Abstract
Background
The American Heart Association (AHA) recently defined a new concept of cardiovascular health-Life’s Essential 8 (LE8). We sought to examine whether LE8 score is associated with a risk of all-cause and cardiovascular disease (CVD)-related mortality in individuals with hypertension.
Methods
This longitudinal study analyzed data from the National Health and Nutrition Examination Survey from 2007 to 2018 in people 20 years or older with hypertension. LE8 score (range 0-100) was measured according to the AHA definition and divided into unweighted tertiles into groups T1 (< 50.00), T2 (50.00-61.25), and T3 (≥ 61.25). Primary outcomes included all-cause mortality and CVD-specific mortality.
Results
A total of 15,318 individuals with hypertension were included in this study, with a mean ± standard error age of 55.06 ± 0.25 years. During the median follow-up period of 76 months, 2525 all-cause mortality occurred, of which 806 were due to CVD. Compared with participants with hypertension in the T1 group, those in T2 and T3 respectively had 28% (adjusted HR = 0.72, 95% CI 0.63–0.83, P < 0.001) and 39% (adjusted HR = 0.61, 95% CI 0.52–0.72, P < 0.001) lower risk of all-cause mortality, the T2 and T3 groups were associated with 32% (adjusted HR = 0.68, 95% CI 0.53–0.88, P = 0.003) and 36% (adjusted HR = 0.64, 95% CI 0.49–0.84, P = 0.001) reduced risk of CVD mortality separately.
Conclusions
A higher LE8 score is associated with a lower risk of all-cause mortality and CVD mortality, and the higher LE8 score can be maintained in the clinic to improve prognosis by modifying the diet and lifestyle habits of individuals with hypertension.
Similar content being viewed by others
Background
Hypertension is a highly prevalent chronic disease worldwide and major modifiable risk factor for cardiovascular disease (CVD), approximately 33% of the global population currently suffer from hypertension [1, 2]. Compared to the general population, individuals with hypertension have a higher risk of all-cause and CVD-related mortality [3]. Hypertension has brought heavy burden to society and family, prevention and treatment of hypertension remains a major long-term public health challenge.
In 2010, the American Heart Association (AHA) constructed Life’s Simple 7 (LS7) to characterize cardiovascular health (CVH) based on 7 health behaviors and health factors, aiming to facilitate a shift from focusing solely on disease treatment to the active promotion and maintenance of health throughout the life course of populations and individuals [4]. In 2022, the AHA updated the definition of CVH based on experience and evidence, which added sleep to construct Life’s Essential 8 (LE8) and quantified each metric from 0 to 100, including health behaviors (diet, physical activity, nicotine exposure, sleep health), and health factors (body mass index (BMI), blood lipids, blood glucose, and blood pressure) [5]. The LE8 is a scoring system that is more sensitive to inter-individual differences and emphasizes the social determinants of health and mental health that maintain or improve cardiovascular health (CVH). Population-based evidence suggests that high LE8-based CVH is associated with a lower risk of all-cause and CVD-related mortality in US adults, this association remains significant regardless of the presence of diabetes [6,7,8]. In addition, cohort studies have shown that LS7-based CVH is significantly inversely associated with the risk of developing hypertension [9]. However, few studies have investigated the applicability of LE8 in individuals with hypertension.
Healthy lifestyles not only are the cornerstone of prevention and treatment of hypertension, but also may improve CVH and general health [10]. LE8 highlights social determinants of health and psychological health for maintaining or improving CVH [5]. To date, the association between LE8 score and the risk of all-cause and CVD-related mortality in individuals with hypertension has not been reported. To fill this research gap, The primary objectives of this study were to explore this issue based on the National Health and Nutrition Examination Survey (NHANES), a representative database.
Methods
Individuals and study design
NHANES is a program of studies designed to assess the health and nutritional status of adults and children in the United States [11]. The National Center for Health Statistics (NCHS) administered the survey, and the NCHS Institutional Ethical Review Board approved the research protocol. NHANES obtained written informed consent from all participants. NHANES data conducted between 2007 and 2018 were used for this study. Hypertension was defined as self-reported hypertension or systolic blood pressure ≥ 130 mmHg, diastolic blood pressure ≥ 80 mmHg (AHA2017 [12]) or taking antihypertensive medication. All experimental protocols were approved by Institutional Review Board (IRB) of Henan Provincial People’s Hospital (2024-59).
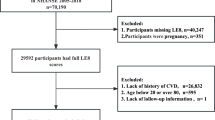
The study involved individuals diagnosed with hypertension (n = 19867) in the NHANES 2007–2018. Exclusion criteria included: (1) age < 20 years; (2) missing complete information on LE8 score assessment; (3) missing complete survival information; (4) missing important co-variates (educational level, marital status, cancer, creatinine). The final study population included 15,318 adult participants (Fig. 1).
Mortality ascertainment
The outcome variables of this study were all-cause mortality and CVD-cause mortality. Mortality information in the National Death Index (NDI) was from the date of survey participation through 31 December 2019. All data in this study are publicly available at https://www.cdc.gov/nchs/data-linkage/mortality.htm. Deaths from any cause were classified as all-cause deaths; deaths due to “disease of the heart (I00-I09, I11, I13, I20-I51)” or “cerebrovascular diseases (I60-I69)” were recorded as CVD-related deaths [13]. The cut-off time for follow-up was December 31, 2019, and the median follow-up duration (T1, T3) was 76 (42, 114) months.
Measurement of life’s essential 8
The LE8 scoring algorithm consists of diet (dietary approach to stop hypertension-style diet), physical activity, nicotine exposure, sleep duration, BMI, non-high-density lipoprotein cholesterol levels, blood glucose status, and blood pressure levels. The eight CVH indicators were scored on a scale of 0 to 100. Detailed scoring criteria for each metric [5, 14] are demonstrated in Supplementary Table 1. The overall LE8 score was calculated as the unweighted average of the eight metrics. In this study, the scores were grouped according to unweighted tertiles: LE8 score < 50.00 is T1; 50.00-61.25 is T2; ≥61.25 is T3.
Study covariates
Covariates in the all-cause mortality as outcome model: age, race (non-Hispanic white, non-Hispanic black, Mexican American, and others), educational level (less than high school, high school, and above high school), marital status (married & living with partner, never married & divorced & separated & widowed), alcohol drinking (yes, no), CVD (yes, no), cancer (yes, no), and waist circumference (low, high, and unknown), and eGFRCKD−EPI. As for covariates in the CVD mortality as outcome model: age, educational level, marital status, CVD, eGFRCKD−EPI.
Statistical analysis
Given the complex sampling design of NHANES, all analyzes in this study account for sample weights, clustering, and stratification to generate nationally representative estimates. Measurement data were described as mean ± standard error (S.E), and t-tests were used to compare differences between groups. Enumeration data were described using the number of cases and proportions, and comparisons of differences between groups were made using the chi-square test or Fisher’s exact test. Variables with P < 0.05 were screened using a weighted univariate Cox model with all-cause and CVD mortality as outcomes. A weighted multivariate Cox model was constructed using all potentially relevant variables, and variables were screened by backward stepwise regression. After adjusting for covariates, a weighted multivariate Cox proportional hazards regression model was used to examine the hazard ratio (HR) and 95% confidence interval (CI) for the associations between LE8 scores and the risk of all-cause death and CVD mortality, respectively. All-cause mortality and CVD-related mortality were used as endpoints, respectively, and a random survival forest model was constructed through the R package randomForestSRC to rank the importance of the variables in the LE8 score using the Variable Importance (VIMP) method. SAS 9.4 was used for data extraction, and R version 4.2.3 was used for data cleaning, interpolation of missing values, comparison of differences, screening of covariates, weighted Cox regression, and subgroup analysis. Differences were considered statistically significant when the P-value was 0.05 or less. All statistical tests were two-sided.
Results
Baseline characteristics
A total of 15,318 individuals aged 20 years or older were included in the study. Table 1 summarizes the baseline characteristics of the study population by all-cause mortality or not. The mean (S.E) individuals age was 55.06 ± 0.25 years, and 7961 (weighted percentage [WP], 51.85%) individuals were male. Only a small number of individuals (n = 2648; WP, 14.42%) suffer from CVD, whereas 81.35% (WP) of individuals (n = 12438) suffer from dyslipidemia. The mean (S.E) LE8 score of the study population was 57.81 ± 0.21, with T1 (< 50.00), T2 (50.00-61.25), and T3 (≥ 61.25) LE8 scores accounting for (WP) 27.89%, 33.27%, and 38.84% respectively. The mean (S.E) LE8 score was lower (55.59 ± 0.53) in individuals who experienced all-cause mortality and the difference was statistically significant (P = 0.001). Among this study population, 2525 individuals experienced all-cause mortality, including 806 individuals who experienced CVD-related mortality; the mean (S.E) survival time for all individuals was 85.07 ± 1.53 months.
Association of life’s essential 8 score with risk of all-cause and cardiovascular disease-related mortality in individuals with hypertension
In a weighted univariate Cox proportional hazards regression model, lower levels of LE8 score were associated with the risk of all-cause mortality (P < 0.001). At the same time, age, race, educational level, marital status, alcohol consumption, CVD, cancer or not, waist circumference, and eGFRCKD−EPI were all associated with the risk of all-cause mortality (Table 2). For individuals with hypertension, the results of the adjusted multiple Cox proportional hazard regression are shown in Model 2 of Table 3, after adjusting for age, race, educational level, marital status, alcohol drinking, CVD, cancer, waist circumference and eGFRCKD−EPI. Compared with individuals with hypertension with low LE8 score (T1: < 50.00), individuals in group T2 (adjusted HR = 0.72, 95% CI 0.63–0.83, P < 0.001) and group T3 (adjusted HR = 0.61, 95% CI 0.52–0.72, P < 0.001) were associated with a lower risk of all-cause mortality.
The risk of CVD-cause mortality among different LE8 score groups differed significantly on the basis of the weighted univariate Cox regression analysis. After adjusting for potential confounders(age, educational level, marital status, CVD, eGFRCKD−EPI), the T2 and T3 groups were associated with 32% (adjusted HR = 0.68, 95% CI 0.53–0.88, P = 0.003) and 36% (adjusted HR = 0.64, 95% CI 0.49–0.84, P = 0.001) reduced risk of CVD mortality separately (Table 3).
Importance of life’s essential 8 score components in predicting all-cause and cardiovascular disease-related mortality
A random survival forest model was constructed using the different components of the LE8 score for the outcomes of all-cause mortality (Fig. 2A) and CVD-related mortality (Fig. 2B), respectively. The importance (VIMP value) of each component was ranked, higher VIMP indicating that the variable contributed more to the prediction of the outcome events. As shown in Fig. 2, the rank order of the components of the LE8 were similar for all-cause mortality and CVD-mortality. In both models, blood pressure was the most important predictor variable, followed by blood glucose and physical activity.
Subgroup analysis
To further observe the association between LE8 score and the risk of mortality in different subgroups of individuals with hypertension, subgroup analyses were conducted according to age (whether or not ≥ 60 years old), gender, BMI, and comorbidities (CVD and cancer), and the results are presented in forest plots (Figs. 3 and 4). Across all subgroups, higher levels of LE8 score were associated with a lower risk of all-cause mortality compared with lower levels of LE8 scores (Fig. 3). The analyses of CVD-mortality showed that the associations of LE8 score with the outcome was generally consistent across the various subgroups (Fig. 4).
Discussion
In this nationally representative longitudinal study, we found that individuals with hypertension with higher LE8 scores had lower all-cause and CVD-specific mortality. Various stratification and sensitivity analyses demonstrated the robustness of our results. These findings suggest that obtaining a higher LE8 score may lead to a substantial reduction in mortality in individuals with hypertension.
A large number of studies have demonstrated a strong stepwise inverse relationship between the number of ideal CVH metrics or overall CVH score and total CVD and CVD mortality, all-cause mortality, and various non-CVD outcomes [6,7,8, 15,16,17]. In a meta-analysis of 9 prospective cohort studies, the highest LS7 score was associated with a relative risk of 25% for CVD mortality (95% CI, 0.10–0.63) and 45% lower risk of all-cause mortality (95% CI, 0.37–0.80) in all individuals [18]. All LS7-defined CVH metrics affect the risk of health outcomes [19]. However, as the precursor to LE8, the LS7 characteristic definitions may not ideally represent the full range of health behaviors and practices in the current context [5, 20]. The AHA updated the definitions of diet, nicotine exposure, blood lipids, and glucose metrics and added sleep health as a new metric for CVH in LE8. Multiple studies have evaluated the association between LE8 score and all-cause and CVD mortality among U.S. adults [6,7,8]. Higher LE8 scores were independently associated with a lower risk of all-cause disease and CVD mortality. There was an approximately linear dose-response association between increases in total CVH index scores and reductions in all-cause and CVD-specific mortality [7]. Analysis on these researches showed close relation among LE8 score and all-cause and CVD-specific mortality.
CVD is the leading cause of death worldwide, and the development of hypertension is a major risk factor for CVD [21]. The REGARDS Study has been shown that optimization of CVH components, as defined by the Life’s Simple 7 metric, might reduce risk of incident hypertension among at-risk adults [9]. It is unknown whether the Life’s Simple 7 metric or LE8 metric is associated with all-cause and CVD mortality in hypertensive individuals. To our knowledge, this is the first attempt to examine the relationship between the AHA’s new LE8 metric and scoring algorithm and long-term prognosis in hypertension. This study suggests that the higher the LE8 index, the lower the risk of all-cause mortality and CVD-related mortality in hypertensive individuals. A higher level of LE8 can be maintained by modifying the diet and lifestyle habits of individuals with hypertension, thereby improving prognosis. As is similar with our result, international society of hypertension position paper also suggests that lifestyle changes be continued even when blood pressure-lowering medications are prescribed [10]. In addition, our results also showed that blood pressure, blood glucose and physical activity in the LE8 score contribute the most to the risk of all-cause and CVD-specific mortality in hypertensive individuals. Because of it, Severe blood pressure, blood sugar control and lifestyle change were recommended to management of hypertension by the hypertension guidelines [10]. There was insufficient evidence for a significant association between T3 and CVD-related mortality compared with T1 of LE8 among hypertensive individuals with CVD and cancer. The possible reason for this is the small number of CVD-related deaths in these two subgroups, which needs to be further explored by increasing the sample size in subsequent studies.
Investigations of mechanisms through which higher CVH is associated with lower CVD risk (or lower CVH with higher risk) have identified several potential pathways involving inflammation, endothelial function, atherosclerosis, cardiac stress and remodeling, hemostatic factors, and epigenetics [22, 23]. Taken together, the substantial body of knowledge gained about CVH indicates that it is uniquely positioned as a health outcome itself related to upstream genetic, social, behavioral, and environmental factors, and as a determinant of major downstream health outcomes. Across the life course, assessment of CVH status has been shown to be an effective means to monitor public and individual health and a strong indicator of the extraordinary potential of primordial prevention strategies to improve and extend countless lives [5].
A major strength of this study is the use of a nationally representative sample of U.S. adults, which allows the findings to be generalized to the broader population, however, potential limitations of our study include the following. First, assessment of health behavior indicators was based on self-report questionnaires subject to measurement error. Second, we were unable to dynamically assess longitudinal changes in participants’ CVH status because NHANES does not provide follow-up examinations. Finally, although we adjusted for several potential confounders, the nature of the longitudinal study design precluded us from drawing causal and temporal conclusions about the relationship between LE8 score and risk of mortality in individuals with hypertension. In future research, Life’s Essential 8 metrics will be used to instruct the comprehension management and control of hypertension, and improve the long-term prognosis of individuals with hypertension.
Conclusions
Our study demonstrated that a higher LE8 score could be especially important for individuals with hypertension not only in reducing the risk of all-cause mortality but also in CVD-specific mortality. Furthermore, it is worth noting that blood pressure, blood glucose and physical activity in the LE8 score contribute the most to reducing the risk. These findings suggest that maintain a higher LE8 score in hypertensive individuals, especially severe blood pressure and blood sugar control and lifestyle change, may reduce the risk of early mortality in the later stages of life.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AHA:
-
American Heart Association
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- CVD:
-
Cardiovascular Disease
- CVH:
-
Cardiovascular Health
- HR:
-
Hazard Ratio
- LE8:
-
Life’s Essential 8
- LS7:
-
Life’s Simple 7
- NCHS:
-
National Center for Health Statistics
- NHANES:
-
National Health and Nutrition Examination Survey
- S.E:
-
Standard Error
- VIMP:
-
Variable Importance
- WP:
-
Weighted Percentage
References
NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Tomaszewski M, Itoh H. ISH2022KYOTO hypertension zero decla-ration. Hypertens Res. 2023;46:1–2.
Aune D, Huang W, Nie J, Wang Y. Hypertension and the risk of all-cause and cause-specific mortality: an Outcome-Wide Association Study of 67 Causes of Death in the National Health interview survey. Biomed Res Int. 2021;2021:9376134.
Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613.
Lloyd-Jones DM, Allen NB, Anderson CAM, et al. Life’s essential 8: updating and enhancing the American Heart Association’s construct of Cardiovascular Health: a Presidential Advisory from the American Heart Association. Circulation. 2022;146(5):e18–43.
Yi J, Wang L, Guo X, Ren X. Association of Life’s essential 8 with all-cause and cardiovascular mortality among US adults: a prospective cohort study from the NHANES 2005–2014 [J]. Nutr Metab Cardiovasc Dis: NMCD. 2023;33(6):1134–43.
Sun J, Li Y, Zhao M, Yu X, Zhang C, Magnussen CG, Xi B. Association of the American Heart Association’s new Life’s essential 8 with all-cause and cardiovascular disease-specific mortality: prospective cohort study. BMC Med. 2023;21(1):116.
Sun Y, Yu Y, Zhang K, Yu B, Yu Y, Wang Y, et al. Association between Life’s essential 8 score and risk of premature mortality in people with and without type 2 diabetes: a prospective cohort study. Diabetes Metab Res Rev. 2023;39(5):e3636.
Plante TB, Koh I, Judd SE, Howard G, Howard VJ, Zakai NA, et al. Life’s simple 7 and Incident Hypertension: the REGARDS Study. J Am Heart Assoc. 2020;9(19):e016482.
Charchar FJ, Prestes PR, Mills C, Ching SM, Neupane D, Marques FZ, et al. Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens. 2023. https://doi.org/10.1097/HJH.0000000000003563. Epub ahead of print.
Centers for Disease Control and Prevention. National health and nutrition examination survey. National center for health statistics.2022. https://www.cdc.gov/nchs/nhanes/index.htm. Accessed 26 Aug 2022.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH et al. /ASPC /NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138(17): e426-e483.
Kim D, Konyn P, Sandhu KK, Dennis BB, Cheung AC, Ahmed A. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J Hepatol. 2021;75(6):1284–91.
Lloyd-Jones DM, Ning H, Labarthe D, Brewer L, Sharma G, Rosamond W, Foraker RE, Black T, Grandner MA, Allen NB, Anderson C, Lavretsky H, Perak AM. Status of Cardiovascular Health in US adults and Children Using the American Heart Association’s New Life’s essential 8 Metrics: Prevalence Estimates from the National Health and Nutrition Examination Survey (NHANES), 2013 through 2018. Circulation. 2022;146(11):822–35.
Xing A, Tian X, Wang Y, Chen S, Xu Q, Xia X, Zhang Y, Zhang X, Wang A, Wu S. Life’s essential 8’ cardiovascular health with premature cardiovascular disease and all-cause mortality in young adults: the Kailuan prospective cohort study. Eur J Prev Cardiol. 2023;30(7):593–600.
Chen H, Tang H, Huang J, Luo N, Zhang X, Wang X. Life’s Essential 8 and Mortality in US Adults with Chronic Kidney Disease. Am J Nephrol. 2023 Aug;17. https://doi.org/10.1159/000533257. Epub ahead of print. PMID: 37591229.
Isiozor NM, Kunutsor SK, Voutilainen A, Laukkanen JA. Life’s essential 8 and the risk of cardiovascular disease death and all-cause mortality in Finnish men. Eur J Prev Cardiol. 2023;30(8):658–67.
Fang N, Jiang M, Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: a meta-analysis. Int J Cardiol. 2016;214:279–83.
Folsom AR, Yatsuya H, Nettleton JA, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690–6.
Gao X, Ma X, Lin P, Wang Y, Zhao Z, Zhang R, Yu B, Hao Y. Predictive Value of Cardiovascular Health Score for Health Outcomes in patients with PCI: comparison between Life’s simple 7 and Life’s essential 8. Int J Environ Res Public Health. 2023;20(4):3084.
Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular diseases and Risk factors, 1990–2019: Update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Joyce BT, Gao T, Zheng Y, Ma J, Hwang SJ, Liu L, et al. Epigenetic age acceleration reflects long-term Cardiovascular Health. Circ Res. 2021;129(8):770–81.
Pottinger TD, Khan SS, Zheng Y, Zhang W, Tindle HA, Allison M, et al. Association of cardiovascular health and epigenetic age acceleration. Clin Epigenetics. 2021;13(1):42.
Acknowledgements
We thank the National Health and Nutrition Examination Survey participants and staff and the National Center for Health Statistics for their valuable contributions.
Funding
This work was supported by the Provincial and Ministry joint construction youth project of Henan Province Medical Science and Technology Public Relations Plan (SBGJ202103006), Joint construction project of Henan Province Medical Science and Technology Public Relations Plan (LHGJ20210038, LHGJ20220001). The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
We have approved the submitted version (and any substantially modified version that involves the author’s contribution to the study).Minghu Zhao: Conceptualization (equal); data curation (equal); formal analysis (equal); methodology (equal); project administration (equal); writing original draft (lead). Haijia Yu: Formal analysis (equal); writing original draft (equal). Suyuan He: Formal analysis (equal); methodology (equal); project administration (equal). Xiaojing He: Investigation (equal); project administration (equal). Jugang Chen: Conceptualization (lead); supervision (lead); validation (lead); writing review and editing (lead).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the institutional review board of the NCHS. Written informed consent to participate in NHANES III was obtained from all participants.
Consent for publication
Consent to publish has been obtained from all authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, M., Yu, H., He, S. et al. Association of life’s essential 8 score with risk of all-cause and cardiovascular disease-related mortality in individuals with hypertension. BMC Cardiovasc Disord 24, 465 (2024). https://doi.org/10.1186/s12872-024-04115-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-04115-3