Abstract
Aims
The preoperative serum levels of inflammatory mediators, including C-reactive protein (CRP), procalcitonin (PCT) and interleukin-6 (IL-6), have been demonstrated to be correlated with patient outcomes in colorectal cancer (CRC); however, the prognostic role of these levels has been less well-studied in postoperative settings.
Materials and methods
A total of 122 stage I-III CRC patients were retrospectively enrolled. Serum levels of CRP, PCT and IL-6 were measured after surgery, and their prognostic value was evaluated. Kaplan-Meier analysis was used to determine the differences in disease-free survival (DFS) and overall survival (OS) between patients with different levels of these mediators, and the Cox proportional hazards model was used to estimate the risk factors.
Results
In contrast to CRP and PCT, only the level of IL-6 was significant in predicting DFS (P = 0.01) but not OS (P = 0.07). A total of 66.39% (81/122) of patients were assigned to the low IL-6 group and no significant differences were found in the collected clinicopathological parameters among the low or high IL-6 subgroups. The level of IL-6 was negatively correlated with postoperative (1 w) (R=-0.24, P = 0.02) absolute lymphocyte counts. Patients with low levels of IL-6 had better DFS (log rank = 6.10, P = 0.01) but not OS (log rank = 2.28, P = 0.13). Finally, the level of IL-6 was an independent risk factor for DFS (HR: 1.81, 95% CI: 1.03–3.15, P = 0.04).
Conclusions
Compared to CRP and PCT, the level of IL-6 was observed to be the only significant factor in predicting the prognosis of stage I-III CRC patients after surgery, and a low level of IL-6 was associated with good DFS.
Similar content being viewed by others
Introduction
It has long been established that inflammation plays a critical role in cancer development, such as by facilitating the proliferation and survival of malignant cells and by promoting important biological processes such as angiogenesis and migration [1, 2]. Colorectal cancer (CRC), which exhibits increased mobility and mortality rates according to the latest statistics [3], is still a serious health problem worldwide. Previously, a substantial number of studies have indicated that inflammation-related mediators, such as C-reactive protein (CRP), procalcitonin (PCT) and interleukin-6 (IL-6), play an important role in the prediction of CRC prognosis.
Interestingly, most previous studies have explored the prognostic value of CRP, PCT and IL-6 levels individually for CRC in the preoperative setting [4, 5] and have yielded inconsistent results when considered together. For example, the study by Groblewska et al. indicated that CRP was the only independent risk factor for survival when compared to IL-6 [6]; in contrast, the study by Lee et al. suggested that IL-6 but not CRP, was an independent risk factor for disease-free survival (DFS) in stage III patients [7]. In addition, the study by Kwon et al. work suggested that both CRP and IL-6 were not independent risk factors for DFS or overall survival (OS) [8]. In recent years, a group of new CRC prognostic markers based on inflammatory cells have been identified; these examples include the neutrophil to lymphocyte ratio (NLR) and lymphocyte to monocyte ratio (LMR), and longitudinal measurements of these markers have suggested that they may be more meaningful when they were analyzed in postoperative settings [9, 10]. For CRP, PCT and IL-6, it is notable that many factors can cause changes in their levels during tumor removal, including surgical stress [11,12,13] and anesthesia [14, 15]. However, only a few studies have investigated their prognostic role concurrently in postoperative scenarios. For example, Hermunen et al. conducted a post hoc analysis for 147 patients (stages II-IV) in the phase III LIPSYT study and found that both postoperative CRP and IL-6 were significant for survival (CRP was a risk factor for DFS but not OS, and IL-6 showed opposite results) but with a low sensitivity (CRP: 20%, IL-6: 28% for DFS) [16]. Hua et al. performed a study with 306 stage II-III patients and found that IL-6 was the most promising prognostic marker in contrast with CRP [17]. Nonetheless, reports that concurrently explore the prognostic value of postoperative CRP, PCT and IL-6 levels in CRC are still lacking.
Based on this background, we aimed to concurrently examine the usefulness of postoperative CRP, PCT and IL-6 levels in determining the prognosis of stage I-III CRC.
Methods
Patient enrollment
Patients who underwent radical resection of colorectal adenocarcinoma from December 2012 to October 2020 at Hainan Hospital of PLA General Hospital were retrospectively enrolled. Patients who met any of the following criteria were not included: (1) accepted neoadjuvant therapies; (2) lacked any of the results of CRP, PCT and IL-6 levels within 7 days (d) (median 1 d; range:1–7 d) after surgery or routine blood tests in the subsequent 7 d and 2 weeks (w) to 3 months (m); (3) lacked any pathological TNM information or stage IV according to the 7th edition of the American Joint Committee on Cancer (AJCC) cancer staging manual; and (4) lost to follow-up. Other clinicopathological parameters were registered as described previously [18, 19]. The study was carried out in accordance with the principles stated in the Declaration of Helsinki and was approved by the ethics committee of Hainan Hospital of PLA General Hospital and the requirement for written informed consent was waived due to its retrospective nature.
Routine blood tests and measurements of the target indicators
Routine laboratory tests and the method to measure blood cell fractions were performed as described previously [19, 20]. The CRP (reference: 0-0.5 mg/dl) was measured by using turbidimetric inhibition immunoassay with the CRPL3 kit (Roche Diagnostics GmbH, Mannheim, Germany) according to the manufacturer’s manual with the automatic analysis system (Cobas e 501, Roche, Switzerland). In addition, PCT (reference: <0.05 ng/ml) and IL-6 (reference: 0–7 pg/ml) were measured via chemiluminescence with the Elecsys BRAHMS PCT kit and Elecsys IL-6 kit (Roche Diagnostics GmbH, Mannheim, Germany) according to the manufacturer’s manual with the automatic analysis system (Cobas e 601 and Cobas e 801, Roche, Switzerland, respectively). The NLR and LMR were calculated as described previously [21].
Endpoints
The follow-up was started immediately after resection according to the procedure described previously [19]. DFS and OS were set as the endpoints for the current study, and DFS was estimated from the time of operation to the time of any recurrence or metastasis or death from any cause; in addition, OS was estimated from the time of operation to the time of death from any cause. The latest follow-up point ended in December 2021.
Statistical analysis
The significance of CRP, PCT and IL-6 in predicting survival was determined by using the receiver operating characteristic curve (ROC), and patients were then divided into low or high subgroups based on the optimal discriminator points when it was statistically significant. Differences in the collected clinicopathological parameters among these subgroups were analyzed via χ2-test or Student’s t test. Correlations of the levels of markers with the ALCs were estimated by using the Pearson or Spearman (when any of the parameters did not meet the Gaussian distribution) correlation coefficients. Moreover, differences in DFS and OS among these subgroups were calculated via Kaplan-Meier analysis. Risk factors for DFS and OS were determined by using the Cox proportional hazards model (with the iterative forward LR method). The statistical analyses were performed by using SPSS 20.0 (SPSS Inc., Chicago, IL, USA) and GraphPad Prism 5 (GraphPad Software Inc., San Diego, CA, USA). Two-sided P < 0.05 was regarded to be statistically significant.
Results
General features of the study cohort and the prognostic significance of CRP, PCT and IL-6
A total of 122 patients were enrolled in the study. There were 44 female and 78 male patients, with a median age of 64 years (y) (range: 26–86 y) and a median follow-up of 44 m (1-108 m). At the end of the follow-up, 52 events were observed with 39 deaths (1 stage I patient, 12 stage II patients and 26 stage III patients). As shown in Fig. 1, in contrast to CRP and PCT, only the level of IL-6 was found to be significant in predicting DFS (area under the curve [AUC] = 0.62, 95% CI: 0.52–0.73, P = 0.02) but not OS (AUC = 0.60, 95% CI: 0.49–0.71, P = 0.07). The optimal discriminator point for IL-6 in predicting DFS was 70.27 pg/ml, and 66.39% (81/122) of patients were then assigned to the low IL-6 group (< 70.27 pg/ml) and 33.61% (41/122) of patients were assigned to the high IL-6 group (≥ 70.27 pg/ml). In addition, no differences were found for the collected clinicopathological parameters among the low or high IL-6 subgroups (Table 1).
Correlation of IL-6 with ALCs
By using the Spearman correlation analysis (Fig. 2), no significant correlations were observed for the level of IL-6 with the ALCs both preoperatively (R=-0.13, P = 0.15) and postoperatively at 2 w-3 m (R=-0.06, P = 0.49); however, a significant correlation was found for the level of IL-6 with the ALCs postoperatively (1 w) (R=-0.21, P = 0.02). Furthermore, significant positive correlations were observed between the levels of IL-6 and CRP (R = 0.52, P < 0.01) and PCT (R = 0.47, P < 0.01).
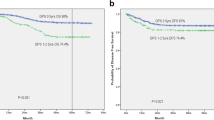
Survival differences among low or high IL-6 subgroups
According to the Kaplan-Meier analysis (Fig. 3), patients in the low level IL-6 group had significantly superior DFS (log rank = 6.10, P = 0.01) compared with the high level group; however, no such difference was found in OS (log rank = 2.28, P = 0.13).
Risk factors determined by univariate and multivariate tests
By using the univariate tests, parameters including type of operation, N stage and TNM stage were demonstrated to be risk factors for both DFS and OS, whereas gender, history of drinking and IL-6 level were found to be additional risk factors for DFS (Table 2). Furthermore, when these factors were entered into the multivariate tests, the IL-6 level was found to be an independent risk factor for DFS (HR = 2.24, 95% CI: 1.19–4.21, P = 0.01) but not OS (Table 3).
Discussion
In this study, we demonstrated that only the postoperative level of IL-6 was a useful prognostic marker in CRC in contrast to CRP and PCT. Patients with a relatively low level of IL-6 had significantly superior survival to those with a high level, and IL-6 was an independent risk factor for DFS. To the best of our knowledge, this is the first report to concurrently compare the prognostic value of CRP, PCT and IL-6 in CRC.
Previously, the prognostic values of CRP, PCT and IL-6 have been individually explored in CRC in preoperative settings; however, only a few studies have been conducted in postoperative settings [22,23,24,25,26,27]. For example, McSorley et al. conducted a study with 377 stage 0-III patients and found that postoperative CRP > 150 mg/L at 4 d was independently associated with poor DFS [22]; in addition, other studies have also indicated that postoperative CRP could be useful in predicting DFS [23,24,25] or OS [26]. In addition, Bae et al. performed a study with 248 stage I-IV patients and found that postoperative PCT was a risk factor for OS; however, it was not an independent factor [27]. Notably, no reports to date have explored the role of postoperative IL-6 alone. Interestingly, two reports have concurrently explored these markers (CRP and IL-6), as mentioned previously [16, 17], but with several limitations. One study included stage IV patients [16], who exhibited different survival rates than others [28], and the other study included patients who received additional treatments (such as radiation and chemotherapy) except for surgery [17]. In our study, we included stage I-III patients who underwent surgery alone and concurrently compared the prognostic value of CRP, PCT and IL-6. The results indicated that IL-6 was significant in predicting DFS, which was partially consistent with these reports [16, 17]. Furthermore, we did not identify any significant differences in the collected clinicopathological parameters, including gender, history of smoking, and BMI, among the low or high level IL-6 subgroups, which was also partially consistent with the results of a previous study [17].
It was notable that the prognostic efficacy of CRP and PCT in CRC was inferior to that of IL-6 in the postoperative scenario in our study. In fact, although previous studies have indicated that CRP and PCT were correlated with the outcome either preoperatively [4, 29,30,31] or postoperatively [23,24,25,26,27] in CRC, there have also been studies suggesting that these factors would be more useful in predicting infective complications [12, 32,33,34] and may not be associated with disease recurrence [33] or outcome [7, 34,35,36,37]. Moreover, one study indicated that IL-6 was the only independent risk factor for survival in contrast to CRP [7]. Additionally, although it was observed that CRP and IL-6 increased within 4 and 24 h, respectively, after the operation [38], CRP normalized within 10 d, but IL-6 did not, which was particularly evident in patients with significantly high preoperative levels [39]. These studies may support the notion that IL-6 would be more robust in predicting survival in CRC to some extent.
Generally, circulating IL-6 levels were found to correlate with systemic inflammatory responses in CRC patients undergoing surgery [40], and it has broad functions in CRC development, such as in promoting tumor growth [41], spreading [42], and angiogenesis [43], as well as in regulating treatment resistance [44, 45]. In recent years, cancer dissemination was found to occur at the very beginning of the disease in CRC [46]. These detached cells, which are also known as circulating tumor cells (CTCs), play a pivotal role in disease recurrence and treatment failure [47, 48]. Interestingly, systemic inflammation can contribute to the metastatic colonization of CTCs [49]. Based on these facts, it is plausible that patients with a surge in IL-6 after surgery are at high risk of cancer metastasis, and these patients can exhibit poor outcomes. Additionally, cancer stem cells (CSCs) were identified as the “true bad seeds” in CRC [50] and are considered to be the source of cancer initiation, recurrence and treatment resistance [51]. Notably, some studies have indicated that a proportion of CTCs are actually CSCs [52, 53], and IL-6 was found to be involved in the expansion [54, 55], promotion [56] and support [57] of these cells. Thus, we speculate that high levels of IL-6 can contribute to the evolution of these CSCs and can also result in poor patient survival. In addition, it was observed that lymphocyte counts as well as T-cell subset counts significantly decline in CRC patients after surgery [38]; additionally, some subsets, such as CD8 + cytotoxic T-lymphocytes, are important in recognizing CSCs [58] and are closely correlated with prognosis [59]. Interestingly, it was also reported that inflammatory conditions not only resulted in a decreased proportion of circulating lymphocytes (although not reported in CRC) [60, 61] but also impaired the anticancer function induced by these cytokines [62]. In our study, the level of IL-6 was observed to be negatively correlated with the ALCs, and although such a correlation seems temporary, it would also partially support its role in survival. Additionally, numerous studies have validated the prognostic value of preoperative inflammation-related markers such as the NLR and LMR in CRC, and it has been generally suggested that a high NLR or a low LMR correlates with poor survival in patients [63,64,65,66]. Interestingly, an increasing number of reports have also postoperatively explored the prognostic value of these markers. For example, in a study with 176 stage II cases, Hayama et al. found that postoperative (7 d after surgery) high NLR is a significant independent indicator for shortened relapse-free survival (RFS) [10]; furthermore, in a study with 568 stage III cases, Yasui et al. found that postoperative NLR and LMR were more accurate in predicting RFS or OS in contrast to preoperative factors [9]. In our study, no prognostic value was observed for either NLR or LMR (both preoperatively and postoperatively), which is possibly due to the small sample size, as in previous studies [67,68,69]. Furthermore, we also demonstrated no correlation of the postoperative IL-6 level with the NLR or LMR (data not shown); thus, its role in prognosis cannot be explained by these markers. We advocate that a larger sample study should be conducted to validate these findings in the future.
Our study has some clinical implications. First, when considering that the bowel is the source of the IL-6 response to surgical trauma in colorectal surgery [70], it is important to select appropriate surgical approaches for these patients. For example, laparoscopic resection is preferred in patients with right-sided lesions due to its advantages in reducing trauma and the systemic inflammatory response [71]. Second, for patients with an obviously high postoperative IL-6 level, it is important to tailor the treatment strategies due to the notorious role of IL-6 in treatment resistance [46, 47] and other functions [41,42,43]. Third, colorectal adenoma was regarded as a risk factor for CRC [72] and was detected in 7.4–52.5% of patients under colonoscopy [73]; in addition, it was also found that up to 39.4% of CRC patients can develop adenomas in postoperative surveillance [74, 75]. Interestingly, IL-6 was observed to be significantly elevated in patients with colorectal adenoma [76], and a decrease in IL-6 was negatively associated with high-risk and advanced adenoma recurrence in a previous study [77]. Based on these facts, it is important in the clinical setting to screen colorectal adenomas in CRC patients with a high postoperative level of IL-6. There were also some other limitations to our study. First, this study included a limited sample and was retrospectively conducted, and many other factors can bias the results. Second, although a long duration of high postoperative IL-6 levels was observed in CRC patients after surgery, the level of IL-6 normalized at approximately 43 d in most cases [39]. Therefore, it would be more valid to comprehensively analyze the value of these different time points in the clinical setting.
Conclusion
Overall, our results suggested that in contrast to CRP and PCT, in postoperative settings, only IL-6 was found to be a significant prognostic factor, and patients with a lower IL-6 level could have a good DFS. However, more studies with large samples are still needed to validate our findings in the future.
Data Availability
The datasets generated or analyzed during the current study are available from the corresponding author on reasonable request.
References
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145–64.
Fuglestad AJ, Meltzer S, Ree AH, McMillan DC, Park JH, Kersten C. The clinical value of C-reactive protein and its association with tumour location in patients undergoing curative surgery for colorectal cancer-a ScotScan collaborative study. Acta Oncol. 2022;61(10):1248–55.
Miyake T, Iida H, Shimizu T, Ueki T, Kojima M, Ohta H, et al. The elevation in preoperative procalcitonin is associated with a poor prognosis for patients undergoing resection for colorectal cancer. Dig Surg. 2021;38(1):80–6.
Groblewska M, Mroczko B, Wereszczyńska-Siemiatkowska U, Kedra B, Lukaszewicz M, Baniukiewicz A, et al. Serum interleukin 6 (IL-6) and C-reactive protein (CRP) levels in colorectal adenoma and cancer patients. Clin Chem Lab Med. 2008;46(10):1423–8.
Lee WS, Baek JH, You DH, Nam MJ. Prognostic value of circulating cytokines for stage III colon cancer. J Surg Res. 2013;182(1):49–54.
Kwon KA, Kim SH, Oh SY, Lee S, Han JY, Kim KH, et al. Clinical significance of preoperative serum vascular endothelial growth factor, interleukin-6, and C-reactive protein level in colorectal cancer. BMC Cancer. 2010;10:203.
Yasui K, Shida D, Nakamura Y, Ahiko Y, Tsukamoto S, Kanemitsu Y. Postoperative, but not preoperative, inflammation-based prognostic markers are prognostic factors in stage III colorectal cancer patients. Br J Cancer. 2021;124(5):933–41.
Hayama T, Hashiguchi Y, Okada Y, Ono K, Nemoto K, Shimada R, et al. Significance of the 7th postoperative day neutrophil-to-lymphocyte ratio in colorectal cancer. Int J Colorectal Dis. 2020;35(1):119–24.
Takakura Y, Hinoi T, Egi H, Shimomura M, Adachi T, Saito Y, et al. Procalcitonin as a predictive marker for surgical site infection in elective colorectal cancer surgery. Langenbecks Arch Surg. 2013;398(6):833–9.
Domínguez-Comesaña E, Estevez-Fernández SM, López-Gómez V, Ballinas-Miranda J, Domínguez-Fernández R. Procalcitonin and C-reactive protein as early markers of postoperative intra-abdominal infection in patients operated on colorectal cancer. Int J Colorectal Dis. 2017;32(12):1771–4.
Galizia G, Orditura M, Romano C, Lieto E, Castellano P, Pelosio L, et al. Prognostic significance of circulating IL-10 and IL-6 serum levels in colon cancer patients undergoing surgery. Clin Immunol. 2002;102(2):169–78.
Ding S, Ma H, Wang G, Yu Z, Li K, Huang A. Effect of remifentanil combined anesthesia on cytokines and oxidative stress in patients undergoing laparoscopic surgery for colon cancer. J Coll Physicians Surg Pak. 2019;29(1):8–11.
Margarit SC, Vasian HN, Balla E, Vesa S, Ionescu DC. The influence of total intravenous anaesthesia and isoflurane anaesthesia on plasma interleukin-6 and interleukin-10 concentrations after colorectal surgery for cancer: a randomised controlled trial. Eur J Anaesthesiol. 2014;31(12):678–84.
Hermunen K, Soveri LM, Boisen MK, Mustonen HK, Dehlendorff C, Haglund CH, et al. Postoperative serum CA19-9, YKL-40, CRP and IL-6 in combination with CEA as prognostic markers for recurrence and survival in colorectal cancer. Acta Oncol. 2020;59(12):1416–23.
Hua X, Kratz M, Malen RC, Dai JY, Lindström S, Zheng Y, et al. Association between post-treatment circulating biomarkers of inflammation and survival among stage II-III colorectal cancer patients. Br J Cancer. 2021;125(6):806–15.
Xu R, You JH, Li F, Yan B. Postoperative fasting blood glucose predicts prognosis in stage I-III colorectal cancer patients undergoing resection. Gastroenterol Res Pract. 2020;2020:2482409.
Zhang Y, Liu Y, Qiu X, Yan B. Concurrent comparison of the prognostic values of tumor budding, tumor stroma ratio, tumor infiltrating pattern and lymphocyte-to-monocyte ratio in colorectal cancer patients. Technol Cancer Res Treat. 2021;20:15330338211045826.
Huang X, Huan Y, Liu L, Ye Q, Guo J, Yan B. Preoperative low absolute lymphocyte count to fibrinogen ratio correlated with poor survival in nonmetastatic colorectal cancer. World J Surg Oncol. 2022;20(1):309.
Hailun Xie, Huang S, Yuan G, Tang S, Gan J. Prognostic significance of preoperative fibrinogen-to-prealbumin ratio in patients with stage I-III colorectal cancer undergoing surgical resection: a retrospective cohort study. Biomed Res Int. 2021;2021:3905353.
McSorley ST, Watt DG, Horgan PG, McMillan DC. Postoperative systemic inflammatory response, complication severity, and survival following surgery for colorectal cancer. Ann Surg Oncol. 2016;23(9):2832–40.
Yamamoto M, Saito H, Uejima C, Tanio A, Takaya S, Sakamoto T, et al. Prognostic value of the combination of pre- and postoperative C-reactive protein in colorectal cancer patients. Surg Today. 2018;48(11):986–93.
Matsubara D, Arita T, Nakanishi M, Kuriu Y, Murayama Y, Kudou M, et al. The impact of postoperative inflammation on recurrence in patients with colorectal cancer. Int J Clin Oncol. 2020;25(4):602–13.
Nakamura Y, Yamaura T, Kinjo Y, Kawase M, Kanto S, Kuroda N. Impact of severe postoperative inflammatory response on recurrence after curative resection of colorectal cancer. Int J Colorectal Dis. 2022;37(11):2375–86.
Aoki S, Migita K, Ueno M, Yasuda S, Fujimoto K, Doi S, et al. Postoperative serum C-reactive protein level predicts long-term outcomes in colorectal cancer patients. Gan To Kagaku Ryoho. 2020;47(13):2113–6.
Bae JH, Lee CS, Han SR, Park SM, Lee YS, Lee IK. Differences in the prognostic impact of post-operative systemic inflammation and infection in colorectal cancer patients: using white blood cell counts and procalcitonin levels. Surg Oncol. 2020;35:374–81.
Meyerhardt JA, Mayer RJ. Systemic therapy for colorectal cancer. N Engl J Med. 2005;352(5):476–87.
Li C, Xu Q, Chen L, Luo C, Ying J, Liu J. C-reactive protein (CRP) as a prognostic factor for colorectal cancer after surgical resection of pulmonary metastases. Bull Cancer. 2017;104(3):232–6.
Woo HD, Kim K, Kim J. Association between preoperative C-reactive protein level and colorectal cancer survival: a meta-analysis. Cancer Causes Control. 2015;26(11):1661–70.
Shibutani M, Maeda K, Nagahara H, Ohtani H, Sugano K, Ikeya T, et al. Elevated preoperative serum C-reactive protein levels are associated with poor survival in patients with colorectal cancer. Hepatogastroenterology. 2014;61(136):2236–40.
Platt JJ, Ramanathan ML, Crosbie RA, Anderson JH, McKee RF, Horgan PG, et al. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19(13):4168–77.
Park BS, Cho SH, Lee SH, Son GM, Kim HS. Role of C-reactive protein, white blood cell counts, and serum glucose levels as early predictors of infectious complications after laparoscopic colorectal surgery for colorectal cancer. Am Surg. 2022:31348221135786.
Keramidaris D, Koronakis N, Lagoudianakis EE, Pappas A, Koukoutsis I, Chrysikos I, et al. Procalcitonin in patients with colorectal cancer. J BUON. 2013;18(3):623–8.
Fujii T, Yajima R, Tabe Y, Yamaguchi S, Tsutsumi S, Asao T, et al. Elevated C-reactive protein is associated with the tumor depth of invasion but not with disease recurrence in stage II and III colorectal cancer. Hepatogastroenterology. 2013;60(126):1343–7.
Swede H, Hajduk AM, Sharma J, Rawal S, Rasool H, Vella AT. Baseline serum C-reactive protein and death from colorectal cancer in the NHANES III cohort. Int J Cancer. 2014;134(8):1862–70.
Hua X, Dai JY, Lindström S, Harrison TA, Lin Y, Alberts SR, et al. Genetically predicted circulating c-reactive protein concentration and colorectal cancer survival: a mendelian randomization consortium study. Cancer Epidemiol Biomarkers Prev. 2021;30(7):1349–58.
Mehigan BJ, Hartley JE, Drew PJ, Saleh A, Dore PC, Lee PW, et al. Changes in T cell subsets, interleukin-6 and C-reactive protein after laparoscopic and open colorectal resection for malignancy. Surg Endosc. 2001;15(11):1289–93.
Kamińska J, Kowalska MM, Nowacki MP, Chwaliński MG, Rysińska A, Fuksiewicz M. CRP, TNF-alpha, IL-1ra, IL-6, IL-8 and IL-10 in blood serum of colorectal cancer patients. Pathol Oncol Res. 2000;6(1):38–41.
Guthrie GJ, Roxburgh CS, Richards CH, Horgan PG, McMillan DC. Circulating IL-6 concentrations link tumour necrosis and systemic and local inflammatory responses in patients undergoing resection for colorectal cancer. Br J Cancer. 2013;109(1):131–7.
Becker C, Fantini MC, Wirtz S, Nikolaev A, Lehr HA, Galle PR, et al. IL-6 signaling promotes tumor growth in colorectal cancer. Cell Cycle. 2005;4(2):217–20.
Ashizawa T, Okada R, Suzuki Y, Takagi M, Yamazaki T, Sumi T, et al. Study of interleukin-6 in the spread of colorectal cancer: the diagnostic significance of IL-6. Acta Med Okayama. 2006;60(6):325–30.
Nagasaki T, Hara M, Nakanishi H, Takahashi H, Sato M, Takeyama H. Interleukin-6 released by colon cancer-associated fibroblasts is critical for tumour angiogenesis: anti-interleukin-6 receptor antibody suppressed angiogenesis and inhibited tumour-stroma interaction. Br J Cancer. 2014;110(2):469–78.
Hara M, Nagasaki T, Shiga K, Takahashi H, Takeyama H. High serum levels of interleukin-6 in patients with advanced or metastatic colorectal cancer: the effect on the outcome and the response to chemotherapy plus bevacizumab. Surg Today. 2017;47(4):483–9.
Li S, Tian J, Zhang H, Zhou S, Wang X, Zhang L, et al. Down-regulating IL-6/GP130 targets improved the anti-tumor effects of 5-fluorouracil in colon cancer. Apoptosis. 2018;23(5–6):356–74.
Hu Z, Ding J, Ma Z, Sun R, Seoane JA, Scott Shaffer J, et al. Quantitative evidence for early metastatic seeding in colorectal cancer. Nat Genet. 2019;51(7):1113–22.
Peach G, Kim C, Zacharakis E, Purkayastha S, Ziprin P. Prognostic significance of circulating tumour cells following surgical resection of colorectal cancers: a systematic review. Br J Cancer. 2010;102(9):1327–34.
Abdalla TSA, Meiners J, Riethdorf S, König A, Melling N, Gorges T, et al. Prognostic value of preoperative circulating tumor cells counts in patients with UICC stage I-IV colorectal cancer. PLoS ONE. 2021;16(6):e0252897.
Li YC, Zou JM, Luo C, Shu Y, Luo J, Qin J, et al. Circulating tumor cells promote the metastatic colonization of disseminated carcinoma cells by inducing systemic inflammation. Oncotarget. 2017;8(17):28418–30.
Koren E, Fuchs Y. The bad seed: Cancer stem cells in tumor development and resistance. Drug Resist Updat. 2016;28:1–12.
Du L, Cheng Q, Zheng H, Liu J, Liu L, Chen Q. Targeting stemness of cancer stem cells to fight colorectal cancers. Semin Cancer Biol. 2022;82:150–61.
Grillet F, Bayet E, Villeronce O, Zappia L, Lagerqvist EL, Lunke S, et al. Circulating tumour cells from patients with colorectal cancer have cancer stem cell hallmarks in ex vivo culture. Gut. 2017;66(10):1802–10.
Ning Y, Zhang W, Hanna DL, Yang D, Okazaki S, Berger MD, et al. Clinical relevance of EMT and stem-like gene expression in circulating tumor cells of metastatic colorectal cancer patients. Pharmacogenomics J. 2018;18(1):29–34.
Kim B, Seo Y, Kwon JH, Shin Y, Kim S, Park SJ, et al. IL-6 and IL-8, secreted by myofibroblasts in the tumor microenvironment, activate HES1 to expand the cancer stem cell population in early colorectal tumor. Mol Carcinog. 2021;60(3):188–200.
Di Franco S, Bianca P, Sardina DS, Turdo A, Gaggianesi M, Veschi V, et al. Adipose stem cell niche reprograms the colorectal cancer stem cell metastatic machinery. Nat Commun. 2021;12(1):5006.
Wang T, Song P, Zhong T, Wang X, Xiang X, Liu Q, et al. The inflammatory cytokine IL-6 induces FRA1 deacetylation promoting colorectal cancer stem-like properties. Oncogene. 2019;38(25):4932–47.
Huynh PT, Beswick EJ, Coronado YA, Johnson P, O’Connell MR, Watts T, et al. CD90(+) stromal cells are the major source of IL-6, which supports cancer stem-like cells and inflammation in colorectal cancer. Int J Cancer. 2016;138(8):1971–81.
Inoda S, Hirohashi Y, Torigoe T, Morita R, Takahashi A, Asanuma H, et al. Cytotoxic T lymphocytes efficiently recognize human colon cancer stem-like cells. Am J Pathol. 2011;178(4):1805–13.
Katayama C, Yokobori T, Ozawa N, Suga K, Shiraishi T, Okada T, et al. Low level of stromal lectin-like oxidized LDL receptor 1 and CD8 + cytotoxic T-lymphocytes indicate poor prognosis of colorectal cancer. Cancer Rep (Hoboken). 2021;4(4):e1364.
Jewell AP, Worman CP, Giles FJ, Goldstone AH. Serum levels of TNF, IL-6 and sCD23 correlate with changes in lymphocyte count in patients with B-cell chronic lymphocytic leukaemia receiving interferon-alpha therapy. Leuk Lymphoma. 1997;24(3–4):327–33.
Yu Y, Wang S, Su N, Pan S, Tu B, Zhao J, et al. Increased circulating levels of CRP and IL-6 and decreased frequencies of T and B lymphocyte subsets are associated with immune-related adverse events during combination therapy with PD-1 inhibitors for liver cancer. Front Oncol. 2022;12:906824.
Bent EH, Millán-Barea LR, Zhuang I, Goulet DR, Fröse J, Hemann MT. Microenvironmental IL-6 inhibits anti-cancer immune responses generated by cytotoxic chemotherapy. Nat Commun. 2021;12(1):6218.
Naszai M, Kurjan A, Maughan TS. The prognostic utility of pre-treatment neutrophil-to-lymphocyte-ratio (NLR) in colorectal cancer: a systematic review and meta-analysis. Cancer Med. 2021;10(17):5983–97.
Gülben K, Berberoğlu U, Öndeş B, Uyar O, Güler OC, Turanlı S. Preoperative neutrophil-to-lymphocyte ratio as a predictive factor for survival in nonmetastatic colorectal cancer. J Cancer Res Ther. 2020;16(Supplement):189–S193.
Wu Q, Hu T, Zheng E, Deng X, Wang Z. Prognostic role of the lymphocyte-to-monocyte ratio in colorectal cancer: an up-to-date meta-analysis. Med (Baltim). 2017;96(22):e7051.
Song W, Wang K, Zhang RJ, Zou SB. Prognostic value of the lymphocyte monocyte ratio in patients with colorectal cancer: a meta-analysis. Med (Baltim). 2016;95(49):e5540.
Shinji S, Ueda Y, Yamada T, Koizumi M, Yokoyama Y, Takahashi G, Hotta M, Iwai T, Hara K, Takeda K, Okusa M, Kan H, Uchida E. Combined use of preoperative lymphocyte counts and the post/preoperative lymphocyte count ratio as a prognostic marker of recurrence after curative resection of stage II colon cancer. Oncotarget. 2017;9(2):2553–64.
Leitch EF, Chakrabarti M, Crozier JE, McKee RF, Anderson JH, Horgan PG, et al. Comparison of the prognostic value of selected markers of the systemic inflammatory response in patients with colorectal cancer. Br J Cancer. 2007;97(9):1266–70.
Cha YJ, Park EJ, Baik SH, Lee KY, Kang J. Clinical significance of tumor-infiltrating lymphocytes and neutrophil-to-lymphocyte ratio in patients with stage III colon cancer who underwent surgery followed by FOLFOX chemotherapy. Sci Rep. 2019;9(1):11617.
Syk I, Mangell P, Bjartell A, Jeppsson B. Systemic interleukin-6 response to colorectal surgery originates from the bowel. Dig Surg. 2002;19(3):210–5.
Zhu P, Miao W, Gu F, Xing C. Changes of serum and peritoneal inflammatory mediators in laparoscopic radical resection for right colon carcinoma. J Minim Access Surg. 2018;15(2):115–8.
Click B, Pinsky PF, Hickey T, Doroudi M, Schoen RE. Association of colonoscopy adenoma findings with long-term colorectal cancer incidence. JAMA. 2018;319(19):2021–31.
Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370(14):1298–306.
Marques-Antunes J, Libânio D, Gonçalves P, Dinis-Ribeiro M, Pimentel-Nunes P. Incidence and predictors of adenoma after surgery for colorectal cancer. Eur J Gastroenterol Hepatol. 2017;29(8):932–8.
Facciorusso A, Di Maso M, Serviddio G, Vendemiale G, Spada C, Costamagna G, et al. Factors associated with recurrence of advanced colorectal adenoma after endoscopic resection. Clin Gastroenterol Hepatol. 2016;14(8):1148–1154e4.
Groblewska M, Mroczko B, Wereszczyńska-Siemiatkowska U, Kedra B, Lukaszewicz M, Baniukiewicz A, Szmitkowski M. Serum interleukin 6 (IL-6) and C-reactive protein (CRP) levels in colorectal adenoma and cancer patients. Clin Chem Lab Med. 2008;46(10):1423–8.
Bobe G, Albert PS, Sansbury LB, Lanza E, Schatzkin A, Colburn NH, Cross AJ. Interleukin-6 as a potential indicator for prevention of high-risk adenoma recurrence by dietary flavonols in the polyp prevention trial. Cancer Prev Res (Phila). 2010;3(6):764–75.
Acknowledgements
None.
Funding
This work was supported by Hainan Provincial Natural Science Foundation of China (823MS164) and the Bureau of Huzhou Science and Technology (2020GY13).
Author information
Authors and Affiliations
Contributions
BY was responsible for the conception of the work. QY, TX and BY obtained the data. SF and BY analyzed the data. SF, ZL, ML and BY wrote the manuscript. ZL, ML and BY critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was carried out in accordance with the principles stated in the Declaration of Helsinki and was approved by the ethics committee of Hainan Hospital of PLA General Hospital and the requirement for written informed consent was waived due to its retrospective nature.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Feng, S., Li, Z., Liu, M. et al. Postoperative serum interleukin-6 levels correlate with survival in stage I-III colorectal cancer. BMC Gastroenterol 23, 156 (2023). https://doi.org/10.1186/s12876-023-02800-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02800-9