Abstract
Background
There are limited data on the burden, characteristics, and outcomes of hospitalized heart failure (HF) patients in Thailand. The aim of this study was to investigate national trend in HF hospitalization rate, in-hospital and 1-year mortality rate, and rehospitalization rate in Thailand.
Methods
We analyzed the claims data of hospitalized patients obtained from the three major Thailand public health reimbursement systems between 2008 and 2013. Patients aged ≥ 18 years with a principal diagnosis of HF by the International Classification of Diseases, Tenth Revision, Thai modification were included. Comorbidities were identified by secondary diagnosis codes. The annual rate of HF hospitalization was calculated per 100,000 beneficiaries. Records of subsequent hospitalization of discharged patients were retrieved. For 1-year mortality rate, vital status of each patient was obtained from Thai Civil Registration of Death database. All outcomes were tested for linear trends across calendar years.
Results
Between 2008 and 2013, 434,933 HF hospitalizations were identified. The mean age was 65.3 years (SD 14.6), and 58.1% were female. The HF hospitalization rate increased from 138 in 2008 to 168 per 100,000 beneficiaries in 2013 (P for trend < 0.001). Nearly half (47.4%) had had a prior HF admission within 1 year. A small proportion of patients (7.4%) received echocardiography during hospitalization. The median length of hospital stay was 3 days. In-hospital mortality declined from 4.4 to 3.8% (P for trend < 0.001). The overall 30-day and 1-year rehospitalization rates were 34 and 73%, respectively, without significant trends over the study period. Most common cause of 30-day rehospitalization was HF (42%). One-year mortality decreased from 31.8% in 2008 to 28.5% in 2012 (P for trend < 0.001).
Conclusion
Between 2008 and 2013, HF hospitalization rate in Thailand increased. The in-hospital and 1-year mortality rates decreased slightly. However, the rehospitalization rate remained high mainly due to recurrent HF hospitalization.
Similar content being viewed by others
Introduction
Heart failure (HF) is increasingly becoming a major health problem in many countries. One of the issues is HF hospitalization. Because HF is a common hospitalized condition in aging populations with a high readmission rate and long-term mortality risk [1, 2], it consumes a significant amount of health budget from both direct and indirect costs [3]. However, epidemiological data of this condition are limited in low- and middle-income countries (LMICs), including Thailand [4]. In addition, there are differences in the epidemiology, characteristics, and prognosis of hospitalized HF patient between countries in different world regions [5]. Until now, ADHERE-Thailand is the only sizable registry of hospitalized HF patients for the country [6]. However, the registry only collects data in cardiac centers in tertiary hospitals or large private hospitals, mostly in the Bangkok metropolitan area. Therefore, their data might not represent the overall picture of nationally for hospitalized patients with HF. Also, this registry has not assessed the long-term outcomes of these patients.
As the health care provision for the Thai population has been improving since the implementation of universal health coverage system for all Thai people in 2002 [7], HF and other conditions that can cause HF, such as hypertension and myocardial infarction, might have been treated more effectively [8]. Thus, the hospitalization rate of HF is supposed to have decreased and prognosis of HF hospitalization is supposed to have improved. Conversely, the number of older adults in Thailand has been increasing [9], and survivors from cardiovascular disease (e.g., acute myocardial infarction without appropriate treatment) might develop HF [8]. Both of these factors may increase the rate of HF hospitalization. To date, the rate and trend of HF hospitalization in Thailand are unknown. Understanding the health burden of HF is necessary to prevent and improve the outcomes of this lethal condition for the future aging society of Thailand.
Thus, we aimed to determine the national HF hospitalization rate, and the characteristics of hospitalized HF patients in Thailand from 2008 to 2013 using public health security scheme data. We also aimed to determine the rates of rehospitalization and mortality of hospitalized HF patients, and the factors associated with them.
Methods
Study design, setting, and sources of data
This was a nationwide, retrospective observational study using in-patient medical expense claims data to identify adult patients hospitalized with HF from 2008 to 2013 in Thailand. The Siriraj Institutional Review Board reviewed the protocol and approved the study with an exemption from requiring consent due to the retrospective nature of the study (ethics committee code 647/2556). All patient identities were encrypted from the data sources. The study followed the Reporting of Studies Conducted Using Observational Routinely-collected Health Data guideline [10].
We retrieved the in-patient electronic health medical expense claims data from three major public health security schemes covering all Thai citizens of all ages. Each citizen is allowed to have only one public health security coverage at any given time. These three schemes are the Civil Servant Medical Benefit scheme (CSMBS) for 4.4 million government officers and their families, the Social Security Scheme (SSS) for 10.6 million employees in the private sector, and the Universal Health Coverage scheme (UCS), which has covered the remaining 48 million persons since 2002 [7]. The public and participating private hospitals throughout Thailand send the electronic discharge records of each hospitalized patient to the online claims reimbursement system of one of these schemes. The amount of payment for hospitalized patient reimbursement is determined by Diagnostic-Related Groups version 5.0 (Office of the Development of Thai Joint Disease Group, Institute of Health Systems Research Institute, Thailand) calculated from each record data. These data include the patient’s unique identifier, age, sex, national identification number (ID), hospital identifier, admission and discharge dates, discharge status, primary diagnosis and secondary diagnoses coded in the International Classification of Diseases, Tenth Revision, Thai modification (ICD-10 TM code), procedure coded in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9 CM), and the amount of hospital expenses charged. The Bureau of Claims and Medical Audit (BCMA) of National Health Service Office (NHSO) periodically audits selected claims medical records for data quality and accuracy.
Participants, data access, and data linkage
We requested the data centers of the three public health security schemes to retrieve the medical claims data of all patients aged ≥ 18 years with HF hospitalization as the principal diagnosis from 2008 to 2013, referred to as the index HF hospitalization. The ICD-10 TM codes for HF were I50.0, I50.1, I50.9, I11.0, I13.0, and I13.2. Next, the records of all hospitalization (with any principal diagnosis) from 2007 to 2013 of corresponding HF patient were identified for analysis of comorbidities and rehospitalizations. Exclusion criteria were erroneous data entries (e.g., very extreme age or duplicate admissions) or overlapping admission periods in the same patient without the code of the patient’s transfer.
For vital status and date of death, each data center linked the patient’s national ID with the Thai Civil Registration of Death (TCRD) from the Bureau of Registration administration of Thailand. The vital statuses of the patients were followed until the 31 December 2013 in the CSMBS and SSS and 26 June 2014 in the UCS. After retrieving the linked information, all patient identifiers were encrypted before the data were sent to the investigators.
Patient comorbidities and procedures
The comorbidities and complications were defined by the ICD-10 TM in secondary diagnosis codes in the claim records of the index HF hospitalizations, which allowed for a maximum of 20 codes per each record. For prior HF, myocardial infarction, and other comorbidities, the codes in either the principal or the secondary diagnosis codes of the previous admissions up to 1 year before the index HF hospitalization were additionally identified to optimize the completeness of the data of comorbidities [11]. There were no changes in the ICD-10 TM code definitions during study period. The procedures performed during hospitalizations were identified by ICD-9 CM. The ICD-10 TM codes for comorbidities were grouped to be comparable to the Centers for Medicare and Medicaid Services ICD-10-CM mapping [11]. The full list of ICD-10 TM codes and ICD-9 CM codes used for grouping is provided in Additional file 1: Table S1.
Primary and secondary outcomes
The main outcome was the annual rate of HF hospitalization and the trend from 2008 to 2013. To calculate the HF hospitalization rate per 100,000 beneficiaries for each year, we divided the number of hospitalized HF patient by the corresponding number of beneficiaries. The number of beneficiaries from the NHSO database were categorized by gender, age, and health security scheme. [12] The range of ages in the beneficiary data was categorized into 5-year intervals from 15–19 years, 20–24 years and etc., except for the oldest age category, ≥ 80 years. Thus, for the analysis of rate of HF hospitalization per 100,000 beneficiaries, we excluded patients aged 18–19 years from the analysis. Because one patient could have been admitted with HF more than once in each calendar year, we calculated HF hospitalization rate as unique person per 100,000 beneficiaries.
The in-hospital mortality rate was calculated by dividing the number of the hospitalizations ending in death identified by the discharge status code by the total of HF hospitalizations for a given year. The hospital length of stay (HLOS) was determined by the time and date of patient admission and discharge. A duration of stay > 6 h was counted as 1 day.
We calculated the all-cause HF rehospitalization and HF-specific rehospitalization rates. We identified rehospitalization after the index HF hospitalization using the encrypted national IDs. The time-to-rehospitalization was calculated by discharge date of the index HF hospitalization and the admission date of the subsequent hospitalization. The rehospitalization rate was calculated using the number of rehospitalizations in given period of interest (e.g., 30 days) divided by the number of index HF hospitalization discharged alive. Records were excluded from the rehospitalization analysis if the discharge status of the index HF hospitalization was either death or transferred. The cause of the rehospitalization was determined by the principal diagnosis of the readmission and was grouped by ICD-10 TM code. The ICD-TM code list for grouping the cause of rehospitalizations is shown in Additional file 1: Table S1.
The 1-year mortality rate was calculated by the time-to-death from the admission date of the index HF hospitalization to the date of death from the TCRD. If a patient as unique person was hospitalized for HF > 1 time in a given year, we randomly selected only one HF hospitalization in that calendar year [11]. We repeated this randomization of HF hospitalization selection three times to calculate the mortality rate. No significant differences in the 1-year mortality rate of each year was observed comparing between these three randomizations (data not shown).
Statistical analysis
To test the statistical significance of changes over study period in patient characteristics, mortality rate, and rehospitalization rate, we used the Mantel–Haenszel-Chi-Squared test of linear association for categorical variables and the Cuzick non-parametric test for continuous variables [13].
For the annual rate of HF hospitalization per 100,000 beneficiaries, we evaluated significance of trend changes using Poisson regression. The age- and gender-adjusted HF hospitalization rate and incidence rate ratio compared to 2008 for each calendar year from 2009 to 2013 were calculated by Poisson regression. Unconditional binary logistic regression was used to test statistical significance of predictors for the outcomes of interest of rehospitalization and death.
Stata/MP, release 14.1 (StataCorp LP) was used for all analyses. A p-value < 0.05 was considered statistically significance using 2-sided tests.
Results
From 2008 to 2013 nationwide hospital claims data, we identified 435,283 HF hospitalizations in patients aged ≥ 18 years, accounting for 1.7% of all the adult hospitalizations during the period. After cleaning the data, 434,933 HF hospitalizations in 302,833 patients were included in the final analysis. Figure 1 depicts a flow diagram of the patient selection and the distribution of the ICD-10 codes of the primary diagnosis. Most of the HF hospitalizations (92%) were under UCS coverage.
Patient characteristics
Table 1 shows the characteristics of patients hospitalized for HF from 2008 to 2013. For the overall 6-year period, the mean age was 65.3 years (SD 14.6) without a significant linear trend over the study period (P for trend = 0.18). Those aged 60 to 79 years accounted for around half (51.4%) of all hospitalizations. The proportion of women hospitalized for HF (58.1%) was greater than that of men. Nearly half of the cohort (47.4%) had had a previous HF hospitalization during the previous year.
The most common comorbidity was hypertension (60.3%). About one-third of the patients had diabetes mellitus (35.4%), and dyslipidemia (30.1%). The proportion of coronary artery disease was 38.2%, and one-tenth (10.7%) had had a previous myocardial infarction. Codes defining atherosclerosis risk factors increased significantly over the study period (P for trend < 0.001 for each of hypertension, diabetes, and dyslipidemia). However, the proportion of coronary artery disease as a comorbidity was relatively unchanged. The proportion of rheumatic valvular heart disease as a comorbidity decreased, but those of non-rheumatic valvular heart diseases, cardiomyopathies, and atrial fibrillation increased. The proportions of several other comorbidities and complications, including renal failure, anemia, and pneumonia increased.
HF hospitalization rate per 100,000 beneficiaries
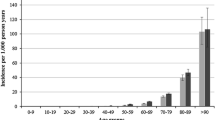
Table 2 shows the numbers and annual rates of HF hospitalization from 2008 to 2013. Between 2008 and 2013, there was an increase in the number of annual hospitalizations from 61,594 to 80,246, respectively (an increase of 30.3%), number of patients from 43,326 to 55,864 per year, respectively (an increase of 28.9%), and the rate of HF hospitalization from 138 to 168 per 100,000 beneficiaries, respectively (an increase of 21.7%) (all P for trend < 0.001). After adjusting for age and sex, the trend of HF hospitalization rate was still significant (P for trend < 0.001). The increasing HF hospitalization rate was driven mostly by the patients under UCS. The oldest age group (≥ 80 years) had the highest HF hospitalization rate of 931 per 100,000 beneficiaries for the overall period. This group also had the most prominent upward trend in the number of hospitalizations, increasing from 8754 to 13,248 from 2008 to 2013 (an increase of 51.3%) (P for trend < 0.001 in Table 1). All age groups had significant upward trends in HF hospitalization rates, especially in age ≥ 80 group as shown in Fig. 2 (P for trend < 0.001 for all age groups). Hospitalization for HF was more common in females (188 per 100,000 female beneficiaries vs. 147 per 100,000 male beneficiaries) (Table 2), especially in those aged ≥ 60 years, and the HF hospitalization rates for both genders significantly increased (both P < 0.001).
Heart failure hospitalization rate per 100,000 beneficiaries stratified by age group between 2008 and 2013. All age groups had significantly upward trend for heart failure (HF) hospitalization rate per 100,000 beneficiaries. P-values for trend were < 0.001 for all age groups using linear trend across years by Poisson regression
In-hospital procedures and outcomes
The median HLOS was 3 days (IQR 1.9–5.0) (P for trend = 0.42) (Table 3). There were increasing trends in some procedural codes, including mechanical ventilator from 6.7 to 8.9% and echocardiography from 4.9 to 9.0% (both P for trend < 0.001). In-hospital mortality rate gradually declined from 4.4% in 2008 to 3.8% in 2013 (P for trend < 0.001) with modest change after adjusting for age and sex (P for trend < 0.001). The significant predictors of in-hospital mortality were the extreme age groups, (i.e., the youngest age category and the oldest age category), concomitant cerebrovascular disease, renal and liver failure, and the presence of codes for complications or organ support procedures, such as mechanical ventilator (Additional file 1: Table S2).
Rehospitalization rate
Overall, rehospitalization rates were 34% in 30 days and 73% in 1 year after discharge without a significant linear trend over study period (P = 0.186 and 0.084 for 1-month and 1-year rehospitalization rate, respectively) (Table 4). The median time for all-cause hospitalization after the index HF hospitalization was 37 days (IQR 12–105).
The most common cause for 30-day rehospitalization was HF, accounting for 42% of all the rehospitalizations. Other common coding groups for 30-day rehospitalization were coronary artery disease (9%) and other cardiovascular condition (10%). Non-cardiovascular conditions contributed to 39% of all the rehospitalization. The most common non-cardiovascular condition causing rehospitalization was renal failure (7%).
The 30-day HF rehospitalization rate was around 16% with a slight increase over the study period (P for trend = 0.001). The trend persisted after adjusting for sex and age (P for trend = 0.001). The 3-month and 1-year HF rehospitalization rates were 27 and 41%, respectively, without a significant linear trend. Most of the HF rehospitalizations occurred at a median time-after-discharge of 48 days (IQR 16–126).
The factors associated with 30-day HF rehospitalization are reported in Additional file 1: Table S3. The youngest age group was more likely to have subsequent HF rehospitalization (20.7 vs. 16.4% overall). Prior HF admission indicated greater risk for future HF rehospitalization (OR 3.35, 95% CI 3.29–3.42). Various cardiovascular and other comorbidities increased the chance of HF readmission such as previous MI (OR 1.92, 95% CI 1.87–1.96). Admission records coded with an echocardiography procedure had a significantly lower rate of 30-day HF rehospitalization (OR 0.65, 95% CI 0.63–0.68).
One-year mortality rate
One-year mortality rate significantly decreased from 31.8 in 2008 to 28.5% in 2012 (both unadjusted and age- and sex-adjusted P for trend < 0.001) (Table 4). Additional file 1: Table S4 shows the predictors of 1-year mortality. The oldest age group had nearly twice the risk of 1-year mortality (OR 1.93, 95% CI 1.85–2.01). Male had a slightly but significantly greater risk than female (OR 1.13, 95% CI 1.11–1.15). Dissimilar to in-hospital mortality, previous hospitalization for HF or myocardial infarction markedly increased the risk of 1-year mortality (OR 1.48, 95% CI 1.46–1.51 and OR 1.45, 95% CI 1.41–1.50, respectively). The mortality risk was lower for patients undergoing echocardiography (OR 0.75, 95% CI 0.73–0.78) and cardiac catheterization codes (OR 0.44, 95% CI 0.38–0.51).
Discussion
To the best of our knowledge, this is the first national population study of hospitalized HF patients in Thailand. Using routinely-collected claims data from three public health security schemes, we found increasing trends in both the number and HF hospitalization rate between 2008 and 2013, driven mostly by the elderly population. The HF hospitalization rate increased with age and was higher in female. The in-hospital and 1-year mortality rates improved slightly between 2008 and 2013. Nevertheless, one-third of these patient were rehospitalized within 1 month, and nearly half of these rehospitalizations were caused by recurrent HF.
The increasing HF hospitalization rate in Thailand is probably caused by a growing number of HF patients in Thai population. The number of elderly and the proportion of the older population in Thailand have been increasing rapidly [14]. HF is more common with increasing age; the elderly population has a higher prevalence of cardiovascular disease, particularly hypertension, valvular heart disease, and coronary heart disease, which can lead to HF. Aging by itself is also an important risk factor for developing HF [15]. Moreover, a sedentary lifestyle with insufficient physical activity and dietary change to a Western diet might lead to a greater prevalence of HF risk factors, such as obesity, diabetes mellitus, and hypertension [16, 17]. Conversely, improved public health care provisions might also contribute to an increase in access to health care services, including hospitalization. Evidenced by the same set of claims data, we observed an increase of 14.2% in any hospitalizations from 5,041,334 in 2008 to 5,757,022 admissions in 2013. However, more access to health care services in high-income countries (HICs) led to fewer hospitalizations due to chronic disease, including HF [18].
Epidemiologic data on HF in LMICs are scarce and are often based on patients hospitalized for acute HF. The true prevalence of HF patient and trends in this region remain unknown [16]. Between HICs, HF hospitalization rates and trends are discrepant. For example, decreasing HF hospitalization rates per population were observed in the United States of America (USA), England, France, and Ireland over a similar time period to the present study [19,20,21,22]. However, the crude HF hospitalization rates were increasing in Germany and Slovenia [23, 24] The differences in rates and trends between countries might be partially explained by heterogenous research methods to identify HF patients, healthcare provision accessibility, and dissimilarity in medical management. In chronic HF, guideline-directed medical therapy can substantially reduce hospitalization events and mortality rate, especially in those with reduced left ventricular ejection fraction [25]. However, these life-saving therapies are still underused even in HICs [26]. Health care policy and quality measurement might also affect the HF hospitalization rate [27].
The characteristics of HF patients in the present study are partly consistent with the Thai ADHERE study and ADHERE-Asia–Pacific study [5, 6], which demonstrated younger patient (mean age of 65 years compared to 72 years in USA [19] and reaching 80 years in some European countries) [21, 24]. Female was more prevalent (58%) in the present study with a higher HF hospitalization rate per population, especially in the older age group. However, other population-based studies in the USA and Singapore showed male had a comparable hospitalization rate [19, 28] or even a higher rate than that of female in France [21]. In the present study, the reasons for the higher HF hospitalization rate in women were not explored, but it was possibly due to the higher prevalence of diabetes and obesity in Thai women, which are risk factors for developing HF [17, 29]. About one-tenth of the hospitalizations had rheumatic heart disease as a comorbidity with a downward trend. In addition, hypertension, diabetes mellitus, and coronary artery disease showed an increasing trend over the study period. Therefore, these metabolic disorders increasingly contribute to HF similar to Western countries [30].
In the present study, the in-hospital mortality rate slightly declined over the study period. Despite of lower mean age, the in-hospital mortality rate was higher than that of a cohort from the United States (4.1 vs. 3.0%) [5]. In the present study, we found a higher rate of mechanical ventilator use (up to 8.9%), indicating a greater severity of HF, especially in the youngest group (age 18–40 years), which had the highest mortality rate of 5.3%. However, some studies from HICs in Europe reported higher mortality rates (6.7–9.3%) and longer HLOS [21, 23, 31] This was probably due to older HF patients. Cohorts of hospitalized HF in high-income Asian countries such as Japan and Korea also demonstrated longer HLOS and high mortality of 6.4 and 5.2%, respectively [32, 33]. Therefore, the lower mortality rate in the cohort from the United States might be partially explained by a much higher HF hospitalization rate in the USA, which probably included less severe patient and shorter HLOS, which might have resulted in post-discharge mortality or readmission instead [34].
In the present study, echocardiography was coded more frequently between 2008 and 2013, reaching 9.0% in 2013. However, this is a small proportion compared with 62–85% performed in Europe and the USA [5]. Echocardiography is the most useful single test for evaluating the cause of HF and guiding the recommended treatment [35]. Moreover, patients who underwent echocardiography during admission had a better 1-year survival rate and less HF hospitalization in the present study. Sonographer-driven echocardiographic study with web-based assessment is feasible and might be applied to hospitals in remote areas with limited cardiology services [36].
Compared to other conditions, patients hospitalized with HF have the highest rate of rehospitalization [1]. In the present study, the 30-day rehospitalization rate was 34%, which is higher than in HICs countries in which the rate was lower than one-third [21, 24, 37,38,39]. The most common cause of rehospitalization in the present study was the decompensation of HF, found in nearly half of the rehospitalizations, and this is a higher proportion compared to the one-third of rehospitalization found in other studies [1, 40]. However, the risk of HF rehospitalization is modifiable, and there is much room for improvement for HF care in Thailand. For example, neurohormonal blocker was prescribed in less than half of the hospitalized HF patients in the Thai ADHERE study [6]. The possible solutions are to optimize HF management and echocardiographic evaluation before discharge. Early follow-up visits for high-risk patients and implementation of guideline directed treatment with comprehensive management can be achieved by a multidisciplinary team [41, 42]. Appropriate health care policy and strategy are needed to implement these into real-world practice [37, 43].
In the present study, 1-year mortality rate improved over the study period and was 28.5% in 2013. However, this is still substantially higher than in HICs, which ranged from 8.9 to 23.6% [44,45,46,47]. This is consistent with International Congestive Heart Failure Cohort (INTER-CHF), which showed high variation in mortality rates in LMICs, including Southeast Asian countries [48]. The INTER-CHF also demonstrated the differences in HF medication and socioeconomic status affecting the outcome of HF patients. Other unmeasured factors, including health-care quality and accessibility along with environmental and genetic factors, might also play roles [48]. Moreover, implantable cardioverter defibrillator (ICD), which prevents sudden cardiac death in HF, is also underutilized in lower income Asian countries. Only 15% of eligible HF patients had an ICD implanted in Thailand according to the Asian Sudden Cardiac Death in Heart Failure (ASIAN-HF) registry [49].
Limitations
Several limitations of our study warrant discussion. First, the claims data did not include HF hospitalizations in some private hospitals because they do not participate in the public health security reimbursement program, which is mainly UCS. People with high social economic status or private health insurance might choose to be hospitalized in private hospitals even though they have public health protection coverage. Therefore, our analysis likely underestimates the national HF hospitalization rate. The extent of the lack of coverage of private hospitals in our data collection is difficult to estimate. Additionally, the outcomes of the patients hospitalized for HF in private hospitals not participating in the public health security program might be different from the present study possibly due to higher socioeconomic status or quality of care [50, 51]. Second, we identified the HF hospitalizations based on ICD codes without validation using clinical data. Despite auditing by the BCMA, coding misclassification or changing coding practices are possible. There is no existing validation study on HF hospitalization based on hospital discharge data in Thailand. Moreover, HF diagnosis may have been misclassified due to lack of expertise or resource limitation, especially in rural hospitals. These possibilities might be demonstrated by the low coding rate for echocardiography in the present study. Although, heart failure is a clinical syndrome, lack of echocardiographic study likely reduced the diagnostic accuracy for this condition. Third, the rehospitalization rate is probably underestimated because patients might have decided to receive treatment in a private hospital not covered by our data collection after the index HF hospitalization, thereby not being included in our data source. Fourth, there are insufficient data for the cause of death analysis mainly due to the non-specific causes of death given in death certificate data. Fifth, interpreting factors associated with the outcomes in the present study should be done with caution because these variables were determined by administrative database data. Furthermore, without the availability of clinical data to adjust for more confounders, there might be residual confounding of estimated associations, and we did not perform multivariable analysis given these limitations. Sixth, our HF hospitalization data do not represent the epidemiology of chronic HF, which should have a higher incidence. However, HF hospitalization rate can still reflect health and economic burden of this condition. Finally, our data from 2013 are considered quite old. Due to lengthy process in requesting the claim data and data linkage which involve many government offices, obtaining new dataset will take considerable amount of time. Moreover, the patient ID were encrypted, so combining the old requested data with the new data will be very complex task. Nevertheless, our study, as the first nationwide HF study in Thailand, would be an important reference to compare HF epidemiology and burden in Thailand and other low-to-medium income country in the future study.
Future perspectives
We are facing a HF epidemic, especially in LMICs, including Thailand. Optimizing modifiable cardiovascular risk factor control, particularly hypertension, is necessary to reduce HF hospitalizations [52]. However, there are the difference in the comorbidities and characteristics of HF patients between the Asian region and Western countries [30]. Prospective population-based studies of HF epidemiology are needed to understand the etiology and prognostic factors of HF in this region. Establishing registries and performing registry-based studies to evaluate the quality of evidenced-based HF treatment might help address the gaps and identify the opportunities to improve patient care for HF with reduced ejection fraction [26]. Nurse-led HF clinics with established protocols can reduce HF hospitalizations and mortality, especially in setting where the physician’s time is limited.53 Implementation of this kind of clinic also has the potential to create a network for patient transfers and the platform for research registries in the future.
Conclusion
In this national population study, there was a trend of increasing HF-hospitalized patients in Thailand from 2008 to 2013. The risk of HF hospitalization increased with age, and a greater proportion were female. In-hospital and 1-year mortality rates gradually improved during the study period. However, the 30-day HF rehospitalization rate remained high.
Availability of data and material
The datasets used in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CSMBS:
-
Civil Servant Medical Benefit scheme
- HIC:
-
High-income county
- HF:
-
Heart failure
- HLOS:
-
Hospital length of stay
- ICD:
-
Implantable cardioverter defibrillator
- ICD-9 CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD-10 TM:
-
The International Classification of Diseases, Tenth Revision, Thai modification
- LMIC:
-
Low- and middle- income country
- SSS:
-
Social Security Scheme
- TRCD:
-
Thai Civil Registration of Death
- UCS:
-
Universal Health Coverage scheme
References
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28.
Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355(3):260–9.
Kilgore M, Patel HK, Kielhorn A, Maya JF, Sharma P. Economic burden of hospitalizations of Medicare beneficiaries with heart failure. Risk Manage Healthc Policy. 2017;10:63–70.
Agbor VN, Ntusi NAB, Noubiap JJ. An overview of heart failure in low- and middle-income countries. Cardiovasc Diagn Ther. 2020;10(2):244–51.
Atherton JJ, Hayward CS, Wan Ahmad WA, Kwok B, Jorge J, Hernandez AF, et al. Patient characteristics from a regional multicenter database of acute decompensated heart failure in Asia Pacific (ADHERE International-Asia Pacific). J Cardiac Fail. 2012;18(1):82–8.
Laothavorn P, Hengrussamee K, Kanjanavanit R, Moleerergpoom W, Laorakpongse D, Pachirat O, et al. Thai Acute Decompensated Heart Failure Registry (Thai ADHERE). CVD Prev Control. 2010;5(3):89–95.
Tangcharoensathien V, Witthayapipopsakul W, Panichkriangkrai W, Patcharanarumol W, Mills A. Health systems development in Thailand: a solid platform for successful implementation of universal health coverage. Lancet. 2018;391(10126):1205–23.
Cahill TJ, Kharbanda RK. Heart failure after myocardial infarction in the era of primary percutaneous coronary intervention: Mechanisms, incidence and identification of patients at risk. World J Cardiol. 2017;9(5):407–15.
Knodel J, Teerawichitchainan B, Prachuabmoh V, Pothisiri W. The situation of Thailand’s older population: an update based on the 2014 Survey of Older Persons in Thailand. Research Collection School of Social Sciences [Internet]. 2015. https://ink.library.smu.edu.sg/soss_research/1948. Accessed on 6 May 2021.
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10): e1001885.
Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306(15):1669–78.
Number of Beneficiary in National Health Security Schemes of Thailand [Internet]. 2013 [cited 18 Feb 2015]. http://www.nhso.go.th/FrontEnd/page-contentdetail.aspx?CatID=NDY=.
Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4(1):87–90.
Aulino F. Narrating the future: population aging and the demographic imaginary in Thailand. Med Anthropol. 2017;36(4):319–31.
Lazzarini V, Mentz RJ, Fiuzat M, Metra M, O’Connor CM. Heart failure in elderly patients: distinctive features and unresolved issues. Eur J Heart Fail. 2013;15(7):717–23.
Lam CSP. Heart failure in Southeast Asia: facts and numbers. ESC Heart Fail. 2015;2(2):46–9.
Aekplakorn W, Chariyalertsak S, Kessomboon P, Assanangkornchai S, Taneepanichskul S, Putwatana P. Prevalence of diabetes and relationship with socioeconomic status in the Thai population: National Health Examination Survey, 2004–2014. J Diabetes Res. 2018;2018:1654530.
Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274(4):305–11.
Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National differences in trends for heart failure hospitalizations by sex and race/ethnicity. Circ Cardiovasc Qual Outcomes. 2017;10(7):e003552.
Brettell R, Soljak M, Cecil E, Cowie MR, Tuppin P, Majeed A. Reducing heart failure admission rates in England 2004–2011 are not related to changes in primary care quality: national observational study. Eur J Heart Fail. 2013;15(12):1335–42.
Gabet A, Juillière Y, Lamarche-Vadel A, Vernay M, Olié V. National trends in rate of patients hospitalized for heart failure and heart failure mortality in France, 2000–2012. Eur J Heart Fail. 2015;17(6):583–90.
Sugrue A, Smyth Y, Hennessy S, Crowley J. Temporal trends in hospitalisations for heart failure. Ir Med J. 2015;108(7):207–9.
Christ M, Störk S, Dörr M, Heppner HJ, Müller C, Wachter R, et al. Heart failure epidemiology 2000–2013: insights from the German Federal Health Monitoring System. Eur J Heart Fail. 2016;18(8):1009–18.
Omersa D, Lainscak M, Erzen I, Farkas J. Mortality and readmissions in heart failure: an analysis of 36,824 elderly patients from the Slovenian national hospitalization database. Wien Klin Wochenschr. 2016;128(7):512–8.
Komajda M, Böhm M, Borer JS, Ford I, Tavazzi L, Pannaux M, et al. Incremental benefit of drug therapies for chronic heart failure with reduced ejection fraction: a network meta-analysis. Eur J Heart Fail. 2018;20(9):1315–22.
Greene SJ, Butler J, Albert NM, DeVore AD, Sharma PP, Duffy CI, et al. Medical therapy for heart failure with reduced ejection fraction: the CHAMP-HF Registry. J Am Coll Cardiol. 2018;72(4):351–66.
Psotka MA, Fonarow GC, Allen LA, Joynt Maddox KE, Fiuzat M, Heidenreich P, et al. The hospital readmissions reduction program: nationwide perspectives and recommendations: a JACC: Heart Failure Position Paper. JACC Heart Fail. 2020;8(1):1–11.
Ng TP, Niti M. Trends and ethnic differences in hospital admissions and mortality for congestive heart failure in the elderly in Singapore, 1991 to 1998. Heart. 2003;89(8):865–70.
Aekplakorn W, Inthawong R, Kessomboon P, Sangthong R, Chariyalertsak S, Putwatana P, et al. Prevalence and trends of obesity and association with socioeconomic status in Thai adults: National Health Examination Surveys, 1991–2009. J Obes. 2014;2014: 410259.
Tromp J, Tay WT, Ouwerkerk W, Teng TK, Yap J, MacDonald MR, et al. Multimorbidity in patients with heart failure from 11 Asian regions: a prospective cohort study using the ASIAN-HF registry. PLoS Med. 2018;15(3): e1002541.
Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola V-P, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–36.
Youn JC, Han S, Ryu KH. Temporal trends of hospitalized patients with heart failure in Korea. Korean Circ J. 2017;47(1):16–24.
Sato N, Kajimoto K, Keida T, Mizuno M, Minami Y, Yumino D, et al. Clinical features and outcome in hospitalized heart failure in Japan (from the ATTEND Registry). Circ J. 2013;77(4):944–51.
Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand SL, et al. Trends in length of stay and short-term outcomes among medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303(21):2141–7.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Singh S, Bansal M, Maheshwari P, Adams D, Sengupta SP, Price R, et al. American Society of Echocardiography: remote echocardiography with web-based assessments for referrals at a distance (ASE-REWARD) study. J Am Soc Echocardiogr. 2013;26(3):221–33.
Bergethon KE, Ju C, DeVore AD, Hardy NC, Fonarow GC, Yancy CW, et al. Trends in 30-day readmission rates for patients hospitalized with heart failure: findings from the get with the guidelines-heart failure registry. Circ Heart Fail. 2016;9(6):e002594.
Chung JE, Noh E, Gwak HS. Evaluation of the predictors of readmission in Korean patients with heart failure. J Clin Pharm Ther. 2017;42(1):51–7.
Aizawa H, Imai S, Fushimi K. Factors associated with 30-day readmission of patients with heart failure from a Japanese administrative database. BMC Cardiovasc Disord. 2015;15:134.
Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355–63.
Ziaeian B, Fonarow GC. The prevention of hospital readmissions in heart failure. Prog Cardiovasc Dis. 2016;58(4):379–85.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147-239.
Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543–51.
Youn YJ, Yoo BS, Lee JW, Kim JY, Han SW, Jeon ES, et al. Treatment performance measures affect clinical outcomes in patients with acute systolic heart failure: report from the Korean Heart Failure Registry. Circ J. 2012;76(5):1151–8.
Tsuchihashi-Makaya M, Hamaguchi S, Kinugawa S, Yokota T, Goto D, Yokoshiki H, et al. Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J. 2009;73(10):1893–900.
Crespo-Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail. 2016;18(6):613–25.
Chang HY, Wang CC, Wu YW, Chu PH, Wu CC, Hsu CH, et al. One-year outcomes of acute decompensated systolic heart failure in Taiwan: lessons from TSOC-HFrEF Registry. Acta Cardiologica Sinica. 2017;33(2):127–38.
Dokainish H, Teo K, Zhu J, Roy A, AlHabib KF, ElSayed A, et al. Global mortality variations in patients with heart failure: results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. Lancet Glob Health. 2017;5(7):e665–72.
Chia YMF, Teng TK, Tan ESJ, Tay WT, Richards AM, Chin CWL, et al. Disparity between indications for and utilization of implantable cardioverter defibrillators in asian patients with heart failure. Circ Cardiovasc Qual Outcomes. 2017;10(11):e003651.
Kim SJ, Park EC, Kim TH, Yoo JW, Lee SG. Mortality, length of stay, and inpatient charges for heart failure patients at public versus private hospitals in South Korea. Yonsei Med J. 2015;56(3):853–61.
Akintoye E, Briasoulis A, Egbe A, Orhurhu V, Ibrahim W, Kumar K, et al. Effect of hospital ownership on outcomes of heart failure hospitalization. Am J Cardiol. 2017;120(5):831–7.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Strömberg A, Mårtensson J, Fridlund B, Levin LA, Karlsson JE, Dahlström U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: results from a prospective, randomised trial. Eur Heart J. 2003;24(11):1014–23.
Acknowledgements
The authors gratefully acknowledge the Central Office for Health Care Information, the National Health Security Office, and the Social Security Office for providing the patient data. The authors are indebted to Dr. Prapat Suriyaphol and Dr. Saowalak Hunnangkul for preparing the data for analysis. We also would like to thank Anthony C.S. Tan for the manuscript preparation and English editing.
Funding
This research was funded by Siriraj Research and Development Fund. The funding source did not have a role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
SJ MD designed the study, obtained reimbursement data and drafted the manuscript. KK provided input into study design, performed main statistical analyses and prepared all data. RK was involved in study design, data analysis and provided input into discussion. All authors have reviewed the manuscript and agreed to submit in the journal.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Siriraj Institutional Review Board (SIRB) reviewed the protocol and approved the study (ethics committee code SIRB 647/2556). This study has been granted an exemption from requiring consent due to the retrospective nature of the study. All methods were performed in accordance with the Declaration of Helsinki. All patient identities were encrypted from the data sources before being analyzed by investigators.
Consent for publication
Not applicable.
Competing interests
I declare that the authors have no competing interests that might be perceived to influence the result and/or discussion reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Table S1 (list of ICD code for grouping comorbidities and procedure) and Table S2 - S4 (Parameters associated with in-hospital mortality, 30-day rehospitalization and 1-year mortality).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Janwanishstaporn, S., Karaketklang, K. & Krittayaphong, R. National trend in heart failure hospitalization and outcome under public health insurance system in Thailand 2008–2013. BMC Cardiovasc Disord 22, 203 (2022). https://doi.org/10.1186/s12872-022-02629-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02629-2