Abstract
Background
Patients with heart failure with preserved ejection fraction (HFpEF) have a low functional status, which in turn is a risk factor for hospital admission and an important predictor of survival in HFpEF. HFpFE is a heterogeneous syndrome and recent studies have suggested an important role for careful, pathophysiological-based phenotyping to improve patient characterization. Cardiac rehabilitation has proven to be a useful tool in the framework of secondary prevention in patients with HFpEF. Facilitating decision-making and implementing cardiac rehabilitation programs is a challenge in public health systems for HFpEF management. The FUNNEL + study proposes to evaluate the efficacy of an exercise and education-based cardiac rehabilitation program on biomechanical, physiological, and imaging biomarkers in patients with HFpEF.
Methods
A randomised crossover clinical trial is presented among people older than 70 years with a diagnosis of HFpEF. The experimental group will receive a cardiac rehabilitation intervention for 12 weeks. Participants in the control group will receive one educational session per week for 12 weeks on HFpEF complications, functional decline, and healthy lifestyle habits. VO2peak is the primary outcome. Biomechanical, imaging and physiological biomarkers will be assessed as secondary outcomes. Outcomes will be assessed at baseline, 12 weeks, and 24 weeks.
Discussion
Identifying objective functional parameters indicative of HFpEF and the subsequent development of functional level stratification based on functional impairment ("biomechanical phenotypes") may help clinicians identify cardiac rehabilitation responders and non-responders and make future clinical decisions. In this way, future pharmacological and non-pharmacological interventions, such as exercise, could be improved and tailored to improve quality of life and prognosis and reducing patients' hospital readmissions, thereby reducing healthcare costs.
Trial registration
NCT05393362 (Clinicaltrials.gov).
Similar content being viewed by others
Background
Cardiovascular diseases continued to be the principal cause of disability-adjusted life years (DALYs) due to non-communicable diseases (NCDs) and the leading cause of death, especially in countries with a higher sociodemographic index and longer life expectancy [1,2,3]. Within cardiovascular diseases, it has been estimated that heart failure (HF) has a prevalence of approximately 2% to 3%, arising in more than 23 million people worldwide [4, 5]. The incidence and prevalence of HF are increasing due to the ageing of the world population, with patients over 75 years of age having the highest risk of developing this condition [4, 6,7,8]. Within the complex entity of HF, three subtypes have been differentiated: HF with preserved ejection fraction (HFpEF), HF with mildly reduced ejection fraction (HFmrEF), and HF with reduced ejection fraction (HFrEF). These three diagnostic entities coexist in the population with HF, the most prevalent being HFpEF, with prevalence rates of 50%. HF constitutes the essential hospital diagnosis in older adults, being the leading cause of hospital admissions for people over 65 and contributing to the increase in healthcare costs in Western societies [4,5,6]. Functional status is a potentially modifiable risk factor for hospital admission and appears to be an important discriminator between the different HF subtypes [9].
HFpEF patients present distinctive functional characteristics, such as reduced aerobic capacity, decreased muscle strength in the lower extremities, low weekly physical activity, and exercise intolerance, accompanied by fatigue and dyspnoea symptoms [10,11,12,13,14,15]. These functional characteristics cause HF patients to show impaired functional abilities, experience impaired ability to perform activities of daily living, and suffer reduced quality of life [10, 12, 15]. Furthermore, it has been shown that patients with chronic HF present some changes in their gait pattern, with a lower gait speed than healthy subjects of the same age [16]. While gait speed is independently associated with survival, death, and hospitalisation in HF patients [8, 9, 17], maximal aerobic capacity has been inversely correlated with the severity of HF and directly related to prognosis and survival life expectancy [11, 12, 18, 19]. Similarly, lower extremity skeletal muscle mass and strength could predict long-term survival in patients with HF [12, 20].
When evaluating functional parameters in patients with HF, maximal oxygen consumption (VO2max) obtained from a cardiopulmonary exercise test (CPET) is considered the Gold Standard measure of cardiovascular functional capacity. Some functional tests have been used in clinical practice, such as the 6-min walk test (6MWT), which indirectly measures cardiovascular functional ability. Strength could also be assessed using the one repetition maximum (1RM) test, handgrip strength measurement (HGS), or the Short Physical Performance Battery (SPPB), as a valuable and indirect measure of this capacity [11]. Most geriatric populations present a high degree of fragility and dependence from the physical, cognitive, and psychological points of view, so their evaluation is essential [21]. SPPB and the Timed Up and Go (TUG) test have been established as practical clinical tests to assess frailty as a phenotype in HF patients [22,23,24,25].
By assessing the functional parameters used in the clinic, it has been possible to evaluate the effectiveness of Cardiac Rehabilitation (CR) in improving quality of life, functional capacity, exercise performance, and HF-related hospitalisations [26, 27]. CR is a multidimensional treatment designed to promote lifestyle changes and physical activity, optimise medical treatment, control risk factors, and address social and psychological problems following the development of heart disease [28]. CR programmes have a strong recommendation (Class 1A) in major HF practice guidelines, as it is considered a cost-effective intervention in HF, reducing recurrent hospitalisations and healthcare expenditure [7, 26, 29]. Benefits have also been shown on anthropometric, blood markers and physiological (VO2max) related outcomes, and cardiac imaging structural biomarkers such as ventricular ejection fraction [29,30,31].
Biomechanical biomarker assessment is possible through the parameterisation of human movement [32]. Inertial sensors have proven to be an accurate and reliable method for biomechanical human motion analysis and are used as a reference for validating motion capture instruments [32,33,34,35]. Currently, a good correlation between measurements obtained by inertial sensors and depth chambers has been demonstrated in the parameterisation of functional tests [34]. Biomechanical biomarkers could identify normal and pathological movements, the degree of impairment, the planning of rehabilitation strategies, and the evaluation of the effect of various interventions [32]. Therefore, it could be interesting to identify objective functional parameters affected in patients with HF, help stratify them based on different levels of functional impairment and identify those patients who are responders and non-responders to CR programmes. However, no biomechanical biomarkers have been assessed as an objective measure of the functionality of HF patients. Thus, the benefits of CR programmes on these biomechanical biomarkers have not been determined.
Facilitating decision-making and implementing CR programmes is a challenge in public health systems for HF management. This study proposes evaluating the efficacy of the CR programmes through a randomised clinical trial (RCT) on biomechanical, physiological, and imaging biomarkers in HF patients. In addition, it aims to validate the biomechanical analysis obtained using motion capture systems to assess objective functionality in elderly patients with HFpEF.
Methods
Trial design
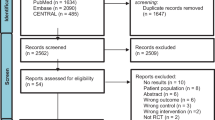
This study protocol followed the SPIRIT 2013 Recommendations [36] during its development. More details are shown in Additional file 1. The present study shows the proposed two-arm crossover RCT comparing an exercise-based CR programme with education in patients with HF. Patients will be randomised into two groups by simple randomisation using a random number generator on the computer. The study design is shown in Fig. 1. The RCT is based on work within the Biomedical Research Institute of Malaga (IBIMA) between the Internal Medicine Unit and the Cardiology Unit of the Regional University Hospital of Malaga (HRUM), together with the support of the University of Malaga (Malaga, Spain). This project has been submitted to the Malaga Provincial Ethics Committee (2198-N-22).
Study duration and timing
Recruitment and eligibility assessment of participants from the Internal-Cardiac Unit will be performed first. Patients who meet the eligibility criteria and wish to participate in the study will be required to provide written informed consent to participate in the study. Once the informed consent is signed, study variables will be collected. After baseline assessment, patients will be randomised to the control (Education) or intervention (CR) group. The interventions will have an estimated duration of 3 months. Patients will be assessed right after the intervention (follow-up/analysis 1) and at six months (follow-up/analysis 2). This way, depending on the group allocation, the different intervention groups will be reassigned. Data collection is expected to be completed about 1 year after the beginning of the study. The timeline of the study is represented in Fig. 2.
Recruitment and inclusion
They will be patients over 70 years of age with a diagnosis of HFpEF, who are clinically stable, and who are being followed in this unit. A clinically stable patient is defined as a patient who has not been hospitalised for HF decompensation, has not undergone treatment modification, and has a stable NYHA grade 2–3 in the last 3 months. The diagnosis of HF and optimal treatment will be established according to Spanish and European HF clinical practice guidelines [29, 37]. Inclusion and exclusion criteria are detailed in Table 1.
Interventions
Both the Education and CR interventions will take place in the internal medicine unit of the HRUM. Medical and nursing care will be available during Education and CR sessions to ensure the safety of participants Study collaborators will be instructed to record any incidents related to possible adverse events that may be associated with the interventions.
Experimental group: CR program
The CR programme will consist of aerobic and strength exercise sessions. Exercises will be individualised after assessment of short (strength exercise) and long (aerobic exercise) efforts. They will be performed two days a week and at least 48 h between sessions. Progression will consider a clinical criterion, determined by the absence of HF symptoms at the current intensity, and a time criterion in which, as long as the clinical criterion is met, the intensity will be increased every two to three weeks. The progression in aerobic training intensity is established based on Skinner's three-phase model [38] and the recommendations of current European cardiac rehabilitation guidelines [29]. The structure of the standard session, the criteria for progression in both aerobic and strength training, the phases of training, the periodisation of the programme, and the monitoring variables in the session can be found in detail in Additional file 2.
In addition, embedded in the exercise intervention, education on healthy lifestyle habits will be needed. A series of competencies in healthy lifestyle habits relevant to the population with HF will be established, which will be evaluated using a questionnaire with an evaluation rubric format for each of the competencies. The competencies will be evaluated during the training sessions in an informal way. Depending on the results obtained, they will be reinforced by strengthening unconsolidated skills using specific educational material.
Control group: Education
The control group will receive personalized educational embedded in the program for twelve weeks on HF complications, functional decline, and healthy lifestyle habits. The format of the sessions will be in the form of face-to-face or online master classes, depending on the availability of the participants, in which the active participation of both volunteers and their relatives/caregivers will be encouraged.
Criteria for dropout
The criteria for discontinuing the assigned interventions are:
-
1.
The patient's willingness to discontinue participation in the study.
-
2.
Worsening prognosis that precludes continuation.
-
3.
The presence of events during the sessions jeopardizes the patient's safety.
-
4.
Absence from training sessions, in the case of the experimental group for unjustified reasons (compliance below 60%).
Study outcomes
Anthropometric and demographic variables will be collected for descriptive analysis only in the first evaluation, including age, gender, weight, height, and body mass index. Participants must complete different questionnaires that will be conducted at each measurement time. The summary of the outcome variables can be found in Additional file 3.
Primary outcome measures
As primary variables, one has been chosen for each of the three domains that are going to be evaluated.
Biomechanical biomarkers
The kinematic parameters during the activity are derived by using inertial measurement units (IMU). IMUs have been shown to have good psychometric properties to estimate kinematic parameters during the performance of functional tests. Kinematic parameters have been seen as objective parameters of functional capacity. It has been shown to have high specificity and sensitivity for tests such as the 6MWT in patients with HF.
Physiological biomarkers
Peak oxygen uptake (VO2peak), in maximal exercise tests, coincides with maximal oxygen consumption (VO2max). It is the most objective parameter of functional capacity and a gold standard indicator of maximal cardiorespiratory fitness. It is the maximum O2 extracted from inhaled air during pulmonary ventilation. It is usually expressed in milliliters per minute (ml/min) or milliliters per kilogram per minute(ml/kg/min). It reflects the severity of the disease in patients with HF [39, 40] and is a significant predictor of mortality in HF patients [41].
Imaging biomarkers
Assessment of ultrasonic body composition parameters can be performed using ultrasonography (US). This technique is reliable and valid for evaluating the number of pennate muscles in older adults, such as the quadriceps femoris (QF) muscle. US has shown reasonable validity in estimating muscle mass compared to MRI and CT. US could have the potential for use in clinical practice for the detection of sarcopenia and to assess body composition or muscle architecture.
Secondary outcome measures
For the secondary variables, we have chosen to describe the instruments used to capture the different variables. The variables assigned to each instrument are well-detailed in Additional file 3.
Objective outcome variables
Physiological biomarkers
Electrical impedance vector analysis (BIVA)
As a measure of body composition, electrical bioimpedance vector analysis (BIVA) has been validated. It has recently been shown to provide information on the overall assessment, management, and prognostic evaluation of HF patients [42, 43]. All measurements derived from BIVA are characterised by excellent test–retest reliability [44]. The BIO 101 BIVA®PRO bioimpedance device (BIA101 Akern, 50,065 Pontassieve FI, Italy) will be used.
Respiratory function tests (RFT)
To measure the patient's respiratory volumes and flows, a spirometry device (Spiro USB, Micro Medical, Kent, UK) [45] and a respiratory pressure meter (MicroRPM, Micromedical, Kent, UK) [46] will be used to test the lung function [46,47,48]. The repeatability of spirometry measurements [49] and the reliability of the MicroRPM device for MIP and MEP [50] variables have been reported. The recommendations of the ARTP statement on pulmonary function tests in 2020 will be followed [51].
High-density electromyography (HD-sEMG)
The high-density electromyography (HD-sEMG) device will be used in conjunction with the S-type load cell (Biometrics Ltd., Newport, UK) to measure the electrical activity of the tibialis anterior (TA) muscle and generate force output. It is a reliable method for assessing the characteristics of the motor unit in different populations and locations [52,53,54,55]. The signal produced will be recorded using the external analog-to-digital signal converter Sessantaquattro (64-channel EMG amplifier; OT Bioelettronica, Turin, Italy), and will be processed using OT Biolab + software (v.1.2.1, OT Bioelettronica, Turin, Italy) [56].
Functional and dynamometric tests (FUN test)
Patients will undergo the Short Physical Performance Battery (SPPB) [57,58,59], Timed Up and Go Test (TUG) [57, 60], and Six-Minute Walk Test (6-MWT) [58, 59, 61, 62]. A digital hand dynamometer will assess isometric quadriceps extension strength (J Tech Medical, Powertrack II Commander, Salt Lake City, UT) [63]. Grip strength will be evaluated using the Jamar Hydraulic, model SH5001 (Lafayette Instrument, Lafayette, USA). Manual dynamometry has proven to be a valid and reliable instrument to measure isometric strength in different populations and locations [64, 65].
Cardiopulmonary Exercise Tests (CPET)
Cardiopulmonary exercise testing (CET) will be performed using a portable Cortex Metamax 3B (MM3B) [66] automated gas analysis system[ref]. Primarily to obtain VO2peak, secondary to collect variables derived from breath-by-breath respiratory gas analysis. The self-limited ramped exercise protocol on an ergometer bike is generally well tolerated by patients with HF [67]. The feasibility and safety of the ramped exercise protocol have been demonstrated [68].
Blood biomarkers
The relevant physician will extract biomarkers in the blood through blood analysis (blood, plasma, and serum). The central blood values of interest in the HF population will be requested.
Biomechanical biomarkers
During functional tests, biomechanical parameters will be assessed using the inertial measurement unit of the Shimmer3 [69] and the structured light-based depth camera manufactured by Xbox360, the Kinect 2.0 sensor [35, 70, 71].
Imaging biomarkers
Standard two-dimensional resting echocardiography (ultrasound) will be used to obtain cardiac imaging variables. Simpson's biplane method will be used in an apical four-chamber view to estimate LVEF (%) [29, 31]. A B-mode ultrasound (SonoSite 180 Plus, SonoSite Japan, Tokyo, Japan) and linear transducer (5–10 MHz) [72] will be used to collect skeletal and pulmonary imaging variables.
Self-reported outcome variables
The abbreviated comprehensive assessment scale (aCGA) [73, 74], the SARC-F questionnaire [75, 76], the Kansas City questionnaire (KCCQ) [77], and the Mini Nutritional Assessment survey (MNA®) [78] are validated and, will be used to obtain the outcome variables self-reported.
Exploratory outcomes
During the sessions, the total exercise time and the exercise intensity reached by the patients during the sessions will be collected. In addition, adverse events during the exercise program will be compiled.
The cost of the CR per session will be estimated from the material required, the clinician's time, and the indirect costs.
Data management
The data will be recorded and stored in database files on a password-protected flash drive. No identifying information is registered in the database, but an identification number is attributed to each patient. This number is associated with the patient's medical record number in a separate table accessible only to FUNNEL + researchers on a corporate computer. All patient information will be pseudonymised and only researchers will have access to the identification data.
Blinding
The researchers conducting the assessments and data analysis will be blinded so that they do not know to which group each patient belongs. Blinding the subjects is unfeasible because of this type of intervention.
Sample size calculation
The sample size was calculated using G Power 3.1.9.2 software (University of Düsseldorf, Germany). Based on an expected difference in VO2max increase of 3.0/ml/kg/min in the intervention group and 0.6 ml/kg/min in the control group (based on the result of the EUCaRE Study, Prescott et al. 2020 PMID 32102550 [48]). Assuming a statistical power of 80% and an alpha error of 0.05, the required sample size is 55 patients per arm and carries a loss rate of 15%, and this would make a total of 126 (63 per arm).
Statistical analysis
Data sets will be processed using the Statistical Package for the Social Sciences (SPSS) for Windows (version 19.0, SPSS Inc., Chicago, IL, USA). Qualitative variables will be described by absolute and relative frequency (percentage). Quantitative variables shall be presented by the mean and standard deviation if the data follow a normal distribution or by the maximum, minimum, and three quartiles if the data do not follow such a distribution. The Shapiro–Wilk test will be used to analyse the normal distribution of the data (p > 0.05). The difference in means between the two groups will be obtained using Pearson's Chi-square test (× 2) for qualitative variables. To express the differences in means in the quantitative variables between the two groups, the bivariate analysis will be used using the parametric Student's t-test for independent samples in the case of normal data distribution, or the non-parametric Mann–Whitney U test, if there is no normal distribution of the data. The degree of statistical significance shall be set at a p-value < 0.05. 95% confidence intervals (CI) will be calculated for the mean differences between the study groups.
Dissemination
The trial findings will be submitted for publication in an unrestricted peer-reviewed clinical journal and reported at pertinent conferences.
Discussion
The aim of this study is to evaluate the efficacy of CR programs through a randomized clinical trial (RCT) on biomechanical, physiological and imaging biomarkers in patients with HFpEF.
Previous cross-sectional studies [79,80,81] have assessed objective functional parameters, providing interesting results that have allowed the estimation of VO2peak and objective measurement of dyspnoea and fatigue in patients with HFpEF.
Although the term HFpEF is used to describe a category of HF, there is great variability in the clinical presentation and progression of the disease in individual patients. For example, patients with HFpEF may present with symptoms such as dyspnoea, fatigue, peripheral oedema, and a wide variety of comorbidities, such as chronic kidney disease, hypertension, diabetes mellitus, and obesity, which can affect disease progression and response to treatment. Patients may require additional treatments to manage these conditions depending on the comorbidities present. Therefore, phenotyping of patients with HFpEF is essential to determine the best treatment strategy [82, 83].
Phenotyping refers to identifying subgroups of patients with common clinical and biological characteristics. In the case of HFpEF, phenotyping may help identify subgroups of patients with different causes, comorbidities, risk factors, and disease severity. Current literature describes the association of HFpEFF with diabetes mellitus, obesity, pulmonary disease, or frailty and proposes treatment strategies according to the different presentations [82, 83].
However, although the poor functional capacity of patients with HF, especially in HFpEF, is well known, no phenotypes describing the functional status of these patients for subsequent treatment prescription have been reported so far. Through the present study, we aim to identify objective functional parameters indicative of HF. The subsequent development of a functional level-based classification ("biomechanical phenotypes") may help clinicians identify CR responders and non-responders and thus make future clinical decisions (Fig. 3. Subtypes responder to the Funnel program). In this way, future pharmacological and non-pharmacological interventions, such as exercise, could be improved and tailored, improving quality of life and prognosis and reducing patients' hospital readmissions, thereby reducing healthcare costs.
Availability of data and materials
Data are accessible under justifiable request at https://riuma.uma.es/xmlui/.
Abbreviations
- aCGA:
-
Abbreviated Comprehensive Assessment Scale
- ARTP:
-
Association for Respiratory Technology and Physiology
- BIVA:
-
Electrical Bioimpedance Vector Analysis
- CPET:
-
Cardiopulmonary Exercise Test
- CR:
-
Cardiac Rehabilitation
- HD-sEMG:
-
High-Density Electromyography
- HGS:
-
Hand Grip Strength
- HF:
-
Heart Failure
- HFpEF:
-
Heart Failure With Preserved Ejection Fraction
- KCCQ:
-
Kansas City Questionnaire
- LVEF:
-
Left Ventricular Ejection Fraction
- MEP:
-
Maximum Expiratory Pressure
- MIP:
-
Maximum Inspiratory Pressure
- MMSA:
-
Mini-Mental State Examination
- MNA®:
-
Mini Nutritional Assessment survey
- NCDs:
-
Non-Communicable Diseases
- NYHA:
-
New York Heart Association
- SARC-F:
-
SARC-F questionnaire
- SPPB:
-
Short Physical Performance Battery
- SPSS:
-
Statistical Package for the Social Sciences
- TUG:
-
Timed Up and Go
- VO2max:
-
Maximal Oxygen Consumption
- VO2peak:
-
Peak Oxygen Uptake
- 1-RM:
-
One-Repetition Maximum
- 6-MWT:
-
Six-Minute Walk Test
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1260–344. https://doi.org/10.1016/S0140-6736(17)32130-X.
Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016 - PubMed. https://pubmed.ncbi.nlm.nih.gov/28919115/ (accessed 8 Mar 2023).
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41. https://doi.org/10.1038/nrcardio.2010.165.
Orso F, Fabbri G, Maggioni AP. Epidemiology of heart failure. Handb Exp Pharmacol. 2017;243:15–33. https://doi.org/10.1007/164_2016_74.
Dharmarajan K, Rich MW. Epidemiology, pathophysiology, and prognosis of heart failure in older adults. Heart Fail Clin. 2017;13:417–26. https://doi.org/10.1016/j.hfc.2017.02.001.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart association task force on practice guidelines. J Am Coll Cardiol. 2013;62:e147-239. https://doi.org/10.1016/j.jacc.2013.05.019.
Pulignano G, Del Sindaco D, Di Lenarda A, et al. Incremental value of gait speed in predicting prognosis of older adults with heart failure: insights From the IMAGE-HF study. JACC Heart Fail. 2016;4:289–98. https://doi.org/10.1016/j.jchf.2015.12.017.
Chaudhry SI, McAvay G, Chen S, et al. Risk factors for hospital admission among older persons with newly diagnosed heart failure: findings from the Cardiovascular Health Study. J Am Coll Cardiol. 2013;61:635–42. https://doi.org/10.1016/j.jacc.2012.11.027.
Fuentes-Abolafio IJ, Stubbs B, Pérez-Belmonte LM, et al. Physical functional performance and prognosis in patients with heart failure: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2020;20:512. https://doi.org/10.1186/s12872-020-01725-5.
Kaminsky LA, Tuttle MS. Functional assessment of heart failure patients. Heart Fail Clin. 2015;11:29–36. https://doi.org/10.1016/j.hfc.2014.08.002.
Gutekunst DJ. Isokinetic torque timing parameters and ceramides as markers of muscle dysfunction in systolic heart failure. J Cardiac Fail. 2016;22:356–7. https://doi.org/10.1016/j.cardfail.2016.03.018.
Watson RD, Gibbs CR, Lip GY. ABC of heart failure. Clinical features and complications BMJ. 2000;320:236–9. https://doi.org/10.1136/bmj.320.7229.236.
Barker J, Smith Byrne K, Doherty A, et al. Physical activity of UK adults with chronic disease: cross-sectional analysis of accelerometer-measured physical activity in 96 706 UK Biobank participants. Int J Epidemiol. 2019;48:1167–74. https://doi.org/10.1093/ije/dyy294.
Kinugawa S, Takada S, Matsushima S, et al. Skeletal muscle abnormalities in heart failure. Int Heart J. 2015;56:475–84. https://doi.org/10.1536/ihj.15-108.
Effect of walking speed in heart failure patients and heart transplant patients - Clinical Biomechanics. https://www.clinbiomech.com/article/S0268-0033(17)30019-0/fulltext (accessed 6 Jun 2022).
Lo AX, Donnelly JP, McGwin G, et al. Impact of gait speed and instrumental activities of daily living on all-cause mortality in adults ≥65 years with heart failure. Am J Cardiol. 2015;115:797–801. https://doi.org/10.1016/j.amjcard.2014.12.044.
Mancini DM, Eisen H, Kussmaul W, et al. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation. 1991;83:778–86. https://doi.org/10.1161/01.cir.83.3.778.
Myers J, Prakash M, Froelicher V, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. https://doi.org/10.1056/NEJMoa011858.
Hülsmann M, Quittan M, Berger R, et al. Muscle strength as a predictor of long-term survival in severe congestive heart failure. Eur J Heart Fail. 2004;6:101–7. https://doi.org/10.1016/j.ejheart.2003.07.008.
Altimir S, Lupón J, González B, et al. Sex and age differences in fragility in a heart failure population. Eur J Heart Fail. 2005;7:798–802. https://doi.org/10.1016/j.ejheart.2004.09.015.
Díez-Villanueva P, Arizá-Solé A, Vidán MT, et al. Recommendations of the geriatric cardiology section of the Spanish society of cardiology for the assessment of frailty in elderly patients with heart disease. Rev Esp Cardiol (Engl Ed). 2019;72:63–71. https://doi.org/10.1016/j.rec.2018.06.035.
Cabrero-García J, Muñoz-Mendoza CL, Cabañero-Martínez MJ, et al. Valores de referencia de la Short Physical Performance Battery para pacientes de 70 y más años en atención primaria de salud. Atención Primaria. 2012;44:540–8. https://doi.org/10.1016/j.aprim.2012.02.007.
Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85-94. https://doi.org/10.1093/geronj/49.2.m85.
Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–61. https://doi.org/10.1056/NEJM199503023320902.
Bozkurt B, Fonarow GC, Goldberg LR, et al. Cardiac rehabilitation for patients with heart failure: JACC expert panel. J Am Coll Cardiol. 2021;77:1454–69. https://doi.org/10.1016/j.jacc.2021.01.030.
Tamulevičiūtė-Prascienė E, Beigienė A, Thompson MJ, et al. The impact of additional resistance and balance training in exercise-based cardiac rehabilitation in older patients after valve surgery or intervention: randomized control trial. BMC Geriatr. 2021;21:23. https://doi.org/10.1186/s12877-020-01964-3.
Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Rev Esp Cardiol (Engl Ed). 2016;69:939. https://doi.org/10.1016/j.rec.2016.09.009.
European Association of Cardiovascular Prevention and Rehabilitation Committee for Science Guidelines, EACPR, Corrà U, et al. Secondary prevention through cardiac rehabilitation: physical activity counselling and exercise training: key components of the position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur Heart J 2010;31:1967–74.
Muller CO, Muthalib M, Mottet D, et al. Recovering arm function in chronic stroke patients using combined anodal HD-tDCS and virtual reality therapy (ReArm): a study protocol for a randomized controlled trial. TRIALS. 2021;22(1):747.
Müller L, Myers J, Kottman W, et al. Long-term myocardial adaptations after cardiac rehabilitation in heart failure: a randomized six-year evaluation using magnetic resonance imaging. Clin Rehabil. 2009;23:986–94. https://doi.org/10.1177/0269215509339003.
Cuesta-Vargas AI, Galán-Mercant A, Williams JM. The use of inertial sensors system for human motion analysis. Phys Ther Rev. 2010;15:462–73. https://doi.org/10.1179/1743288X11Y.0000000006.
Kavanagh JJ, Menz HB. Accelerometry: a technique for quantifying movement patterns during walking. Gait Posture. 2008;28:1–15. https://doi.org/10.1016/j.gaitpost.2007.10.010.
Merchán-Baeza JA, González-Sánchez M, Cuesta-Vargas AI. Reliability in the parameterization of the functional reach test in elderly stroke patients: a pilot study. Biomed Res Int. 2014;2014: 637671. https://doi.org/10.1155/2014/637671.
Moreno F-Á, Merchán-Baeza JA, González-Sánchez M, et al. Experimental validation of depth cameras for the parameterization of functional balance of patients in clinical tests. Sensors (Basel). 2017;17:424. https://doi.org/10.3390/s17020424.
Chan A-W, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158:200–7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
Berenguel Senén A, Martín Sierra C, Gallango BM. Actualización en rehabilitación cardíaca y prevención secundaria. Medicine - Programa de Formación Médica Continuada Acreditado. 2017;12:2232–42. https://doi.org/10.1016/j.med.2017.06.022.
Skinner JS, McLellan TM. The transition from aerobic to anaerobic metabolism. Res Q Exerc Sport. 1980;51:234–48. https://doi.org/10.1080/02701367.1980.10609285.
Herdy AH, Ritt LEF, Stein R, et al. Cardiopulmonary exercise test: background, applicability and interpretation. Arq Bras Cardiol. 2016;107:467–81. https://doi.org/10.5935/abc.20160171.
Ritt LE, Myers J, Stein R, et al. Additive prognostic value of a cardiopulmonary exercise test score in patients with heart failure and intermediate risk. Int J Cardiol. 2015;178:262–4. https://doi.org/10.1016/j.ijcard.2014.10.025.
Guazzi M, Bandera F, Ozemek C, et al. Cardiopulmonary exercise testing: what is its value? J Am Coll Cardiol. 2017;70(13):1618–36.
Scicchitano P, Ciccone MM, Iacoviello M, et al. Respiratory failure and bioelectrical phase angle are independent predictors for long-term survival in acute heart failure. Scandinavian Cardiovascular Journal. 2022;56:28–34. https://doi.org/10.1080/14017431.2022.2060527.
Oreopoulos A, Kalantar-Zadeh K, McAlister FA, et al. Comparison of direct body composition assessment methods in patients with chronic heart failure. J Card Fail. 2010;16:867–72. https://doi.org/10.1016/j.cardfail.2010.06.416.
Massari F, Mastropasqua F, Guida P, et al. Whole-body bioelectrical impedance analysis in patients with chronic heart failure: reproducibility of the method and effects of body side. Ital Heart J. 2001;2:594–8.
MicroMedical_SpiroUSB_Brochure_v3.pdf. https://www.hospital-hispania.com/opencms/export/sites/default/.content/documentos/catalogos/respiratorio/MicroMedical_SpiroUSB_Brochure_v3.pdf (accessed 24 Oct 2022).
Vieira D, Pessoa IS, Pereira H, et al. Test-retest reliability and concurrent validity of a digital manovacuometer. European Respiratory Journal 2014;44.https://erj.ersjournals.com/content/44/Suppl_58/P4304 (accessed 24 Oct 2022).
Forgiarini LA, Rubleski A, Douglas G, et al. Evaluation of respiratory muscle strength and pulmonary function in heart failure patients. Arq Bras Cardiol. 2007;89:36–41. https://doi.org/10.1590/s0066-782x2007001300007.
Messaggi-Sartor M, Guillen-Sola A, Depolo M, et al. Inspiratory and expiratory muscle training in subacute stroke a randomized clinical trial. Neurology. 2015;85:564–72. https://doi.org/10.1212/WNL.0000000000001827.
Berntsen S, Stølevik SB, Mowinckel P, et al. Lung function monitoring; a randomized agreement study. Open Respir Med J. 2016;10:51–7. https://doi.org/10.2174/1874306401610010051.
Dimitriadis Z, Kapreli E, Konstantinidou I, et al. Test/retest reliability of maximum mouth pressure measurements with the MicroRPM in healthy volunteers. Respir Care. 2011;56:776–82. https://doi.org/10.4187/respcare.00783.
Sylvester KP, Clayton N, Cliff I, et al. ARTP statement on pulmonary function testing 2020. BMJ Open Respir Res. 2020;7: e000575. https://doi.org/10.1136/bmjresp-2020-000575.
Martinez-Valdes E, Laine CM, Falla D, et al. High-density surface electromyography provides reliable estimates of motor unit behavior. Clin Neurophysiol. 2016;127:2534–41. https://doi.org/10.1016/j.clinph.2015.10.065.
van Helden JFL, Martinez-Valdes E, Strutton PH, et al. Reliability of high-density surface electromyography for assessing characteristics of the thoracic erector spinae during static and dynamic tasks. J Electromyogr Kinesiol. 2022;67: 102703. https://doi.org/10.1016/j.jelekin.2022.102703.
Imrani L, Boudaoud S, Lahaye C, et al. High-density surface electromyography as a biomarker of muscle aging. J Gerontol A Biol Sci Med Sci 2022;:glac143.
Drost G, Stegeman DF, van Engelen BGM, et al. Clinical applications of high-density surface EMG: a systematic review. J Electromyogr Kinesiol. 2006;16:586–602. https://doi.org/10.1016/j.jelekin.2006.09.005.
index.pdf. https://www.otbioelettronica.it/index.php?preview=1&option=com_dropfiles&format=&task=frontfile.download&catid=47&id=16&Itemid=1000000000000 (accessed 24 Oct 2022).
Herman T, Giladi N, Hausdorff JM. Properties of the ‘Timed Up and Go’ Test: more than meets the eye. Gerontology. 2011;57:203. https://doi.org/10.1159/000314963.
Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–23.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111–7.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80:837–41. https://doi.org/10.1016/s0003-9993(99)90236-8.
Gochicoa-Rangel L, Mora-Romero U, Guerrero-Zúñiga S, et al. Prueba de caminata de 6 minutos: recomendaciones y procedimientos. Neumología y cirugía de tórax. 2015;74:127–36.
Powertrack II Manual.pdf. https://chiroform.dk/wp-content/uploads/pdf/Powertrack%20II%20Manual.pdf (accessed 24 Oct 2022).
Karthikbabu S, Chakrapani M. Hand-held dynamometer is a reliable tool to measure trunk muscle strength in chronic stroke. J Clin Diagn Res. 2017;11:YC9-12.
Park H, Baek S, Kim H, et al. Reliability and validity of a new method for isometric back extensor strength evaluation using a hand-held dynamometer. Ann Rehabil Med. 2017;41:793. https://doi.org/10.5535/arm.2017.41.5.793.
Macfarlane DJ, Wong P. Validity, reliability and stability of the portable Cortex Metamax 3B gas analysis system. Eur J Appl Physiol. 2012;112:2539–47. https://doi.org/10.1007/s00421-011-2230-7.
Wasserman K. Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications. Philadelphia: 2005.
Huang W-M, Chen C-N, Chen Y-H, et al. The feasibility and safety of stepwise protocol in cardiopulmonary exercise testing-exercise stress echocardiography for subjects with heart failure. J Chin Med Assoc. 2022;85:815–20. https://doi.org/10.1097/JCMA.0000000000000763.
Shimmer User Manual. 2017;:76.
Mentiplay BF, Hasanki K, Perraton LG, et al. Three-dimensional assessment of squats and drop jumps using the Microsoft Xbox One Kinect: reliability and validity. J Sports Sci. 2018;36:2202–9. https://doi.org/10.1080/02640414.2018.1445439.
Clark RA, Mentiplay BF, Hough E, et al. Three-dimensional cameras and skeleton pose tracking for physical function assessment: a review of uses, validity, current developments, and Kinect alternatives. Gait Posture. 2019;68:193–200. https://doi.org/10.1016/j.gaitpost.2018.11.029.
Cruz-Montecinos C, Guajardo-Rojas C, Montt E, et al. Sonographic measurement of the quadriceps muscle in patients with chronic obstructive pulmonary disease: functional and clinical implications. J Ultrasound Med. 2016;35:2405–12. https://doi.org/10.7863/ultra.15.11032.
Extermann M, Aapro M, Bernabei R, et al. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol. 2005;55:241–52. https://doi.org/10.1016/j.critrevonc.2005.06.003.
Overcash JA, Beckstead J, Extermann M, et al. The abbreviated comprehensive geriatric assessment (aCGA): a retrospective analysis. Crit Rev Oncol Hematol. 2005;54:129–36. https://doi.org/10.1016/j.critrevonc.2004.12.002.
Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14:531–2. https://doi.org/10.1016/j.jamda.2013.05.018.
Sánchez-Rodríguez D, Marco E, Dávalos-Yerovi V, et al. Translation and validation of the Spanish version of the SARC-F questionnaire to assess sarcopenia in older people. J Nutr Health Aging. 2019;23:518–24. https://doi.org/10.1007/s12603-019-1204-z.
Comín-Colet J, Garin O, Lupón J, et al. Validación de la versión española del Kansas City Cardiomyopathy Questionnaire. Rev Esp Cardiol. 2011;64:51–8. https://doi.org/10.1016/j.recesp.2010.10.003.
Muñoz Díaz B, Molina-Recio G, Romero-Saldaña M, et al. Validation (in Spanish) of the mini nutritional assessment survey to assess the nutritional status of patients over 65 years of age. Fam Pract. 2019;36:172–8. https://doi.org/10.1093/fampra/cmy051.
Fuentes-Abolafio IJ, Escriche-Escuder A, Bernal-López MR, et al. Estimation of functional aerobic capacity using the sit-to-stand test in older adults with heart failure with preserved ejection fraction. J Clin Med. 2022;11:2692. https://doi.org/10.3390/jcm11102692.
Fuentes-Abolafio IJ, Trinidad-Fernández M, Escriche-Escuder A, et al. Kinematic parameters that can discriminate in levels of functionality in the six-minute walk test in patients with heart failure with a preserved ejection fraction. J Clin Med. 2022;12:241. https://doi.org/10.3390/jcm12010241.
Fuentes-Abolafio IJ, Trinidad-Fernández M, Ricci M, et al. Kinematic parameters related to functional capacity, fatigue, and breathlessness during the six-minute walk test in older adults with heart failure with preserved ejection fraction. Eur J Cardiovasc Nurs 2023; zvad027.
Zawadzka MM, Grabowski M, Kapłon-Cieślicka A. Phenotyping in heart failure with preserved ejection fraction: a key to find effective treatment. Adv Clin Exp Med. 2022;31:1163–72. https://doi.org/10.17219/acem/149728.
Shah SJ, Kitzman DW, Borlaug BA, et al. Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation. 2016;134:73–90. https://doi.org/10.1161/CIRCULATIONAHA.11.
Acknowledgements
Professor Dr. Ricardo Gomez-Huelgas, Head of the Internal Medicine Service Servicio de Medicina Interna, Hospital Regional Universitario de Málaga, Instituto de Investigación Biomédica de Málaga, Universidad de Málaga for advice and support.
Funding
Funding for this work was provided by a competitive grant by the Spanish Government, Health Research Grant, Instituto de Salud Carlos III (ISCIII) Fondo de Investigacion Sanitaria (FIS; exp. (PI22/00315), cofunded by European Union, title “Efectividad de un programa de rehabilitación cardiaca en biomarcadores cinemáticos, estructurales y fisiológicos en pacientes de edad avanzada con insuficiencia cardíaca. FUNNEL + . The ISCIII is not involved in the study design, data collection, data analysis, data interpretation or report writing.
Author information
Authors and Affiliations
Contributions
All authors met the criteria recommended by the International Committee of Medical Journal Editors. AIC-V, LPB formulated the conception, design and methods for the study. AIC-V, LPB, CG-C, EBD and drafted the manuscript. AIC-V and CG-C adapted the manuscript to the journal. All authors agreed on the definitive version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This proposal obtained approval from the local provincial committee (Malaga Provincial Ethics Committee; reference number 2198-N-22) in February 2023. Any modifications proposed to the protocol will be subject to a new review and approval. This trial also complies with the principles of the Declaration of Helsinki. All participants will give written informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
SPIRIT_Fillable-checklist.
Additional file 2.
Summary of CR programme.
Additional file 3.
Summary of Study outcomes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cuesta-Vargas, A.I., Fuentes-Abolafio, I.J., García-Conejo, C. et al. Effectiveness of a cardiac rehabilitation program on biomechanical, imaging, and physiological biomarkers in elderly patients with heart failure with preserved ejection fraction (HFpEF): FUNNEL + study protocol. BMC Cardiovasc Disord 23, 550 (2023). https://doi.org/10.1186/s12872-023-03555-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03555-7