Abstract
This study explores the association between LE8 scores and mortality risks among individuals diagnosed with cardiovascular disease (CVD). Utilizing data from the NHANES conducted between 2005 and 2018, survey-weighted multivariable Cox proportional hazards regression models were utilized. Life’s Essential 8 (LE8) scores dose–response associations were assessed using restricted cubic spline regression. Sub-analyses were performed for different categories of CVD. The study consisted of 2164 participants diagnosed with CVD, ranging in age from 20 to 80 years (weighted mean [SE] age, 61.47 [0.34] years; The average total LE8 was 64.97 [0.54]. 499 participants experienced mortality, with 350 deaths attributed to CVD. After accounting for potential covariates, LE8 score was found to be associated with a decreased both all-cause mortality (OR 0.34, CI 0.22–0.51) and CVD mortality (OR 0.40, CI 0.23–0.68). A survey-weighted multivariable Cox model with restricted cubic splines identified the lowest all-cause mortality (P < 0.001) and CVD mortality (P < 0.001) risk when LE8 reach at 63.75 (P < 0.001). The results highlight the association between LE8 scores and reduced mortality in CVD patient population. The implementation of comprehensive initiatives that prioritize healthy dietary patterns, will play a crucial role in alleviating the impact of cardiovascular disease and improving cardiovascular health outcomes.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is a prominent contributor to mortality rates and presents a substantial health burden on a global scale1. The most recent Global Burden of Disease (GBD) study revealed that CVD accounted for 12.1 million deaths worldwide, with ischemic heart disease and stroke being the primary causes, comprising 49% and 35% of the total burden, respectively2. Despite a consistent decline in mortality rates associated with CVD3, with the increasing and aging world population, CVD has emerged as the most prevalent burden of disease worldwide4. The implementation of effective preventive measures for CVD is of utmost importance in mitigating the future disease burden and enhancing cardiovascular health (CVH), particularly among individuals already afflicted with CVD5, which can reduce the risk of CVD, mortality, and disease burden.
Several large epidemiological studies have found that sleep is associated with CVD, short and long sleep durations are emerging as important behavioral risk factors for mortality. To address more comprehensive CVH concerns and establish quantifiable measures for monitoring and assessing it within the broader population, the American Heart Association has recently introduced the revised algorithm for evaluating CVH known as Life’s Essential 8 (LE8) score6. This updated algorithm encompasses various factors such as diet, physical activity, smoking habits, body mass index (BMI), blood lipids, blood glucose levels, blood pressure, and sleep time, which is more and more importance factor for CVH. Thus, the LE8 score may act as a novel, personalized, and comprehensive indicator to assess the prognosis and clinical outcomes of CVD, which requires additional research in CVD groups and special populations. The intricate interplay between individual health behaviors and physiological measures reveals distinctive associations with diverse risk factors linked to CVD. The need for additional evidence becomes apparent, especially when utilizing comprehensive measures of CVD and mortality. A detailed examination focusing on all components is indispensable. This thorough analysis is crucial for customizing preventive strategies and interventions, specifically directed at nuanced aspects of lifestyle and health. By doing so, there is potential for a significant impact on CVD outcomes. The imperative for further research persists to refine our comprehension of these complex relationships within the realm of CVH.
The initial investigation documented significant correlations, revealing that higher LE8 scores were associated with extended lifespans among adults in the United States (US)7. Another independent study corroborated these findings, highlighting that a higher LE8 score exhibited a distinct correlation with reduced risks of both all-cause and cardiovascular mortality among US adults8. Trend research suggests that the overall CVH of US adults remained stable from 2005 to 2018. During this period, positive developments were noted in nicotine exposure, blood lipids, and sleep health. However, there were simultaneous deteriorations in BMI and blood glucose levels9. Despite the wealth of studies on LE8, there is a noticeable gap in research concerning the correlation between all-cause mortality and CVD mortality with LE8 scores among individuals with CVD. Additionally, limited research has explored the dose–response relationship between levels of LE8 score and mortality in individuals with CVD. This study, utilizing data from the National Health and Nutrition Examination Survey (NHANES), aims to evaluate the associations between the LE8 score and the likelihood of mortality. Furthermore, it seeks to investigate the dose–response relationship between levels of LE8 score and mortality in participants diagnosed with CVD.
Methods
NAHNES was a nationally representative survey of the civilian, noninstitutionalized US population, which was conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention (CDC). Initiated in 1999, NHANES has been carried out in 2-year cycles, serving as a pivotal tool in monitoring the health and nutritional status of the entire US population. The protocols of NHANES were subject to approval by the ethics review board of the National Center for Health Statistics, with written informed consent obtained from all participants. This modeling investigation was granted exemption from review, as it solely utilized deidentified datasets that did not contain any personally identifiable information. All methods were performed in accordance with the relevant guidelines and regulations.
Study population
This cross-sectional study included participants from the nationally representative consecutive NHANES 2005–2018 cohort. The selection of this timeframe was based on the incorporation of sleep data into the LE8 from the year 2005 onwards (https://www.cdc.gov/nchs/data_access/restrictions.htm). Among the 70,190 subjects in the NHANES 2005–2018 cohort, individuals were excluded based on the following criteria: (1) missing data on the LE8 (n = 40,247), (2) pregnancy status (n = 351), (3) any missing values for CVD history (n = 26,832), (4) age falling outside the range of 20–80 years (n = 595), and (5) any missing values for mortality status (n = 1). Ultimately, 2164 subjects were deemed eligible and included in this research study. The patient selection flowchart can be seen in Fig. 1.
Definition of CVD
For this study, participants were classified as individuals with CVD if they responded affirmatively to any of the following inquiries: "Has a doctor or other health professional ever informed you of a diagnosis of congestive heart failure (CHF), coronary heart disease (CHD), angina pectoris, heart attack, or stroke?".
Measurement of LE8
The LE8 score is composed of four primary health behaviors, namely, diet, physical activity, nicotine exposure, and sleep duration, along with four health factors, including BMI, non-high-density lipoprotein cholesterol (non-HDL cholesterol), blood glucose, and blood pressure. Dietary patterns were evaluated using the Healthy Eating Index (HEI) 2015, obtained from the subjects' 24-h dietary recall10. Information on physical activity11, nicotine exposure12, sleep patterns, history of diabetes, and medication usage was gathered through a self-report questionnaire. Physical examination procedures were employed for the measurement of height, weight, and blood pressure, with BMI derived from the quotient of weight (in kilograms) divided by the square of height (in meters). Blood samples were collected for the assessment of non-HDL cholesterol, plasma glucose, and hemoglobin A1c. The detailed algorithm utilized for calculating the LE8 scores from the NHANES data has been previously documented7 (Supplementary Table S1). Each of the eight CVH indicators was assigned a score ranging from 0 to 100, with the total LE8 score calculated as an unweighted average of these eight indicators. In line with prior conventions, participants were categorized into three groups based on their CVH levels: those with high CVH were allocated LE8 scores in the range of 80–100, moderate CVH corresponded to scores of 50–79, and low CVH was represented by scores falling within the 0–49 range.
Ascertainment of mortality
Data for deaths were obtained by linking to the NHANES-linked National Death Index public access files. Cause of death was defined using the International Statistical Classification of Disease, Tenth Revision (ICD-10). All-cause, CVD, and non-CVD mortality were primary outcomes. Death from all reasons was defined as all-cause mortality, CVD mortality was defined as ICD-10 codes, otherwise, deaths were defined as non-CVD mortality. The follow-up duration was calculated from the date of the initial interview to the date of death or the conclusion of the follow-up period (December 31, 2019).
Covariate assessment
Demographic characteristics were collected by questionnaires during the home interview. In this study, age was stratified into 3 strata: 20–39 years, 40–59 years, or ≥ 60 years. Race/ethnicity was categorized as non-Hispanic (NH)White, NH Black, Hispanic, and Other. The poverty ratio was calculated as the ratio of monthly family income to poverty levels defined by Department of Health and Human Services guidelines and was categorized into 3 groups: < 1.3 (low income), 1.3–3.5 (middle income), and > 3.5 (high income). Education levels were categorized as high school graduate, less or above. Marital status was categorized as coupled and single or separated. The medical history and health status of participants were collected by self-report questionnaires. Depression was measured using the Patient Health Questionnaire 9 (PHQ-9). Scores of ≥ 10 out of 27 points of PHQ-9 are the validated threshold for screening probable depression.
Statistical analysis
In this study, all analyses considered sample weights, clustering, and stratification to generate nationally representative estimates, acknowledging the complex sampling design of NHANES. All reported percentages are weighted. The NHANES recommended “WTMEC2YR” weight was utilized to account for the planned oversampling of specific groups in this study. Baseline characteristics were compared using the Chi-square test for categorical variables and ANOVA for continuous variables. Survey-weighted multivariable Cox proportional hazards regression models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations of LE8 scores with risks of all-cause mortality and CVD mortality. Model 1 was not adjusted for any covariates. Model 2 was adjusted for age (continuous, years), gender, ethnicity, education levels, marital status, and poverty impact ratio (PIR). Model 3 further incorporated drink history, depression, and cancer history. Trend tests were performed using linear regression by entering the median value of each subgroup of LE8 score as a continuous variable in the models. Sub-analyses were conducted to examine different categories of CVD, with the analysis stratified based on specific CVD conditions, including CHF, CHD, angina pectoris, heart attack, or stroke. The objective was to ascertain potential variations in the influence of LE8 on mortality across diverse cardiovascular conditions.
To investigate dose–response relationships and associations between the LE8 scores and both all-cause mortality and CVD mortality, the study employed survey-weighted multivariable Cox proportional hazards regression models with restricted cubic spline (RCS). The RCS utilized three knots at percentiles 25, 50, and 75. The LE8 scores were positioned on the horizontal axis, while the HR values with 95% CIs were plotted on the vertical coordinate. The RCS model was adjusted for age, gender, race, marital status, education, PIR, drinking history, depression, and cancer history. The cut-off value on the RCS curve where the HR value equaled 1 was considered. Nonlinearity assessments were conducted using the likelihood ratio test, P < 0.05 indicating a nonlinear dose–response relationship. Statistical tests were 2-sided, and statistical significance was set at P < 0.05. All analyses were performed using SAS version 9.4 (SAS Institute Inc.) and using the “SURVEY” procedures with R software, version 4.2.4 (R Core Team, Vienna, Austria).
Ethics approval and consent to participate
NHANES is conducted by the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics (NCHS). The NCHS Research Ethics Review Committee reviewed and approved the NHANES study protocol. All participants signed written informed consent.
Results
Characteristics of the participants
The baseline characteristics of the study population were presented in Table 1, stratified by the LE8 score. The study included 2164 participants with CVD, aged between 20 and 80 years (weighted mean [SE] age, 61.47 [0.34] years; 57.21% male). The average total LE8 score was 64.97 [0.54]. Over the follow-up period, 499 participants (19.19%) died, with 350 deaths attributed to CVD. A comparison between participants with low and high LE8 scores revealed that those with higher LE8 scores were older, more likely to be male, had higher education levels, and exhibited lower rates of both all-cause mortality and CVD mortality.
Association of LE8 with all-cause and CVD mortality
In all three models, each increase of 10 points in LE8 scores was associated with a significant reduction in all-cause mortality and CVD mortality. In the unadjusted model 1, participants with higher LE8 scores exhibited significantly lower all-cause mortality (HR 0.48, 95% CI 0.32–0.73, P < 0.001) and CVD mortality (HR 0.55, 95% CI 0.33–0.92, P = 0.023). After adjusting for age, gender, race, marital status, education level, and PIR, individuals with high LE8 scores showed a substantial reduction in all-cause mortality (HR 0.33, 95% CI 0.22–0.49, P < 0.001) and CVD mortality (HR 0.38, 95% CI 0.23–0.64, P < 0.001)in Model2, while those with moderate LE8 scores also exhibited a lower risk in all-cause mortality (HR 0.57, 95% CI 0.42–0.76, P < 0.001) and CVD mortality (HR 0.67, 95% CI 0.47–0.97, P = 0.035) compared to those with low LE8 scores among participants with CVD. Further adjustments in model 3, including variables cancer history, drink status, and depression, maintained the association, with high LE8 scores associated with a decreased risk of all-cause mortality (HR 0.34, 95% CI 0.22–0.51, P < 0.001) and moderate LE8 scores associated with a reduced risk (HR 0.57, 95% CI 0.43–0.77, P < 0.001) compared to low LE8 scores. For CVD mortality, participants with high LE8 scores had a significantly lower risk (HR 0.40, 95% CI 0.23–0.68, P < 0.001) compared to those with low LE8 scores, as shown in Table 2.
Supplementary Tables S2 to S6 present detailed insights into the specific patterns of all-cause mortality and CVD mortality among patients with different types of CVD history. An increase of 10 points in the LE8 scores consistently correlates with a lower risk of all-cause mortality across various subgroups, including those with CHF, CHD, angina pectoris, heart attack, and stroke. The findings outlined in Supplementary Table S7 indicate a significant reduction in both all-cause mortality and CVD mortality with higher diet scores, physical activity scores, nicotine exposure scores, and overall health behavior.
Trend analysis and dose–response relationships
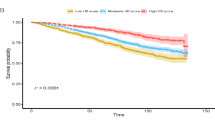
The trend analysis demonstrated a significant association between the LE8 score in Table 2, all-cause mortality (P for trend < 0.001), and CVD mortality (P for trend = 0.006) in the initial model. This association persisted in all-cause mortality (P for trend < 0.001) and CVD mortality (P for trend < 0.001) even after adjusting for age, gender, race, marital status, education level, and PIR. Further adjustments in model 3, incorporating variables such as cancer history, drink status, and depression, maintained this association in both all-cause mortality (P for trend < 0.001) and CVD mortality (P for trend < 0.001). The dose–response analyses unveiled a nonlinear association between LE8 scores and both all-cause mortality (P < 0.001, Fig. 2a) and CVD mortality (P < 0.001, Fig. 2b) among participants with CVD. A discernible threshold for a significant reduction in the risk of both all-cause mortality and CVD mortality was identified at an LE8 score of 63.75.
Association of Life’s Essential 8 score with mortality in a restricted cubic spline model. Multivariable adjusted odds ratios (red solid line) with 95% confidence interval (pink shaded area) for the association of Life’s Essential 8 score with all-cause mortality. Adjusted for age (continuous, years), gender, ethnicity, education levels, marital status, PIR, drink history, depression, and cancer history. (a) With all-cause mortality; (b) with CVD mortality.
Discussion
This study provides valuable insights into the relationship between LE8 scores and mortality risks among participants with CVD, utilizing data from the NHANES. Over the follow-up period, a total of 499 (19.19%) deaths occurred, including 350 deaths attributed to CVD. Examining the association between LE8 scores and mortality, after adjusting for various confounders, including age, gender, race, marital status, education level, income, cancer history, alcohol consumption, and depression, the inverse association persisted. High LE8 scores were associated with a substantially lower risk of all-cause mortality (HR 0.34, 95% CI 0.22–0.51) and CVD mortality (HR 0.40, 95% CI 0.23–0.68) compared to low LE8 scores. The trend analysis and the dose–response analysis confirmed a consistent reduction in both all-cause and CVD mortality risks with increasing LE8 scores. These results underscore the critical role of LE8 score in mitigating mortality risks among individuals with CVD.
This study represents a pioneering investigation as the inaugural exploration into the associations of a novel metric for assessing LE8 scores with mortality specifically within the demographic of US adults with CVD. While antecedent research has probed the relationship between LE8 and mortality in the whole US adults13,14. Our findings are consistent with several other studies that have highlighted the significant associations between dietary patterns, physical activity levels, and overall health behavior with both all-cause and CVD mortality. A Prospective Urban Rural Epidemiology study revealed that healthy diet score that is associated with lower CVD (HR 0.82; 0.75–0.91) and mortality (HR 0.70; 0.63–0.77) in all world regions15. In a Spanish and US cohort, found the Mediterranean diet, and predicts future CVD risk independent of traditional risk factors16. In the influential Nurses' Health Study, focusing on a substantial cohort of nurses and healthcare professionals, emphasized the role of diet, exercise, and other lifestyle behaviors in shaping CVH outcomes, underlining the pivotal importance of lifestyle modifications in mitigating cardiovascular risks17. These findings underscore the critical significance of LE8 in foreseeing and alleviating mortality risks among individuals with pre-existing cardiovascular conditions. This contribution adds substantial value to the ongoing discussions on lifestyle modifications and their repercussions on CVH outcomes. Our study introduces a novel and comprehensive perspective by focusing specifically on the unique context of the CVD population.
The intricate connections between LE8 and mortality may suggest potential mechanistic insights into the attenuation of chronic inflammation, a recognized driver of CVD. In the context of CVD mortality, chronic inflammation plays a pivotal role in influencing disease severity and prognostic outcomes18. Existing scientific evidence consistently links elevated levels of inflammatory markers19, such as C-reactive protein and interleukin-620,21, with an increased risk of adverse cardiovascular events and mortality. Chronic inflammation contributes to the formation, instability, and rupture of atherosclerotic plaques22, leading to acute cardiovascular events that significantly contribute to CVD mortality. Furthermore, chronic inflammation has systemic effects, impacting various physiological processes associated with heightened mortality risk23. The newly introduced and comprehensive LE8 score, encompassing a healthful diet24, routine physical activity25,26, avoidance of tobacco27, weight control and establishment of healthy sleep patterns28,29, emerges as a crucial tool in suppressing inflammatory cascades. The LE8 score aim not only to quell inflammation but also to enhance cardiovascular outcomes, thereby reducing mortality risks in individuals navigating the complexities of cardiovascular conditions. In summary, the LE8 score influence inflammation through lifestyle modifications targeting dietary, physical, and behavioral factors. By promoting an anti-inflammatory environment, LE8 contributes to CVH and potentially protects against the development and progression of CVD. Vigilant monitoring of LE8 components is imperative for effective secondary prevention of CVD. Consistent tracking and management of factors such as blood pressure, cholesterol levels, blood sugar, physical activity, diet, weight, sleep and smoking cessation significantly contribute to reducing the risk of recurrent cardiovascular events and improving long-term outcomes in individuals with CVD30.
Strengths and limitations
The study exhibits notable strengths and some limitations, contributing to a more comprehensive understanding of our results. Firstly, the utilization of NHANES data enhances the generalizability of our findings, augmenting their broader applicability. Secondly, the introduction of the novel LE8 scoring system for assessing the relationship between all-cause mortality and CVD mortality among participants with CVD adds depth to our investigation. This innovation not only facilitates a more comprehensive evaluation of these critical parameters but also sets a foundation for understand how LE8 influences mortality in the CVD population. However, several limitations should be acknowledged. The reliance on self-reported lifestyle factors, such as diet and sleep duration, in the NHANES dataset introduces inherent measurement errors. Moreover, information on the LE8 was only available at baseline, and the lack of information on changes in LE8 during the follow-up period limits our ability to consider potential variations over time. The inclusion of only White, Black, and Mexican participants in racial/ethnic group analyses may limit the generalizability of findings to other groups due to sample size constraints. We controlled for several potential confounders, the nature of the cross-sectional study design precludes us from concluding causality and temporality between LE8 and all-cause mortality and CVD mortality risk. Finally, based on Table S10, the impact of confounding factors affecting both the response to the LE8 questionnaire and the outcome appears to be present. This additional information will help us limit the outcomes to the specific population of CVD patients with LE8 scores, rather than generalizing to the entire population of CVD patients. Therefore, we specify that our research results pertain to this specific population rather than a nationally representative sample, but they still have the novelty and innovativeness to address issues about the prevention and treatment of CVD in patients.
Conclusions
The findings highlight a positive correlation between LE8 score and reduced mortality among individuals with CVD. Implementing comprehensive programs that prioritize achieving higher LE8 scores can play a pivotal role in alleviating the burden of cardiovascular disease and improving CVH outcomes.
Data availability
The National Health and Nutrition Examination Survey dataset is publicly available at the National Center for Health Statistics of the Center for Disease Control and Prevention (https://www.cdc.gov/nchs/nhanes/index.htm).
References
Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England). 392, 1736–1788. https://doi.org/10.1016/s0140-6736(18)32203-7.
Mokdad, A. H. et al. The State of US Health, 1990–2016: Burden of diseases, injuries, and risk factors among US states. JAMA 319, 1444–1472. https://doi.org/10.1001/jama.2018.0158 (2018).
QuickStats: Age-adjusted death rates* from heart disease(†) among adults aged 45-64 years, by urbanization level(§) and sex—National vital statistics system, United States, 2019. MMWR. Morb. Mortal. Wkly. Rep. 70, 1621. https://doi.org/10.15585/mmwr.mm7046a8.
Mohebi, R. et al. Cardiovascular disease projections in the United States based on the 2020 census estimates. J. Am. Coll. Cardiol. 80, 565–578. https://doi.org/10.1016/j.jacc.2022.05.033 (2022).
Pedamallu, H., Zmora, R., Perak, A. M. & Allen, N. B. Life course cardiovascular health: Risk factors, outcomes, and interventions. Circ. Res. 132, 1570–1583. https://doi.org/10.1161/circresaha.123.321998 (2023).
Lloyd-Jones, D. M. et al. Status of cardiovascular health in US adults and children using the American Heart Association’s new “Life’s Essential 8” metrics: Prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013 through 2018. Circulation 146, 822–835. https://doi.org/10.1161/circulationaha.122.060911 (2022).
Ma, H. et al. Cardiovascular health and life expectancy among adults in the United States. Circulation 147, 1137–1146. https://doi.org/10.1161/circulationaha.122.062457 (2023).
Yi, J., Wang, L., Guo, X. & Ren, X. Association of Life’s Essential 8 with all-cause and cardiovascular mortality among US adults: A prospective cohort study from the NHANES 2005–2014. Nutr. Metab. Cardiovasc. Dis. NMCD 33, 1134–1143. https://doi.org/10.1016/j.numecd.2023.01.021 (2023).
Li, C. et al. Using the new “Life’s Essential 8” metrics to evaluate trends in cardiovascular health among US adults from 2005 to 2018: Analysis of serial cross-sectional studies. JMIR Public Health Surveill. 9, e45521. https://doi.org/10.2196/45521 (2023).
Krebs-Smith, S. M. et al. Update of the healthy eating index: HEI-2015. J. Acad. Nutr. Diet. 118, 1591–1602. https://doi.org/10.1016/j.jand.2018.05.021 (2018).
Zhao, G. et al. Leisure-time aerobic physical activity, muscle-strengthening activity and mortality risks among US adults: The NHANES linked mortality study. Br. J. Sports Med. 48, 244–249. https://doi.org/10.1136/bjsports-2013-092731 (2013).
Tsai, J. et al. Exposure to secondhand smoke among nonsmokers—United States, 1988–2014. MMWR. Morb. Mortal. Wkly. Rep. 67, 1342–1346. https://doi.org/10.15585/mmwr.mm6748a3 (2018).
Howard, G. et al. Comparative discrimination of Life’s Simple 7 and Life’s Essential 8 to stratify cardiovascular risk: Is the added complexity worth it?. Circulation https://doi.org/10.1161/circulationaha.123.065472 (2024).
Yuan, Y. E. et al. Association between Life’s Simple 7 and biomarkers of cardiovascular disease: Aldosterone, Interleukin-6, C-reactive protein. J. Am. Heart Assoc. 12, e028718. https://doi.org/10.1161/jaha.122.028718 (2023).
Mente, A. et al. Diet, cardiovascular disease, and mortality in 80 countries. Eur. Heart J. 44, 2560–2579. https://doi.org/10.1093/eurheartj/ehad269 (2023).
Li, J. et al. The Mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur. Heart J. 41, 2645–2656. https://doi.org/10.1093/eurheartj/ehaa209 (2020).
Glenn, A. J. et al. Portfolio diet score and risk of cardiovascular disease: Findings from 3 prospective cohort studies. Circulation https://doi.org/10.1161/circulationaha.123.065551 (2023).
Ridker, P. M. et al. Inflammation and cholesterol as predictors of cardiovascular events among 13970 contemporary high-risk patients with statin intolerance. Circulation https://doi.org/10.1161/circulationaha.123.066213 (2024).
Mangge, H. & Almer, G. Immune-mediated inflammation in vulnerable atherosclerotic plaques. Molecules (Basel, Switzerland) https://doi.org/10.3390/molecules24173072 (2019).
Opotowsky, A. R. et al. Prospective cohort study of C-reactive protein as a predictor of clinical events in adults with congenital heart disease: Results of the Boston adult congenital heart disease biobank. Eur. Heart J. 39, 3253–3261. https://doi.org/10.1093/eurheartj/ehy362 (2018).
Ridker, P. M. et al. IL-6 inhibition with ziltivekimab in patients at high atherosclerotic risk (RESCUE): a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet (London, England) 397, 2060–2069. https://doi.org/10.1016/s0140-6736(21)00520-1 (2021).
Tomas, L. et al. Altered metabolism distinguishes high-risk from stable carotid atherosclerotic plaques. Eur. Heart J. 39, 2301–2310. https://doi.org/10.1093/eurheartj/ehy124 (2018).
Möhlenkamp, S. et al. Quantification of coronary atherosclerosis and inflammation to predict coronary events and all-cause mortality. J. Am. Coll. Cardiol. 57, 1455–1464. https://doi.org/10.1016/j.jacc.2010.10.043 (2011).
Hill, E. B., Cubellis, L. T., Wexler, R. K., Taylor, C. A. & Spees, C. K. Differences in adherence to American Heart Association’s Life’s Essential 8, diet quality, and weight loss strategies between those with and without recent clinically significant weight loss in a nationally representative sample of US adults. J. Am. Heart Assoc. https://doi.org/10.1161/jaha.122.026777 (2023).
Swain, C. T. V. et al. Television viewing time and all-cause mortality: Interactions with BMI, physical activity, smoking, and dietary factors. Int. J. Behav. Nutr. Phys. Act. 19, 30. https://doi.org/10.1186/s12966-022-01273-5 (2022).
Bryant, R. A. et al. Augmenting trauma-focused psychotherapy for post-traumatic stress disorder with brief aerobic exercise in Australia: A randomised clinical trial. Lancet Psychiatry https://doi.org/10.1016/s2215-0366(22)00368-6 (2023).
Mori, K. M. et al. Lung mitochondrial DNA copy number, inflammatory biomarkers, gene transcription and gene methylation in vapers and smokers. EBioMedicine 85, 104301. https://doi.org/10.1016/j.ebiom.2022.104301 (2022).
Wen, X. et al. Signaling pathways in obesity: Mechanisms and therapeutic interventions. Signal Transduct. Target. Ther. 7, 298. https://doi.org/10.1038/s41392-022-01149-x (2022).
Freeman, D., Sheaves, B., Waite, F., Harvey, A. G. & Harrison, P. J. Sleep disturbance and psychiatric disorders. Lancet Psychiatry 7, 628–637. https://doi.org/10.1016/s2215-0366(20)30136-x (2020).
Goldfarb, M. et al. Severe Mental illness and cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 80, 918–933. https://doi.org/10.1016/j.jacc.2022.06.017 (2022).
Acknowledgements
We thank the National Health and Nutrition Examination Survey participants and staff and the National Center for Health Statistics for their valuable contributions.
Author information
Authors and Affiliations
Contributions
Y.Y.: conceptualization, methodology, data curation, formal analysis, writing—original draft preparation, writing—review and editing; Y.W.: data curation, formal analysis, writing—review and editing; Y.M.: methodology, writing—review and editing; F.Z.: data curation; M.Z.: data curation; P.M.: data curation; T.Y.: data curation; X.J.: data curation; R.C.: supervision; writing—review and editing; funding acquisition; W.Z.: conceptualization, supervision, project administration, writing—review and editing; funding acquisition. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, Y., Wang, Y., Mao, Y. et al. Association of life’s essential 8 with mortality among the individuals with cardiovascular disease. Sci Rep 14, 18520 (2024). https://doi.org/10.1038/s41598-024-69603-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69603-0
- Springer Nature Limited