Abstract
Background
The disparity between ST-segment and non-ST-segment elevation myocardial infarction without obstructive coronary artery (STE-MINOCA and NSTE-MINOCA) are unclear. Our study aims to compare the clinical features and outcomes in patients with STE-MINOCA and NSTE-MINOCA.
Methods
This cross-sectional study consecutively enrolled patients diagnosed with acute myocardial infarction (AMI) from January 2013 to January 2020. MINOCA were identified as angiographic stenosis < 50%. Clinical characteristics, angiographic features, and clinical outcomes of STE-MINOCA and NSTE-MINCOA were documented. The primary endpoint was composite events in the different time periods.
Results
A total of 1966 AMI patients were screened, 107 (5.4%) were diagnosed as MINOCA. Among, there were 34 (31.8%) of STE-MINOCA and 73 (68.2%) of NSTE-MINOCA. STE-MINOCA group were younger, had lower N-terminal pro-brain natriuretic peptide (NT-proBNP), and smaller left atrial diameter (P < 0.05). Dual antiplatelet therapy (DAPT) was more likely to be prescribed to STE-MINOCA patients (P = 0.015). During median follow-up time of 24.5 months, STE-MINOCA group also demonstrated lower risks for primary endpoint and cardiovascular-related (CVS) rehospitalization. In univariate Cox regression analyses, NSTE-MINOCA showed an increased risk of long-term primary endpoint (HR 2.57, 95 CI%: 1.10–6.02) and CVS-related rehospitalization (HR 3.14, 95% CI: 1.16–8.48). After adjusting for NT-proBNP and DAPT, NSTE-MINOCA remained an independent risk factor for CVS-related rehospitalization in long-term follow-up (HR 2.78, 95% CI: 1.03–7.49).
Conclusion
Although STE-MINOCA and NSTE-MINOCA patients showed similar clinical characteristics, NSTE-MINOCA group presented a worse long-term outcome mainly driven by CVS-related hospitalization which suggested that NSTE-MINOCA patients might also require prompt medical attention.
Similar content being viewed by others
Introduction
Myocardial infarction without obstructive coronary artery (MINOCA) is a distinctive entity differing from classic acute myocardial infarction (AMI) [1]. Previous literature reported a prevalence of MINOCA of 5%-15% [2,3,4,5]. AMI can be classified as ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI) according to the presentation of electrocardiogram (ECG) [6]. Generally, the main pathogenesis of classic AMI is the plaque disruption or erosion based on significant stenosis, subsequently forming a cascade thrombosis [7]. Likewise, MINOCA can also be categorized by ST-segments changes (STE-MINOCA and NSTE-MINOCA).
However, the mechanism of MINOCA was poorly understood. Several specific causes were proposed, including atherosclerotic causes (plaque rupture, plaque erosion) and non-atherosclerotic causes (epicardial coronary spasm, coronary microvascular dysfunction, coronary embolism, spontaneous coronary artery dissection, and supply–demand mismatch) [1]. For MINOCA, any causes leading to total occlusion of a coronary artery tend to have STEMI, or partial occlusion of arteries tend to have NSTEMI [7]. Reportedly, worse short-term outcome was observed in STEMI patients, and worse long-term outcome in NSTEMI patients [8, 9]. Consider the distinct pathophysiology in MINOCA, there were lack of evidence regarding the outcomes in patients with STE-MINOCA and NSTE-MINOCA.
Therefore, the purpose of our study was to investigate the characteristics and prognosis between STE-MINOCA and NSTE-MINOCA patients in Chinese population.
Methods
Definition
According to the “Fourth Universal Definition of Myocardial Infarction” criteria [6] acute myocardial infarction (AMI) was defined as follows: (1) detection of a rise or fall of cardiac troponin (cTn) with at least one value exceeding the 99th percentile upper reference limit. (2) clinical evidence of infarction evidenced by at least one of the following: a) symptoms of myocardial infarction. b) new ischemic electrocardiographic changes. c) development of pathological Q waves. d) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality. e) identification of a coronary thrombus by angiography. Nonobstructive coronary arteries on angiography were defined as any major epicardial vessels within 50% stenosis including normal coronary arteries (no angiographic stenosis), mild luminal irregularities (angiographic disease < 30% stenosis), and moderate coronary atherosclerotic lesions (stenosis > 30% but < 50%).
Thus, MINOCA was diagnosed as myocardial infarction with nonobstructive coronary artery stenosis and no specific alternate causes for above clinical presentations. In accordance with ST segments changes on electrocardiogram (ECG), MINOCA was classified as STE-MINOCA and NSTE-MINOCA.
To further characterize the pathological changes, the following features were assessed accordingly. Coronary thrombosis was identified as ground glass opacification or filling defect by coronary angiography, or detected by optical coherence tomography (OCT). Plaque disruption were determined by OCT as discontinuous cap of lipid plaque. Coronary spasm was considered as transient stenosis of angiographic artery or absence of stenosis after intracoronary administration of nitrates. Coronary slow flow was confirmed by corrected TIMI frame count.
Study population
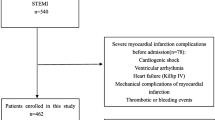
This is a cross-sectional study comprised of all consecutive patients with MINOCA in the First Affiliated Hospital of Nanjing Medical University from January 2013 to January 2020. Patients with conformed diagnosis of AMI according to guidelines [6] were eligible for this study. Among 1996 patients with AMI, 107 participants were diagnosed as MINOCA. Patients were further assigned to different group according to the presentation of ST-segments. Of those, 73 patients (68.2%) were diagnosed as NSTE-MINOCA, 34 patients (31.8%) were diagnosed as STE-MINOCA (Fig. 1).
Exclusion criteria were thrombolytic therapy prior to coronary angiography, women at pregnant or breastfeeding stage, presumed myocarditis, takotsubo syndrome, an expected survival time of less than one year due to any malignancy. Our study was approved by the independent ethical review board of the First Affiliated Hospital of Nanjing Medical University and in accordance with the Declaration of Helsinki. Written informed consents were obtained from all participants.
Data collection
Baseline characteristics including demographics, vitals at admission, medical history, and medication were collected. Blood samples were collected to assess high-sensitive cardiac troponin T (hs-cTnT) at the peak, total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), lipid protein a (Lp-a), alanine aminotransferase (ALT), aspartate aminotransferase (AST), uric acid (UA), serum creatinine (SCr), fasting blood glucose, glycate hemoglobin, N-terminal pro-brain natriuretic peptide (NT-proBNP), etc. The data of transthoracic echocardiography (TTE) and coronary angiography were documented.
In order to differentiate selected ambiguous cases of AMI, cardiac magnetic resonance imaging (CMRI) was used to exclude other potential causes, including myocarditis, takotsubo syndrome, and cardiomyopathies. Left ventriculography were performed to differentiate AMI from takotsubo syndrome. Intravascular ultrasound (IVUS) or OCT was applied to selective patients for insight etiology of plaque disruption or erosion.
Endpoint and follow-up
The primary endpoint was composite events in different time period. The in-hospital composite events included cardiac death, malignant arrhythmia, and heart failure (HF). The 1-year or long-term composite events were defined as all-cause mortality, HF, recurrence of AMI (re-AMI), cardiovascular-related (CVS) rehospitalization and stroke. And the secondary endpoint was each component of the primary outcome.
The diagnosis of HF is established according to the ESC guidelines for the management of HF. Malignant arrhythmia referred to tachyarrhythmia and bradyarrhythmia that required drug or medical equipment support. Re-AMI was defined as typical chest pain with dynamic change of ST-segments or T wave change on the ECG, or elevation of serum cTn level. Stroke referred to ischemic cerebral infarction or hemorrhagic stroke detected by computed tomography or magnetic resonance.
Patients were followed up from discharge through outpatient visit, inpatient chart review, and/or telephone interview every six months until the end of follow-up. The endpoint events were confirmed by reviewing of medical records or contacting with patients, their family members, and/or physicians.
Statistical analysis
Data distribution was assessed by Kolgormonov-Smirnov test. As cTnT, AST, NT-proBNP were tested as skewness distribution, therefore were presented as median with interquartile range (IQR) and compared by non-parametric Mann–Whitney U test. Numerical variables with normal distribution were presented as the mean ± standard deviation and were compared by independent sample student’s t-test. Categorical variables were calculated using counts and percentages and were evaluated by Chi-square test or Fisher exact test as appropriate.
The cumulative incidence was estimated by Kaplan–Meier (K-M) method and were compared using log-rank test. Cox proportional-hazards models were applied to calculate hazard ratios with and without adjustment. We included in the multivariable model only when variables showed P < 0.05 at univariate analysis. As NT-proBNP reflects the state of cardiac function, and dual antiplatelets therapy (DAPT) is the basic medication in patients with AMI. These variables were used as covariables in the model to identify independent risk factors for clinical endpoint in patients with MINOCA. A two-sided P < 0.05 was considered as statistical significance. All the analyses were performed using SPSS version 25 software.
Results
Baseline characteristics
Figure 1 showed the detailed flow chart of the study. Of the 1966 patients with AMI, 1859 (94.6%) having obstructive myocardial infarction: 1479 (79.6%) with STEMI and 380 (20.4%) with NSTEMI. There were 107 (5.4%) patients identified as MINOCA and median follow-up time was 24.5 (IQR:12.0–44.5) months.
Among the patients with MINOCA, 34 (31.8%) were categorized to STE-MINOCA and 73 (68.2%) were categorized to NSTE-MINOCA. The proportion of patients with NSTE-MINOCA was greater than that of patients with NSTEMI.
Table 1 showed the baseline clinical characteristics between two groups. Compared with patients with NSTE-MINOCA, patients with STE-MINOCA were younger (57.09 ± 13.73 vs 62.55 ± 11.80, P = 0.037), had lower NT-proBNP level (310[88–708] vs 575[143–1450], P = 0.038), and smaller left atrial diameter (LAD) (35.55 ± 3.68 vs 37.94 ± 5.25, P = 0.021). Gender, past medical history, other myocardial biomarkers, serum lipid profile, and TTE parameter were similar between groups (All P > 0.05).
Angiographic findings
Table 2 presented the angiographic features of patients with MINOCA. Approximately half of vessels showed normal or near normal artery in MINOCA patients (28 normal coronary artery and 24 minimal lumen irregularities) and proportion of angiographic severity had no significant difference in two groups. For the vessels with atherosclerotic plaque, similar proportion of single vessel lesions, two-vessels lesions, and three-vessels lesions were observed between groups.
The possible mechanism of MINOCA was identified as 3 (2.8%) for coronary thrombosis, 2 (1.9%) for plaque disruption, 10 (9.3%) for coronary spasm, and 18 (16.8%) for coronary slow-flow. Further evaluation including left ventriculography and OCT were rarely performed, only 5(4.7%) patients underwent left ventriculography, 3(2.8%) patients received OCT examination.
Medication at discharge
Medication regimen at discharge between groups were demonstrated in Fig. 2. Dual antiplatelet therapy (DAPT) consists of aspirin and P2Y12 receptor inhibitor. Aspirin, clopidogrel, and ticagrelor were more used in patients with STEMI numerically (P > 0.05). However, patients with NSTE-MINOCA were less likely to be prescribed DAPT on discharge (41.4% vs 66.7%, P = 0.015). There were no significant differences between groups on angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ACEI/ARB) (60.6% vs 47.9%, P = 0.227), non-dihydropyridine calcium channel blockers (NDHP-CCB) (48.5% vs 30.1%, P = 0.068), statins (87.9% vs 86.3%, P = 0.824) and beta receptor blockers (33.3% vs 45.2%, P = 0.251) (Fig. 2).
Clinical outcome between STE-MINOCA and NSTE-MINOCA
A total of 6 patients had in-hospital primary endpoint, including 1 (2.9%) for cardiac death, 3 (2.8%) for malignant arrhythmia, and 2 (1.9%) for acute HF. No significant difference was found between two groups.
In terms of 1-year outcome, patients with NSTE-MINOCA had higher rate of CVS-related rehospitalization (17.8% vs 2.9%, P = 0.035), but no significant difference in all-cause mortality, re-AMI, HF, and stroke compared with patients with STE-MINOCA.
There were 34 (31.8%) cases of primary endpoint occurring during the long-term follow-up in MINOCA patients, including 2 (1.9%) of all-cause mortality, 2 (1.9%) of re-AMI, 2 (1.9%) of HF, 3(2.8%) of stroke, and 27(25.2%) of CVS-related rehospitalization. There were no statistical differences in terms of long-term outcome between patients with STE-MINCOA and NSTE-MINOCA (Table 3).
Kaplan–Meier analysis showed that patients with NSTE-MINOCA had a trend of higher cumulative risks of composite endpoint and rehospitalization during the first year of follow-up, but log-rank test showed no statistical difference (Fig. 3). In addition, NSTE-MINOCA was statistically associated with higher risks for composite endpoint and CVS-related rehospitalization during long-term follow-up compared to STE-MINOCA (All P < 0.05).
Kaplan–Meier survival curve of STE-MINOCA and NSTE-MINOCA during one year and long-term follow-up. A Cumulative long-term primary endpoint risks between STE-MNOCA and NSTE-MINOCA. B Cumulative one-year primary endpoint risks between STE-MINOCA and NSTE-MINOCA. C Cumulative long-term cardiovascular-related rehospitalization risks between STE-MINOCA and NSTE-MINOCA. D Cumulative one-year cardiovascular-related rehospitalization risks between STE-MINOCA and NSTE-MINOCA
In a univariate Cox regression analysis, NSTE-MINOCA had higher increased risks for long-term primary endpoint (HR 2.57, 95 CI% 1.10–6.02) and CVS-related rehospitalization (HR 3.14, 95% CI: 1.16–8.48). In a multivariate analysis, adjusted for NT-proBNP and DAPT, NSTE-MINOCA retained a significantly higher hazard ratio for CVS-related rehospitalization in the long-term follow-up (HR 2.78, 95% CI: 1.03–7.49), but showed no significant difference in primary endpoint (HR 1.856, 95% CI:0.77–4.43) (Table 4).
Discussion
This study compared the clinical and prognostic disparity between STE-MINOCA and NSTE-MINOCA. While age, NT-proBNP, and LAD were shown significant between STE-MINOCA and NSTE-MINOCA groups, other clinical characteristics showed no statistical differences. Patients with MINOCA often showed coronary arteries with mild atherosclerosis, but intracoronary imaging or coronary functional examination for further etiology were seldom performed. Patients with STE-MINOCA were more likely to be prescribed DAPT. There were no significant differences in in-hospital primary endpoint between groups. However, NSTE-MINOCA presented a trend of worse clinical outcome in terms of composite events and CVS-related rehospitalization in the longer-term follow-up.
Previous studies demonstrated that demographic and clinical characteristics were comparable between MINOCA and AMI-CAD [3,4,5, 10]. Patients with MINOCA are often younger, female, and less comorbidity. Moreover, presentation of NSTE-MINOCA account for great proportion in all MINOCA cases. COAPT study showed that NSTE-MINOCA patients were more common in MINOCA (STE-MINOCA vs NSTE-MINOCA, 73.7% vs. 26.3%) [11]. Our studies presented a prevalence of MINOCA of 5.4% in all AMI cases, and 68.2% NSTE-MINOCA cases among the MINOCA cases, which consisted with the previous studies [4, 10].
Clinical features in patients with STEMI and NSTEMI were well established [8, 9]. Patients with NSTEMI are usually older, women, higher incidence of hypertension, diabetes mellitus, dyslipidemia, and renal dysfunction. Consistently, our results showed that NSTE-MINOCA shared similar clinical features with NSTEMI as younger age and lower level of NT-proBNP. However, there were no significant differences on gender, lipid profiles, and past medical history between STE-MINOCA and NSTE-MINOCA.
Lower than 50% angiographic stenosis defined as non-obstructive is somewhat arbitrary but pragmatic in clinical practice [1]. Visual estimation of lesion severity is variable by different clinical physicians, it is useful to categorize MINOCA into three degrees according to angiographic diameter stenosis with absolute normal artery, near normal artery (0–30%) and mild-moderate stenosis (30–50%) [1]. Montone et al. reported 54.8% near normal vessels in MINOCA subjects [4]. COAPT study also demonstrated that 63.2% of MINOCA patients had no angiographic evidence of CAD [11]. In our study, normal or near normal vessels accounted for 50.5% in all cases, which was close to the results of previous reports.
Plaque disruption occurred at the segments that appeared angiographically normal in approximately half of the MINOCA cases with rupture and/or ulceration [14]. While large plaque of coronary artery was associated with poorer prognosis [13], these vessels with mild to moderate stenosis are recommended to perform functional coronary tests or intracoronary examinations to determine the specific etiology for MINOCA [1]. However, these specific intracoronary inspections such as IVUS or OCT were insufficiently performed to patients with MINOCA [1]. Previous studies reported that OCT or IVUS was seldom performed due to its high financial burden [1, 4]. Likewise, although only three patients underwent OCT examination in our study, all patients have positive findings, of which, 2 were identified as plaque disruption and 1 was recognized as coronary white-thrombosis attached to vessel wall. For patients with MINOCA, intracoronary examinations are crucial to seek underlying mechanisms and to guide the optimal management.
For traditional AMI patients, secondary prevention medications (includes DAPT, statins, ACEI/ARB, and β-blockers) are strongly recommended [7]. On the contract, application of the secondary prevention therapy to patients with MINOCA remain controversial. A study from SWEDEHEART registry reported that DAPT might not be beneficial for patients with MINOCA [15]. Paolisso et al. showed that the use of DAPT and β-blockers were not associated with long-term prognosis [16]. However, MINOCA patients with explicit plaque disruption should be considered to receive anti-platelet agents [15]. As mentioned above, 38% of MINOCA patients had coronary plaque disruption found by OCT. One small study demonstrated that patients of ACS with plaque erosion receiving dual anti-platelet agents alone without stenting showed an acceptable outcome [17], which meant, to some extent, DAPT may have beneficial effects to patients with coronary plaque disruption. This emphasizes that intracoronary imaging is conducive to guide medication use and to optimize these patients’ prognosis.
We observed that STE-MINOCA patients were more likely to be discharged with aspirin or DAPT than NSTE-MINOCA in our study. Due to lack of guidelines of MINOCA managements, decision of anti-platelet therapy is challenging [16]. Thus, adopting anti-platelet therapies to STE-MINOCA patients was more crucial and easier to than NSTE-MINOCA.
Approximately 25% of patients with MINOCA will experience recurrent angina in the subsequent one year affecting patients’ quality of life [19]. In terms of clinical outcomes, previous studies indicated that the in-hospital mortality rate of MINOCA was quite low. While our study observed only 1 (0.9%) in-hospital death in 107 patients, ACTION-GWTG study showed similar in-hospital death rate of 1.1% in 19,000 patients with MINOCA. While our study observed only 1 (0.9%) in-hospital death in 107 patients, However, a meta-analysis demonstrated that 1-year mortality rate was risen up to 4.7%. Furthermore, SWEDEHEART study showed the long-term mortality rate of 13.4%, re-AMI of 7.1% and rehospitalization of 10%. And our results presented long term mortality rate of 2.9% and rehospitalization rate of 25.2%. It was reported that these substantial recurrence events were more frequent in MINOCA patients than in general population [1].
A study of Danish cohort, NSTEMI patients showed poorer outcome in multivariate analysis [8]. Spanish cohort study presented that higher 7-year survival rate was observed in the cohort of NSTEMI compared with the cohort of STEMI [18]. However, Hyun-Woong et al. reported worse early clinical outcome in patient with STEMI and more late-term favorable outcome in patients with NSTEMI [9]. As it shown in our study, STE-MINOCA appeared to show better outcome than NSTE-MINOCA during long-term follow-up, whereas no significant difference in 1-year follow-up. In this sense, MINOCA was not benign, especially for NSTE-MINOCA. In conclusion, recognizing these different characteristic of various AMI types is curial for the optimal management. Intravascular assessment could provide important evidence in such aspect and should be considered in MINOCA patients.
There are several limitations in current study. Firstly, use of CMR is strongly encouraged to exclude alternative diagnoses, however CMR examinations were seldom performed in our study, which may influence the accuracy of diagnosis of MINOCA. Secondly, approximately half of patients had mild to moderate atherosclerosis in this study, further examination assisting differentiation such as fractional flow reserve (FFR) testing to explore functional significant stenoses were no included. Also, intracoronary imaging to identify the possible pathological changes of plaque disruption and/or erosion were seldomly perform. Additionally, retrospective design, single-center study and small size may contribute a bias in present study.
Conclusion
Our study indicates that NSTE-MINOCA accounted for approximately two-thirds of MINOCA. Compared with STE-MINOCA, NSTE-MINOCA seemed to be associated with worse long-term clinical outcomes, which was mainly driven by CVS-related hospitalization.
Availability of data and materials
The data analyzed in this study are not publicly available due to the privacy policy of the hospital but are available from the corresponding author on reasonable request.
Abbreviations
- STE-MINOCA:
-
ST-segment elevation myocardial infarction without obstructive coronary artery
- NSTE-MINOCA:
-
Non-ST-segment elevation myocardial infarction without obstructive coronary artery
- AMI:
-
Acute myocardial infarction
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- DAPT:
-
Dual antiplatelet therapy
- CVS:
-
Cardiovascular
- HR:
-
Hazard ratio
- ECG:
-
Electrocardiogram
- OCT:
-
Optical coherence tomography
- hs-cTnT:
-
High-sensitive cardiac troponin T
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- LDL-C:
-
Low-density cholesterol
- HDL-C:
-
High-density cholesterol
- Lp-a:
-
Lipid protein a
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- UA:
-
Uric acid
- SCr:
-
Serum creatinine
- CMRI:
-
Cardiac magnetic resonance imaging
- IVUS:
-
Intravascular ultrasound
- HF:
-
Heart failure
- re-AMI:
-
Recurrence of AMI
- IQR:
-
Interquartile range
- LAD:
-
Left atrial diameter
- ACEI:
-
Angiotensin-converting enzyme inhibitors
- ARB:
-
Angiotensin receptor blockers
- NDHP-CCB:
-
Non-dihydropyridine calcium channel blockers
- CAD:
-
Coronary artery disease
- FFR:
-
Fractional flow reserve
References
Tamis-Holland JE, Jneid H, Reynolds HR, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation. 2019;139(18):e891–908.
Smilowitz NR, Mahajan AM, Roe MT, et al. Mortality of myocardial infarction by sex, age, and obstructive coronary artery disease status in the ACTION registry-GWTG (acute coronary treatment and intervention outcomes network registry-get with the guidelines). Circ Cardiovasc Qual Outcomes. 2017;10(12):e003443.
Safdar B, Spatz ES, Dreyer RP, et al. Presentation, clinical profile, and prognosis of young patients with myocardial infarction with nonobstructive coronary arteries (MINOCA): results from the VIRGO study. J Am Heart Assoc. 2018;7(13):e009174.
Abdu FA, Liu L, Mohammed AQ, et al. Myocardial infarction with non-obstructive coronary arteries (MINOCA) in Chinese patients: clinical features, treatment and 1 year follow-up. Int J Cardiol. 2019;287:27–31.
Barr PR, Harrison W, Smyth D, Flynn C, Lee M, Kerr AJ. Myocardial infarction without obstructive coronary artery disease is not a benign condition (ANZACS-QI 10). Heart Lung Circ. 2018;27(2):165–74.
Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–64.
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery [published correction appears in Circulation. 2016 Sep 6;134(10):e192–4]. Circulation. 2016;134(10):e123–e155.
Terkelsen CJ, Lassen JF, Nørgaard BL, et al. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J. 2005;26(1):18–26.
Park HW, Yoon CH, Kang SH, et al. Early- and late-term clinical outcome and their predictors in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction. Int J Cardiol. 2013;169(4):254–61.
Pasupathy S, Air T, Dreyer RP, et al. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries [published correction appears in Circulation. 2015 May 12;131(19):e475]. Circulation. 2015;131(10):861–870.
Bainey KR, Welsh RC, Alemayehu W, et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA): Insights from the Alberta contemporary acute coronary syndrome patients invasive treatment strategies (COAPT) study. Int J Cardiol. 2018;264:12–7.
Reynolds HR, Srichai MB, Iqbal SN, et al. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation. 2011;124(13):1414–25.
Emond M, Mock MB, Davis KB, et al. Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1994;90(6):2645–57.
Iqbal SN, Feit F, Mancini GB, et al. Characteristics of plaque disruption by intravascular ultrasound in women presenting with myocardial infarction without obstructive coronary artery disease. Am Heart J. 2014;167(5):715–22.
Lindahl B, Baron T, Erlinge D, et al. Medical therapy for secondary prevention and long-term outcome in patients with myocardial infarction with nonobstructive coronary artery disease. Circulation. 2017;135(16):1481–9.
Paolisso P, Bergamaschi L, Saturi G, et al. Secondary prevention medical therapy and outcomes in patients with myocardial infarction with non-obstructive coronary artery disease. Front Pharmacol. 2020;10:1606.
Xing L, Yamamoto E, Sugiyama T, et al. EROSION Study (effective anti-thrombotic therapy without stenting: intravascular optical coherence tomography-based management in plaque erosion): a 1-year follow-up report. Circ Cardiovasc Interv. 2017;10(12):e005860.
García-García C, Subirana I, Sala J, et al. Long-term prognosis of first myocardial infarction according to the electrocardiographic pattern (ST elevation myocardial infarction, non-ST elevation myocardial infarction and non-classified myocardial infarction) and revascularization procedures. Am J Cardiol. 2011;108(8):1061–7.
Grodzinsky A, Arnold SV, Gosch K, et al. Angina frequency after acute myocardial infarction in patients without obstructive coronary artery disease. Eur Heart J Qual Care Clin Outcomes. 2015;1(2):92–9.
Acknowledgements
The authors thank Dr. Shengen Liao (The First Affiliated Hospital of Nanjing Medical University) for valuable advice on statistical analysis.
Funding
This paper was funded by “Natural Science Foundation of Jiangsu Provincial (BK2012648 to Hui Wang)” and “General Scientific Research Project of Jiangsu Provincial Health Commission (M2020083)”. The funding body played no role in the design, writing or decision to publish this paper.
Author information
Authors and Affiliations
Contributions
ML: Conceptualization, methodology, investigation, formal analysis and writing-original draft. XK: Validation and supervision. HW: Conceptualization and investigation. YH: Formal analysis and writing-review and editing. IC: Writing-review and editing. YL: Data curation. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Our study was approved by the independent ethical review board of the First Affiliated Hospital of Nanjing Medical University and complied with the Declaration of Helsinki. Written informed consents were obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, M., He, Y., Cheang, I. et al. Clinical characteristics and outcome in patients with ST-segment and non-ST-segment elevation myocardial infarction without obstructive coronary artery: an observation study from Chinese population. BMC Cardiovasc Disord 22, 21 (2022). https://doi.org/10.1186/s12872-021-02359-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02359-x