labeling (ASL) magnetic resonance showed that regional CBF of AD patients was significantly lower in both the bilateral frontal and temporal lobes, and the value of VaD patients was significantly in left frontal and temporal white matter [105]. SPECT imaging of regional benzodiazepine receptors (rBZR) can reflect neuronal integrity in the cerebral cortex. VaD and mixed AD/VaD dementia showed predominant reduction of regional CBF and rBZR in the frontal lobe, and AD in parietotemporal lobe. Furthermore, rBZR images of VaD and mixed dementia showed more extensive and severe defects than CBF images, and CBF images of AD showed more extensive defects than rBZR [106]. Although the heterogeneity index of the whole brain CBF on SPECT images was not significantly different between the AD and VaD groups, the herogeneity of CBF for AD and VaD was posterior and anterior-dominant respectively [107].
Conclusion
The use in clinical practice of neuroimaging biomarkers of brain pathological processes could permit to perform an early diagnosis and to estimate the disease progression. Some neuroimaging-biomarkers have been widely used in clinical diagnosis of AD. The more neuroimaging biomarkers are still used for clinical studies. The use of neuroimaging biomarkers depended on the stage of disease progress. The proposed pathophysiological sequence contains Aβaccumulation, neuronal dysfunction (synaptic dysfunction, glial activation, tangle formation), brain atrophy due to neuronal death, and finally cognitive impairment [108].
Amyloid imaging is useful for differential diagnosis in early-onset dementia and clinical diagnosis of AD in noncarriers of ApoEε4 who are older than 70 years [5]. However, amyloid imaging may not be sufficient to make correct diagnosis in an individual [109]. PET with FDG, tau and other neurochemical tracers, fMRI and SPECT are used to measure the neuronal dysfunction. Finally, sMRI, advanced MRI techniques, such as DTI and MRS are used to show atrophy and hypoperfusion in cortex and white matter. The ordering and the sigmoidal-like time changes of imaging biomarkers are useful to detect early pathophysiological changes in preclinical stage; the extensive and severe impairment means greater AD-like pathology. Therefore, imaging biomarkers often are used to detect the comversion of preclinical AD and MCI to AD and predict outcomes of clinical intervention trials. Particularly, imaging biomarkers are helpful to differentiate AD dementia from VaD and other non-AD dementia. To find early different vascular pathological contribution to AD and VaD, an advanced dynamic contrast-enhanced MRI could quantify hippocampus blood brain barrier permeability in the living human brain; CA1 and dentate gyrus subdivisions showed obviously worsened in patients with mild cognitive impairment,which was correlated with injury to BBB-associated pericytes [110].
The combination of structural, functional neuroimaging and fluid biomarkers improved the accuracy of prediction [111]. With same diagnosis power, one should give preference to the less expensive, safer and less invasive techniques. However, some factors, including environmental factor, ApoE genetic variation and brain or cognitive reserve can affect or alter the cuves of these biomarkers.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Abbreviations
- [(11)C]PIB:
-
C-labeled Pittsburgh Compound-B
- [(18)F]FDDNP:
-
2-(1-{6-[(2-fluorine 18-labeled fluoroethyl)methylamino]-2-napthyl}ethylidene) malononitrile
- [11C]-DED:
-
11C-deuterium-L-deprenyl
- AA:
-
arachidonic acid
- AD:
-
Alzheimer’s disease
- ApoE:
-
apolipoprotein E
- Aβ42:
-
amyloid-β42
- BPF:
-
brain parenchymal fraction
- CBF:
-
cerebral blood flow
- CNS:
-
central nervous system
- cPLA2:
-
cytosolic phospholipase A2
- CSF:
-
cerebrospinal fluid
- DMN:
-
default-mode network
- DTBZ:
-
[11C]dihydrotetrabenazine
- DTI:
-
diffusion tensor imaging
- FA:
-
fractional anisotropy
- FBB:
-
(18)F-florbetaben
- FDG:
-
fludeoxyglucose
- ISF:
-
interstitial fluid
- MAO-B:
-
monoamine oxidase B
- MCI:
-
mild cognitive impairment
- mMT:
-
model-based magnetization transfer
- MRI:
-
magnetic resonance imaging
- MTR:
-
magnetization transfer ratio
- NIAAA:
-
National Institute on Aging-Alzheimer’s Association
- PBB:
-
phenyl/pyridinyl-butadienyl-benzothiazoles/benzothiazolium
- PET:
-
positron emission tomography
- p-tau:
-
phosphorylated tau
- RA:
-
radial diffusivity
- rBZR:
-
regional benzodiazepine receptors
- rs6971:
-
single nucleotide polymorphism
- sMRI:
-
structural MRI
- SPECT:
-
single-photon emission computed tomography
- sPLA2:
-
secretory phospholipase A2
- STARDdem:
-
Standards for the Reporting of Diagnostic accuracy studies in dementia
- TSPO:
-
translocator protein
- VaD:
-
vascular dementia
- WMH:
-
white matter hyperintensities
References
Braak H, Del Tredici K. Where, when, and in what form does sporadic Alzheimer disease begin? Curr Opin Neurol. 2012;25(6):708–14.
McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9.
Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303–8.
Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging—Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9.
Jansen WJ, Ossenkoppele MR, Knol DL, et al. Prevalence of cerebral amyloid pathology in persons without dementia A meta-analysis. JAMA. 2015;313(19):1924–38.
Villemagne VL, Burnham S, Bourgeat P, et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: A prospective cohort study. Lancet Neurol. 2013;12(4):357–67.
Dixon-Woods M, Agarwal S, Jones D, et al. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy. 2005;10:45–53.
Hannes K, Macaitis K. A move to more systematic and transparent approaches in qualitative evidence synthesis: update on a review of published papers. Qual Res. 2012;12:402–42.
Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009;9:59.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108.
Noel-Storr AH, McCleery JM, Richard E, et al. Reporting standards for studies of diagnostic test accuracy in dementia: The STARDdem Initiative. Neurology. 2014;83(4):364–73.
Jack Jr CR, Petersen RC, Xu YC, et al. Prediction of AD with MRI-based hippocampal volume in mild cognitive impairment. Neurology. 1999;52(7):1397–403.
Risacher SL, Saykin AJ, West JD, et al. Baseline MRI predictors of conversion from MCI to probable AD in the ADNI cohort. Curr Alzheimer Res. 2009;6(4):347–61.
Whitwell JL, Przybelski SA, Weigand SD, et al. 3D maps from multiple MRI illustrate changing atrophy patterns as subjects progress from mild cognitive impairment to Alzheimer’s disease. Brain. 2007;130(Pt 7):1777–86.
Stoub TR, Bulgakova M, Leurgans S, et al. MRI predictors of risk of incident Alzheimer disease: a longitudinal study. Neurology. 2005;64(9):1520–4.
Jack Jr CR. Alzheimer disease: new concepts on its neurobiology and the clinical role imaging will play. Radiology. 2012;263:344–61.
Wiest R, Burren Y, Hauf M, et al. Classification of mild cognitive impairment and Alzheimer disease using model-based MR and magnetization transfer imaging. Am J Neuroradiol. 2013;34(4):740–6.
Nettiksimmons J, Harvey D, Brewer J, et al. Subtypes based on cerebrospinal fluid and magnetic resonance imaging markers in normal elderly predict cognitive decline. Neurobiol Aging. 2010;31(8):1419–28.
Kong D, Giovanello KS, Wang Y, et al. Predicting Alzheimer’s Disease Using Combined Imaging-Whole Genome SNP Data. J Alzheimers Dis. 2015;46(3):695–702.
Mangialasche F, Westman E, Kivipelto M, et al. Classification and prediction of clinical diagnosis of Alzheimer’s disease based on MRI and plasma measures of α-/γ-tocotrienols and γ-tocopherol. J Intern Med. 2013;273(6):602–21.
Vemuri P, Wiste HJ, Weigand SD, et al. MRI and CSF biomarkers in normal, MCI, and AD subjects: diagnostic discrimination and cognitive correlations. Neurology. 2009;73(4):287–93.
Vemuri P, Wiste HJ, Weigand SD, et al. Serial MRI and CSF biomarkers in normal aging, MCI, and AD. Neurology. 2010;75(2):143–51.
Eckerström C, Olsson E, Bjerke M, et al. A combination of neuropsychological, neuroimaging, and cerebrospinal fluid markers predicts conversion from mild cognitive impairment to dementia. J Alzheimers Dis. 2013;36(3):421–31.
Shaffer JL, Petrella JR, Sheldon FC, et al. Predicting cognitive decline in subjects at risk for Alzheimer disease by using combined cerebrospinal fluid, MR imaging, and PET biomarkers. Radiology. 2013;266(2):583–91.
Landau SM, Harvey D, Madison CM, et al. Comparing predictors of conversion and decline in mild cognitive impairment. Neurology. 2010;75(3):230–8.
van Rossum IA, Vos SJ, Burns L, et al. Injury markers predict time to dementia in subjects with MCI and amyloid pathology. Neurology. 2012;79(17):1809–16.
Karow DS, McEvoy LK, Fennema-Notestine C, et al. Relative capability of MR imaging and FDG PET to depict changes associated with prodromal and early Alzheimer disease. Radiology. 2010;256(3):932–42.
Kantarci K, Weigand SD, Przybelski SA, et al. Risk of dementia in MCI: combined effect of cerebrovascular disease, volumetric MRI, and 1H MRS. Neurology. 2009;72(17):1519–25.
Caselli RJ, Jack Jr CR, Petersen RC, et al. Asymmetric cortical degenerative syndromes: clinical and radiologic correlations. Neurology. 1992;42:1462–8.
Varma AR, Adams W, Lloyd JJ, et al. Diagnostic patterns of regional atrophy on MRI and regional cerebral blood flow change on SPECT in young onset patients with Alzheimer’s disease, frontotemporal dementia and vascular dementia. Acta Neurol Scand. 2002;105(4):261–9.
Niemantsverdriet E, Feyen BF, Le Bastard N, et al. Overdiagnosing vascular dementia using structural brain imaging for dementia work-up. J Alzheimers Dis. 2015;45(4):1039–43.
Chu WZ, Gong L, Xu YQ, et al. Apolipoprotein E gene variants of Alzheimer’s disease and vascular dementia patients in a community population of Nanking. Med Chem. 2014;10(8):783–8.
Smith CD, Johnson ES, Van Eldik LJ, et al. Peripheral (deep) but not periventricular MRI white matter hyperintensities are increased in clinical vascular dementia compared to Alzheimer’s disease. Brain Behav. 2016;16:e00438. doi:10.1002/brb3.438.
Logue MW, Posner H, Green RC, et al. Magnetic resonance imaging-measured atrophy and its relationship to cognitive functioning in vascular dementia and Alzheimer’s disease patients. Alzheimers Dement. 2011;7(5):493–500.
Boutoleau-Bretonnière C, Lebouvier T, Delaroche O, et al. Value of neuropsychological testing, imaging, and CSF biomarkers for the differential diagnosis and prognosis of clinically ambiguous dementia. J Alzheimers Dis. 2012;28(2):323–36.
Racine AM, Adluru N, Alexander AL, et al. Associations between white matter microstructure and amyloid burden in preclinical Alzheimer’s disease: A multimodal imaging investigation. Neuroimage Clin. 2014;4:604–14.
Dyrba M, Barkhof F, Fellgiebel A, et al. Predicting Prodromal Alzheimer’s disease in subjects with Mild Cognitive Impairment using machine learning classification of multimodal multicenter diffusion-tensor and magnetic resonance imaging data. J Neuroimaging. 2015;25(5):738–47.
Balachandar R, John JP, Saini J, et al. A study of structural and functional connectivity in early Alzheimer’s disease using rest fMRI and diffusion tensor imaging. Int J Geriatr Psychiatry. 2015;30(5):497–4.
Lee DY, Fletcher E, Martinez O, et al. Regional pattern of white matter microstructural changes in normal aging, MCI, and AD. Neurology. 2009;73(21):1722–8.
Zarei M, Damoiseaux JS, Morgese C, et al. Regional white matter integrity differentiates between vascular dementia and Alzheimer disease. Stroke. 2009;40(3):773–9.
Stahl R, Dietrich O, Teipel SJ, et al. White matter damage in Alzheimer disease and mild cognitive impairment: assessment with diffusion-tensor MR imaging and parallel imaging techniques. Radiology. 2007;243(2):483–92.
Meier IB, Manly JJ, Provenzano FA, et al. White matter predictors of cognitive functioning in older adults. J Int Neuropsychol Soc. 2012;18(3):414–27.
Smith EE, Egorova S, Blacker D, et al. Magnetic resonance imaging white matter hyperintensities and brain volume in the prediction of mild cognitive impairment and dementia. Arch Neurol. 2008;65(1):94–100.
Yoshita M, Fletcher E, Harvey D, et al. Extent and distribution of white matter hyperintensities in normal aging, MCI, and AD. Neurology. 2006;67(12):2192–8.
Prescott JW, Guidon A, Doraiswamy PM, et al. The Alzheimer structural connectome: changes in cortical network topology with increased amyloid plaque burden. Radiology. 2014;273(1):175–84.
Teipel SJ, Grothe MJ, Filippi M, et al. Fractional anisotropy changes in Alzheimer’s disease depend on the underlying fiber tract architecture: a multiparametric DTI study using joint independent component analysis. J Alzheimers Dis. 2014;41(1):69–83.
Zhang Y, Schuff N, Jahng GH, et al. Diffusion tensor imaging of cingulum fibers in mild cognitive impairment and Alzheimer disease. Neurology. 2007;68(1):13–9.
Kantarci K, Jack Jr CR, Xu YC, et al. Mild cognitive impairment and Alzheimer disease: regional diffusivity of water. Radiology. 2001;219(1):101–7.
Takahashi R, Ishii K, Senda M, et al. Equal sensitivity of early and late scans after injection of FDG for the detection of Alzheimer pattern: an analysis of 3D PET data from J-ADNI, a multi-center study. Ann Nucl Med. 2013;27(5):452–9.
Mendez MF, Ottowitz W, Brown CV, et al. Dementia with leukoaraiosis: clinical differentiation by temporoparietal hypometabolism on (18)FDG-PETimaging. Dement Geriatr Cogn Disord. 1999;10(6):518–25.
Mosconi L, De Santi S, Brys M, et al. Hypometabolism and altered cerebrospinal fluid markers in normal apolipoprotein E E4 carriers with subjective memory complaints. Biol Psychiatry. 2008;63(6):609–18.
Mosconi L, Mistur R, Switalski R, et al. Declining brain glucose metabolism in normal individuals with a maternal history of Alzheimer disease. Neurology. 2009;72(6):513–20.
Chételat G, Desgranges B, de la Sayette V. Mild cognitive impairment: can FDG-PET predict who is to rapidly convert to Alzheimer’s disease? Neurology. 2003;60:1374–7.
Klupp E, Förster S, Grimmer T, et al. In Alzheimer’s disease, hypometabolism in low-amyloid brain regions may be a functional consequence of pathologies in connected brain regions. Brain Connect. 2014;4(5):371–83.
Kim MJ, Lee KM, Son YD, et al. Increased basal forebrain metabolism in mild cognitive impairment: an evidence for brain reserve in incipient dementia. J Alzheimers Dis. 2012;32(4):927–38.
Landau SM, Harvey D, Madison CM, et al. Associations between cognitive, functional, and FDG-PET measures of decline in AD and MCI. Neurobiol Aging. 2011;32(7):1207–18.
Shokouhi S, Claassen D, Kang H, et al. Longitudinal progression of cognitive decline correlates with changes in the spatial pattern of brain 18 F-FDG PET. J Nucl Med. 2013;54(9):1564–9.
Ossenkoppele R, Tolboom N, Foster-Dingley JC, et al. Longitudinal imaging of Alzheimer pathology using [11C]PIB, [18 F]FDDNP and [18 F]FDG PET. Eur J Nucl Med Mol Imaging. 2012;39(6):990–1000.
Chen Y, Wolk DA, Reddin JS, et al. Voxel-level comparison of arterial spin-labeled perfusion MRI and FDG-PET in Alzheimer disease. Neurology. 2011;77(22):1977–85.
Albin RL, Koeppe RA, Burke JF, et al. Comparing fludeoxyglucose F18-PET assessment of regional cerebral glucose metabolism and [11C]dihydrotetrabenazine-PET in evaluation of early dementia and mild cognitive impairment. Arch Neurol. 2010;67(4):440–6.
Ji B, Maeda J, Sawada M, et al. Imaging of peripheral benzodiazepine receptor expression as biomarkers of detrimental versus beneficial glial responses in mouse models of Alzheimer’s and other CNS pathologies. J Neurosci. 2008;28(47):12255–67.
Zimmer ER, Leuzy A, Benedet AL, et al. Tracking neuroinflammation in Alzheimer’s disease: the role of positron emission tomography imaging. J Neuroinflammation. 2014;11:120.
Carter SF, Scholl M, Almkvist O, et al. Evidence for astrocytosis in prodromal Alzheimer disease provided by 11C-deuterium-L-deprenyl: a multitracer PET paradigm combining 11C-Pittsburgh compound B and 18 F-FDG. J Nucl Med. 2012;53:37–46.
Balsinde J, Winstead MV, Dennis EA. Phospholipase A(2) regulation of arachidonic acid mobilization. FEBS Lett. 2002;531:2–6.
Mizrahi R, Rusjan PM, Kennedy J, et al. Translocator protein (18 kDa) polymorphism (rs6971) explains in-vivo brain binding affinity of the PET radioligand [18 F]-FEPPA. J Cereb Blood Flow Metab. 2012;32:968–72.
Rosenberg PB, Wong DF, Edell SL, et al. Cognition and amyloid load in Alzheimer disease imaged with florbetapir F18(AV-45) positron emission tomography. Am J Geriatr Psychiatry. 2013;21(3):272–8.
Jagust WJ, Bandy D, Chen K, et al. The Alzheimer’s Disease Neuroimaging Initiative positron emission tomography core. Alzheimers Dement. 2010;6(3):221–9.
Klunk WE, Engler H, Nordberg A, et al. Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann Neurol. 2004;55:306–19.
Rowe CC, Ng S, Ackermann U, et al. Imaging beta-amyloid burden in aging and dementia. Neurology. 2007;68:1718–25.
Doraiswamy PM, Sperling RA, Johnson K, et al. Florbetapir F 18 amyloid PET and 36-month cognitive decline: a prospective multicenter study. Mol Psychiatry. 2014;19(9):1044–51.
Doraiswamy PM, Sperling RA, Coleman RE, et al. Amyloid-β assessed by florbetapir F 18 PET and 18-month cognitive decline: a multicenter study. Neurology. 2012;79(16):1636–44.
Okello A, Koivunen J, Edison P, et al. Conversion of amyloid positive and negative MCI to AD over 3 years: an 11C-PIB PET study. Neurology. 2009;73(10):754–60.
Johnson KA, Sperling RA, Gidicsin CM, et al. Florbetapir (F18-AV-45) PET to assess amyloid burden in Alzheimer’s disease dementia, mild cognitive impairment, and normal aging. Alzheimers Dement. 2013;9(5 Suppl):S72–83.
Camus V, Payoux P, Barré L, et al. Using PET with 18 F-AV-45 (florbetapir) to quantify brain amyloid load in a clinical environment. Eur J Nucl Med Mol Imaging. 2012;39(4):621–31.
Furst AJ, Rabinovici GD, Rostomian AH, et al. Cognition, glucose metabolism and amyloid burden in Alzheimer’s disease. Neurobiol Aging. 2012;33(2):215–25.
Ong KT, Villemagne VL, Bahar-Fuchs A, et al. Aβ imaging with 18 F-florbetaben in prodromal Alzheimer’s disease: a prospective outcome study. J Neurol Neurosurg Psychiatry. 2015;86(4):431–6.
Landau SM, Lu M, Joshi AD, et al. Comparing positron emission tomography imaging and cerebrospinal fluid measurements of β-amyloid. Ann Neurol. 2013;74(6):826–36.
Small GW, Siddarth P, Kepe V, et al. Prediction of cognitive decline by positron emission tomography of brain amyloid and tau. Arch Neurol. 2012;69(2):215–22.
Murray ME, Graff-Radford NR, Ross OA, et al. Neuropathologically defined subtypes of Alzheimer’s disease with distinct clinical characteristics: a retrospective study. Lancet Neurol. 2011;10(9):785–96.
Braak H, Braak E. Development of Alzheimer-related neurofibrillary changes in the neocortex inversely recapitulates cortical myelogenesis. Acta Neuropathol. 1996;92(2):197–201.
Chien DT, Bahri S, Szardenings AK, et al. Early clinical PET imaging results with the novel PHF-tau radioligand [F-18]-T807. J Alzheimers Dis. 2013;34(2):457–68.
Chien DT, Szardenings AK, Bahri S, et al. Early clinical PET imaging results with the novel PHF-tau radioligand [F18]-T808. J Alzheimers Dis. 2014;38(1):171–84.
Maruyama M, Shimada H, Suhara T, et al. Imaging of tau pathology in a tauopathy mouse model and in Alzheimer patients compared to normal controls. Neuron. 2013;79(6):1094–108.
Greicius MD, Srivastava G, Reiss AL, et al. Default-mode network activity distinguishes Alzheimer’s disease from healthy aging: evidence from functional MRI. Proc Natl Acad Sci U S A. 2004;101(13):4637–42.
Pihlajamaki M, Jauhiainen AM, Soininen H. Structural and functional MRI in mild cognitive impairment. Curr Alzheimer Res. 2009;6(2):179–85.
Jin M, Pelak VS, Cordes D. Aberrant default mode network in subjects with amnestic mild cognitive impairment using resting-state functional MRI. Magn Reson Imaging. 2012;30(1):48–61.
Sperling RA, Dickerson BC, Pihlajamaki M, et al. Functional alterations in memory networks in early Alzheimer’s disease. Neuromolecular Med. 2010;12(1):27–43.
Gomez-Ramirez J, Wu J. Network-based biomarkers in Alzheimer’s disease: review and future directions. Front Aging Neurosci. 2014;6:12.
Wang Y, Risacher S, West J, et al. Altered default mode network connectivity in older adults with cognitive complaints and amnestic mild cognitive impairment. J Alzheimers Dis. 2013;35:751–60.
Zhu DC, Majumdar S, Korolev IO, et al. Alzheimer’s disease and amnestic mild cognitive impairment weaken connections within the default-mode network: a multi-modal imaging study. J Alzheimers Dis. 2013;34(4):969–84.
Petrella JR, Sheldon FC, Prince SE, et al. Default mode network connectivity in stable vs progressive mild cognitive impairment. Neurology. 2011;76(6):511–7.
Flicker L. Modifiable lifestyle risk factors for Alzheimer’s disease. J Alzheimers Dis. 2010;20:803–11.
Dickerson BC, Salat DH, Greve DN, et al. Increased hippocampal activation in mild cognitive impairment compared to normal aging and AD. Neurology. 2005;65(3):404–11.
O’Brien JL, O’Keefe KM, LaViolette PS, et al. Longitudinal fMRI in elderly reveals loss of hippocampal activation with clinical decline. Neurology. 2010;74(24):1969–76.
Mondadori CR, Buchmann A, Mustovic H, et al. Enhanced brain activity may precede the diagnosis of Alzheimer’s disease by 30 years. Brain. 2006;129(Pt 11):2908–22.
Bero AW, Yan P, Roh JH, et al. Neuronal activity regulates the regional vulnerability to amyloid-β deposition. Nat Neurosci. 2011;14(6):750–6.
Kim J, Basak JM, Holtzman DM. The role of apolipoprotein E in Alzheimer’s disease. Neuron. 2009;63:287–303.
Lacalle-Aurioles M, Mateos-Pérez JM, Guzmán-De-Villoria JA, et al. Cerebral blood flow is an earlier indicator of perfusion abnormalities than cerebral blood volume in Alzheimer’s disease. J Cereb Blood Flow Metab. 2014;34(4):654–9.
Huang C, Wahlund LO, Svensson L, et al. Cingulate cortex hypoperfusion predicts Alzheimer’s disease in mild cognitive impairment. BMC Neurol. 2002;2:9.
Encinas M, De Juan R, Marcos A, et al. Regional cerebral blood flow assessed with 99mTc-ECD SPET as a marker of progression of mild cognitive impairment to Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2003;30(11):1473–80.
Habert MO, Horn JF, Sarazin M, et al. Brain perfusion SPECT with an automated quantitative tool can identify prodromal Alzheimer’s disease among patients with mild cognitive impairment. Neurobiol Aging. 2011;32(1):15–23.
Devanand DP, Van Heertum RL, Kegeles LS, et al. (99 m)Tc hexamethyl-propylene-aminoxime single-photon emission computed tomography prediction of conversion from mild cognitive impairment to Alzheimer disease. Am J Geriatr Psychiatry. 2010;18(11):959–72.
Chen YJ, Deutsch G, Satya R, et al. A semi-quantitative method for correlating brain disease groups with normal controls using SPECT: Alzheimer’s disease versus vascular dementia. Comput Med Imaging Graph. 2013;37(1):40–7.
Borroni B, Anchisi D, Paghera B, et al. Combined 99mTc-ECD SPECT and neuropsychological studies in MCI for the assessment of conversion to AD. Neurobiol Aging. 2006;27(1):24–31.
Gao YZ, Zhang JJ, Liu H, et al. Regional cerebral blood flow and cerebrovascular reactivity in Alzheimer’s disease and vascular dementia assessed by arterial spinlabeling magnetic resonance imaging. Curr Neurovasc Res. 2013;10(1):49–53.
Hanyu H, Kume K, Sato T, et al. Regional differences in cortical benzodiazepine receptors of Alzheimer, vascular, and mixed dementiapatients. J Neurol Sci. 2012;323(1-2):71–6.
Yoshikawa T, Murase K, Oku N, et al. Heterogeneity of cerebral blood flow in Alzheimer disease and vascular dementia. AJNR Am J Neuroradiol. 2003;24(7):1341–7.
Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–92.
Price JL, Morris JC. Tangles and plaques in nondementted aging and “preclinical” Alzheimer’s disease. Ann Neurol. 1999;45:358–68.
Montagne A, Barnes SR, Sweeney MD, et al. Blood-brain barrier breakdown in the aging human hippocampus. Neuron. 2015;85(2):296–302.
Jack CRJ, Lowe VJ, Senjem ML, et al. 11C PiB and structural MRI provide complementary information in imaging of Alzheimer’s disease and amnestic mild cognitive impairment. Brain. 2008;131(Pt 3):665–80.
Acknowledgments
This study was supported by the Shanghai Hospital Development Center (No. SHDC12014221) and Shanghai Key Laboratory of Clinical Geriatric Medicine (13dz2260700).
Funding
The authors did not receive grants or outside funding in support of their research for or preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
QR and GD conceived of the study. QR, ZB and ZY created the search protocol. QR examined abstracts retrieved. QR and GD contributed to manuscript preparation. DS, AG, ZB and ZY contributed to analysis, drafting the paper and the conclusions. The authors confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. The authors further confirm that the order of authors listed in the manuscript has been approved by all.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ruan, Q., D’Onofrio, G., Sancarlo, D. et al. Potential neuroimaging biomarkers of pathologic brain changes in Mild Cognitive Impairment and Alzheimer’s disease: a systematic review. BMC Geriatr 16, 104 (2016). https://doi.org/10.1186/s12877-016-0281-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-016-0281-7