Abstract
Background
Patient reported experiences (PREMs) are important indices of quality of care. Similarities in demography between patient and doctor, known as social concordance, can facilitate patient-doctor interaction and may be associated with more positive patient experiences. The aim of this research is to study associations between gender concordance, age concordance and PREMs (doctor-patient communication, involvement in decision making, comprehensiveness of care and satisfaction) and to investigate whether these associations are dependent on a countries’ Gender Equality Index (GEI).
Methods
Secondary analysis on a multinational survey (62.478 patients, 7.438 GPs from 34 mostly European countries) containing information on general practices and the patient experiences regarding their consultation. Multi-level analysis is used to calculate associations of both gender and age concordance with four PREMs.
Results
The female/female dyad was associated with better experienced doctor-patient communication and patient involvement in decision making but not with patient satisfaction and experienced comprehensiveness of care. The male/male dyad was not associated with more positive patient experiences. Age concordance was associated with more involvement in decision making, more experienced comprehensiveness, less satisfaction but not with communication. No association was found between a country’s level of GEI and the effect of gender concordance.
Conclusion
Consultations in which both patient and GP are female are associated with higher ratings of communication and involvement in decision making, irrespective of the GEI of the countries concerned. Age concordance was associated with all PREMs except communication. Although effect sizes are small, social concordance could create a suggestion of shared identity, diminish professional uncertainty and changes communication patterns, thereby enhancing health care outcomes.
Similar content being viewed by others
Introduction
Patient reported experience measures (PREMs) are health care quality indices derived from the perspective of patients. Although patient experiences are distinct from more classic measures for clinical effectiveness (e.g. decrease in blood pressure) and patient safety, these measures are interrelated [1, 2]. Therefore, understanding what improves or undermines patient experiences can help achieve treatment goals and improve quality of care.
Social concordance is a concept of similarity based on demographic characteristics. Most research in this field has focused on the influence of ethnic concordance, gender concordance or language concordance on health care consultation outcomes. Studies focusing on gender concordance are inconclusive whether PREMs are affected by the doctor-patient gender composition. For example, female gender concordance can be associated with better communication [3], higher health care provider score [4], more harmonious connection [5] and more agreement on advice [6]. Gender concordance is also associated with patients experiencing more overall satisfaction [7], although this finding is refuted in a large comprehensive American study [8]. This study, containing over 100.000 patient experience survey’s, showed no association between gender concordance and Press Ganey scores (reflecting the likelihood of recommending the physician to others). Also, other studies find that gender concordance is not related to experienced participatory decision-making, encounter quality, trust, quality of life or quality of care [9,10,11,12,13]. Research on age concordance is scarce, but existing evidence suggests associations with enhanced health care quality perceptions [7]. In conclusion, whether doctor-patient concordance regarding gender and age can influence PREMs is still under debate.
In this study, we will investigate the influence of both gender concordance and age concordance on doctor-patient communication, patient involvement in decision making, experienced comprehensiveness of care and patient satisfaction in primary care. It is hypothesized that gender and age concordance are associated with higher scores on PREMs.
The extent to which gender and age concordance affect PREMs could also be culturally determined. In particular gender, which is a social construct, can have different interpretations among different countries [14]. Countries differ in gender norms (e.g. masculinity norms or ideas how man and women should relate to each other) [15], possibly influencing how gender concordance affects patient-doctor interaction. Therefore, we will investigate whether associations between gender concordance and PREMs vary between countries with a different degree of gender equality. It is hypothesized that in countries with a lower gender equality index (GEI), gender stereotypes are stronger resulting into a higher likelihood of gender concordance/discordance influencing PREMs. This aligns with the convergence hypothesis, which states that health inequalities between man and women decrease as gender equality increases [16, 17].
Methods
Data source
For this study, the ‘Quality and Costs of Primary Care in Europe’ database (QUALICOPC) is used, provided by the Netherlands Institute for Health Services Research (Nivel). The QUALICOPC is a multinational survey held among GPs and their patients, aimed at gathering extensive information on the participating general practices, the professional behavior of GPs and the experiences of their patients [18, 19]. Recently, this database has also been used by other researchers studying the association of migration concordance with PREMs [20].
Data collection procedure
Between 2011 and 2013, data was collected across 31 European countries, Australia, Canada and New Zealand. The primary objective was to establish a nationally representative sample of GPs in each participating country, with a predefined target sample size of 220 GPs per country (Cyprus, Iceland, Luxembourg and Malta had a target of 80 GPs). In most countries (19/34), this was achieved by drawing a random list sample from the national register of GPs. To prevent clustering, only one GP per practice was included. In countries where a national register was not available (5/34), a multistage sampling procedure was used. This involved combining registers from different regions within the country and subsequently selecting GPs through a random process. Notably, in larger countries with discernible variations in healthcare systems across regions (4/34), GPs were exclusively sampled from nationally representative regions. Conversely, in smaller countries (3/34), the entire GP population was approached for participation. In Italy and Norway, GPs were included by opportunity sampling. The overall mean response rate was 38%. Importantly, the participating GPs demonstrated representativeness concerning age and gender in comparison to the broader GP population within their respective countries [21].
In each participating practice, one GP and nine adult patients filled in a questionnaire. Patients who just had a face to face consultation with their GP were consecutively invited by trained fieldworkers to fill in a questionnaire about their experiences resulting from the consultation. This was continued until nine questionnaires per practice were collected. Participation was voluntary and informed consent was obtained. The average response rate of patients was 74%. In total, 63.887 patients completed a questionnaire and 7.438 GPs completed a questionnaire. 62.478 (97.8%) of the patient experience questionnaires were successfully matched with the GP questionnaires. All included respondents were 18 years or older and all information was made anonymous. More details about the study protocol, the questionnaire background and survey design have been published elsewhere [21,22,23].
Variables
Of the questionnaire directed to the GPs, only the information concerning gender, age and practice location (city/suburbs/town/urban–rural/rural) was used. The questionnaire directed to the patients consisted of statements which could be answered yes/no and were designed to measure, amongst others, the latent variables ‘doctor-patient communication’ (5 items) and ‘comprehensiveness of care’ (2 items). Moreover, 2 items were selected which were interpreted as measuring ‘patient satisfaction’. The variable ‘patient involvement in decision making’ was measured with one item (dichotomous). For the multiple item latent variables, scales were constructed using multilevel latent variable analyses in a four-level model (items nested within patients, nested within GPs, nested within countries). The reliability of these scales are reported in Appendix A. Gender concordance was considered a four category variable, containing these dyads: male/male, male/female, female/male and female/female (gender GP/gender patient). Age concordance was defined as a maximum age difference of five years between patient and GP, which is similar to how this construct was defined in other studies [7, 24]. Age discordance was divided into two groups: patients being substantially younger than their GP (‘younger patient/older GP’ dyad) and more involvement in decision making and patients being substantially older than their GP (‘older patient/younger GP’ dyad).
Countries were given a score on the gender equality index (GEI) using the indexation of 2015 published by the European Institute of Gender Equality [25], based on datapoints originating from 2012. No GEI scores were available for Iceland, Norway, Switzerland, Turkey, Australia, Canada, New Zealand and FYR Macedonia. Scores ranged from 50.10 (Greece) to 79.70 (Sweden), with higher scores corresponding with more gender equality. Countries were categorized into ‘low GEI’ (index < 55), ‘average GEI’ (index 55–65) and ‘high GEI’ (index > 65). Table 1 shows all countries and their corresponding GEI.
Statistics
Due to clustering of observations at the level of countries and GPs, we performed multi-level analysis [26], using three different data levels: patients (1) nested within GPs (2) nested withing countries (3). We predicted doctor-patient communication, patient satisfaction and comprehensiveness of care using linear regressions and patient involvement in decision making using logistic regressions (with a fixed intercept and random effects at the country and GP level). Main predictors in our models are ‘gender concordance’ and ‘age concordance’ and the control variables are ‘GP age’, ‘patient age’, ‘chronic condition’ (yes/no), ‘origin of patient’ (native/not native), ‘education’ (primary/secondary/post-secondary), ‘self-reported level of household income’ (low/average/high) and ‘location of practice’ (big city/town/mixed rural/rural). Comparisons between low, middle and high GEI countries were made by adding interaction terms (gender concordance * GEI-categories) to the model. All analyses were performed using STATA 17.0.
Results
Descriptive statistics
About half of the questionnaires were filled in after the patient visited a male GP (47,8%) and most of the included patients were female (61.2%). Half of the consultations were gender concordant (54.3%) and 20.2% were age concordant. All gender dyad characteristics and age dyad characteristics are reported in Table 2. Notably, the age of the patient varies greatly between the three age dyads. Prevalence of one or more chronic conditions is also higher in the dyad with older patients and the dyad with younger patients contained more higher educated individuals.
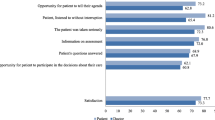
Scores for communication, satisfaction, involvement and comprehensiveness were negatively skewed (towards high scores). Figure 1 shows that especially in consultations with a female GP, there are notable differences in PREM-scores between concordant and discordant gender dyads. In consultations with a male GP, scores given by male and female patients are more or less equal. Figure 2 shows that patients aged younger than their GP report the lowest scores on communication, satisfaction, involvement and comprehensiveness, whereas patients aged older than their GP report better communication and higher satisfaction.
Main results
Female concordance is associated with higher scores on communication (p ≤ 0.01) and more involvement in decision making (p ≤ 0.01) compared to the other dyads (Table 3). The female/female dyad is associated with higher patient satisfaction compared to the male/female dyad (p = 0.01) and the male/male dyad (p = 0.02), but not compared to the female/male dyad. Findings are similar for comprehensiveness of care: the female/female dyad is associated with higher scores compared to both dyads with a male GP (p = 0.00), but not compared to the female/male dyad. Patient satisfaction and comprehensiveness of care are thus associated with the gender of the GP (higher scores when the GP is female) and not with gender concordance.
Age concordance was not associated with experienced communication. Consultations with an older patient/younger GP dyad were associated with higher satisfaction (p = 0.01) and less experienced comprehensiveness (p = 0.02) compared to consultations with age concordance. Consultations with a younger patient/older GP dyad were associated with lower involvement scores compared to consultations with age concordance (OR 0.92, p = 0.02).
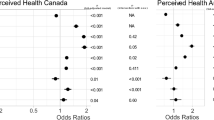
In contrast to the former model (Table 3), there are no associations between gender concordance and all four PREMs in both low and high GEI countries (Table 4). In both low and high GEI countries, consultations with a female GP were associated with higher scores for communication and satisfaction. Male concordance was associated with lower involvement in decision making compared to female concordance in low GEI countries whereas in high GEI countries, both dyads with a female GP were associated with higher involvement in decision. There are no associations between gender dyads and comprehensiveness of care in low GEI countries, however consultations with a female GP were associated with better experienced comprehensiveness compared to consultations with a male GP in high GEI countries. Our findings do not support the hypothesis that associations between gender concordance and PREMs are stronger in countries with a low GEI.
Model properties
The extent to which the combination of independent variables used in the model (Table 3) explain the variance of communication, satisfaction and involvement in decision making on the country and GP level is limited (ranging from 0.3% to 4.4%). The model explains 15.7% of the variance in comprehensiveness of care on the country level. After adding the GEI variable to the model (and excluding the countries of which a GEI was not available), the variance of the communication, satisfaction and involvement in decision making was explained to a bigger extend (Table 4). This was especially true on the country level (reduction of variance ranging from 7.0% to 27.1%).
Discussion
Summary
Female concordance is associated with better communication and more involvement in decision making. The age concordant dyad is associated with more experienced comprehensiveness and less satisfaction (compared to the older patient/younger GP dyad) and with more involvement in decision making (compared to the younger patient/older GP dyad). Communication was not associated with age concordance. The hypothesis that countries with a lower GEI would demonstrate stronger associations between gender concordance and PREMs could not be supported.
Strengths and limitations
The combination of a large number of respondents gathered across a large number of countries and the ability to take into account the nested nature of our respondents, strengthens the reliability of our results. The response rates among GPs and patients, at 38% and 74% respectively, introduce a risk of selection bias. Although the participating GPs generally reflected the age and gender distribution of the broader GP population in their respective countries, the representativeness regarding other characteristics, such as ethnicity, remains uncertain. Additionally, it is possible that participating GPs have greater interest in research or have more time availability compared to their non-participating counterparts, potentially influencing our study outcomes. Varying GP response rates (e.g., less than 10% in Sweden, over 70% in Spain) impact result generalizability in those particular countries. Notably, one in four patients opted not to participate, with the reasons for non-participation uncollected. Possible explanations for patient non-participation may include time constraints and privacy concerns. The latter, in particular, raises the possibility that GP visits for specific sensitive issues (e.g., psychological or sexual problems) may be underrepresented in our study sample. However, the precise impact of this possible underrepresentation on the measured patient experiences is challenging to ascertain.
The surveys contained patient experiences reported directly after consultation, which strengthens their validity. Moreover, the questions used to operationalize patient experiences were derived from various validated sources. However, all of them consisted out of yes/no answers which is less nuanced than for example Likert-scales. The distribution of scores were negatively skewed meaning most respondents reported very high scores, which is a common finding in post-consultation evaluation studies [8]. Most PREMs were measured by integrating multiple items into a scale, creating latent constructs. Although this method helps to provide more valid variables, this also makes the interpretation of scores somewhat abstract.
We used the gender equality indexation of the European Institute of Gender Equality, which is among the most comprehensive indexations available. However, this report did not contain indexations for 8 out of the 34 countries included in this study. These countries were therefore excluded in our model, lowering the statistical power.
Comparison with existing literature
Research on gender concordance and patient experiences show mixed results. It should however be taken into account that there are a lot of derivates of patient experiences, making it challenging to compare these study results. Some studies find associations between female concordance and specific PREMs [3,4,5,6,7], such as physician communication or experienced agreement on advice. Other studies find no significant association between gender concordance and PREMs [8,9,10,11,12,13]. Some of these findings can be explained by lack of statistical power [9] or the use of too broad outcome variables [10]. Nonetheless, the study of Takeshita et al. [8] was large and comprehensive and showed no association between gender concordance and one specific PREM: the likelihood of recommending the physician to a friend (on a 1 to 5 scale). Although this appears to contrast our findings, it should be noted that our studied PREMs are dissimilar. Moreover, as in most studies finding significant associations, especially the female-female dyad appears to be linked with higher scores on PREMs. This distinction was not specifically reported in the study of Takeshita et al.
Associations between age concordance and PREMs are poorly studied. In an observational study, age concordance was part of the construct social concordance (also entailing race, gender and education concordance). Social concordance was associated with higher satisfaction of care, but it is not clear to what extent age concordance contributed to this finding [7]. Our finding that age concordance can be associated with patient experiences is consistent with the idea that proximity in demographics may positively influence patient experiences.
This is the first study which takes the cross-national variability of gender equality into account when focusing on gender concordance. We hypothesized that more gender equality would diminish effects of gender concordance. However, we did not find a pattern to substantiate this. Possibly, the impact of specific gender dyads on consultations outcomes mainly arises from interpersonal factors and are to a lesser extent related to sociocultural norms.
How social concordance between patient and GP influences health care consultations is not clear. However, there are multiple conceivable explanations. First, sharing demographic characteristics can give the persons involved a suggestion of shared identity, ideas and beliefs [5, 12, 27], smoothening for example shared decision making. Secondly, social concordance is associated with a more patient-centered communication style applied by GPs [28,29,30], which is marked by GPs more actively attempting to understand the patient perspective and reaching shared understanding. Lastly, doctors treating patients who are more like themselves might experience less professional uncertainty because they can better relate to the patient’s problems [5]. These processes could occur simultaneously.
We suggest that future research should focus on more qualitative views on what actually happens in the consultation room. For example, performing qualitative analysis on video recorded consultations could give more insight into consultations room dynamics within each gender dyad. Also, interviewing GPs or patients after a consultation could be an interesting opportunity to unravel how social concordance affects consultation room dynamics.
Conclusion
We conclude from our study results that age concordance and female/female gender concordance can positively affect PREMs regardless of the gender equality of the countries concerned, although differences were small. This contributes to the idea that the mere act of matching basic demographic characteristics, especially matching a female patient to a female GP, can have a beneficial impact on the experience of healthcare.
Availability of data and materials
The raw data used in this study is the property of the international QUALICOPC consortium, and is not available for publication by the authors. The data is available upon reasonable request and can be obtained from W. Schäfer (w.schafer@nivel.nl).
Abbreviations
- PREM:
-
Patient reported experience measure
- GEI:
-
Gender equality index
- GP:
-
General practitioner
- QUALICOPC:
-
Quality and costs of primary care
References
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570.
Price RA, Elliott MN, Zaslavsky AM, Hays RD, Lehrman WG, Rybowski L, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71(5):522–54.
Peimani M, Stewart AL, Garmaroudi G, Shakibazadeh E, Nasli-Esfahani E. The impact of gender patient-physician concordance on interpersonal processes of care and patients’ outcomes in the diabetes care setting. Patient Educ Couns. 2023;106:68–74.
Chekijian S, Kinsman J, Taylor RA, Ravi S, Parwani V, Ulrich A, et al. Association between patient-physician gender concordance and patient experience scores. Is there gender bias? Am J Emerg Med. 2021;45:476–82.
Gross R, McNeill R, Davis P, Lay-Yee R, Jatrana S, Crampton P. The association of gender concordance and primary care physicians’ perceptions of their patients. 2008;48(2):123–44. https://doi.org/10.1080/03630240802313464. [cited 2021 Sep 2].
Schieber AC, Delpierre C, Lepage B, Afrite A, Pascal J, Cases C, et al. Do gender differences affect the doctor-patient interaction during consultations in general practice? Results from the INTERMEDE study. Fam Pract. 2014;31(6):706–13.
Thornton RLJ, Powe NR, Roter D, Cooper LA. Patient-physician social concordance, medical visit communication and patients’ perceptions of health care quality. Patient Educ Couns. 2011;85(3):201–8.
Takeshita J, Wang S, Loren AW, Mitra N, Shults J, Shin DB, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw Open. 2020;3(11):e2024583.
Jackson JL, Kay C, Scholcoff C, Nickoloff S, Kuriyama A, Slykhouse L, et al. Associations between gender and racial patient-physician concordance and visit outcomes among hypertensive patients in primary care. J Gen Intern Med. 2022;37(6):1569–71.
Hassan AM, Ketheeswaran S, Adesoye T, Shah SA, Cox SE, Kapur SK, et al. Association between patient–surgeon race and gender concordance and patient-reported outcomes following breast cancer surgery. Breast Cancer Res Treat. 2023;198(1):167–75.
Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. J Am Med Assoc. 1999;282(6):583–859.
Street RL, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: Personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6(3):198–205.
Prasad T, Buta E, Cleary PD. Is patient–physician gender concordance related to the quality of patient care experiences? J Gen Intern Med. 2021;36(10):3058–63.
Manandhar M, Hawkes S, Buse K, Nosrati E, Magar V. Gender, health and the 2030 agenda for sustainable development. Bull World Health Organ. 2018;96(9):644–53.
Heise L, Greene ME, Opper N, Stavropoulou M, Harper C, Nascimento M, et al. Gender inequality and restrictive gender norms: framing the challenges to health. Lancet. 2019;393(10189):2440–54. [cited 2022 Jun 9]. Available from: http://www.thelancet.com/article/S014067361930652X/fulltext.
King TL, Kavanagh A, Scovelle AJ, Milner A. Associations between gender equality and health: a systematic review. Health Promot Int. 2020;35(1):27–41. [cited 2022 Jul 21]. Available from:https://pubmed.ncbi.nlm.nih.gov/31916577/.
Backhans MC, Lundberg M, Månsdotter A. Does increased gender equality lead to a convergence of health outcomes for men and women? A study of Swedish municipalities. Soc Sci Med. 2007;64(9):1892–903.
Schäfer WLA, Boerma WGW, Schellevis FG, Groenewegen PP. GP practices as a one-stop shop: how do patients perceive the quality of care? A cross-sectional study in thirty-four countries. Health Serv Res. 2018;53(4):2047–63.
Schäfer WLA, Boerma WGW, Murante AM, Sixma HJM, Schellevis FG, Groenewegen PP. Assessing the potential for improvement of primary care in 34 countries: a cross-sectional survey. Bull World Health Organ. 2015;93(3):161–8.
Groenewegen PP, Spreeuwenberg P, Siriwardena AN, Sirdifield C, Willems S. Migrant GPs and patients: a cross-sectional study of practice characteristics, patient experiences and migration concordance. Scand J Prim Health Care. 2022;40(2):181–9.
Groenewegen PP, Greß S, Schäfer W. General practitioners’ participation in a large, multicountry combined general practitioner-patient survey: recruitment procedures and participation rate. Int J Family Med. 2016;2016:4929432.
Schäfer WLA, Boerma WGW, Kringos DS, De Ryck E, Greß S, Heinemann S, et al. Measures of quality, costs and equity in primary health care instruments developed to analyse and compare primary care in 35 countries. Qual Prim Care. 2013;21(2):67–79.
LA Schäfer W, Boerma WG, Kringos DS, De Maeseneer J, Greß S, Heinemann S, et al. QUALICOPC, a multi-country study evaluating quality, costs and equity in primary care. BMC Fam Pract. 2011;12:115.
Eggermont D, Kunst AE, Hek K, Verheij RA. Gender and age concordance between patient and GP: an observational study on associations with referral behaviour. BJGP Open. 2022;6(4):BJGPO.2022.0091.
European Institute for Gender Equality. Gender Equality Index 2020. Key findings for the EU [Internet]. 2020. Available from: http://eige.europa.eu/gender-equality-index
Leyland AH, Groenewegen PP. Multilevel modelling for public health and health services research. 2020.
Krupat E, Bell RA, Kravitz RL, Thom D, Azari R. When physicians and patients think alike: Patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001;50(12):1057–62.
Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–15.
Bertakis KD, Azari R. Patient-centered care: The influence of patient and resident physician gender and gender concordance in primary care. J Womens Health. 2012;21(3):326–33.
Bradley G, Sparks B, Nesdale D. Doctor communication style and patient outcomes: Gender and age as moderators. J Appl Soc Psychol. 2001;31(8):1749–73.
Acknowledgements
The authors thank their partners in the QUALICOPC project; J De Maeseneer, J Detollenaere, L Hanssens, S Willems (Belgium); S Greß, S Heinemann (Germany); G Capitani, S De Rosis, AM Murante, S Nuti, C Seghieri, M Vainieri (Italy); D Kringos, T Van Loenen (the Netherlands); D Rotar Pavlič, I Švab (Slovenia). The authors thank the coordinators of the data collection in each country: L Jorm, I McRae (Australia); K Hoffmann, M Maier (Austria); P Salchev (Bulgaria); W Wodchis, W Hogg (Canada); G Samoutis (Cyprus); B Seifert, N Šrámková (Czech Republic); J Reinholdt Jensen, P Vedsted (Denmark); M Lember, K Põlluste (Estonia); E Kosunen (Finland); C Lionis (Greece); I Rurik (Hungary); J Heimisdóttir, O Thorgeirsson (Iceland); C Collins (Ireland); G Ticmane (Latvia); S Macinskas (Lithuania); M Aubart, J Leners, R Stein (Luxembourg); G Bezzina, P Sciortino (Malta); T Ashton, R McNeill (New Zealand); T Bjerve Eide, H Melbye (Norway); M Oleszczyk, A Windak (Poland); L Pisco (Portugal), D Farcasanu (Romania); E Jurgova (Slovakia); T Dedeu (Spain); C Björkelund, T Faresjö (Sweden); T Bisschoff, N Senn (Switzerland); K Stavric (The former Yugoslav Republic of Macedonia); M Akman (Turkey); C Sirdifield, N Siriwardena (United Kingdom).
The authors thank P Spreeuwenberg for his contributions related to the statistical analysis performed in this study.
Funding
This article is based on data from the QUALICOPC (Quality and Costs of Primary Care) project, co-funded by the European Commission under the Seventh Framework Programme [FP7/2007–2013] under grant agreement 242141 and was carried out by a consortium of six research institutes from Belgium, Germany, Italy, The Netherlands and Slovenia. This secondary analysis was not separately funded. The funding body played no role in the design of the study and collection, analysis, interpretation of data, and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
DE conceived the study with input from AEK, PG and RAV. DE retrieved the data from the QUALICOPC consortium and performed the data analysis with input from PG. DE drafted the manuscript. All authors read, provided critical review and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Netherlands Institute for Health Services Research (Nivel) and all methods were performed in accordance with the relevant guidelines and regulations. For the QUALICOPC (Quality and Costs of Primary Care) study, ethical approval was acquired in accordance with the legal requirements in each participating country. The surveys were carried out voluntarily (based on informed consent) and anonymously. As the use of the QUALICOPC data for this study is in line with the original goals of the data collection and no additional data was collected, the initial ethical approval is sufficient for this study.
Ethic approval was granted by:
Australia: The Australian National University (ANU) Human Research Ethics Committee, University of Western Sydney Human Research Ethics Committee, The Royal Australian College of General Practitioners (RACGP) National Research and Evaluation Ethics Committee,
Austria: Ethics committee of the Medical University of Vienna,
Belgium: University Hospital Ghent—Commission for Medical Ethics.
Bulgaria: The coordinator sent an official letter to the Ministry of Health which gave consent and support for the survey. The coordinator confirmed that there is no statutory requirement for ethical approval for this study.
Canada: Behavioural Research Ethics Board, Community Research Ethics Board of Alberta, University of Sakatchewan Behavioural Research Ethics Board, Health Research Ethics Board, Health Sciences Research Ethics Board, Health Sciences and Science Research Ethics Board, Comité institutionnel d'éthique de la recherche avec les êtres humains, Research Ethics Board, Health Sciences Research Ethics Board, Interdisciplinary Committee on Ethics in Human Research.
Cyprus: National Bioethical Committee of Cyprus.
Czech Republic: General University Hospital linked to the First Faculty of Medicine, Charles University in Prague.
Denmark: The coordinator confirmed that there is no statutory requirement for ethical approval for this study.
Estonia: The national coordinator consulted with the Ethics Review Committee on Human Research of the University of Tartu. It was confirmed that there is no statutory requirement for ethical approval for this study.
Finland: The ethical committee of Pirkanmaa Hospital District.
Germany: Ethics Commission of the "Landesärtzenkammer Hessen".
Greece: Bioethical committees of seventy hospitals.
Hungary: National Ethical Committee.
Iceland: The Icelandic Bioethics Committee. A national committee under the Ministry of Welfare.
Ireland: Irish College of General Practitioners Research Ethics Committee – National Committee.
Italy: At Local Health Authorities level. Approval was requested from LHA Ethical Committees.
Latvia: Latvian Physicians Association Board of Certification.
Lithuania: Kauno Regionus Biomedicininu Tyrimu Etikos Komitetas.
Luxembourg: National committee of Research Ethic (CNER) in Luxembourg.
FYR Macedonia: Medical Faculty Skopje, R.Macedonia.
Matla: University of Malta Research Ethics Committee.
Netherlands: The ethics committee of VU Medisch Centrum confirmed via an official letter that the research is outside the scope of the WMO (Medical Research Involving Human Subjects Act).
New Zealand: Northern regional committee (Northern Y) for the nationally coordinated Health and Disability Ethics Committees (HDEC).
Norway: The coordinator confirmed that there is no statutory requirement for ethical approval for this study.
Poland: Bioethics approval of Jagiellonian University.
Portugal: Ethical committee of Lisbon and Oporto regions; the National Commission for Health Data Safety.
Romania: Scientific Committee of CPSS.
Spain: Research Units of Primary Care of the Autonomous Community in the Basque Country. In all other Autonomous Communities, the study was approved at the Healthcare Area level.
Slovakia: The national coordinator consulted the Council of the Slovak Society of General Practice. It was confirmed that there is no statutory requirement for ethical approval for this study.
Slovenia: National medical ethics committee.
Sweden: Regional Research Ethics Committte.
Switzerland: Ethical Committee of the University of Lausanne.
Turkey: Ethical committee of Kartal Research and Education Hospital in Istanbul.
United Kingdom: University of Lincoln School of Health and Social Care Ethics Committee; National Research Ethics Service.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Eggermont, D., Kunst, A.E., Groenewegen, P.P. et al. Social concordance and patient reported experiences in countries with different gender equality: a multinational survey. BMC Prim. Care 25, 97 (2024). https://doi.org/10.1186/s12875-024-02339-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02339-y