Abstract
Background
The development of metabolic syndrome (MS) augments risk for atherosclerotic cardiovascular disease (CVD), but pathophysiological mechanisms of this relation are still under discussion. Overlapping CVD risk factors make it difficult to assess the importance of individual elements. This study aimed to analyze subclinical atherosclerosis based on arterial structure and function parameters in patients with MS and different triglycerides levels.
Methods
Patients (aged 40–65 years) were divided into two groups: patients with MS and with or without hypertriglyceridemia (hTG). Noninvasive assessment of vascular parameters—aortic augmentation index adjusted for heart rate 75 bpm (AIxHR75), pulse wave velocity (PWV), and common carotid artery intima-media thickness (cIMT) were performed.
Results
Carotid-femoral PWV (cfPWV) and carotid-radial PWV (crPWV) were significantly higher in patients with hTG. After adjusting for age, gender, waist circumference, fasting glucose, smoking status, cardiovascular family history and mean arterial pressure, crPWV (OR 1.150; CI 95% 1.04–1.28), cfPWV (OR 1.283; CI 95% 1.14–1.42) and cIMT (OR 1.13; CI 95% 1.02–1.25) were significantly associated with hTG (p < 0.05), while AIxHR75 did not show significant association.
Conclusion
Increased triglycerides are independently associated with a cfPWV, crPWV, and cIMT and may modify CVD risk in patients with MS.
Similar content being viewed by others
Background
The metabolic syndrome (MS) is a cluster of obesity-associated cardiovascular risk factors including abdominal obesity, impaired glucose tolerance, hypertriglyceridemia (hTG), decreased high-density lipoprotein cholesterol (HDL-C), and increased blood pressure. Each component of the MS is an independent risk factor for cardiovascular disease (CVD) and the development of MS augments risk for type 2 diabetes mellitus and atherosclerotic CVD [1].
The discussion of MS remains to determine whether a single underlying pathophysiological substrate exists that consolidates the MS components or it involves multiple etiologic mechanisms. The pathophysiological mechanism by which the MS increases cardiovascular risk also remains under debate. In recent years the link between MS and atherosclerosis has been analyzed increasingly. Studies have shown that the increased grade of obesity and MS score are associated with accelerated atherosclerosis and a greater incidence of coronary heart disease [2]. Patients with MS have an approximately twofold increased risk for myocardial infarction [3]. It is often stated that insulin resistance is a basic component of MS [4]. Insulin resistance could promote atherosclerosis through mechanisms that involve systemic factors, such as dyslipidaemia, hypertension, and a proinflammatory state, also through the mechanisms at the cellular level [5, 6]. During the last decades, interleukin-1 (IL-1) family were significantly associated with the initiation and progression of obesity-induced insulin resistance [7]. High-sensitivity C-reactive protein (hsCRP) were associated with future insulin resistance in non-diabetic adults [8]. Clear evidence indicates that cytokines, for instance, adipokines, hepatokines, inflammatory cytokines (IL-1, IL-6), myokines, and osteokines, contribute substantially to the development of abnormal glucose and lipid metabolism [9].
Nevertheless, other components of MS, such as triglycerides (TG) also are important. There is no doubt that TG is a residual, modifiable, and causal atherosclerotic CVD risk factor [10]. However, the assessment of the relationship between TG and CVD remains controversial due to the coincidence of TG with other risk factors.
Therefore, the aim of the present study was to analyze subclinical atherosclerosis (for carotid artery intima-media thickness—cIMT) and arteriosclerosis (for pulse wave velocity—PWV) in high-risk patients with MS and different TG levels.
Methods
All patients included in this community-based cross-sectional study were recruited from the Lithuanian High Cardiovascular Risk (LitHiR) primary prevention program. Methods are taken from LitHiR program methodology. A detailed description of the LitHir program protocol is presented elsewhere [11].
Study design
The inclusion criteria were: men and women age between 40 and 65 years without overt cardiovascular disease (see exclusion criteria), diagnosed with MS, who were investigated between 2006 and 2015 years in Vilnius University Hospital Santaros klinikos. The study protocol has been priorly approved by the Lithuanian Bioethics Committee. Informed consent was waived by Lithuanian Bioethics Committee due to the retrospective study design.
The exclusion criteria were: (a) proved (clinically evident) coronary heart disease: myocardial infarction or unstable angina, angina on effort with positive stress test results, coronary pathology found on coronary angiography or multislice computed tomography angiography, coronary artery bypass grafting, or angioplasty, acute coronary events in the past; (b) proved (clinically evident) cerebrovascular disease: acute cerebrovascular events in the past or proved stenoses in the carotid arteries; (c) proved (clinically evident) peripheral artery disease: acute ischaemic syndrome, proved chronic ischaemia in limbs, aortic aneurism; (d) end-stage oncological disease; (e) any other end-stage somatic disease.
The MS was defined according to the revised National Cholesterol Education Program Adult Treatment Panel III (NCEP ATPIII) criteria, meeting three or more criteria: waist circumference ≥ 102 cm in men and ≥ 88 cm in women; systolic blood pressure (SBP) ≥ 130 mmHg and/or diastolic blood pressure (DBP) ≥ 85 mmHg, or if the diagnosis of hypertension was documented in the medical record; fasting plasma glucose ≥ 100 mg/dL or type 2 diabetes mellitus; TG concentration ≥ 150 mg/dL or special treatment is administered to reduce TG concentration; HDL-C < 40 mg/dL in men, < 50 mg/dL in women [12]. All patients were categorized into two groups: patients with MS and hTG (TG > 200 mg/dL) and a control group – patients without hTG (TG < 150 mg/dL).
Study variables
All participants filled in the structured questionnaire about demographic and social characteristics, including age, cardiovascular family history, and smoking (see in Additional file 1). All the patients underwent measurements of height, weight, waist circumference, and arterial blood pressure. Waist circumference was measured midway between the top of the hip bone and the bottom of the ribs. Body mass index (BMI) was calculated as body weight (kg) divided by height (m) squared. Arterial hypertension was determined when SBP was ≥ 140 mmHg and/or DBP was ≥ 90 mmHg, or diagnosis of hypertension was documented in a medical record [13]. All the patient’s laboratory tests were performed in the morning after 12 h of fasting, and the following variables were determined: total cholesterol (TC), low-density lipoprotein cholesterol, (LDL-C), HDL-C, TG, and fasting glucose (FG).
Non-invasive assessment of arterial stiffness
The participants were refrained from eating and drinking alcohol, coffee, or tea for at least 12 h before the study. The test of arterial stiffness was performed in the supine position in a quiet, temperature-controlled room (22–24 °C). PWV was determined by measuring the carotid-to-radial (crPWV) and carotid-to-femoral (cfPWV) pulse wave transit time. Carotid-radial or carotid-femoral pulse waves were obtained non-invasively by applanation tonometry using high-fidelity micromanometer (Sphygmocor (v.7.01) AtCor Medical Pty. Ltd 1999–2002, Sydney, Australia). Pulse waves obtained consecutively from the radial or femoral and carotid arteries were referenced to a simultaneously recorded ECG, and transit time was computed from the time difference between the carotid and radial or femoral waveforms. The distance between the surface markings of the sternal notch and the radial or femoral artery was used to estimate the difference in path length between the carotid and radial or femoral arteries, and PWV adjusted for mean blood pressure was calculated. Aortic augmentation index (AIx) adjusted for heart rate 75 bpm (AIxHR75) was calculated from radial pulse waves of the non-dominant arm [14, 15]. Validated transfer function from peripheral pulse wave analysis was used to generate a corresponding central waveform. From this, aortic AIx was calculated by using the integrated software. The systolic part of the central arterial waveform is characterized by two pressure peaks. The first peak is caused by left ventricular ejection, whereas the second peak is a result of pulse wave reflection. The difference between both pressure peaks reflects the degree to which central arterial pressure is augmented by wave reflection. AIx, a measure of systemic arterial stiffness, is calculated as the difference between the second and first systolic peaks expressed as a percentage of the pulse pressure [16]. Blood pressure was recorded in the left arm using an automatic blood pressure monitor (HEM-757; Omron Corporation, Kyoto, Japan).
Carotid artery ultrasound examination
Carotid artery ultrasound examination was performed with high-resolution ArtLab Esaote (Italy) ultrasonic apparatus with an automatic Wall Tracing System, which consists of multiple sensors (Doppler signal in conjunction with a 128 Hz frequency radio wave signal). Before an examination, the patient lies on the back for 10 min. The sensor is placed on the outstretched neck and the optimal view of the carotid artery needs to be found. cIMT is measured in the common carotid artery 1–2 cm from the bifurcation on the bottom wall in a live two-dimensional view, which comprises 4 cm automatic recognition. The result is alive 6 s’ video clip together with ECG. Radiofrequency signal resolution is 0.21 μm.
Statistical analysis
Data were presented as numbers and frequencies with percentages for categorical variables, and mean ± standard deviation (SD) for continuous variables. Group differences were tested using Student’s t-tests because sample sizes were sufficiently large and the assumption of normality could be made according to the central limit theorem [17]. Multivariable logistic regression was used to identify associations of arterial parameters and hTG after adjusting for age, gender, waist circumference, FG, smoking status, and cardiovascular family history. Each of the four main arterial parameters (cfPWV, crPWV, AIxHR75, and cIMT av.) were included separately in the models to avoid collinearity. In each case, three types of models were constructed, unadjusted (Model 1), adjusted only for age and gender (Model 2), and adjusted for major risk factors (Model 3). Overall, 12 (4 × 3) different models were tested.
A P value < 0.05 was considered statistically significant. All analyses were done using STATISTICA software (version 10).
Results
A total of 1938 patients with MS were included in this study, 1041 of them had hTG (585 men, 52.24 ± 6.22 years). The basic characteristics of the study population are shown in Table 1. Significant differences were displayed in the levels of age, gender, weight, waist circumference, SBP and DBP, TC, LDL-C, DTL-C, FG, and smoking status between MS patients with hTG (> 200 mg/dL) and normal TG levels (< 150 mg/dL).
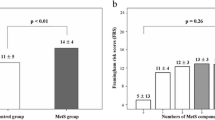
In hTG group the mean cfPWV was 8.74 ± 1.58 m/s, mean crPWV 9.24 ± 1.26 m/s, AIxHR75 21.21 ± 10.57, and average of cIMT was 666.36 ± 103.22 μm. As shown in Table 2, cfPWV, crPWV, and mean arterial pressure (MAP) were significantly higher in patients with hTG, while AIxHR75 was the lowest in this group. cIMT was the highest in the control group, but this finding was statistically insignificant. In a logistic regression analysis, both cfPWV and crPWV were significantly associated with hTG even in the model without adjustment for potentially influencing variables (Model 1). After adjusting for age, gender, waist circumference, FG, smoking status, cardiovascular family history and, MAP (Model 3), crPWV (OR 1.150; CI 95% 1.04–1.28), cfPWV (OR 1.283; CI 95% 1.14–1.42), and cIMT (OR 1.13; CI 95% 1.02–1.25) showed a significant association with hTG (p < 0.05). Similar associations were found after adjusting only for age and gender (Model 2). In the nonadjusted model (Model 1), AIxHR75 showed reversed association, but in adjusted models, the results were not significant. (Table 3).
Discussion
The main finding of the present study is that an increased TG was independently associated with a cfPWV, crPWV, and cIMT, but not with higher AIxHR75. PWV is a useful biomarker for the prediction of CVD risk [18]. It correlates well not only with the presence of coronary, cerebral, and carotid artery atherosclerosis but also with its extent [19]. An association between hTG and PWV has been shown previously [20,21,22]. The higher level of TG was demonstrated as an independent predictor of increased cfPWV [23]. The current study combines previous reports and shows that hTG could impact PWV in patients with MS. In our study, both crPWV and cfPWV were associated with hTG after adjusting for mean blood pressure, age, gender, waist circumference, FG, and more potentially influencing variables.
The relationship between TG and PWV could be mediated through left ventricular mass (LVM). TG is associated with LVM index in hypertensive patients, independently of other risk factors [24]. Whereas vascular stiffness induce left ventricular hypertrophy, PWV is a surrogate marker for LVM. To further enhance the predictive role of TGs, a recent study showed that TG and remnant cholesterol, but not LDL cholesterol, are associated with CVD outcomes [25]. AixHR75, as well as PWV, is an early marker of vascular changes in stiffness and elasticity and more useful in younger subjects. Although there is controversy about the prognostic role of Aix [26], a meta-analysis demonstrated that AIx75 is an independent predictor of future cardiovascular events and all-cause mortality [27]. The current study showed a disparity in aortic AIxHR75—the patients with lower TG levels had higher AIxHR75, but it disappeared after adjusted influencing variables. Obesity may be the key factor that mediates this relationship. In our study, more obese patients were in a control group, and their BMI was higher, though waist circumference was smaller. Although some studies are emphasizing central obesity [28], a meta-analysis confirmed the relationship between obesity/overweight and increased AIX without underestimating general obesity [29]. Moreover, increased pro-inflammatory factors (IL-6, TNF-α) may influence increased arterial stiffness [30, 31], while in our study they were not analyzed.
Several studies have shown an association between cIMT and future CVD events [32]. A longitudinal, 13 years follow-up study showed MS association with progression of cIMT, but only in those below 50 years of age [33]. Several studies have found that all single components of the MS may promote endothelial dysfunction leading to arterial injury. We also find an association between cIMT and TG level which appeared after adjusting for influencing variables.
Well-known factors leading to arterial stiffening are arterial hypertension, diabetes, and chronic kidney diseases. However, new promising research directions are mitochondrial oxidative stress, genome mutations, epigenetics, metabolism, and dyslipidemia [34]. Despite the fact that the correlation between fasting TG levels and cIMT remains controversial [35], there is growing evidence about hTG impact on oxidative stress and inflammation [36] which leads to the thickening of artery walls and atherosclerosis [23]. Limitations of the current analysis include the design and criteria of a preventive program. We could not carry out analyses of certain age groups and perform a follow-up. Moreover, the study includes only a Lithuanian population and the results cannot be directly applied to people of other nationalities. The strengths of this study include its large sample from a community-based population and adjustment for many covariates.
Conclusions
Higher TG is associated with cfPWV, crPWV, and cIMT but not with the AixHR75 in patients with MS. Whereas vascular changes are associated with an increased CVD risk, high TG may differentiate the prognosis of patients with MS.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to the fact that the LitHiR program is continued and the data is filled, but are available from the corresponding author on reasonable request.
Abbreviations
- AIX:
-
Aortic augmentation index
- AIxHR75:
-
Aortic augmentation index adjusted for heart rate 75 bpm
- BMI:
-
Body mass index
- CCA IMT:
-
Common carotid artery intima-media thickness
- cfPWV:
-
Carotid-femoral PWV
- crPWV:
-
Carotid-radial PWV
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- FG:
-
Fasting glucose
- HDL-C:
-
High-density lipoprotein cholesterol
- hTG:
-
Hypertriglyceridemia
- IMT:
-
Intima-media thickness
- LDL-C:
-
Low-density lipoprotein cholesterol
- MAP:
-
Mean arterial pressure
- MS:
-
Metabolic syndrome
- OR:
-
Odds ratio
- PWV:
-
Pulse wave velocity
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
References
Sperling LS, Mechanick JI, Neeland IJ, Herrick CJ, Després J-P, Ndumele CE, et al. The cardiometabolic health alliance: working toward a new care model for the metabolic syndrome. J Am Coll Cardiol. 2015;66(9):1050–67.
Grundy SM. Obesity, metabolic syndrome, and coronary atherosclerosis. Circulation. 2002;105(23):2696–8.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32.
Grundy SM. Metabolic syndrome update. Trends Cardiovasc Med. 2016;26(4):364–73.
Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14(5):575–85.
Lin D, Bridgeman MB, Brunetti L. Evaluation of alterations in serum immunoglobulin concentrations in components of metabolic syndrome, obesity, diabetes, and dyslipidemia. BMC Cardiovasc Disord. 2019;19(1):319.
Ballak DB, Stienstra R, Tack CJ, Dinarello CA, van Diepen JA. IL-1 family members in the pathogenesis and treatment of metabolic disease: focus on adipose tissue inflammation and insulin resistance. Cytokine. 2015;75(2):280–90.
Yan Y, Li S, Liu Y, Bazzano L, He J, Mi J, et al. Temporal relationship between inflammation and insulin resistance and their joint effect on hyperglycemia: the Bogalusa Heart Study. Cardiovasc Diabetol. 2019;18(1):109.
Shi J, Fan J, Su Q, Yang Z. Cytokines and abnormal glucose and lipid metabolism. Front Endocrinol (Lausanne). 2019;10:703.
Tada H, Nohara A, Kawashiri M. Serum triglycerides and atherosclerotic cardiovascular disease: insights from clinical and genetic studies. Nutrients. 2018;10(11):1789.
Llaucevicius A, Kasiulevičius V, Jatuzis D, Petrulioniene Z, Ryliskyte L, Rinkūnienė E, et al. Lithuanian High Cardiovascular Risk (LitHiR) primary prevention programme - rationale and design. Semin Cardiovasc Med. 2012;18:1–6.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–357.
Wilkinson IB, Cockcroft JR, Webb DJ. Pulse wave analysis and arterial stiffness. J Cardiovasc Pharmacol. 1998;32(Suppl 3):S33-37.
Kelly R, Hayward C, Avolio A, O’Rourke M. Noninvasive determination of age-related changes in the human arterial pulse. Circulation. 1989;80(6):1652–9.
O’Rourke MF, Gallagher DE. Pulse wave analysis. J Hypertens Suppl. 1996;14(5):S147-157.
Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23(1):151–69.
Zhong Q, Hu M-J, Cui Y-J, Liang L, Zhou M-M, Yang Y-W, et al. Carotid-femoral pulse wave velocity in the prediction of cardiovascular events and mortality: an updated systematic review and meta-analysis. Angiology. 2018;69(7):617–29.
Kim H-L, Kim S-H. Pulse wave velocity in atherosclerosis. Front Cardiovasc Med. 2019;6:41.
Zachariah JP, Rong J, Larson MG, Hamburg NM, Benjamin EJ, Vasan RS, et al. Metabolic predictors of change in vascular function: prospective associations from a community-based cohort. Hypertension. 2018;71(2):237–42.
Gottsäter M, Östling G, Persson M, Engström G, Melander O, Nilsson PM. Non-hemodynamic predictors of arterial stiffness after 17 years of follow-up: the Malmö Diet and Cancer study. J Hypertens. 2015;33(5):957–65.
Johansen NB, Vistisen D, Brunner EJ, Tabák AG, Shipley MJ, Wilkinson IB, et al. Determinants of aortic stiffness: 16-year follow-up of the Whitehall II Study. PLoS ONE. 2012;7(5):e37165.
Wang X, Ye P, Cao R, Yang X, Xiao W, Zhang Y, et al. Triglycerides are a predictive factor for arterial stiffness: a community-based 4.8-year prospective study. Lipids Health Dis. 2016;15:1–9.
Pietri P, Georgiopoulos G, Tsiachris D, Kordalis A, Vlachopoulos C, Vyssoulis G, et al. Triglycerides are related to left ventricular mass in hypertensive patients independently of other cardiometabolic risk factors: the effect of gender. Sci Rep. 2020;10(1):13253.
Castañer O, Pintó X, Subirana I, Amor AJ, Ros E, Hernáez Á, et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. 2020;76(23):2712–24.
Protogerou AD, Blacher J, Aslangul E, Le Jeunne C, Lekakis J, Mavrikakis M, et al. Gender influence on metabolic syndrome’s effects on arterial stiffness and pressure wave reflections in treated hypertensive subjects. Atherosclerosis. 2007;193(1):151–8.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31(15):1865–71.
Pal S, Radavelli-Bagatini S. Association of arterial stiffness with obesity in Australian women: a pilot study. J Clin Hypertens. 2013;15(2):118–23.
Li P, Wang L, Liu C. Overweightness, obesity and arterial stiffness in healthy subjects: a systematic review and meta-analysis of literature studies. Postgrad Med. 2017;129(2):224–30.
Pettersson-Pablo P, Cao Y, Breimer LH, Nilsson TK, Hurtig-Wennlöf A. Pulse wave velocity, augmentation index, and carotid intima-media thickness are each associated with different inflammatory protein signatures in young healthy adults: the lifestyle, biomarkers and atherosclerosis study. Atherosclerosis. 2020;313:150–5.
Tuttolomondo A, Pecoraro R, Buttà C, Di Raimondo D, Ferrante A, Della Corte V, et al. Arterial stiffness indexes and serum cytokine levels in seronegative spondyloarthritis: relationships between stiffness markers and metabolic and immunoinflammatory variables. Scand J Rheumatol. 2015;44(6):474–9.
Øygarden H. Carotid intima-media thickness and prediction of cardiovascular disease. J Am Heart Assoc. 2017;6(1):e005313.
Herder M, Arntzen KA, Johnsen SH, Mathiesen EB. The metabolic syndrome and progression of carotid atherosclerosis over 13 years. The Tromsø study Cardiovasc Diabetol. 2012;11:77.
Lacolley P, Regnault V, Laurent S. Mechanisms of Arterial Stiffening. Arterioscler Thromb Vasc Biol. 2020;40(5):1055–62.
Gao L, Bai L, Shi M, Ni J, Lu H, Wu Y, et al. Association between carotid intima-media thickness and fasting blood glucose level: a population-based cross-sectional study among low-income adults in rural China. J Diabetes Investig. 2017;8(6):788–97.
Le N-A. Postprandial triglycerides, oxidative stress, and inflammation. In: Apolipoproteins, triglycerides and cholesterol. 2020 Feb 25. https://www.intechopen.com/books/apolipoproteins-triglycerides-and-cholesterol/postprandial-triglycerides-oxidative-stress-and-inflammation
Acknowledgements
Our thanks go to all the patients and staff from Vilnius University Hospital Santaros klinikos who participated in this research.
Funding
No funding was received to assist with the preparation of this manuscript. LitHiR is a state-funded program.
Author information
Authors and Affiliations
Contributions
ER, VD, LR, and EM contributed to the literature search, study design, data analysis, data interpretation, and writing and editing of the article. RP contributed to the statistical analyses. JB, ŽP, AL, and RN contributed to the study design, data interpretation, and editing of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Lithuanian Bioethics Committee approved this study. Study data were collected from the Lithuanian High Cardiovascular Risk (LitHiR) primary prevention program. Only non-personally data was gathered. Informed consent was waived by Lithuanian Bioethics Committee due to the retrospective study design.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Study questionaire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rinkūnienė, E., Dženkevičiūtė, V., Petrulionienė, Ž. et al. Hypertriglyceridemia impact on arterial parameters in patients with metabolic syndrome. BMC Cardiovasc Disord 21, 393 (2021). https://doi.org/10.1186/s12872-021-02202-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02202-3