Abstract
Background
Myocardial injury after non-cardiac surgery (MINS) is a frequent complication caused by cardiac and non-cardiac pathophysiological mechanisms, but often it is subclinical. MINS is associated with increased morbidity and mortality, justifying the need to its diagnose and the investigation of their causes for its potential prevention.
Methods
Prospective, observational, pilot study, aiming to detect MINS, its relationship with silent coronary artery disease and its effect on future adverse outcomes in patients undergoing major non-cardiac surgery and without postoperative signs or symptoms of myocardial ischemia. MINS was defined by a high-sensitive cardiac troponin T (hs-cTnT) concentration > 14 ng/L at 48–72 h after surgery and exceeding by 50% the preoperative value; controls were the operated patients without MINS. Within 1-month after discharge, cardiac computed tomography angiography (CCTA) and magnetic resonance imaging (MRI) studies were performed in MINS and control subjects. Significant coronary artery disease (CAD) was defined by a CAD-RADS category ≥ 3. The primary outcomes were prevalence of CAD among MINS and controls and incidence of major cardiovascular events (MACE) at 1-year after surgery. Secondary outcomes were the incidence of individual MACE components and mortality.
Results
We included 52 MINS and 12 controls. The small number of included patients could be attributed to the study design complexity and the dates of later follow-ups (amid COVID-19 waves). Significant CAD by CCTA was equally found in 20 MINS and controls (30% vs 33%, respectively). Ischemic patterns (n = 5) and ischemic segments (n = 2) depicted by cardiac MRI were only observed in patients with MINS. One-year MACE were also only observed in MINS patients (15.4%).
Conclusion
This study with advanced imaging methods found a similar CAD frequency in MINS and control patients, but that cardiac ischemic findings by MRI and worse prognosis were only observed in MINS patients. Our results, obtained in a pilot study, suggest the need of further, extended studies that screened systematically MINS and evaluated its relationship with cardiac ischemia and poor outcomes.
Trial registration Clinicaltrials.gov identifier: NCT03438448 (19/02/2018).
Similar content being viewed by others
Introduction
Annually, over 300 million people undergo major noncardiac surgery worldwide [1]. Despite preoperative screening, surgical improvements and increased patient monitoring, myocardial infarction remains the first cardiovascular cause of morbidity and mortality within 30 days after surgery [2]. Atherothrombosis is the underlying cause for most non-operative myocardial infarctions; but the mechanisms of the myocardial injury in noncardiac surgery (MINS), including perioperative myocardial infarction, are multiple and difficult to identify in the usual clinical practice. Theoretically, myocardial injury may be caused by four distinct mechanisms: coronary plaque rupture [3, 4], myocardial oxygen supply–demand mismatch [5, 6], non-ischemic cardiac disorders, such an atrial fibrillation episode [7], or non-cardiac causes, such as pulmonary embolism [8]. However, the angiographic, histological, or imaging studies required to identify all the MINS etiological mechanisms of are difficult to be implemented in all patients undergoing non-cardiac surgery [9]. Better understanding of causes originating MINS could help to develop potential preventive and therapeutic interventions. Recently, cardiac computed tomography angiography (CCTA), has demonstrated to improve the value of revised cardiac risk index [10], an established prognostic indicator of major cardiac events after surgery [11]. Moreover, cardiac magnetic resonance imaging (MRI) is considered the gold standard for noninvasively study of myocardial functionality. Therefore, minimally invasive diagnostic tests, like CCTA and cardiac MRI, could be promising tools to identify the occurrence and elucidate the underlying mechanisms of MINS.
In this pilot study, we aimed to identify with CCTA and MRI the existence of non-clinically evident coronary artery disease (CAD) and/or focal myocardial fibrosis in patients with or without MINS after undergoing major non-cardiac surgery. In addition, we aimed to analyse the relationship between MINS occurrence and the future major cardiovascular events (MACE). The primary outcomes were prevalence of CAD among MINS and controls and incidence of MACE at 1-year. Secondary outcomes were incidence of all 1-year outcomes, including mortality and individual components of MACE.
Methods
We adhered to the STROBE reporting guidelines (Additional file 1: Table S1). The protocol and the informed consent for troponin sampling and cardiac image studies were approved by the Ethics Committee of Clinical Research of the Hospital de la Santa Creu i Sant Pau in May 11th, 2016. The other participating centre (Hospital Vall d´Hebron) adhered to this approval (permitted by our local legislation) and used the same informed consents. The study was registered at Clinicaltrials.gov (NCT03438448). All participants provided written informed consent before recruitment.
Study design
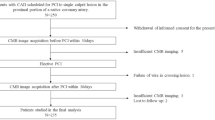
The current was a prospective, observational, cohort study in patients undergoing major noncardiac (elective or urgent) surgery (mainly digestive, gynaecologic, neurosurgery, orthopaedic, otorhinolaryngologic, plastic, thoracic, traumatological and vascular), requiring at least an overnight hospital admission. The study was carried out in two University Spanish hospitals, between July 2016 and December 2019. In the one of the participating centres (Hospital de la Santa Creu i Sant Pau) the current study was one of the sub-studies of a large cohort study aiming to evaluate the feasibility and impact of implementation of the systematic preoperative and postoperative hs-cTnT screening, as well as its cost-effectiveness., where systematic hs-cTnT screening program for MINS, was implemented at the routine perioperative care. Therefore, all patients provided informed consent for troponin sampling before surgery. In the other centre (Hospital Vall d´Hebron), where hs-cTnT screening was not performed systematically, the samplings were included in the framework of the study using the same informed consent for troponin sampling before surgery. All included patients at the cardiac imaging study, from two participating centres were identified and invited to participate after surgery and provided their specific imaging study informed consent.
Study participants
The study was focused on acute postoperative myocardial injury, i.e., MINS (excluding myocardial infarction). All patients had to meet at least one of the following inclusion criteria: (1) age ≥ 65 years old, (2) antecedents of stroke or transient ischemic attack or peripheral vascular disease if < 65 years old, or (3) preoperative estimated glomerular filtration rate (eGFR) between 30–59 mL/min/1.73 m2 Exclusion criteria included: (1) antecedents of ischemic heart disease and/or chronic heart failure, and (2) any contraindication to perform cardiac CCTA or MRI. Patients fulfilling inclusion criteria were identified by research personnel at post-surgery units, invited to participate in the image study and those accepting to be included signed a specific informed consent.
Hs-cTnT measurements
In the included patients, we measured the high-sensitive cardiac Troponin T (hs-cTnT, Roche Diagnostics, Basel, Switzerland) at three times: preoperatively and 48 and 72 h after surgery. The values of the limit of detection, 99th upper reference percentile (URL) and 10% coefficient of variation were 5.0 ng/L, 14.0 ng/L (both sexes) and 13.0 ng/L, respectively.
MINS definition and management
When a postoperative rise and/or fall pattern in hs-cTnT, with at least one value above the URL, was detected in a patient a 12-lead electrocardiogram (ECG) was performed. If the postoperative ECG showed changes vs the ECG before surgery, an echocardiography was conducted to rule out wall motion abnormalities. After completing the process, MINS was defined as any postoperative hs-cTnT value higher than the URL and showing at least a 50% increase respect to the preoperative concentration, in a patient without ECG signs or symptoms of myocardial ischemia. The control group included the patients without hs-cTnT elevations. A structured cardiology consultation was performed in MINS and control groups.
Advanced cardiac imaging studies (CCTA and cardiac MRI)
CCTA and MRI were performed in all patients within the first month after discharge and at the same centre (Hospital de Sant Pau, who acted as core-lab for cardiac imaging). On the previous days of the CCTA, patients were treated with a beta-blocker (atenolol 25–50 mg or ivabradine 5–7.5 mg to achieve a heart rate ≤ 60 beats per minute). A pair of expert evaluators formed by a cardiologist and a radiologist with level 3 training in interpretation of CCTA, read each angiogram using a 17-segment model of the coronary arteries without knowledge of the clinical data. Per-patient anatomical severity was classified according to the Coronary Artery Disease—Reporting and Data System (CAD-RADS) [12]. Triple-rule-out CCTA examinations (coronary artery disease, pulmonary embolism, and acute aortic pathology) were also performed. After the CCTA study, an MRI exam was performed to evaluate the global and segmental cardiac contractility and presence of focal fibrosis, using late gadolinium enhancement (LGE) contrast. We classified the LGE pattern as “ischemic” if subendocardial or transmural delayed contrast enhancement in a vascular distribution was observed and “non-ischemic” if enhancement was distributed patchy or diffuse, not following a vascular territory, mainly in mesocardial or epicardial locations [13]. Finally, in those with significant CAD in the CCTA (CAD-RADS ≥ 3), a pharmacological stress with adenosine was conducted, to assess functional impact of each coronary stenosis. A more detailed version of the study protocol was previously published [14].
Follow-up and data collection
All patients were followed for the study outcomes at 1 month, and at 1 year, after the date of surgery. The follow-up visits were conducted by telephone, supported by clinical electronic records. If the patients (or relatives) indicated that they had experienced any of the main outcomes, we obtained the relevant source documents from the corresponding electronic health records. All variables including risk factors (including the Revised Cardiac Risk Index-RCRI- [15]), comorbidities, medical treatment, and perioperative data (intraoperative hypotension was defined as a 30% drop of systolic blood pressure from baseline, intra and postoperative bleeding were defined as a 30 g/L drop from preoperative haemoglobin, need for transfusion or requiring haemostatic surgery, and intra and postoperative shock) were collected by study personnel on case report forms and entered at secure online database (www.clinapsis.com).
Main outcomes
The primary outcomes were prevalence of CAD among MINS and no-MINS patients and incidence of MACE at 1-year. MACE was defined as a composite of myocardial infarction, unstable angina, need of cardiac revascularization, heart failure, new atrial fibrillation episode, stroke, or pulmonary embolism (according definitions of the most recent guidelines). All-cause death was also registered. Secondary outcomes were incidence of all 1-year outcomes, including mortality and individual components of MACE.
Statistical considerations
Sample size
In the original protocol of this cardiac imaging sub-study, it was estimated that it would be necessary to recruit 260 participants (130 MINS cases and 130 matched controls) to detect an association between MINS condition and significant coronary atherosclerosis.
To calculate these sample sizes, we assume a prevalence of significant coronary atherosclerosis of around 19% in our high-risk population. The prevalence data was based in a previous study [16] of some of the current co-authors in a similar population to that of the study.
Statistical analysis
For categorical variables, the percentage and the number of cases and the mean and standard deviation or median and interquartile range for quantitative variables were provided. Comparisons between groups were assessed with the Student’s T test or the Mann–Whitney’s U-test for continuous variables and with the chi-square tests or the Fisher exact test for comparing the proportions of categorical variables. Two-sided significance levels of 0.05 were used in all analyses. Data were analysed using STATA SE Version 13.0 (StataCorp LLC, College Station, TX, USA).
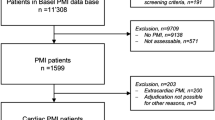
Results
Clinical characteristics of the study population and risk assessment of index surgery
From total 373 screened MINS patients, 58 did not fulfilled inclusion criteria, other 192 declined to participate, additional 5 withdrawn from the study after had provided informed consent, and finally, 66 were not included due to logistic issues (discharged before complete sampling, CCTA not available, frailty). Therefore, we included 52 MINS patients and completed their follow-up. Regarding the control group and owing to the large number of eligible patients (1,972), we proposed to participate to a similar number no-MINS patients as the needed to achieve our previous size calculations. Unfortunately, in this group we obtained even lower participation rate than in MINS, mainly due to the same reasons as in the MINS group plus a huge number of refusals. We could only include and complete the follow-up in 12 controls. In the recruiting centre with a systematic MINS screening a 10.5% of screened patients were lost by lack on hs-cTnT value at 72 h after surgery. The 1-year follow-up of several cases coincide with the first and second COVID-19 waves in Spain; thus, an indeterminate number of missed follow-ups, particularly in control subjects (no-MINS), could be attributed to the inability of some elderly, frail patients to answer to the follow-up request due to their current clinical condition. Most patients (58, 90.6%) were ≥ 65 years old (mean age 75.1), 30 (46.9%) were females, all Caucasians, with a high prevalence of cardiovascular risk factors mainly hypertension, diabetes mellitus and different dyslipidaemias, and, accordingly, on current treatment with antihypertensive drugs, statins, and aspirin. Peripheral artery disease and chronic obstructive pulmonary disease were also frequent (~ 15%). There were no relevant differences in the baseline features of patients between MINS and control groups, though diabetes mellitus was found in 42.3% (22) of MINS patients and in 16.7% (2) of controls (Table 1).
Regarding risk assessment prior to index surgery, the RCRI class I was separately analysed from the other classes, since it was the most frequently observed among the patients, to try to avoid that a difference on risk assessment between MINS and controls could remain «unseen» in the general statistical assessment of the fourth RCRI groups. Low RCRI was more frequent in controls (11, 91.7%) than in MINS patients (31, 59.6%, p < 0.01); eGFR was lower, in patients with MINS than in controls (71.1 vs. 76.5 mL/min/1.73 m2) though the difference was not statistically significant (p = 0.136) (Table 2). Hs-cTnT concentrations were not different between MINS and controls previously to surgery, but the MINS group showed median values two to three times higher than controls at 48 h (41 vs 14 ng/L, p < 0.002) and 72 h (31 vs 11 ng/L, p < 0.001) of surgery. During intervention, hypotension was frequent in MINS and controls (65.3% and 83.3%, respectively) requiring therapy in most cases (71.0% and 90.0%, respectively). In the MINS group, intraoperative bleeding (10.4%) and intra and postoperative shock (16% and 10%, respectively) were found compared with their complete absence in the control group, though owing the few cases the differences between groups did not reach statistical significance.
Advanced cardiac imaging findings
Out of 64 patients, we performed an echocardiogram, a CCTA scan, and a cardiac MRI in 64 (100%), 62 (97%), and 49 (77%), respectively. Table 3 describes the main findings of the advanced cardiac imaging studies. The median left ventricular ejection fraction (LVEF) measured by echocardiogram was normal in both groups, and abnormal wall motion was observed only in three MINS patients. The frequency of significant CAD (CAD-RADS ≥ 3) was similar in MINS (n = 15, 30%) than in the control group (n = 4, 33%); a total of nineteen subjects of both groups had a CAD-RADS ≥ 3. Calcified plaques were found in approximately two thirds of patients of both groups (29 MINS: 58.0%, 7 controls: 58.3%); vulnerable plaques were quite infrequent. In the MRI explorations, LVEF and abnormal wall motion findings were similar than those of CCTA. Late gadolinium enhancement (LGE) was similarly found in near to one third of MINS (n = 11, 28.2%) and controls (n = 3, 30.3%). An adenosine test was performed in the nineteen subjects with a significant CAD by the CAD-RADS index. No differences were observed between groups in the frequency of abnormalities of wall perfusion, as it was found in the echocardiographic or MRI explorations; we found cardiac ischemic patterns in five and ischemic segments in two MINS patients compared with any in the control group.
Outcomes in the follow-up
All cause-mortality (4 patients, 7.7% after 1-year follow-up) only occurred in the MINS group; a sudden cardiac death happened in a patient with many treated cardiovascular risk factors and the other deaths were due to malignancies. MACE was also only detected in MINS patients (n = 8, 15.4%) (Table 4). Three patients with MINS developed ischemic symptoms; two of them undergone coronary angiography, which showed significant coronary artery disease. Both patients were revascularized during the procedure without further complications. The third patient with ischemic symptoms was managed with medical treatment, because due to his/her fragility a coronary interventionism was discouraged.
Discussion
In the current study, conducted in a group of patients with high cardiovascular risk undergoing major non-cardiac surgery, we have analysed the frequency of myocardial injury (MINS) detected with high-sensitive troponin T (hs-cTnT), the occurrence of subclinical coronary artery disease (CAD) detected with advanced imaging techniques, and the occurrence of cardiovascular complications after one year follow-up.
We found several interesting findings. First, the Revised Cardiac Risk Index (RCRI) stage I, associated to the lowest cardiac risk, was significantly more frequent in control subjects than in MINS patients. Though differences in the preoperative variables included in the RCRI between both groups did not achieve statistical significance, MINS patients received more often thoracic, abdominal, and vascular surgeries and have an eGFR lower than controls; taking together, all these differences could justify the predominance of a RCRI value associated to low cardiac risk in the control population. Second, in our study, we measured hs-cTnT pre and postoperatively and MINS was defined by percentual increases against the preoperative concentration. In the MINS group, the postsurgical hs-cTnT concentrations were only mildly elevated (2–3 times) over the upper reference limit (URL) of 14 ng/L, but between 3 to 4-times over the preoperative values. This result support that the extent of myocardial injury in the MINS group was small and that it was easier to detect by hs-cTnT serial changes rather than by reference to the URL. Our findings agree with the low individuality index of hs-cTnT observed in different studies both in control subjects and in patients with cardiac or renal disease [17]. When the individuality index of a variable is low, the signification of its value must be analysed against its serial evolution rather than against its URL. Moreover, patients as those included in our study often have basal hs-cTnT values higher than the URL; thus, to define an ongoing myocardial injury serial values and significant changes are required [18]. Third, by CCTA we found that significant CAD, measured as a CAD-RADS ≥ 3.0, existed in 30% of MINS and in 33.3% of controls; these findings superseded the assumptions made in our protocol. Our results agreed with those of OPTIMUS [19] and CORONARY Vision-CTA [11] studies, which observed that atherothrombosis was implicated in one third of cases of cardiac damage in non-cardiac surgery patients. However, as outlined in a sub-study of the CORONARY Vision-CTA study, many patients with severe coronary lesions in the CCTA did not have postoperative complications suggesting that CCTA could overestimate the future risk of these patients. The authors of the study suggested that MRI could improve the identification of patients at risk of postoperative outcomes [20]. Of note, the CCTA explorations in the CORONARY Vision-CTA were performed preoperatively and, in our study, postoperatively. Fourth, by late gadolinium enhanced cardiac MRI, we identified focal fibrosis, a sign of myocardial ischemia, in one-third of both MINS patients and controls. Our population, although exclude patients with previous ischemic cardiac disease or chronic heart failure, included many subjects with cardiovascular risk factors or antecedents of cerebrovascular and peripheral arterial diseases. Thus, our patients would be prone to have subclinical myocardial ischemic features in MRI; same MRI findings have been observed in large studies in asymptomatic individuals or general population presenting similar health status than our patients [21, 22],. There are only one study using MRI to detect postoperative myocardial injury after non-cardiac surgery in 22 patients with an age and health status similar to ours and with significative CAD detected by CCTA, although myocardial injury was assigned using a contemporary cardiac troponin I assay with lower analytical and clinical sensitivity than high sensitive assays used in our study [23]. The study found clinically silent pulmonary embolism in one-third of patients with myocardial injury, an alteration that we did not observe in our study. Late gadolinium enhancement and perfusion defect were observed in one-third of cases, same proportion as in our study. The small number of included patients in the referred study and in own study could be the cause of highly discrepant proportions, but really derived from very small numbers. Fifth, adenosine stimulation, only conducted in patients with a CAD-RADS ≥ 3.0, revealed that unlike the similar frequency of the index and abnormal wall reperfusion defects in both MINS and controls, only MINS group had ischemic segments in MRI. Pharmacological stress perfusion with adenosine is the non-invasive investigation of choice in patients with suspected, but uncertain myocardial ischemia diagnosis [24]. As mentioned, our patients, both those with MINS and those without, have an increased preoperatory risk of cardiovascular complications. However, despite the similarities between both groups in some cardiac postoperative image features, the adenosine stimulation revealed that ischemic segments only existed in MINS patients. Thus, adenosine stimulation was a useful tool to finely distinguish patients with non-clinically evident cardiac lesions that are associated with poorer prognosis as observed in our MACE results. Sixth, intraoperative hypotension requiring therapy was equally frequent in MINS and controls; however, intraoperative bleeding and intra and postoperative shock were only found in MINS. Both the bleeding and shock occurring in the MINS patients are well-known causes of myocardial oxygen supply–demand mismatch. Thus, bleeding and shock, linked with a frequent although undetected CAD, are probably the ultimate causes of many of the observed MINS in our study. These results agreed with those found in the OPTIMUS and CORONARY Vision-CCTA studies which attributed two-thirds of the myocardial damage observed after non-cardiac surgery to the supply–demand imbalance mechanism, whereas only one-third could be attributed to atherothrombosis [11, 19]. And, seven, whatever the cause at their origin, the occurrence of MINS was associated with a 15% frequency of MACE in the 1-year follow-up, whereas in the control group any MACE was detected in the follow-up. This result outlines the importance of MINS screening and diagnosis.
Implications for practice and research
Understanding the pathophysiology of MINS is crucial to develop potential prophylactic and therapeutic interventions to improve the prognosis of patients undergoing noncardiac surgery. Our results, as hypothesis generating from a pilot study, must be confirmed by further large studies, but could inform prophylactic and therapeutic interventions, and eventually, improve the prognosis of MINS patients. Moreover, our study was performed in two Spanish hospitals, so further large research involving a more racially diverse study population will help to extend the clinical implications of our results.
Limitations and strengths
We acknowledge several limitations of our study. First, we were unable to achieve initially estimated sample size. A small size, with a low number of patients in the control group, makes difficult to provide some statistically significant conclusions. As mentioned, we screened 373 individuals in each group, but the losses due to failing a complete hs-cTnT sampling, the reluctancy of the controls to undergone imaging tests, the difficulty for displacements of old, frail patients recently operated and the temporal coexistence of part of the 1-year follow-up with COVID waves that restricted the participation of individuals could explain our small recruitment. A study with a very close design as our protocol, included 46 patients with myocardial injury and 20 controls after screening 1205 candidates in pre-COVID times [23]. Therefore, our results should be interpreted as a pilot study, providing a “proof of concept” paving the way to design further studies in this field. Second, the assumptions made at the time of initial protocol development were superseded by the higher significant CAD-RADS ≥ 3 atherosclerosis frequency found by CCTA both in MINS (30.0%) and controls without MINS (33.3%) (Table 3). Third, we assessed coronary anatomy by CCTA and cardiac functionality by MRI after surgery; thus, it is possible that some of the cardiac findings existed before the intervention. Fourth, our selection criteria resulted in a population of patients with not known CAD and with or without isolated MINS; our results may be difficult to apply to other populations.
Regarding strengths, our study has some. The study addresses a very important topic in perioperative medicine, often not addressed in clinical practice, and provides some new knowledge using fine techniques as high-sensitive cardiac troponin, CCTA and cardiac MRI. In our knowledge, this is the first application of CCTA together with cardiac MRI in the evaluation of major non-cardiac surgery patients. We identified two different groups in our subjects with some similarities in coronary anatomy and occurrence of coronary disease features, but clear differences regarding cardiac ischemia and adverse outcomes in the follow-up that only were observed in patients with MINS. These observations reinforce the need of implementing systematic screening in major non-cardiac surgery patients to identify MINS and implement therapies that could decrease their occurrence.
Conclusions
This study with advanced imaging methods found a similar CAD frequency in MINS and control patients, but that cardiac ischemic findings in the MRI exploration and worse prognosis were only observed in MINS patients. Our results, obtained in a pilot study, suggest the need of further, extended studies that screened systematically MINS and evaluated its relationship with cardiac ischemia and poor outcomes.
Availability of data and materials
The data used in the present study is part of a larger dataset. The datasets generated and analysed during the current study are available and can be supplied from the corresponding authors upon reasonable request. The data not used for this manuscript will be employed in future manuscripts.
Abbreviations
- MINS:
-
Myocardial injury after non cardiac surgery
- CAD:
-
Coronary artery disease
- CAD-RADS:
-
Coronary Artery Disease-Reporting and Data System
- CCTA:
-
Cardiac computed tomography angiography
- MRI:
-
Magnetic resonance imaging
- ECG:
-
Electrocardiogram
- MACE:
-
Major cardiovascular events
- hs-cTnT:
-
High-sensitive cardiac troponin
- URL:
-
Upper reference percentile
- RCRI:
-
Revised Cardiac Risk Index
- LGE:
-
Late gadolinium enhancement
- LVEF:
-
Left ventricular ejection fraction
References
Puelacher C, Bollen Pinto B, Mills NL, et al. Expert consensus on peri-operative myocardial injury screening in noncardiac surgery: a literature review with expert consensus. Eur J Anaesthesiol. 2021. https://doi.org/10.1097/EJA.0000000000001486.
Gualandro DM, Puelacher C, Lurati Buse G, et al. Incidence and outcomes of perioperative myocardial infarction/injury diagnosed by high-sensitivity cardiac troponin I. Clin Res Cardiol. 2021;110(9):1450–63. https://doi.org/10.1007/s00392-021-01827-w.
Dawood MM, Gutpa DK, Southern J, et al. Pathology of fatal perioperative myocardial infarction: implications regarding pathophysiology and prevention. Int J Cardiol. 1996;57(1):37–44. https://doi.org/10.1016/s0167-5273(96)02769-6.
Cohen MC, Aretz TH. Histological analysis of coronary artery lesions in fatal postoperative myocardial infarction. Cardiovasc Pathol. 1999;8(3):133–9. https://doi.org/10.1016/s1054-8807(98)00032-5.
Ellis SG, Hertzer NR, Young JR, et al. Angiographic correlates of cardiac death and myocardial infarction complicating major nonthoracic vascular surgery. Am J Cardiol. 1996;77(12):1126–8. https://doi.org/10.1016/s0002-9149(96)00130-0.
Menosi Gualandro D, Augusto Campos C, Calderaro D, et al. Coronary plaque rupture in patients with myocardial infarction after noncardiac surgery: frequent and dangerous. Atherosclerosis. 2012;222(1):191–5. https://doi.org/10.1016/j.atherosclerosis.2012.02.021.
Bessissow A, Khan J, Devereaux PJ, Alvarez-Garcia J, et al. Postoperative atrial fibrillation in non-cardiac and cardiac surgery: an overview. J Thromb Haemost. 2015;13(Suppl 1):S304–12. https://doi.org/10.1111/jth.12974.
Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 1999;353(9162):1386–9. https://doi.org/10.1016/s0140-6736(98)07534-5.
Grobben RB, Van Klei WA, Grobbee DE, et al. The aetiology of myocardial injury after non-cardiac surgery. Neth Heart J. 2013;21(9):380–8. https://doi.org/10.1007/s12471-013-0463-2.
Sheth T, Chan M, Butler C, et al. Prognostic capabilities of coronary computed tomographic angiography before non-cardiac surgery: prospective cohort study. BMJ. 2015;350:h1907. https://doi.org/10.1136/bmj.h1907.
Hwang JW, Kim EK, Yang JH, et al. Assessment of perioperative cardiac risk of patients undergoing noncardiac surgery using coronary computed tomographic angiography. Circ Cardiovasc Imaging. 2015;8(3):e002582. https://doi.org/10.1161/CIRCIMAGING.114.002582.
Cury RC, Abbara S, Achenbach S, et al. CAD-RADSTM Coronary Artery Disease – Reporting and Data System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr. 2016;10(4):269–81. https://doi.org/10.1016/j.jcct.2016.04.005.
Cummings KW, Bhalla S, Javidan-Nejad C, et al. A pattern-based approach to assessment of delayed enhancement in nonischemic cardiomyopathy at MR imaging. Radiographics. 2009;29(1):89–103. https://doi.org/10.1148/rg.291085052.
Popova E, Paniagua Iglesias P, Alvarez Garcia J, et al. Rationale and design of perioperative myocardial ischemia: a protocol for troponin monitoring, prognostic thresholds, economic analysis and further insights into pathophysiology for non-cardiac surgery patients. F1000Res. 2019;8:850.
Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–9. https://doi.org/10.1161/01.cir.100.10.1043.
Descalzo M, Leta R, Rosselló X, et al. Subclinical coronary atherosclerosis identified by coronary computed tomography angiography in asymptomatic population by coronary artery disease risk level. Rev Esp Cardiol (Engl Ed). 2013;66(6):504–5. https://doi.org/10.1016/j.rec.2012.12.012.
Lan NSR, Bell DA. Revisiting the biological variability of cardiac troponin: Implications for clinical practice. Clin Biochem Reviews. 2019;40:201–16. https://doi.org/10.33176/AACB-19-00032.
Apple FS, Jaffe AS, Collinson P, et al. International Federation of Clinical Chemistry (IFCC) Task Force on Clinical Applications of Cardiac Bio-Markers. IFCC educational materials on selected analytical and clinical applications of high sensitivity cardiac troponin assays. Clin Biochem. 2015;48:201–3. https://doi.org/10.1016/j.clinbiochem.2014.08.021.
Sheth T, Natarajan MK, Hsieh VV, et al. Incidence of thrombosis in perioperative and nonoperative myocardial infarction. Br J Anaesth. 2018;120:725–33. https://doi.org/10.1016/j.bja.2017.11.063.
Dowsley TF, Sheth T, Chow BJW. Coronary computed tomography angiography and nuclear myocardial perfusion imaging in non-cardiac surgery: A VISION-CTA sub-study. J Nucl Cardiol. 2020;27(4):1331–7. https://doi.org/10.1007/s12350-019-01779-9.
Yoneyama K, Venkatesh BA, Bluemke DA, et al. Cardiovascular magnetic resonance in an adult human population: serial observations from the multi-ethnic study of atherosclerosis. J Cardiovasc Magn Reason. 2017;19:52. https://doi.org/10.1186/s12968-017-0367-1.
Anand D, Lim E, Raval U, et al. Prevalence of silent myocardial ischemia in asymptomatic individuals with subclinical atherosclerosis detected by electron beam tomography. J Nucl Cardiol. 2004;11:450–7. https://doi.org/10.1016/j.nuclcard.2004.06.125.
Grobben RB, Van Waes JAR, Leiner T, et al. Unexpected cardiac computed tomography findings in patients with postoperative myocardial injury. Anesth Analg. 2018;126(5):1462–8. https://doi.org/10.1213/ANE.0000000000002580.
Valbuena-López S, Hinojar R, Puntmann VO. Cardiovascular magnetic resonance in cardiology practice: a concise guide to image acquisition and clinical interpretation. Rev Esp Cardiol (Engl Ed). 2016;69:202–10. https://doi.org/10.1016/j.rec.2015.11.011.
Acknowledgements
Ekaterine Popova (EP) is a PhD candidate in the doctorate program of “Methodology of biomedical research and Public Health” of the Paediatrics, Obstetrics and Gynaecology and Preventive Medicine Department, Universitat Autònoma de Barcelona, Spain and she is funded by a research contract ((PERIS SLT017/20/000089) of the Health Department, Generalitat de Catalunya, Spain. We thank all patients and their families that agreed to be included in the study and provided the requested information. We wish also to acknowledge to the research nurses at participating hospitals: Ana Fernandez Martinez and Dina Burton Carmona.
Disclaimer
The funders had no role in the study design, data collection, management, analysis, writing of the report, the decision to submit the report for publication, and they will not have ultimate authority over any of these activities.
Dissemination declaration
The dissemination of data results to study participants and or patient organizations in this research project is not possible/applicable as the data are de‑identified.
Patient and public involvement
Patients were not involved in the design, conduct and reporting of this study as it was not applicable to this research project.
Transparency declaration
Authors affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and if relevant) have been explained.
Funding
The study has been supported by research grant from the Instituto de Salud Carlos III, Spain (PI16/01162), partly funded by Fondo Europeo de Desarrollo Regional (FEDER), Unión Europea, “Una manera de hacer Europa” to Ekaterine Popova, by Generalitat de Catalunya (PERIS SLT017/20/000089) to Ekaterine Popova and by a "Marato de TV3" grant (20150110) to Pablo Alonso-Coello.
Author information
Authors and Affiliations
Contributions
JAG and EP wrote the original manuscript. JAG, EP, PAC, FCC, JOL and JZ made substantial contributions to conception and design of the study. PAC, JOL, FCC and IFG contributed to writing, review and editing. JAG, EP, MVB, MdN, GO, MRL, AHM, ESG, PPI, XGMM, DVM, RLP, IFG ensured project administration, data curation visualization. JAG, JZ and JOL performed formal analysis. EP and PAC ensured funding acquisition. PAC and FCC both senior authors contributed equally to supervision, re-view and editing of this work. All authors warrant that they have reviewed and approved the manuscript prior to submission, and they accept the responsibility for the information contained in the submission. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethic approval and consent to participate
The study ethics approval was obtained from corresponding Ethical Committees (Hospital Universitari de la Santa Creu i Sant Pau, and Hospital Univestitari Vall d’Hebron, Barcelona, Spain) on 11/05/2016. Specific written informed consent for the image study was provided by the patients before recruitment during index hospitalization. All methods were carried out in accordance with relevant guidelines and regulations. Study was registered at Clinicaltrials.gov (NCT03438448).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
STROBE-Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Álvarez-Garcia, J., Popova, E., Vives-Borrás, M. et al. Myocardial injury after major non-cardiac surgery evaluated with advanced cardiac imaging: a pilot study. BMC Cardiovasc Disord 23, 78 (2023). https://doi.org/10.1186/s12872-023-03065-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03065-6