Abstract
Background
Preoperative absolute lymphocyte count (LC) and fibrinogen (FIB) are useful prognostic indicators in colorectal cancer (CRC). However, the prognostic value of the LC to FIB ratio (LFR) has never been addressed.
Methods
A total of 189 nonmetastatic CRC patients after resection were enrolled retrospectively. The significance of the LFR in predicting disease-free survival (DFS) and overall survival (OS) was estimated by receiver operating characteristic curve analysis, and the prognostic efficacy was compared with individual LC and FIB. Patients were assigned to LFR low or high subgroups. Differences in clinicopathological features among these subgroups were calculated, and the survival differences of these subgroups were determined by the Kaplan-Meier analysis. A Cox proportional hazards model was applied to test the risk factors for survival.
Results
Taking 0.54 as the optimal cutoff point, the LFR had sensitivities of 79.70% and 86.40% and specificities of 52.30% and 51.00% in predicting the DFS and OS, respectively. A total of 109/189 (57.67%) patients were assigned to the LFR low group, and these patients were more likely to be characterized by criteria such as T3 + T4 (P < 0.01), stage 3 (P < 0.01), tumor deposits (P = 0.01), high CEA (P < 0.01), or CA19-9 levels (P = 0.04). And they also displayed worse DFS (log rank = 18.57, P < 0.01) and OS (log rank = 20.40, P < 0.01) than the high LFR group. Finally, the LFR was independently associated with inferior DFS (HR = 0.32, 95% CI: 0.16–0.61, P < 0.01) and OS (HR = 0.23, 95% CI: 0.09–0.55, P < 0.01).
Conclusions
The LFR is a useful prognostic indicator in nonmetastatic CRC, and patients with a relatively low LFR had poor survival.
Similar content being viewed by others
Colorectal cancer (CRC) is still a major cause of cancer-related death worldwide [1]. In contrast to the USA, in which the age-standardized incidence and mortality rates of the disease have decreased noticeably in recent years, the incidence rate is still increasing in China [2]. Although the majority of early stage cases can be cured by surgery or surgery plus adjuvant chemotherapy (AC) [3], over a third of patients will die within 5 years [4]. Developing for a reliable and easily accessible prognostic indicator is still important in practice, particularly for the determination of therapeutic strategies.
Cancer-associated inflammation is regarded as one of the hallmarks of cancer [5] and plays an essential role at different stages of cancer development [6]. The elevated cytokines and chemokines in the inflammatory environment can alter not only the proportions of inflammatory cells [7, 8] but also their functions [9]. Lymphocytes are an important component of leukocytes and are the main player in adaptive anticancer immunity [10]. Lymphocytes have profound effects in many aspects of cancer, such as inhibiting their occurrence [11], preventing dissemination [12] or recurrence [13], and regulating treatment response [14]. Not unexpectedly, the count of these cells in peripheral blood as well as in the tumor microenvironment (TME) was also found to have an important role in prognosis in many malignancies [15,16,17] including CRC [18,19,20]. Taking into consideration that the altered proportion of leukocytes in the inflammatory environment would also be meaningful in reflecting the anticancer immune response, a series of new prognostic indicators were established to further improve the prognostic efficacy based on absolute lymphocyte count (LC) in CRC, including the neutrophil to lymphocyte ratio (NLR: defined as the absolute number of neutrophils divided by the number of lymphocytes) [21], lymphocyte to monocyte ratio (LMR: defined as the absolute number of lymphocytes divided by the number of monocytes) [22], and LANR (defined as the absolute number of lymphocytes multiplied by the level of albumin and divided by the absolute number of neutrophils) [23].
Interestingly, some inflammation-related proteins were also found to be prognostically meaningful in addition to these inflammatory cells. Fibrinogen (FIB), which is a glycoprotein that is mainly synthesized by the liver as an acute-phase response, was previously thought to play a role mainly in coagulation [24]. However, it was found that FIB could also be released by cancer cells [25] and involved in many other biological processes including tumor angiogenesis, cancer cell proliferation, adhesion, and migration [26, 27]. Based on these data, mounting evidence indicates that a frequently elevated FIB in cancer patients is associated with poor survival [28,29,30,31,32,33] which includes CRC [34, 35]. Nonetheless, it is worth noting that neither single LC nor single FIB was sufficient to provide a precise prediction of the prognosis in CRC. As previous studies have indicated, the area under the curves (AUCs) for individual LC in predicting the outcome ranged from 0.58 to 0.61 with a relatively low sensitivity or specificity [19, 36]. In line with this, the AUC for FIB in predicting overall survival (OS) was only 0.57 [37], and the optimal cutoff points were highly inconsistent in these studies for both LC and FIB [19, 34, 38]. Therefore, it is plausible that a combination of these two indicators, namely, the LC to FIB ratio (LFR) could be more reliable in prognosis for CRC patients. However, there is currently little research on the LFR in CRC.
In this study, we aimed to explore the prognostic value of LFR and compare its prognostic efficacy with individual LC and FIB. Further, we tested the usefulness of LFR in normal carcinoembryonic antigen (CEA) cases in CRC.
Methods
Study population
Data from patients who received radical resection of the primary lesion at the Hainan Hospital of Chinese PLA General Hospital were retrospectively collected from December 2012 to June 2020. Those who met any one of the following criteria were excluded: (1) any preoperative neoadjuvant therapies, (2) evidence of distant metastasis by imaging examinations, (3) in situ lesions or active immune system diseases, (4) the usage of any anticoagulant drugs, (5) lacking preoperative laboratory results for blood or coagulation function tests, (6) lacking any of pathological TNM information, and (7) lacking reliable follow-up or a follow-up duration less than 3 years (y)/36 months (m). Other data, including tobacco or alcohol use history and complications (mainly hypertension and type 2 diabetes), were collected as described previously [39,40,41]. Tumor stage was followed by the seventh edition of the American Joint Committee on Cancer staging manual. The study was performed in line with the principles stated in the Declaration of Helsinki and was approved by the ethics committee of the Hainan Hospital of Chinese PLA General Hospital (ID: 301HLFYLS15). Patients or their relatives authorized provided the informed consent.
Definition of LFR and other prognostic indicators
Peripheral venous blood was collected between 6:00 am and 9:00 am before breakfast within 1 week before the operation and processed in clinical laboratory center as described previously [40]. The blood sample was centrifuged at 3000–3600 r/min (ST-16, Thermo Fisher Scientific, USA), and upper plasma was then tested for tumor markers (CEA: 0–5 μg/ml, CA19-9: 0–37 μg/ml) using the electrochemiluminescence method with the automatic analysis system (Cobas e 601, Roche, Switzerland) and FIB using the Fibrinogen-C XL Kit according to the manufacturer’s instructions (ACL TOP 700, A Werfen Company, USA). The specific cell fraction in blood was analyzed using an automatic blood cell analyzer (XN3000, Sysmex Corporation, Japan). The blood sample was placed in the analyzer where a portion of it was automatically diluted to a 1:60 dilution and lysed by the addition of the special Sysmex lysing reagent (Lysercell WDF). Fluorocell WDF was then added, and the entire dilution was maintained at a constant temperature for a defined time period to label the nucleated cells in the sample. The labeled sample was then moved into the sheath flow detector where side scattered light and side fluorescence were measured allowing the LC to be computed. The LFR was calculated by the absolute number of LCs divided by the level of the FIB and then divided by 109 to facilitate the data input. Other established prognostic indices, including NLR, LMR, platelet counts to lymphocyte ratio (PLR: defined as the absolute number of lymphocytes divided by the number of platelets), and prognostic nutritional index (PNI: defined as the level of albumin plus 5 multiplied by the absolute number of lymphocytes and then divided by 109), were also collected as previously described [21, 22, 42].
Definition of disease-free survival (DFS) and OS
The follow-up was conducted as described previously [40] and routine laboratory tests and imaging examinations including computed tomography, magnetic resonance imaging, and ultrasonography were performed in this period. DFS was defined from the date of surgery to the date of any recurrence or metastasis or the date of death from any cause, and OS was defined from the same point to the point of any cause of death. The latest follow-up point ended in December 2021.
Statistical analysis
All statistical analyses were performed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA), MedCalc v19.0.7 (MedCalc Software Ltd., Ostend, Belgium), and GraphPad Prism 5 (GraphPad Software Inc., San Diego, CA, USA). Receiver operating characteristic curve (ROC) analysis was used to identify the predicting efficacy of LFR for DFS and OS, with an optimal discriminator point to check the sensitivity and specificity. In addition, the AUC of LFR was compared with individual LC and FIB. The relationship of the LFR with the NLR, LMR, PLR, and PNI was determined by the Pearson correlation coefficient. Patients were assigned to LFR low or high subgroups based on the optimal discriminator point, and the differences in clinicopathological data among these subgroups were using a χ2 test or Student’s t-test. DFS and OS differences between LFR low and high subgroups were estimated by a Kaplan-Meier analysis followed by log-rank tests. Risk factors for survival were checked using the Cox proportional hazards model. All tests were two sided with P < 0.05 regarded as statistically significant, and all the results were kept to a maximum of two decimal places.
Results
Patients’ demographics and the prognostic efficacy of LFR
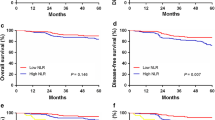
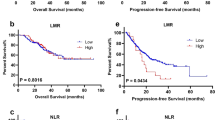
A total of 189 patients were included in the study (Fig. 1) with 40, 77, and 72 stages 1, 2, and 3 cases, respectively. During the follow-up, 2 patients in stage 1, 17 patients in stage 2, and 25 patients in stage 3 died, and the 3-year (y) overall survival rate was 76.72% (145/189). The mean age of these patients was 59.61 years (range: 26–85 years). And the mean follow-up period was 64.40 m (range: 1–114 m). By ROC tests, the LFR had sensitivities of 79.70% and 86.40% and specificities of 52.30% and 51.00% in predicting the DFS (AUC = 0.67, P < 0.01) and OS (AUC = 0.74, P < 0.01), respectively (Fig. 2 A–B). The prognostic efficacy of LFR was superior to LC (AUC = 0.68, Z = 2.04, P = 0.04) or FIB (AUC = 0.66, Z = 2.14, P = 0.03) alone for OS but not for DFS (LC: AUC = 0.63, Z = 1.04, P = 0.30; FIC: AUC = 0.58, Z = 1.95, P = 0.05). Interestingly, the prognostic efficacy of LFR was also significant in CEA normal cases both for DFS (AUC = 0.67, P = 0.01) and OS (AUC = 0.75, P < 0.01; Fig. 2 C–D).
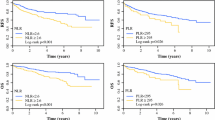
Correlation of LFR with NLR, LMR, PLR, and PNI
Using a Pearson correlation analysis, we found a significant positive correlation between LFR and LMR (r = 0.46, P < 0.01) and LFR and PNI (r = 0.66, P < 0.01) and a negative correlation between LFR and NLR (r = −0.41, P < 0.01) and LFR and PLR (r = −0.56, P < 0.01). The strengths of these correlations were moderate, with the LFR and PNI being the strongest (Fig. 3).
Differences in clinicopathological parameters among LFR subgroups
Taking 0.54 as the optimal cutoff point according to the Youden index in ROC tests, patients were assigned to the LFR low (< 0.54) or high (≥ 0.54) subgroups, and patients in the LFR low group were more likely to be characterized by criteria such as T3 + T4 (P < 0.01), stage 3 (P < 0.01), tumor deposits (P = 0.01), high CEA (P < 0.01), or CA19-9 levels (P = 0.04; Table 1).
Survival differences in LFR subgroups
Using a Kaplan-Meier analysis, we found that patients in the low LFR group displayed an obviously worse DFS in stage 3 and OS in stages 2–3 than those in the high LFR group (Fig. 4 A–F). Patients with a relatively low LFR showed significantly poorer DFS (log rank = 18.57, P < 0.01) and OS (log rank = 20.40, P < 0.01) than those with a high LFR in the whole cohort (Fig. 4 G–H). Additionally, the DFS (log rank = 8.46, P < 0.01) and OS (log rank = 10.43, P < 0.01) were also worse in those patients with a normal CEA level (Fig. 4 I–J).
Univariate and multivariate tests of risk factors for DFS and OS
Using univariate analysis, gender, tumor deposits, CEA, or CA19-9 levels, combined T and N stages, TNM stages, BMI, and LFR, were found to be significant risk factors for both DFS and OS; additionally, age and histological grade were found to also be significant risk factors for OS (Table 2). When these factors (only P < 0.05) were integrated into multivariate analysis, the LFR was found to be an independent risk factor for both DFS (HR = 0.32, 95% CI: 0.16–0.61, P < 0.01) and OS (HR = 0.23, 95% CI: 0.09–0.55, P < 0.01) (Table 3).
Discussion
In this study, we found that the LFR could be used as a reliable prognostic indicator in nonmetastatic CRC, and its prognostic efficacy is likely to be superior to individual LC or FIB with regard to OS. Patients with a relatively low LFR had worse survival than those with a high LFR, and the LFR was an independent risk factor for the outcome in these patients. Additionally, the role of LFR in prognosis was maintained in CEA normal cases and could be effectively distinguished from those that have a poor outcome. To the best of our knowledge, this is the first report concerning the role of LFR in CRC.
It is notable that the prognostic value of LC and FIB has been validated in CRC previously but with individual limitations. For LC, Liang et al. collected 1332 stage 2 patients which included 459 patients who presented high risk of AC, and their results showed that pretreatment LC (cutoff 1300/mm3) was independently associated with survival [24]. In line with this, Noh et al. performed a study with 231 stages 2–3 patients who received curative surgery in addition to the subsequent FOLFOX regimen AC and suggested that LC was also independently correlated with the outcome [18]. However, the use of LC in predicting survival may limited by its relatively small AUC and inconsistent cutoff points. For example, Iseki et al. reported that the AUC for a single LC (cutoff 1700/mm3) in predicting DFS was 0.55, which was not statistically significant, but it was useful in predicting OS (cutoff 1100/mm3, AUC = 0.59) [19]. Similarly, Tanio et al. found that the AUC for a single LC (cutoff 1460/mm3) in predicting OS was only 0.55 [43]. For FIB, Silvestris et al. conducted a study with 139 metastatic cases that received bevacizumab-based therapy and found that the AUC for FIB in forecasting DFS was 0.62 and further reduced to 0.57 in predicting OS [37]. However, similar to single LC, the cutoff points for FIB were highly inconsistent as described by a systematic review and meta-analysis [34]. In recent years, some new prognostic indicators have been established based on these markers in CRC to improve prognostic efficacy. Examples have been reported, such as NLR [21], LMR [44], the FIB and NLR ratio [45], and the FIB to prealbumin ratio [41, 42]. However, it is notable that reports regarding the role of LFR in cancer are still scarce, with only a few relevant studies but only with some relevant studies. For example, Liu et al. included 375 stages 1–4 non-small cell lung cancer patients and explored the prognostic role of the FIB-to-lymphocyte percentage ratio (FLpR), and the results indicated that patients with a high FLpR would have an increased risk of death [46]. In addition, Huang et al. indicated that a high FIB to LC ratio (FLR) correlated with peritoneal dissemination in gastric cancer [47]. Though these results are not from CRC, they could also support the idea that a low LFR (equal to a high FLpR or FLR) correlates with poor outcome. Interestingly, we also found a positive correlation of FLR with LMR and PNI but a negative correlation with NLR and PLR. As the prognostic role of these markers has been extensively validated in previous reports [21, 41, 43], we believe it could partly validate the value of LFR in our study.
Mechanistically, it is well established that lymphocytes have an extensive effect in cancer, including the inhibition of occurrence and growth [11, 48], prevention of dissemination [12], and recurrence [13]. In recent years, colorectal cancer stem cells (CCSCs) or cancer-initiating cells have been identified and are thought to be the ultimate source of cancer initiation, progression, resurrection, and treatment resistance [49,50,51]. These cells in the circulatory system play a key role in cancer metastasis and recurrence [52, 53]. Interestingly, lymphocytes can efficiently recognize and eradicate these cells [54]. In addition, FIB has been found to have a broad effect on cancer development except for the aforementioned involvement of biological processes [27, 28]. Recently, it has also been reported that FIB in the TME can contribute to the invasiveness of glioblastoma tumor-initiating cells [55], and it can promote malignant biological tumor behavior by regulating epithelial-mesenchymal transition [56]. As in CRC, other researchers have found that FIB can coordinate with platelets in protecting cancer cells from natural killer cytotoxicity [57] and support tumor growth as well as local invasion and metastasis [58]. These functions could contribute to the support of CCSCs. Additionally, cancer-related inflammation is regarded as a hallmark of the disease [5], and some inflammatory factors can have a profound role in the development of the disease, particularly IL-6. As previous studies have indicated, peripheral blood IL-6 is significantly elevated in CRC patients [59, 60], which could contribute to T-lymphocyte cell-mediated immunosuppression [61]. As indicated in another study conducted in lung cancer, patients with high circulating IL-6 levels have significantly more T-regulatory cells and increased programmed cell death protein-1 expression on lymphocytes [62]. Notably, FIB was found to act not only as an inhibitor of lymphocyte adherence and cytotoxicity against cancer cells [63] but also as a source of induction of IL-6 [64]. Taking these studies into account, it is reasonable that patients with a low LFR could have impaired anticancer immunity (in particular those with abnormally elevated IL-6) and attenuated efficacy in killing CCSCs but with enhanced tumor aggressiveness and strengthened tumor protection, which could then lead to a poor prognosis. However, these ideas require further study.
Traditionally, CEA was a reliable prognostic indicator as recommended by ASCO in CRC [65]. However, its prognostic value is largely limited by its minimal sensitivity, as only 21–36% of patients are positive at diagnosis [66]. In addition, its efficacy is weaker in patients with type 2 diabetes or with a history of smoking [67, 68]. Some investigators have looked in normal patients for candidates for CEA, such as CA724 [69] and CA19-9 [70], and the Glasgow prognostic score [71]. However, these reports did not show the AUCs for the tested markers [69,70,71], and a large proportion of patients with normal CEA would also have normal CA724 (242/295) [69] and CA19-9 (333/385) [70]. In our study, the AUC for LFR in CEA normal cases in predicting DFS and OS was 0.67 and 0.75, respectively, meaning that patients with a low LFR also had a significantly inferior outcome. These results indicate that the LFR could also be a useful prognostic indicator in such a scenario.
There are still several limitations to the present study. First, the study is retrospective in nature with a relatively small sample size, and some biases are present. Second, peripheral lymphocytes are highly heterogeneous with distinct or even opposite functions, and some of these cells was have been found to have no impact on survival [72]. It would be more reasonable to sort a specific cluster, such as CD4+ or CD8+ cells and then examine the value of LFR. Third, both the LC and FIB are dynamic markers in the patients and could be affected by surgery and AC [73, 74]. Longitudinal measurements of LFR and further validation of its prognostic value are necessary in the future.
Conclusion
Overall, our results indicated that the LFR could be regarded as a reliable prognostic indicator in nonmetastatic CRC, and that patients with a relatively low LFR have worse survival.
Availability of data and materials
The datasets generated or analyzed during the current study are available from the corresponding author (BY) on reasonable request.
Abbreviations
- LC:
-
Lymphocyte count
- FIB:
-
Fibrinogen
- CRC:
-
Colorectal cancer
- LFR:
-
LC to FIB ratio
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- AC:
-
Adjuvant chemotherapy
- TME:
-
Tumor microenvironment
- NLR:
-
Neutrophil to lymphocyte ratio
- LMR:
-
Lymphocyte to monocyte ratio
- AUCs:
-
Area under the curves
- CEA:
-
Carcinoembryonic antigen
- PLR:
-
Platelet counts to lymphocyte ratio
- PNI:
-
Prognostic nutritional index
- ROC:
-
Receiver operating characteristic curve
- CCSCs:
-
Colorectal cancer stem cells
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Xia C, Dong X, Li H, Cao M, Sun D, He S, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J. 2022;135(5):584–90.
Markowitz SD, Bertagnolli MM. Molecular origins of cancer: molecular basis of colorectal cancer. N Engl J Med. 2009;361(25):2449–60.
Klintrup K, Mäkinen JM, Kauppila S, Väre PO, Melkko J, Tuominen H, et al. Inflammation and prognosis in colorectal cancer. Eur J Cancer. 2005;41(17):2645–54.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Thorsson V, Gibbs DL, Brown SD, Wolf D, Bortone DS, Ou Yang TH, et al. The immune landscape of cancer. Immunity. 2018;48(4):812–830.e14.
Tosolini M, Kirilovsky A, Mlecnik B, Fredriksen T, Mauger S, Bindea G, et al. Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, Th2, Treg, Th17) in patients with colorectal cancer. Cancer Res. 2011;71(4):1263–71.
Fiegle E, Doleschel D, Koletnik S, Rix A, Weiskirchen R, Borkham-Kamphorst E, et al. Dual CTLA-4 and PD-L1 blockade inhibits tumor growth and liver metastasis in a highly aggressive orthotopic mouse model of colon cancer. Neoplasia. 2019;21(9):932–44.
Disis ML. Immune regulation of cancer. J Clin Oncol. 2010;28(29):4531–8.
Imai K, Matsuyama S, Miyake S, Suga K, Nakachi K. Natural cytotoxic activity of peripheral-blood lymphocytes and cancer incidence: an 11-year follow-up study of a general population. Lancet. 2000;356(9244):1795–9.
Lissoni P, Barni S, Rovelli F, Rescaldani R, Rizzo V, Biondi A, et al. Correlation of serum interleukin-2 levels, soluble interleukin-2 receptors and T lymphocyte subsets in cancer patients. Tumori. 1990;76(1):14–7.
McMillan DC, Fyffe GD, Wotherspoon HA, Cooke TG, McArdle CS. Prospective study of circulating T-lymphocyte subpopulations and disease progression in colorectal cancer. Dis Colon Rectum. 1997;40(9):1068–71.
Paijens ST, Vledder A, de Bruyn M, Nijman HW. Tumor-infiltrating lymphocytes in the immunotherapy era. Cell Mol Immunol. 2021;18(4):842–59.
Clark EJ, Connor S, Taylor MA, Madhavan KK, Garden OJ, Parks RW. Preoperative lymphocyte count as a prognostic factor in resected pancreatic ductal adenocarcinoma. HPB. 2007;9(6):456–60.
Park SJ, Lee J, Kim H, Shin K, Lee M, Park JM, et al. Association between absolute lymphocyte count and overall mortality in patients with surgically resected gastric cancer. Korean J Intern Med. 2021;36(3):679–88.
Yamanouchi K, Maeda S, Takei D, Koga Y, Yamashita M, Hamada T, et al. Pretreatment absolute lymphocyte count and neutrophil-to-lymphocyte ratio are prognostic factors for stage III breast cancer. Anticancer Res. 2021;41(7):3625–34.
Noh OK, Oh SY, Kim YB, Suh KW. Prognostic significance of lymphocyte counts in colon cancer patients treated with FOLFOX chemotherapy. World J Surg. 2017;41(11):2898–905.
Iseki Y, Shibutani M, Maeda K, Nagahara H, Tamura T, Ohira G, et al. The impact of the preoperative peripheral lymphocyte count and lymphocyte percentage in patients with colorectal cancer. Surg Today. 2017;47(6):743–54.
Idos GE, Kwok J, Bonthala N, Kysh L, Gruber SB, Qu C. The prognostic implications of tumor infiltrating lymphocytes in colorectal cancer: a systematic review and meta-analysis. Sci Rep. 2020;10(1):3360.
Li Z, Zhao R, Cui Y, Zhou Y, Wu X. The dynamic change of neutrophil to lymphocyte ratio can predict clinical outcome in stage I-III colon cancer. Sci Rep. 2018;8(1):9453.
Stotz M, Pichler M, Absenger G, Szkandera J, Arminger F, Schaberl-Moser R, et al. The preoperative lymphocyte to monocyte ratio predicts clinical outcome in patients with stage III colon cancer. Br J Cancer. 2014;110(2):435–40.
Liang X, Yao S, Lu P, Ma Y, Xu H, Yin Z, et al. The prognostic value of new index (LANR) composed of pre-operative lymphocytes, albumin, and neutrophils in patients with resectable colorectal cancer. Front Oncol. 2021;11:610264.
Tennent GA, Brennan SO, Stangou AJ, O'Grady J, Hawkins PN, Pepys MB. Human plasma fibrinogen is synthesized in the liver. Blood. 2007;109(5):1971–4.
Sahni A, Simpson-Haidaris PJ, Sahni SK, Vaday GG, Francis CW. Fibrinogen synthesized by cancer cells augments the proliferative effect of fibroblast growth factor-2 (FGF-2). J Thromb Haemost. 2008;6(1):176–83.
Sahni A, Francis CW. Vascular endothelial growth factor binds to fibrinogen and fibrin and stimulates endothelial cell proliferation. Blood. 2000;96(12):3772–8.
Simpson-Haidaris PJ, Rybarczyk B. Tumors and fibrinogen. The role of fibrinogen as an extracellular matrix protein. Ann N Y Acad Sci. 2001;936:406–25.
Zhang Y, Cao J, Deng Y, Huang Y, Li R, Lin G, et al. Pretreatment plasma fibrinogen level as a prognostic biomarker for patients with lung cancer. Clinics. 2020;75:e993.
Wakatsuki K, Matsumoto S, Migita K, Ito M, Kunishige T, Nakade H, et al. Preoperative plasma fibrinogen is associated with lymph node metastasis and predicts prognosis in resectable esophageal cancer. World J Surg. 2017;41(8):2068–77.
Mei Y, Liu H, Sun X, Li X, Zhao S, Ma R. Plasma fibrinogen level may be a possible marker for the clinical response and prognosis of patients with breast cancer receiving neoadjuvant chemotherapy. Tumour Biol. 2017;39(6):1010428317700002.
Yu X, Hu F, Yao Q, Li C, Zhang H, Xue Y. Serum fibrinogen levels are positively correlated with advanced tumor stage and poor survival in patients with gastric cancer undergoing gastrectomy: a large cohort retrospective study. BMC Cancer. 2016;16:480.
Selzer E, Grah A, Heiduschka G, Kornek G, Thurnher D. Pre-therapeutic fibrinogen levels are of prognostic significance in locally advanced head and neck cancer. Wien Klin Wochenschr. 2016;128(9-10):320–8.
Sun Y, Han W, Song Y, Gao P, Yang Y, Yu D, et al. Prognostic value of preoperative fibrinogen for predicting clinical outcome in patients with nonmetastatic colorectal cancer. Cancer Manag Res. 2020;12:13301–9.
Li M, Wu Y, Zhang J, Huang L, Wu X, Yuan Y. Prognostic value of pretreatment plasma fibrinogen in patients with colorectal cancer: a systematic review and meta-analysis. Medicine. 2019;98(37):e16974.
Hong T, Shen D, Chen X, Wu X, Hua D. Preoperative plasma fibrinogen, but not D-dimer might represent a prognostic factor in non-metastatic colorectal cancer: a prospective cohort study. Cancer Biomark. 2017;19(1):103–11.
Shinji S, Ueda Y, Yamada T, Koizumi M, Yokoyama Y, Takahashi G, et al. Combined use of preoperative lymphocyte counts and the post/preoperative lymphocyte count ratio as a prognostic marker of recurrence after curative resection of stage II colon cancer. Oncotarget. 2017;9(2):2553–64.
Silvestris N, Scartozzi M, Graziano G, Santini D, Lorusso V, Maiello E, et al. Basal and bevacizumab-based therapy-induced changes of lactate dehydrogenases and fibrinogen levels and clinical outcome of previously untreated metastatic colorectal cancer patients: a multicentric retrospective analysis. Expert Opin Biol Ther. 2015;15(2):155–62.
Milasiene V, Stratilatovas E, Norkiene V, Jonusauskaite R. Lymphocyte subsets in peripheral blood as prognostic factors in colorectal cancer. J Buon. 2005;10(2):261–4.
Xu R, You JH, Li F, Yan B. Postoperative fasting blood glucose predicts prognosis in stage I-III colorectal cancer patients undergoing resection. Gastroenterol Res Pract. 2020;2020:2482409.
Zhang Y, Liu Y, Qiu X, Yan B. Concurrent comparison of the prognostic values of tumor budding, tumor stroma ratio, tumor infiltrating pattern and lymphocyte-to-monocyte ratio in colorectal cancer patients. Technol Cancer Res Treat. 2021;20:15330338211045826.
Ying HQ, Sun F, Liao YC, Cai D, Yang Y, Cheng XX. The value of circulating fibrinogen-to-pre-albumin ratio in predicting survival and benefit from chemotherapy in colorectal cancer. Ther Adv Med Oncol. 2021;13:17588359211022886.
Xie H, Huang S, Yuan G, Tang S, Gan J. Prognostic significance of preoperative fibrinogen-to-prealbumin ratio in patients with stage I-III colorectal cancer undergoing surgical resection: a retrospective cohort study. Biomed Res Int. 2021;2021:3905353.
Tanio A, Saito H, Uejima C, Takaya S, Yamamoto M, Tokuyasu N, et al. A prognostic index for colorectal cancer based on preoperative absolute lymphocyte, monocyte, and neutrophil counts. Surg Today. 2019;49(3):245–53.
Ozawa T, Ishihara S, Kawai K, Kazama S, Yamaguchi H, Sunami E, et al. Impact of a lymphocyte to monocyte ratio in stage IV colorectal cancer. J Surg Res. 2015;199(2):386–92.
Li X, An B, Zhao Q, Qi J, Wang W, Zhang D, et al. Combined fibrinogen and neutrophil-lymphocyte ratio as a predictive factor in resectable colorectal adenocarcinoma. Cancer Manag Res. 2018;10:6285–94.
Liu M, Yang J, Wan L, Zhao R. Elevated pretreatment fibrinogen-to-lymphocyte percentage ratio predict tumor staging and poor survival in non-small cell lung cancer patients with chemotherapy or surgery combined with chemotherapy. Cancer Manag Res. 2021;13:4921–33.
Huang C, Liu Z, Xiao L, Xia Y, Huang J, Luo H, et al. Clinical significance of serum CA125, CA19-9, CA72-4, and fibrinogen-to-lymphocyte ratio in gastric cancer with peritoneal dissemination. Front Oncol. 2019;9:1159.
Paholyuk TD, Zacharzeva LM, Koshel KV, Oliynichenko GP, Berezhnaya NM. Stage of differentiation, proliferative index of tumor cells and cytotoxic activity of peripheral blood lymphocytes in colorectal cancer patients. Exp Oncol. 2004;26(2):161–3.
Gupta R, Bhatt LK, Johnston TP, Prabhavalkar KS. Colon cancer stem cells: Potential target for the treatment of colorectal cancer. Cancer Biol Ther. 2019;20(8):1068–82.
Zhou Y, Xia L, Wang H, Oyang L, Su M, Liu Q, et al. Cancer stem cells in progression of colorectal cancer. Oncotarget. 2017;9(70):33403–15.
Du L, Cheng Q, Zheng H, Liu J, Liu L, Chen Q. Targeting stemness of cancer stem cells to fight colorectal cancers. Semin Cancer Biol. 2022;82:150–61.
Pilati P, Mocellin S, Bertazza L, Galdi F, Briarava M, Mammano E, et al. Prognostic value of putative circulating cancer stem cells in patients undergoing hepatic resection for colorectal liver metastasis. Ann Surg Oncol. 2012;19(2):402–8.
Grillet F, Bayet E, Villeronce O, Zappia L, Lagerqvist EL, Lunke S, et al. Circulating tumour cells from patients with colorectal cancer have cancer stem cell hallmarks in ex vivo culture. Gut. 2017;66(10):1802–10.
Inoda S, Hirohashi Y, Torigoe T, Morita R, Takahashi A, Asanuma H, et al. Cytotoxic T lymphocytes efficiently recognize human colon cancer stem-like cells. Am J Pathol. 2011;178(4):1805–13.
Dzikowski L, Mirzaei R, Sarkar S, Kumar M, Bose P, Bellail A, et al. Fibrinogen in the glioblastoma microenvironment contributes to the invasiveness of brain tumor-initiating cells. Brain Pathol. 2021;31(5):e12947.
Zhang F, Wang Y, Sun P, Wang ZQ, Wang DS, Zhang DS, et al. Fibrinogen promotes malignant biological tumor behavior involving epithelial-mesenchymal transition via the p-AKT/p-mTOR pathway in esophageal squamous cell carcinoma. J Cancer Res Clin Oncol. 2017;143(12):2413–24.
Zheng S, Shen J, Jiao Y, Liu Y, Zhang C, Wei M, et al. Platelets and fibrinogen facilitate each other in protecting tumor cells from natural killer cytotoxicity. Cancer Sci. 2009;100(5):859–65.
Adams GN, Rosenfeldt L, Frederick M, Miller W, Waltz D, Kombrinck K, et al. Colon cancer growth and dissemination relies upon thrombin, stromal PAR-1, and fibrinogen. Cancer Res. 2015;75(19):4235–43.
Kamińska J, Kowalska MM, Nowacki MP, Chwaliński MG, Rysińska A, Fuksiewicz M. CRP, TNF-alpha, IL-1ra, IL-6, IL-8 and IL-10 in blood serum of colorectal cancer patients. Pathol Oncol Res. 2000;6(1):38–41.
Kim B, Seo Y, Kwon JH, Shin Y, Kim S, Park SJ, et al. IL-6 and IL-8, secreted by myofibroblasts in the tumor microenvironment, activate HES1 to expand the cancer stem cell population in early colorectal tumor. Mol Carcinog. 2021;60(3):188–200.
Bent EH, Millán-Barea LR, Zhuang I, Goulet DR, Fröse J, Hemann MT. Microenvironmental IL-6 inhibits anti-cancer immune responses generated by cytotoxic chemotherapy. Nat Commun. 2021;12(1):6218.
Rice SJ, Liu X, Zhang J, Jia B, Zheng H, Belani CP. Advanced NSCLC patients with high IL-6 levels have altered peripheral T cell population and signaling. Lung Cancer. 2019;131:58–61.
Biggerstaff JP, Weidow B, Dexheimer J, Warnes G, Vidosh J, Patel S, et al. Soluble fibrin inhibits lymphocyte adherence and cytotoxicity against tumor cells: implications for cancer metastasis and immunotherapy. Clin Appl Thromb Hemost. 2008;14(2):193–202.
Masamune A, Kikuta K, Watanabe T, Satoh K, Hirota M, Hamada S, et al. Fibrinogen induces cytokine and collagen production in pancreatic stellate cells. Gut. 2009;58(4):550–9.
Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N, Macdonald JS, et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol. 2006;24(33):5313–27.
Carriquiry LA, Piñeyro A. Should carcinoembryonic antigen be used in the management of patients with colorectal cancer? Dis Colon Rectum. 1999;42(7):921–9.
Huang CS, Chen CY, Huang LK, Wang WS, Yang SH. Postoperative serum carcinoembryonic antigen levels cannot predict survival in colorectal cancer patients with type II diabetes. J Chin Med Assoc. 2020;83(10):911–7.
Huang CS, Chen CY, Huang LK, Wang WS, Yang SH. Prognostic value of postoperative serum carcinoembryonic antigen levels in colorectal cancer patients who smoke. PLoS One. 2020;15(6):e0233687.
Kuang J, Gong Y, Xie H, Yan L, Huang S, Gao F, et al. The prognostic value of preoperative serum CA724 for CEA-normal colorectal cancer patients. PeerJ. 2020;8:e8936.
Lin PC, Lin JK, Lin CC, Wang HS, Yang SH, Jiang JK, et al. Carbohydrate antigen 19-9 is a valuable prognostic factor in colorectal cancer patients with normal levels of carcinoembryonic antigen and may help predict lung metastasis. Int J Color Dis. 2012;27(10):1333–8.
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Kubota K. Inflammation-based prognostic system predicts postoperative survival of colorectal cancer patients with a normal preoperative serum level of carcinoembryonic antigen. Ann Surg Oncol. 2012;19(11):3422–31.
Dylag-Trojanowska K, Rogala J, Pach R, Siedlar M, Baran J, Sierzega M, et al. T regulatory CD4+CD25+FoxP3+ lymphocytes in the peripheral blood of left-sided colorectal cancer patients. Medicina. 2019;55(6):307.
Chu-Yuan H, Jing P, Yi-Sheng W, He-Ping P, Hui Y, Chu-Xiong Z, et al. The impact of chemotherapy-associated neutrophil/ lymphocyte counts on prognosis of adjuvant chemotherapy in colorectal cancer. BMC Cancer. 2013;13:177.
Borg C, Ray-Coquard I, Philip I, Clapisson G, Bendriss-Vermare N, Menetrier-Caux C, et al. CD4 lymphopenia as a risk factor for febrile neutropenia and early death after cytotoxic chemotherapy in adult patients with cancer. Cancer. 2004;101(11):2675–80.
Acknowledgements
None
Funding
The study was conducted with grants from the Chinese Natural Science Foundation (grant nos. 81873215 and 82003006).
Author information
Authors and Affiliations
Contributions
BY was responsible for the conception of the work. QY and BY obtained the data. BY analyzed the data. XH, YH, ZZ, and LL wrote the manuscript. ZZ, JG, and BY critically revised the manuscript. All authors are accountable for the contents of this work. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was performed in line with the principles stated in the Declaration of Helsinki and was approved by the ethics committee of Hainan Hospital of Chinese PLA General Hospital (ID: 301HLFYLS15). Written informed consent was obtained from the patients or their authorized relatives.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, X., Huan, Y., Liu, L. et al. Preoperative low absolute lymphocyte count to fibrinogen ratio correlated with poor survival in nonmetastatic colorectal cancer. World J Surg Onc 20, 309 (2022). https://doi.org/10.1186/s12957-022-02775-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02775-z