Abstract
Background
The demand for home healthcare is increasing in Japan, and a 24-hour on-call system could be a burden for primary care physicians. Identifying high-risk patients who need frequent emergency house calls could help physicians prepare and allocate medical resources. The aim of the present study was to develop a risk score to predict the frequent emergency house calls in patients who receive regular home visits.
Methods
We conducted a retrospective cohort study with linked medical and long-term care claims data from two Japanese cities. Participants were ≥ 65 years of age and had newly started regular home visits between July 2014 and March 2018 in Tsukuba city and between July 2012 and March 2017 in Kashiwa city. We followed up with patients a year after they began the regular home visits or until the month following the end of the regular home visits if this was completed within 1 year. We calculated the average number of emergency house calls per month by dividing the total number of emergency house calls by the number of months that each person received regular home visits (1–13 months). The primary outcome was the “frequent” emergency house calls, defined as its use once per month or more, on average, during the observation period. We used the least absolute shrinkage and selection operator (LASSO) logistic regression with 10-fold cross-validation to build the model from 19 candidate variables. The predictive performance was assessed with the area under the curve (AUC).
Results
Among 4888 eligible patients, frequent emergency house calls were observed in 13.0% of participants (634/4888). The risk score included three variables with the following point assignments: home oxygen therapy (3 points); long-term care need level 4–5 (1 point); cancer (4 points). While the AUC of a model that included all candidate variables was 0.734, the AUC of the 3-risk score model was 0.707, suggesting good discrimination.
Conclusions
This easy-to-use risk score would be useful for assessing high-risk patients and would allow the burden on primary care physicians to be reduced through measures such as clustering high-risk patients in well-equipped medical facilities.
Similar content being viewed by others
Introduction
In recent years, the organization of primary healthcare after office hours has changed in many countries. There are new models for after-hours care, such as large-scale general practice cooperatives, primary care centers integrated into hospital emergency departments, or telephone triage and consultation services [1]. These changes are partly due to primary care physicians’ reluctance to commit to being on-call 24-hour a day and 7 days a week because of the workload burden, increasing patients’ demand for after-hours care, and regional shortages of primary care physicians [2, 3].
In Japan, where the population is aging the fastest in the world [4], the demand for home healthcare has also increased due to the aging population and the government-sponsored shift of care from the hospital to the community [5]. All citizens in Japan have medical care coverage under a universal health insurance system, which consists of occupational insurance for salaried workers (employees), National Health Insurance for self-employed and retirees under 75 years of age, and Late-stage medical care system for the all elderly aged 75 and over [6, 7]. Japan also started a mandatory long-term care insurance system in 2000, distinct from the national medical insurance system [8]. Under the statutory long-term care insurance system, older people who need living assistance can receive care services based on the seven levels of the certificate of need for long-term care: Support 1 (lowest disability) to 2 and Care 1 to 5 (highest disability) [9]. Long-term care need level is a nationally standardized certification that is assessed based on a person’s physical and cognitive functioning [10]. All Japanese citizens who are ≥65 and individuals 40–64 years whose need of care is derived from aging-related diseases, such as stroke, cancer, and rheumatoid arthritis, are eligible for these benefits.
Home healthcare in Japan entails physicians making regular home visits to diagnose and monitor medical conditions, as well as prescribe medications. To be enrolled in physician-led home healthcare, patients apply by themselves or the primary care physician identifies patients who require home healthcare, under the condition that the patients cannot get to an outpatient clinic. In addition, they must reside within roughly 16 km of the hospital or clinic that provides these services. Physicians are required to provide regular home visits once or twice per month depending on the patients’ medical needs. Additionally, patients who receive physicians’ home visits often use the nursing care visits and home help services offered by a variety of care facilities [11].
To promote home healthcare, especially for emergency house calls and end-of-life care, the Ministry of Health, Labour, and Welfare introduced home care support clinics and hospitals (HCSCs) in 2006, with home care support functions available 24-hour a day until the patient dies [12]. HCSCs have a system that enables 24-hour emergency house call at the patient’s request. However, previous research has shown that more than 70% of physicians in HCSCs feel burdened by the 24-hour on-call coverage mandated for HCSCs [13]. To enhance home healthcare, it is essential to identify a high-risk population with frequent emergency house calls, and take measures to reduce physical and psychological burdens for primary care physicians.
Studies have shown that the common reasons for emergency house calls are fever, end-of-life care, dyspnea, and cough among patients who receive regular home visits in Japan [14, 15]. However, these studies focused on the chief complaint and did not consider factors of the patient’s condition such as comorbidities or medical procedures performed in the home care setting. In addition, they were single- or few-center studies, which limits their generalizability. To take measures to relieve the burden on primary care physicians, it is necessary to assess the risk of patients with frequent rates of emergency house calls. However, to date, no study has developed risk prediction models for the frequent emergency house calls.
Therefore, we developed and validated a risk score that includes comorbidities and medical interventions in home healthcare to predict frequent emergency house calls among older people who receive regular home visits.
Methods
Study design and data source
We conducted a retrospective cohort study. We obtained linked data on medical and long-term care insurance claims from the municipal governments of two cities (Tsukuba city, Ibaraki Prefecture, and Kashiwa city, Chiba Prefecture) in Japan. As both cities are suburbs in the Tokyo metropolitan area, we combined their data.
Medical claims data included data from individuals with National Health Insurance and Late-stage medical care system for the elderly for individual prefectures, while data from individuals with other health insurance credentials (e.g., insurance for corporate employees) were not included [6, 7]. Generally, the National Health Insurance covered 74% of the population in 2016 [16], aged 65–74, and the Late-stage medical care system covers the entire population, aged 75 and over. Medical insurance claims records included covered diagnoses, medical procedure information, and prescription information on a monthly basis. The recorded diagnoses were based on the original Japanese disease codes linked to the International Classification of Diseases 10th Revision (ICD-10) codes [17]. Long-term care insurance claims data contains information on the care need levels and services used for all residents receiving long-term care services.
The linkage between medical and long-term claims data was made in each municipal government using personally identifiable information. In the data we received, anonymized ID numbers were assigned to individuals in both medical and long-term care insurance claim datasets.
Study population
Individuals who had newly started availing regular home visits between July 2014 and March 2018 in Tsukuba city and between July 2012 and March 2017 in Kashiwa city were included (n = 5895). Individuals who did not receive regular home visits between April and June 2014 in Tsukuba city and between April and June 2012 in Kashiwa city were considered newly enrolled. First, we excluded people whose medical and long-term care claims data could not be linked (n = 534). Next, we excluded people who were < 65 years when they started regular home visits (n = 242). The age of 65 years was chosen as the lower limit because (i) all people ≥65 years are eligible for long-term care insurance benefits, (ii) the vast majority (over 95%) of regular home visits are conducted for this age group [18]. We then excluded those who had a certificate of support level 1 or 2 (n = 231). Long-term care need levels correlate well with the Barthel Index, an internationally accepted indicator for activities of daily living (ADL) [9]. While almost all the people with care need level 5 have a Barthel Index score of 0–40, most with support levels 1 or 2 had a Barthel Index score of ≥60 [9], which is the cut-off point for difficulty in performing basic ADL and dependence on the care of others [19]. Since home visits are generally performed for patients who are disabled and cannot visit a clinic or hospital, we excluded such people. Thus, a final sample of 4888 individuals was evaluated (Fig. 1).
Outcome variable
The primary outcome of the present study was the “frequent” emergency house calls during the period of regular home visits. This was defined as the use once per month or more (on average) during the observation period. We followed up with patients 1 year after the start of the regular home visit or until the month following the end of the regular home visit if this was completed within 1 year. During the period, the total number of emergency house calls was determined using medical insurance records. We calculated the average number of emergency house calls per month by dividing the total number of emergency house calls by the number of months that each person received regular home visits (1–13 months).
Predictor variable
For each patient, we identified variables potentially associated with the frequent emergency house calls, including age (categorized as 65–74, 75–84, 85–94, or ≥ 95 years); gender; medical procedures performed in home medical care including self-injection, central venous nutrition, enteral nutrition, home oxygen therapy [14], use of ventilator/tracheostomy performed, and urinary self-catheterization; long-term care need levels [14] classified as care need level 1, 2–3, and 4–5; medical diagnosis at the start of the regular home visit, including cerebrovascular diseases, cardiac diseases, lower respiratory tract diseases, joint diseases, dementia, Parkinson’s disease, diabetes, visual of hearing impairment, fractures, and cancer. Medical interventions performed in the month in which the regular home visit began were identified from medical insurance claims records. In contrast, the long-term care need levels were determined at the time of the most recent use of long-term care insurance services within 3 months of the start of the regular home visit. We identified medical diagnoses from medical insurance claims data during the 3 months before the start of the regular home visit. Medical diagnoses were categorized based on ICD-10 codes related to diseases associated with the initiation of long-term care in the Comprehensive Survey of Living Conditions in Japan [20] (Supplementary Appendix 1). The “suspected” diagnosis codes were excluded from the datasets.
Statistical analysis
First, we compared those with frequent emergency house calls and the others by using chi-square tests or Fisher’s exact test when the expected frequency was less than 5. Then we performed multivariable logistic regression analysis with all candidate variables included.
To create the most efficient and easy-to-use risk score in actual clinical practice, we used the least absolute shrinkage and selector operation (LASSO) logistic regression, with 10-fold cross-validation and the largest lambda at which the mean-squared error (MSE) was within one standard error of the minimal MSE [21]. LASSO is an extended standard regression model, developed as a parsimonious prediction model by selecting important predictors [22]. The model resulting from LASSO is known to have better predictive model selection performance and predictor identification than classical regression methods [23]. A scoring system was derived by multiplying each beta coefficient from the LASSO logistic regression by 4 and rounding them to the nearest whole number [24]. The integer values of all applicable variables were then summed up to determine a total score for each patient. In the assessment of the discrimination ability of the prediction model, the receiver operating characteristic (ROC) curve for the risk score was drawn, and the area under the curve (AUC) was compared with the model in which all candidate variables were included. Calibration was assessed graphically by plotting the average predicted probabilities against the observed probabilities corresponding to the quintiles of predicted probabilities.
As a post hoc analysis, as we suspected that the discrimination ability of the prediction model varies with age, we compared the characteristics between the different age group (65–84 and over 85 years) using chi-square tests or Fisher’s exact for categorical variables and Mann-Whitney U tests for continuous variables. Thereafter, we assessed AUCs of the 3-factor risk score for the 65–84 and over 85 age groups, separately.
All analyses were conducted using STATA version 15 (Stata Corp., Texas, USA). Statistical significance was set at P < 0.05.
The development and validation of this risk model followed the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) statement [25].
Results
Clinical characteristics of the entire sample are summarized in Table 1. The mean age was 84.1 (standard deviation 7.4) years, and 40.3% of participants were male. In the first year after the start of the regular home visit or by the month after the end of the regular home visit, 13.0% (634/4888) had an emergency house call once a month or more, on average. The distributions of the average number of emergency house calls per month is shown in Supplementary Appendix 2. It showed right-skewed distributions, with 0 accounting for approximately 50%.
The characteristics associated with frequent emergency house calls in the univariable analysis (chi-squared or Fisher’s exact tests) and multivariable analysis are shown in Table 2. In the univariable analysis, patients in the group that made frequent emergency house calls tended to be 65–74 and ≥ 95 years old, male, more likely to be receiving central venous nutrition or home oxygen therapy, and had a higher long-term care need level. Regarding patients’ diseases, lower respiratory diseases and cancer were greater in the group with frequent emergency house calls, whereas those with cerebrovascular diseases, dementia, and fractures were less frequent. In the multivariable logistic regression analysis, home oxygen therapy, care need level 2–5 (compared with care need level 1), and cancer showed positive associations with frequent emergency house calls, whereas cerebrovascular diseases and dementia showed negative associations.
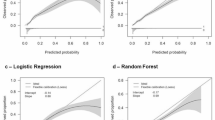
Of the 19 candidate predictors included in the LASSO logistic regression, three were found to be significant predictors of frequent emergency house calls: home oxygen therapy, care need level 4–5, and cancer. The result of the beta coefficient and the created score are summarized in Table 2. The distribution of the total score is shown in Supplementary Appendix 3. The ROC curve and the AUC for the risk score are shown in Fig. 2. Compared with the model of all candidate variables (AUC; 0.734), the predictive ability of the 3-factor risk score (AUC; 0.707) was only slightly lower, which indicates a good discriminatory ability. The calculation of the score and the estimated probability of frequent emergency house calls are shown in Fig. 3. Figure 4 shows the calibration of the prediction model. The plotted points are relatively close to the 45° line, demonstrating good calibration over the whole range of the predictions.
In our post hoc analysis, the 65–84 age group had a higher proportion of males and more medical procedures done at home. Regarding medical diagnoses at the start of the regular home visit, Parkinson’s disease, diabetes, and cancer were more prevalent in the 65–84 age group, whereas cardiac disease, joint diseases, dementia, and fractures were more common in the over 85 age group. The 65–84 age group tended to have shorter duration of regular home visits and more frequent emergency house calls (Supplementary Appendix 4). The AUC of the 3-factor risk score model for the 65–84 age group was 0.766, while for the over 85 age group, it was 0.643.
Discussion
Using claims data from two Japanese cities, we developed and internally validated a multivariable risk prediction model and scoring system to predict frequent emergency house calls. This risk score showed good discrimination and calibration, and satisfactory internal validity. It provides a useful and easily applicable tool for identifying high-risk patients who may require frequent emergency house calls in the community. The home healthcare team should inform patients and families at high risk for frequent emergency house calls and be prepared to contact their health-care provider easily in the unanticipated events. This risk score may also be used as a trigger to initiate advanced care planning for patients who are at a high risk of having frequent emergency house calls.
Our findings regarding the association between cancer patients and frequent emergency house calls are consistent with a previous study reporting that cancer patients are almost seven times more likely to become frequent attenders at primary care after-hours services compared with non-cancer patients [26]. According to a previous study, cancer in the digestive or respiratory system was the most frequent reason for cancer patients’ use of primary care after-hours services [27]. Another previous study showed that the most common complaints in patients with advanced cancer in the emergency department were pain, shortness of breath, and vomiting, which could also be the reason for emergency house calls [28]. In addition, as “death” is one of the major reasons for emergency house calls in Japan [14, 15], calls due to end-of-life care may be included for cancer patients.
Since cancer patients often experience a rapid decline in physical status, appropriate and timely symptom management and palliative care are necessary to continue their stay at home. Despite offering higher quality end-of-life care compared to the inpatient palliative care units, home palliative care remains uncommon in Japan [29]. Indeed, while more than half of the Japanese people stated that they would prefer to stay at home even when facing their end of life, especially in cancer area [30], most cancer deaths occur in general wards of hospitals (72%), followed by palliative care unit (13%); only 11% of deaths occurred at home in 2016 [31]. To provide end of life care in accordance with the wishes of cancer patients, it is necessary to further establish a system that can handle frequent emergency house calls and provide palliative care at home.
We found that frequent emergency house calls were more likely to occur in patients with high care need levels. This finding may be explained as follows: Higher level of care needed is associated with fever events, and fever is a significant reason for emergency house calls [14]. A previous study in Japan found that fever was more likely in patients with care need levels ≥3 than ≤2, and the conditions most likely to cause fever were pneumonia/bronchitis, skin and soft tissue infections, and urinary tract infections [32]. The authors explained that this was due to an increased risk of aspiration because of decreased strength to cough and increased susceptibility to infections caused by decreased muscle strength and poor nutritional status.
Home oxygen use was associated with frequent emergency house calls. This is consistent with a study in Japan, in which dyspnea was a common chief complaint and there was an association between emergency house calls for dyspnea and home oxygen use [14]. Another study has shown that chronic obstructive pulmonary disease (COPD) is more prevalent among those requiring frequent primary care after-hours services, and that complications and exacerbations of chronic diseases are the reasons for this help-seeking behavior [26].
Our results shows that the AUC is higher for those who are 65–84 years old, making this predictive model more applicable. This may be because the 65–84 age group is dominated by patients with cancer and home oxygen therapy, which are included in the 3-factor risk score, while the over 85 age group tends to have more patients with stable chronic diseases. In addition, the decision to request an emergency house call may be more greatly influenced by caregiver factors in very old patients, making the prediction more difficult.
This risk score would be useful to allocate medical resources and maintain a home medical care system in the community. After the Ministry of Health, Labour, and Welfare introduced HCSCs in 2006, enhanced HCSCs, which required the appointment of three or more full-time doctors, were institutionalized in 2012 [12]. Although the number of HCSCs facilities are increasing, enhanced HCSCs account for only a small percentage of the total HCSCs (approximately 24% in 2018) [13]. Moreover, many general clinics do not meet HCSCs requirements while providing home visits [13]. Most of these clinics are in solo practice and have difficulties providing three or more full-time doctors [33]. Therefore, our tool would be helpful for identifying high-risk patients who may require the frequent emergency house calls and reduce the burden on primary care physicians, especially for solo practitioners, by associating high-risk patients to well-staffed medical institutions, such as enhanced HCSCs.
Our tool is based on information that is readily available in a primary care setting. Therefore, this score can indicate the risk at the start of the regular home visits to allow for targeting a timely approach for high-risk patients. Furthermore, because this score contains only three factors, it is easy to remember and can be quickly calculated in clinical practice.
To the best of our knowledge, this is the first study to develop a risk prediction model for the frequent emergency house calls among older people who receive regular home visits. However, this study has several limitations. First, we did not externally validate the proposed model. Since we derived the study population from two different suburbs of Tokyo, the results may be applicable to other suburbs in large cities in Japan. However, external validation using other cohorts with different regional characteristics would be necessary to confirm the generalizability. Furthermore, to build a prediction model that could be implemented across Japan, future studies using nationwide data are necessary. Second, we did not examine some potential predictors that are known risk-factors, such as the urethral catheter placement [14], because information on these factors was not available. Third, some clinical information generally obtained in clinical settings (such as symptoms, laboratory data, and imaging findings) were unavailable in the database. Fourth, although the instances in which patients and their families perceive the need to request emergency house calls may be influenced by appropriate symptom management, enhanced home medical care, palliative care with team coordination, and family caregiver education and support, we were unable to consider these factors. These factors should be included to improve risk score performance in future studies.
Conclusions
This easy-to-use risk scoring allows physicians to prospectively identify patients who are at high risk for emergency house calls. It can help reduce the physical and psychological burdens placed on primary care physicians, by taking measures such as clustering high-risk patients in well-equipped medical facilities, ultimately helping to preserve home medical care in the community.
Availability of data and materials
The data that support the findings of this study are available from Tsukuba city and Kashiwa city but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Tsukuba city and Kashiwa city.
References
Leibowitz R, Day S, Dunt D. A systematic review of the effect of different models of after-hours primary medical care services on clinical outcome, medical workload, and patient and GP satisfaction. Fam Pract. 2003;20:311–7.
T Huibers L, Giesen P, Wensing M, Grol R. Out-of-hours care in western countries: assessment of different organizational models. BMC Health Serv Res. 2009;9:105.
van Uden CJ, Giesen PH, Metsemakers JF, Grol RP. Development of out-of-hours primary care by general practitioners (GPs) in the Netherlands: from small-call rotations to large-scale GP cooperatives. Fam Med. 2006;38:565–9.
Japan cabinet office. Annual report on the aging society. 2019. https://www8.cao.go.jp/kourei/english/annualreport/2019/pdf/2019.pdf. Accessed 20 Apr 2022.
Ministry of Health, Labour and Welfare. Promotion of Long-Term Care and Home Care (in Japanese) 2011. http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000061944.html. Accessed 20 Apr 2022.
Ikegami N, Yoo BK, Hashimoto H, Matsumoto M, Ogata H, Babazono A, et al. Japanese universal health coverage: evolution, achievements, and challenges. Lancet. 2011;378:1106–15.
Ministry of Health, Labour and Welfare. An Outline of the Japanese Medical System. https://www.mhlw.go.jp/english/policy/health-medical/health-insurance/index.html. Accessed 20 Apr 2022.
Tamiya N, Noguchi H, Nishi A, Reich MR, Ikegami N, Hashimoto H, et al. Population ageing and wellbeing: lessons from Japan's long-term care insurance policy. Lancet. 2011;378:1183–92.
Matsuda T, Iwagami M, Suzuki T, Jin X, Watanabe T, Tamiya N. Correlation between the Barthel index and care need levels in the Japanese long-term care insurance system. Geriatr Gerontol Int. 2019;19:1186–7.
Tsutsui T, Muramatsu N. Care-needs certification in the long-term care insurance system of Japan. J Am Geriatr Soc. 2005;53:522–7.
Fukui S, Yamamoto-Mitani N, Fujita J. Five types of home-visit nursing agencies in Japan based on characteristics of service delivery: cluster analysis of three nationwide surveys. BMC Health Serv Res. 2014;14:644.
Ohta H. Current conditions and issues for home care support clinics. Jpn Med Assoc J. 2015;58:6–9.
General meeting materials of central social insurance medical council (in Japanese). 2019. https://www.mhlw.go.jp/content/12404000/000563523.pdf. Accessed 20 Apr 2022.
Kuroda K, Miura T, Kuroiwa S, Kuroda M, Kobayashi N, Kita K. What are the factors that cause emergency home visit in home medical care in Japan? J Gen Fam Med. 2021;22:81–6.
Kaneko M, Van Boven K, Takayanagi H, Kusaba T, Yamada T, Matsushima M. Multicentre descriptive cross-sectional study of Japanese home visit patients: reasons for encounter, health problems and multimorbidity. Fam Pract. 2020;37:227–33.
National Health Insurance Survey Report in 2016 (in Japanese). https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450397&tstat=000001111735&result_page=1. Accessed 20 Mar 2022.
ICD-10 Corresponding Diagnosis Code Master (in Japanese). http://www2.medis.or.jp/stdcd/byomei/index.html. Accessed 15 Nov 2021.
Reference materials for the 1st National Conference on home medical care (in Japanese). 2016. https://www.mhlw.go.jp/file/05-Shingikai-10801000-Iseikyoku-Soumuka/0000129546.pdf. Accessed 20 Apr 2022.
Uyttenboogaart M, Stewart RE, Vroomen PC, De Keyser J, Luijckx GJ. Optimizing cutoff scores for the Barthel index and the modified Rankin scale for defining outcome in acute stroke trials. Stroke. 2005;36:1984–7.
Iwagami M, Taniguchi Y, Jin X, Adomi M, Mori T, Hamada S, et al. Association between recorded medical diagnoses and incidence of long-term care needs certification: a case control study using linked medical and long-term care data in two Japanese cities. Ann Clin Epidemiol. 2019;1:56–68.
Sabourin JA, Valdar W, Nobel AB. A permutation approach for selecting the penalty parameter in penalized model selection. Biometrics. 2015;71:1185–94.
Tibshirani R. Regression shrinkage and selection via the Lasso. J R Stat Soc B. 1996;58:267–88.
Oh E, Yoo TK, Park EC. Diabetic retinopathy risk prediction for fundus examination using sparse learning: a cross-sectional study. BMC Med Inform Decis Mak. 2013;13:106.
Moons KG, Harrell FE, Steyerberg EW. Should scoring rules be based on odds ratios or regression coefficients? J Clin Epidemiol. 2002;55:1054–5.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162:55–63.
Sandvik H, Hunskaar S. Frequent attenders at primary care out-of-hours services: a registry-based observational study in Norway. BMC Health Serv Res. 2018;18:492.
Thoresen CK, Sandvik H, Hunskaar S. Cancer patients’ use of primary care out-of-hours services: a cross-sectional study in Norway. Scand J Prim Health Care. 2016;34:232–9.
Alsirafy SA, Raheem AA, Al-Zahrani AS, Mohammed AA, Sherisher MA, El-Kashif AT, et al. Emergency department visits at the end of life of patients with terminal cancer: pattern, causes, and avoidability. Am J Hosp Palliat Care. 2016;33:658–62.
Miyashita M, Morita T, Sato K, Tsuneto S, Shima Y. A nationwide survey of quality of end-of-life cancer care in designated cancer centers, inpatient palliative care units, and home hospices in Japan: the J-HOPE study. J Pain Symptom Manag. 2015;50:38–47.
Japanese Ministry of Health, Labour and Welfare. The results of the survey on awareness of the elderly people about their health (in Japanese). 2017. https://www.mhlw.go.jp/file/05-Shingikai-10801000-Iseikyoku-Soumuka/0000200749.pdf. Accessed 20 Apr 2022.
Hospice and palliative care white paper 2018. https://www.hospat.org/assets/templates/hospat/pdf/hakusyo_2018/2018-all.pdf. Accessed 20 Apr 2022.
Yokobayashi K, Matsushima M, Watanabe T, Fujinuma Y, Tazuma S. Prospective cohort study of fever incidence and risk in elderly persons living at home. BMJ Open. 2014;4:e004998.
General meeting materials of central social insurance medical council (in Japanese). 2013. https://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000027959.pdf. Accessed 20 Apr 2022.
Acknowledgments
We would like to thank Editage (www.editage.jp) for its English language editing.
Funding
This research was supported by a grant-in-aid from the Ministry of Health, Labour and Welfare; Health, Labour and Welfare Sciences Research Grant, Japan; Research on Region Medical (21IA1010) and JSPS KAKENHI (Grant Number 19K19430).
Author information
Authors and Affiliations
Contributions
Study concept and design: Yu Sun, Masao Iwagami, Miho Ishimaru, Kazuaki Uda. Acquisition of data: Naoaki Kuroda, Satoru Yoshie, Tatsuro Ishizaki, Katsuya Iijima. Maintenance of data: Jun Komiyama, Miho Ishimaru. Statistical analysis and interpretation of data: Yu Sun, Masao Iwagami, Kazuaki Uda. Preparation of manuscript: all authors contributed to the drafting and critical revision of the manuscript. All authors have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the University of Tsukuba (approval numbers: 1445–6 and 1666). All methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Consent of individual participants was waived because of the anonymous nature of the data.
Competing interests
The authors have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Appendix 1.
List of medical diagnosis categories and International Classification of Diseases 10th Revision codes.
Additional file 2: Supplementary Appendix 2.
Distribution of the average number of emergency house calls per month.
Additional file 3: Supplementary Appendix 3.
Distribution of the total score.
Additional file 4: Supplementary Appendix 4.
Comparison of patient characteristics across age groups.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, Y., Iwagami, M., Sakata, N. et al. Development and validation of a risk score to predict the frequent emergency house calls among older people who receive regular home visits. BMC Prim. Care 23, 132 (2022). https://doi.org/10.1186/s12875-022-01742-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-022-01742-7