Abstract
Background
There has always been a debate on the optimal timing of endoscopy in patients with acute variceal bleeding (AVB).
Objective
This study aimed to examine the relation between the timing of endoscopy and the short-term outcomes of patients with AVB.
Methods
Patients with AVB who underwent endoscopy within 24 h after admission at our tertiary care center from 2014 to 2022 were evaluated retrospectively. The primary outcomes were the 6-week mortality and re-bleeding. The secondary outcomes included the total number of blood units transfused, the length of hospital stay, and the need for salvage therapy. We used Cox proportional hazards model to analyze the predictors of 6-week mortality in all patients as well as in those who were at high risk of further bleeding or death.
Results
A total of 312 patients were enrolled. Among them, 170 patients (54.49%) underwent urgent endoscopy (< 6 h), and 142 patients (45.51%) underwent early endoscopy (6–24 h). There were no significant differences between the urgent-endoscopy group and the early-endoscopy group, regarding the 6-week mortality (16.47% vs. 10.56%; P value = 0.132) and 6-week re-bleeding rate (11.2% vs. 16.2%; P value = 0.196). In multivariate analysis, time to endoscopy was independent of 6-week mortality (P value = 0.170), but the time between the beginning of bleeding and endoscopy (within 12 h) was significantly associated with low 6-week mortality (OR: 0.16; 95% CI: 0.06–0.46; P value = 0.001). Time to endoscopy was still not associated with 6-week mortality in patients at high risk for further bleeding or death (Glasgow-Blatchford score ≥ 12, n = 138, P value = 0.902).
Conclusions
Endoscopy performed within 6 h of admission, rather than within 6 to 24 h, did not improve six-week clinical outcomes in patients in stable condition with AVB and even those who were at high risk of further bleeding and death.
Similar content being viewed by others
Introduction
Acute variceal bleeding (AVB) is a common and life-threatening complication of cirrhosis. Although there have been significant improvements in diagnostic and therapeutic modalities for the management of AVB in the recent several decades [1] [2], the mortality rate remains as high as 12–22% [3,4,5]. The mainstay of the management of patients with AVB includes resuscitation, pharmacological treatment (eg., Schistosoma and prophylactic antibiotics [6]), endoscopic treatment, etc. [7] Endoscopic procedures and endoscopic hemostasis techniques including endoscopic variceal ligation (EVL), Endoscopic injection sclerotherapy (EIS) and tissue adhesive (e.g. N-butyl-cyanoacrylate) are considered essential in the treatment of AVB [8, 9] (Fig. 1).
Endoscopic hemostasis techniques in patients with acute variceal bleeding. A and B: Endoscopic injection sclerotherapy and tissue adhesive is applied in the treatment of acute gastric variceal hemorrhage. C and D: Endoscopic variceal ligation is used in the treatment of acute esophageal variceal hemorrhage
Current European consensus and American guidelines recommend emergency endoscopy to be performed within 12 h of admission [8,9,10], while Chinese guideline recommends emergency endoscopy to be performed 12–24 h after bleeding [9]. However, these recommendations are based on “expert opinion” and lack of solid evidence. There is a little related research to support these current recommendations. These researches were mostly retrospective and revealed contradictory results [11,12,13,14,15]. To date, a gold standard recommending the timing of endoscopy in patients with AVB has not been clearly determined.
This study aimed to explore the clinical outcomes in patients with AVB according to different timing to endoscopy. In addition, we aimed to investigate the clinical predictors of short-term mortalities, especially in patients at high risk for further bleeding or death.
Methods
Patients and study design
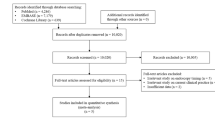
Medical records of esophagogastric varices bleeding patients undergoing endoscopy from our tertiary hospital were retrospectively reviewed between July 2014 and May 2022. The diagnosis of cirrhosis was established according to the previous history or on the combination of laboratory and imaging tests. The inclusion criteria were as follows: (1) Emergency patients admitted via the emergency room (ER) with upper gastrointestinal bleeding (UGIB); (2) Esophagogastric varices confirmed as the source of bleeding; (3) Endoscopy was performed within 24 h; (4) aged > 18 years. The exclusion criteria were as follows: (1) Severe dysfunction of a major organ (e.g., pulmonary disease, heart failure, and terminal malignancy except hepatocellular carcinoma); (2) UGIB from other than variceal bleeding (e.g., peptic ulcer bleeding); (3) Prior acute variceal bleeding (AVB) in the past three months; (4) Loss to follow-up within 6 weeks after AVB. This study protocol was approved by the Institutional Ethics Committee of Shanghai East Hospital and was performed in accordance with the Declaration of Helsinki.
Interventions and data collection
When a patient with suspected AVB arrived at the ER, adequate fluid resuscitation, a vasoactive drug with somatostatin, and a prophylactic antibiotic were administered immediately. Packed red blood cell (PRBC) was given in the case of persisting bleeding or hemoglobin < 7 g/dl.
The endoscopy procedures were performed by five senior endoscopists with more than 3 years experience in the field of endoscopy. The timing of endoscopy depended on hemodynamic status, the discretion of the endoscopists on duty, and the patient’s will.
Endoscopic therapy was performed under the circumstances as follows: (a) Active bleeding of the varices; (b) Presence of adherent blood clot or the “white nipple” sign; (c) Presence of blood in the upper gastrointestinal tract and the varices as the only potential bleeding source; (d) In the case of the presence of varices without blood in the upper gastrointestinal tract, the endoscopist decided whether to perform the therapeutic endoscopy. The varices were treated by endoscopic band ligation (EBL), injection of a tissue adhesive (e.g., cyanoacrylate), sclerotherapy, or with the combination of hemoclips according to the discretion of the endoscopist.
Two independent investigators screened the medical records, including demographic, endoscopic reports, laboratory results, and clinical data. Model for End-stage Liver Disease (MELD) score [16], the Glasgow-Blatchford score (GBS) [17], Child-Turcotte-Pugh score (CTP) [18] were calculated.
Follow-up and outcome assessment
The timing of endoscopy was defined as the interval between the hospital arrival and the initial endoscopic procedure, while the bleeding time was regarded as the duration between the beginning of the presence of bleeding and the initial endoscopic procedure. Endoscopy performed within 6 h of admission was defined as urgent endoscopy, and endoscopy performed within 6–24 h of admission was considered as early endoscopy.
The primary outcomes of this study were the 6-week mortality and re-bleeding rates. The secondary outcomes were the total number of blood units transfused, the length of hospital stay, and the need for salvage therapy (e.g., additional endoscopic therapy, balloon tamponade, transjugular intrahepatic portosystemic shunt [TIPS]).
Statistical analysis
Means with standard deviations and frequencies with percentages were used for descriptive statistics. Statistical differences between the groups were investigated by the chi-square test and Fisher’s exact test for categorical variables and the Student’s t-test for continuous variables. Cumulative 6-week survival rates were estimated by Kaplan–Meier method and compared by log-rank test. Predictors of 6-week mortality were assessed by Cox’s proportional hazards model. A P value less than 0.05 was considered significant. Hazard ratios (HRs) and 95% confidence intervals (CIs) were also calculated. All statistical analyses were performed by SPSS version 20.0 (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics
Overall, 352 AVB patients meeting the inclusion criteria from our tertiary center were admitted. Among them, according to the exclusion criteria, 40 patients were excluded. Finally, the remaining 312 patients were enrolled. Among them, 170 patients (54.49%) underwent urgent endoscopy, and 142 patients (45.51%) underwent early endoscopy.
As shown in Table 1, 195 (62.5%) patients were male, and the mean age was 62.98 ± 12.20. 142 (45.5%) patients had previous upper GI bleeding history. 61 (19.6%) patients had hepatocellular carcinoma (HCC). The most common etiology was chronic hepatitis B virus (HBV) infection, followed by AIH (autoimmune hepatitis) and alcohol use. The average time to endoscopy was 9.14 ± 8.70 h. The average Glasgow-Blatchford score, MELD score, and CTP were 11.22 ± 3.07, 14.21 ± 4.99, and 8.05 ± 1.69, respectively. 234 patients (75.0%) took beta blockers as prophylactic therapy for AVB before the bleeding episode. 138 patients (44.23%) were on anti-HBV specific treatment. 6 patients (1.92%) had portal vein tumor thrombus.
The baseline patient characteristics, including age (P value = 0.051), gender (P value = 0.089), Glasgow-Blatchford score (P value = 0.91), CTP score (P value = 0.11), MELD scores (P value = 0.502), etc., did not differ significantly between the two groups. The median time to endoscopy was significantly different between the two groups (2.57 ± 1.40 vs. 17.03 ± 7.07; P < 0.001).
Primary and secondary outcomes according to endoscopy timing
The overall 6-week mortality rate was 13.8% (n = 43). Concerning the 6-week mortality, there were no significant differences between the urgent-endoscopy group and the early-endoscopy group (16.5% vs. 10.6%; P value = 0.117; Fig. 2). The overall 6-week re-bleeding rate was 13.5% (n = 42). There were no significant differences in the 6-week re-bleeding rate between the urgent-endoscopy group and the early-endoscopy group (11.2% vs. 16.2%; P value = 0.196). The overall 5-day re-bleeding rate was 4.49% (n = 14). The number of transfusions per patient (2.13 ± 3.17 vs. 1.4 ± 1.83; P value = 0.004) was significantly higher in the early-endoscopy group than in the urgent-endoscopy group. The length of hospital stay (15.1 ± 8.09 vs. 16.40 ± 7.88; P value = 0.153) and the rate of need for salvage therapy (5.9% vs. 3.5%; P value = 0.332) were not significantly different between the urgent-endoscopy group and the early-endoscopy group. (Table 2).
Predictive factors of 6-week mortality
By multivariate analysis, clinical predictors associated with 6-week mortality were explored, as shown in Table 3. Compared with early-endoscopy, urgent-endoscopy was not independently associated with short-term mortality (P = 0.345). However, the bleeding time shorter than 12 h (vs. more than 12 h) was independently associated with low short-term mortality (OR: 0.16; 95% CI: 0.06–0.46; P value = 0.001). The other independent risk factors of 6-week mortality were as follows: the presence of HCC (OR: 4.12; 95% CI: 1.94–8.71; P value < 0.001), the presence of encephalopathy (OR: 10.77; 95% CI: 4.35–26.62 P value < 0.001), high Glasgow-Blatchford score (OR: 1.14; 95% CI: 1.01–1.30; P value = 0.036) and high MELD score (OR: 1.15; 95% CI: 1.05–1.25; P value = 0.002).
In patients stratified by Glasgow-Blatchford score of 12 or higher (n = 138), multivariate analysis revealed HCC (OR: 2.56; 95% CI: 1.09–6.03; P value = 0.032) and encephalopathy (OR: 5.93; 95% CI: 2.22–15.89; P value < 0.001) as significant predictors of 6-week mortality. However, time to endoscopy was not associated with 6-week mortality (P value = 0.902). (Table 4).
Discussion
The current study revealed that urgent endoscopy (< 6 h) is not significantly superior to early endoscopy (6–24 h) regarding the 6-week mortality or the 6-week re-bleeding rate. This phenomenon could be explained by the fact that basic resuscitation and medical treatments have a major influence on the patient’s outcome in the early stages of treatment [8, 10, 19]. Evidentially, if a patient undergoes an endoscopic procedure, basic resuscitation may be interfered during the critical early period of management, leading to a bad prognosis. Moreover, if endoscopy is performed too early, the quality of endoscopic examination may be suboptimal due to poor preparation. It may be marred by food residues and remnant blood clots. Thus, the procedure may be prolonged, and the risk of a procedure-related complication tends to increase [20, 21].
To explore the potential benefits of urgent endoscopy, we selected high-risk patients to perform the subgroup analysis. We applied the Glasgow–Blatchford score as a measure of risk, which has been shown to correlate with mortality [22]. An observational study revealed that a delay of endoscopy in high-risk non-variceal upper gastrointestinal bleeding (NVUGIB) patients with a Glasgow–Blatchford score of 12 or higher was correlated to a significant increase in mortality [23]. However, our study showed that urgent endoscopy remained unrelated to 6-week mortality in high-risk patients (Glasgow-Blatchford score ≥ 12).
To the best of our knowledge, five retrospective studies have investigated the optimal timing of endoscopic treatment in AVB patients. Two studies published in Taiwan in 2009 [11] and 2012 [13] showed that delayed endoscopy increased short-term re-bleeding and mortality. However, the technology and instruments in the field of endoscopy have been greatly developed in recent decades. The conclusion of these studies may not be representative of that of nowadays. Conversely, the Korean research published in 2019 [15] indicated that urgent endoscopy was significantly related to a poorer outcome in patients with AVB. Both the Canadian study published in 2009 [12] and the Korean study published in 2018 [14] revealed that the timing of endoscopy is independent of short-term mortality. A meta-analysis including the above five retrospective studies demonstrated that the time to endoscopy does not affect the mortality or re-bleeding rate of patients with AVB. However, there was significant heterogeneity in the process of analyses [24]. Our study also indicated that urgent endoscopy is not associated with short-term outcomes.
Most of the previous studies defined “urgent endoscopy” as within 12 h of admission. This study is one of the very few studies to compare the short-term outcomes in patients with AVB between urgent endoscopy (< 6 h) and early endoscopy (6–24 h) with a big sample size. Actually, it is difficult in many countries to perform urgent endoscopy within 6 h of admission. In the randomized controlled trial aiming to explore the timing of endoscopy for acute upper gastrointestinal bleeding, patients assigned to undergo endoscopy within 6 h were regarded as urgent-endoscopy group. However, in this urgent-endoscopy group, the time from presentation to gastroenterologic consultation was 7.4 ± 6.2 h; the time from gastroenterologic consultation to endoscopy was 2.5 ± 1.7 h; time from presentation to endoscopy was 9.9 ± 6.1 h [25]. In the present study, this limitation was overcome. Commonly, gastroenterologic consultation in our center was conducted within 1–2 h.
It is essential to select appropriate outcomes in studies of endoscopy. Since the long-term prognosis of patients with AVB is mainly associated with their basal liver function, it is inappropriate to demonstrate the precise effect of a single-point endoscopy by a long-term prognosis. Therefore, the endpoints were set to be the composite outcomes at 6 weeks in this study [8].
This is the first study to report the bleeding time (the duration between the start of bleeding and endoscopy), which might be more precise and valuable than the timing to endoscopy (the duration between the hospital arrival and endoscopy). Furthermore, we found that the bleeding time within 12 h was independently related to low 6-week mortality, while the timing to endoscopy was not associated with 6-week mortality. The inconsistency might be explained that basic resuscitation and medical treatments immediately after bleeding, other than timing to endoscopy, played an important role in short-term outcomes of patients with AVB. Endoscopy is a relatively invasive treatment, compared with other medical treatments. If unnecessary urgent endoscopies are frequently performed, medical staff fatigue and medical costs may increase dramatically [20]. Further researches are needed to explore the relationship between the bleeding time and short-term mortality of patients with AVB. This is also the first study to investigate the optimal timing to endoscopy in patients with AVB in the mainland of China. The main etiology of cirrhosis was HBV in our study, which was different from the baseline characteristics of the western countries, causing that the result of this study should be interpreted discreetly worldwide.
Despite these originalities, this study has some limitations. First, some bias may exist due to the retrospective nature of this study. Conducting patient randomization could address this limitation, but it would be problematic in these acutely ill patients because of their unstable vital signs and obvious ethical concerns. Second, the MELD score was recorded soon after the admission, but it might have changed after resuscitation and pharmacological treatment. Re-calculate the MELD score before the endoscopy might be more appropriate in predicting the risks. Third, those who had persistent hypotensive shock despite initial resuscitation were not included. Therefore, our trial findings should not be generalizable to AVB patients with persistent hypotensive shock. Forth, the Fibroscan value is not available in the present study, which might be useful in the multivariate analysis.
In conclusion, we found that the time to endoscopy does not appear to be associated with short-term mortality in patients with AVB and those who were at high risk for further bleeding or death. However, the bleeding time more than 12 h is an independent risk factor of high short-term mortality in patients with AVB. Our results should be taken into consideration when making clinical decisions. A multi-center prospective study with a bigger sample size from different countries is in demand to explore the optimal timing for endoscopy.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
McCormick PA, O’Keefe C. Improving prognosis following a first variceal haemorrhage over four decades. Gut. 2001;49(5):682–5.
Carbonell N, Pauwels A, Serfaty L, Fourdan O, Lévy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40(3):652–9.
Seo YS, Park SY, Kim MY, Kim JH, Park JY, Yim HJ, Jang BK, Kim HS, Hahn T, Kim BI, et al. Lack of difference among terlipressin, somatostatin, and octreotide in the control of acute gastroesophageal variceal hemorrhage. Hepatology. 2014;60(3):954–63.
Villanueva C, Piqueras M, Aracil C, Gómez C, López-Balaguer JM, Gonzalez B, Gallego A, Torras X, Soriano G, Sáinz S, et al. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol. 2006;45(4):560–7.
Reverter E, Tandon P, Augustin S, Turon F, Casu S, Bastiampillai R, Keough A, Llop E, González A, Seijo S, et al. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding. Gastroenterology. 2014;146(2):412-419.e413.
Chavez-Tapia NC, Barrientos-Gutierrez T, Tellez-Avila F, Soares-Weiser K, Mendez-Sanchez N, Gluud C, Uribe M. Meta-analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding–an updated Cochrane review. Aliment Pharmacol Ther. 2011;34(5):509–18.
Seo YS. Prevention and management of gastroesophageal varices. Clin Mol Hepatol. 2018;24(1):20–42.
de Franchis R. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–52.
Chinese Society of Hepatology CMACSoG, Chinese Medical Association; Chinese Society of Endoscopy, Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension (2015) Clinical journal of gastrointestinal endoscopy (Chinese). 2015; 2(004):1–21.
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65(1):310–35.
Cheung J, Soo I, Bastiampillai R, Zhu Q, Ma M. Urgent vs. non-urgent endoscopy in stable acute variceal bleeding. Am J Gastroenterol. 2009;104(5):1125–9.
Hsu YC, Chung CS, Tseng CH, Lin TL, Liou JM, Wu MS, Hu FC, Wang HP. Delayed endoscopy as a risk factor for in-hospital mortality in cirrhotic patients with acute variceal hemorrhage. J Gastroenterol Hepatol. 2009;24(7):1294–9.
Chen PH, Chen WC, Hou MC, Liu TT, Chang CJ, Liao WC, Su CW, Wang HM, Lin HC, Lee FY, et al. Delayed endoscopy increases re-bleeding and mortality in patients with hematemesis and active esophageal variceal bleeding: a cohort study. J Hepatol. 2012;57(6):1207–13.
Yoo JJ, Chang Y, Cho EJ, Moon JE, Kim SG, Kim YS, Lee YB, Lee JH, Yu SJ, Kim YJ, et al. Timing of upper gastrointestinal endoscopy does not influence short-term outcomes in patients with acute variceal bleeding. World J Gastroenterol. 2018;24(44):5025–33.
Huh CW, Kim JS, Jung DH, Yang JD, Nam SW, Kwon JH, Kim BW. Optimal endoscopy timing according to the severity of underlying liver disease in patients with acute variceal bleeding. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2019;51(7):993–8.
D’Amico G, Maruzzelli L, Airoldi A, Petridis I, Tosetti G, Rampoldi A, D’Amico M, Miraglia R, De Nicola S, La Mura V, et al. Performance of the model for end-stage liver disease score for mortality prediction and the potential role of etiology. J Hepatol. 2021;75(6):1355–66.
Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000;356(9238):1318–21.
Abad-Lacruz A, Cabré E, González-Huix F, Fernández-Bañares F, Esteve M, Planas R, Llovet JM, Quer JC, Gassull MA. Routine tests of renal function, alcoholism, and nutrition improve the prognostic accuracy of Child-Pugh score in nonbleeding advanced cirrhotics. Am J Gastroenterol. 1993;88(3):382–7.
Bernard B, Grangé JD, Khac EN, Amiot X, Opolon P, Poynard T. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with ascites: a meta-analysis. Digestion. 1998;59(Suppl 2):54–7.
Lee JG, Turnipseed S, Romano PS, Vigil H, Azari R, Melnikoff N, Hsu R, Kirk D, Sokolove P, Leung JW. Endoscopy-based triage significantly reduces hospitalization rates and costs of treating upper GI bleeding: a randomized controlled trial. Gastrointest Endosc. 1999;50(6):755–61.
Schacher GM, Lesbros-Pantoflickova D, Ortner MA, Wasserfallen JB, Blum AL, Dorta G. Is early endoscopy in the emergency room beneficial in patients with bleeding peptic ulcer? A “fortuitously controlled” study. Endoscopy. 2005;37(4):324–8.
Stanley AJ, Laine L, Dalton HR, Ngu JH, Schultz M, Abazi R, Zakko L, Thornton S, Wilkinson K, Khor CJ, et al. Comparison of risk scoring systems for patients presenting with upper gastrointestinal bleeding: international multicentre prospective study. BMJ Clin Res Ed. 2017;356:i6432.
Lim LG, Ho KY, Chan YH, Teoh PL, Khor CJ, Lim LL, Rajnakova A, Ong TZ, Yeoh KG. Urgent endoscopy is associated with lower mortality in high-risk but not low-risk nonvariceal upper gastrointestinal bleeding. Endoscopy. 2011;43(4):300–6.
Jung DH, Huh CW, Kim NJ, Kim BW. Optimal endoscopy timing in patients with acute variceal bleeding: a systematic review and meta-analysis. Sci Rep. 2020;10(1):4046.
Lau JYW, Yu Y, Tang RSY, Chan HCH, Yip HC, Chan SM, Luk SWY, Wong SH, Lau LHS, Lui RN, et al. Timing of endoscopy for acute upper gastrointestinal bleeding. N Engl J Med. 2020;382(14):1299–308.
Acknowledgements
We thank the medical staff at the Shanghai East Hospital for their essential support and assistance with data collection.
Funding
This work was supported by grants from The Medical Discipline Construction Project of Pudong Health Committee of Shanghai (PWYgf2021-2), the Shanghai Committee of Science and Technology (21JC1405200), and the municipal health commission of Pudong new area (PW2021B-11).
Author information
Authors and Affiliations
Contributions
XY analyzed the literature and wrote the manuscript. MX studied concept and design. ZL QX ZZ and JL collected the data. JL analyzed the data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study protocol was approved by the Institutional Ethics Committee of Shanghai East Hospital and was performed in accordance with the Declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations. We obtained written informed consent from all patients.
Consent for publication
Not Applicable.
Competing interests
The authors who have taken part in this study declared that they do not have anything to disclose regarding funding or conflicts of interest with respect to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, X., Leng, Z., Xu, Q. et al. The influences of timing of urgent endoscopy in patients with acute variceal bleeding: a cohort study. BMC Gastroenterol 22, 506 (2022). https://doi.org/10.1186/s12876-022-02595-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02595-1