Abstract
Background
The metabolic syndrome (MetS) is associated with increased risk of cardiovascular disease. In this study, we examine if metabolic syndrome predicts progression of atherosclerosis over 13 years.
Methods
Participants were 1442 men and 1532 women in the population-based Tromsø Study who underwent carotid ultrasound examinations at baseline in the 4th (1994–5) and at follow-up in the 6th survey (2007–8). Of these, 278 men and 273 women fulfilled the criteria for the MetS, defined according to a modified version of the National Cholesterol Education Program Adult Treatment Panel III (NCEP, ATPIII). Carotid atherosclerosis was assessed as total plaque area (TPA) and mean intima-media thickness (IMT) at follow-up and as change in IMT and TPA from baseline to follow-up. Associations between MetS and its components and carotid atherosclerosis were assessed in linear regression models adjusted for age, total cholesterol and daily smoking, stratified by sex.
Results
IMT and TPA levels at follow-up (p < 0.0001) and progression of TPA (p = 0.02) were higher in the MetS group compared to the non-MetS group. In stepwise multivariable models, MetS was associated with TPA (β = 0.372 mm2, p = 0.009) and IMT (β = 0.051 mm, p < 0.0001) in men, and with IMT (β = 0.045 mm, p = 0.001) in women after 13 years of follow-up, but not with progression of IMT or TPA. In analyses stratified by age, MetS predicted progression of IMT (β = 0.043 mm, p = 0.046) and TPA (β = 1.02 mm2, p = 0.002) in men below 50 years of age. Hypertension was predictive of follow-up TPA and IMT in both genders and of progression of TPA in women. Impaired glucose tolerance was associated with follow up levels of IMT and TPA as well as progression in IMT in men. None of the other components of MetS were associated with progression of atherosclerosis.
Conclusions
Subjects with MetS had higher levels of IMT and TPA at follow up than those without MetS. Mets predicted progression of IMT and TPA in those below 50 years of age, but not in other age groups, indicating that MetS may be involved in the initiation of the atherosclerotic process.
Similar content being viewed by others
Metabolic syndrome (MetS) is a cluster of metabolic and non-metabolic cardiovascular risk factors, including insulin resistance, dyslipidaemia, visceral adiposity and hypertension. However, the pathophysiological basis and utility of MetS are debated, although several studies have shown associations between MetS and increased risk of cardiovascular disease (CVD)[1–7].
Atherosclerosis is the underlying process of a majority of cardiovascular disease and mortality. While the clinical manifestations of atherosclerosis usually do not occur until middle age, atherosclerosis develops early in life. Noninvasive ultrasonographic assessment of carotid intima-media thickness (IMT) and total plaque area (TPA) is suitable for evaluation of the burden of atherosclerosis, and are predictive of future risk of CVD. Although inter-correlated, measurements of IMT and TPA are thought to reflect different biological aspects of and stages in the development of atherosclerosis. Whereas TPA measures formed plaques, IMT can be measured where no focal disease is present. Both cross-sectional and prospective studies have shown association between MetS and IMT[1, 3, 8–10]. Data on associations between plaque measurements and MetS are scarce[6, 9, 11]. In a study on 166 members of the Canadian Oji-Cree community, a population with one of the world`s highest prevalence rates of the MetS, MetS was associated with IMT and total plaque volume after 7 years of follow-up[9]. In the prospective Bruneck study, subjects with MetS had higher progression of atherosclerosis as assessed by formation of new plaques and carotid stenosis[11]. In a cross-sectional study, plaque presence was associated with metS in women only[6].
In the prospective population-based Tromsø Study, we explored the relationship between MetS and progression of atherosclerosis in 2795 persons after 13 years. Information on MetS and cardiovascular risk factors were obtained at baseline. Carotid atherosclerosis, assessed as IMT, TPA and plaque number, was measured at baseline and at follow-up.
Subjects and methods
Subjects
The Tromsø Study is a longitudinal population-based health study with repeated surveys of the adult population in the municipality of Tromsø, Norway[12]. The study has been approved by the Regional Committee for Medical and Health Research Ethics, the Norwegian Directorate of Health and the Data Inspectorate.
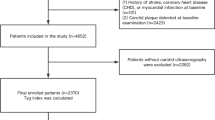
Subjects eligible for the present study were those who participated in ultrasound examination in the 4th (1994–1995) and 6th survey (2007–2008) of the Tromsø Study. The 4th survey consisted of two screening visits, and ultrasound examination of the carotid arteries was done at the 2nd visit. All inhabitants of Tromsø aged 55–74 years and random 5-10% samples of subjects in the age groups 20–54 years and 75–84 years were invited to the 2nd visit, and 6885 subjects attended (79% of the eligible population). Carotid ultrasound examination was performed in 6727 subjects. During follow-up, 1451 persons died and 486 moved from Tromsø. Forty-one subjects were excluded because they had withdrawn their written consent to further research. Of the remaining 4750 subjects who were still alive and living in Tromsø, 2974 subjects (62.6%) attended the carotid ultrasound examination in the 6th survey in 2007–2008, and were included in the present study. All included participants gave informed, written consent.
Baseline risk factors
At baseline, information on diabetes mellitus, use of insulin and/or anti diabetic drugs, smoking habits, history of cardiovascular diseases and treated hypertension (never/previous/current) were obtained from self-administered questionnaires. Height and weight were measured with subjects wearing light clothing and without shoes. BMI was calculated as weight in kilograms divided by squared height in meters (kg/m2). Waist circumference was measured at the umbilical line. Blood pressure was recorded three times at one-minute intervals after two minutes of seated resting with the use of an automatic device (Dinamap Vital Signs Monitor 1846, Criticon) and by specially trained technicians. The mean of the last two recordings was used in the report. Analyses of non-fasting serum total cholesterol and triglycerides were done using commercial kits. Serum high density lipoprotein (HDL) cholesterol was measured after the precipitation of lower-density lipoprotein with heparin and manganese chloride. The low density lipoprotein (LDL) concentration was calculated according to Friedewald’s formula: LDL-cholesterol = Total cholesterol – HDL-cholesterol – (0.45 x triglycerides) in 2961 subjects with triglyceride levels below 4.52 mmol/L. Lipid levels were measured twice with an interval of 4–12 weeks and the averages of these values were used in the analyses. Serum uric acid was measured by photometry with COBAS® instruments (Roche diagnostics, Switzerland) using an enzymatic colorimetric test, the uricase/PAP method. Glycosylated haemoglobin (HbA1C) levels were measured with a liquid chromatographic procedure. All analyses were performed at the Department of Clinical Chemistry, University Hospital of Northern Norway.
Definition of metabolic syndrome
MetS was defined according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP, ATPIII)[13]. According to this definition, the MetS is present when three or more of the following five criteria are fulfilled; abdominal obesity, hypertriglyceridemia, low HDL-cholesterol, hypertension, or elevated fasting glucose. Abdominal obesity is defined as waist circumference ≥ 102 cm in men and ≥ 88 cm in women. Hypertriglyceridemia is defined as elevated triglycerides ≥ 150 mg/dL (1.7 mmol/L) or self-reported lipid lowering drug treatment. Low HDL cholesterol is defined as < 40 mg/dL (1.0 mmol/L) for men and < 50 mg/dL (1.30 mmol/L) for women or self-reported lipid lowering drug treatment. As fasting glucose was not measured in the Tromsø Study, HbA1c ≥6.1% and/or non-fasting plasma glucose >11.1 mmol/L and/or self-reported diabetes and/or use of anti-diabetic medication was defined as impaired glucose tolerance. Hypertension was defined as elevated systolic blood pressure ≥ 130 mmHg, or diastolic blood pressure ≥ 85 mmHg, or self-reported current antihypertensive drug treatment[14].
Carotid ultrasound measurements
High-resolution B-mode ultrasonography at baseline was performed with Acuson Xp10 128, ART-upgraded duplex scanners equipped with 7.5 MHz linear array transducers, while GE Vivid 7 duplex scanners with linear 12 MHz transducers were used at follow-up[15]. Subjects were examined in the supine position with the head slightly tilted to the opposite side. No fixed angle of insonation was used; the sonographers were instructed to view the arteries from all possible angles, in order to find the optimal view for visualization of plaque and IMT in each subject. The far- and near walls of the right common carotid artery (CCA), bifurcation (bulb) and internal carotid artery (ICA) (six locations) were scanned for the presence of plaques. A plaque was defined as a localized protrusion into the vessel lumen with thickening of the vessel wall of more than 50% compared to the adjacent IMT. The outline of each plaque was marked manually on still images, with calculation of plaque area. In subjects with more than one plaque, TPA was calculated as the sum of all plaque areas. Semi-automated ECG-triggered measurement of IMT was performed in 10 mm segments of the far (CCA-FW-IMT) and near wall (CCA-NW-IMT) of the CCA and in the most proximal 10 mm far wall segment of the bulb (BULB-FW-IMT). Mean IMT from the 3 pre-selected images was calculated for each location. If present in the predefined location of interest, plaques were included in the IMT measurements. The average of mean IMT from the three locations was used in the analyses (hereafter referred to as IMT). Final reading of IMT and plaque area was done off line using the automated Artery Measurement System II[16]. The inter- and intra-observer and inter-equipment reproducibility of IMT and plaque measurements was acceptable[15, 17–19].
Statistical analysis
Stata SE 11 (StataCorp LP, College Station, TX, USA) and the SAS software, version 9, were used for all analyses. Differences between subjects with and without MetS were analyzed using t-test (continuous variables) Wilcoxon rank-sum test and χ ² (dichotomous variables). Values are presented as means (SD) or numbers (%). TPA was square-root-transformed to approximate normal distribution. Changes in IMT and square-root-transformed TPA were calculated by subtracting the value at baseline from the follow-up value (ΔIMT and ΔTPA). Linear regression models were fitted with IMT and TPA as dependent variables and MetS, age, total cholesterol and smoking as independent variables. Similarly, stepwise linear multivariable models with forward selection and significance level 0.05 for entry into the model were fitted with each component of the metabolic syndrome entered as separate independent variables, together with age, total cholesterol and smoking. Interaction with sex was examined with IMT and TPA as the dependent variable and sex, risk factor, and sex*risk factor as independent variables. There was significant interaction between sex and MetS in the IMT models, all analyses were therefore stratified by sex. Further adjustments were made for uric acid and use of lipid-lowering, anti-platelet and antihypertensive drugs at baseline and follow-up. Two-sided p-values < 0.05 were considered statistically significant.
Results
Baseline characteristics of the 273 women and 278 men who met the criteria for MetS are shown in Table 1. Women with MetS were older and fewer smokers than women without MetS. Subjects with MetS had increased IMT, more plaques and larger TPA at baseline (Table 1).
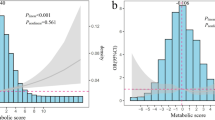
Mean observation time was 13.2 years. Follow-up levels of IMT and TPA were higher in subjects with MetS than in controls, most pronounced in those below 70 years of age. Change in IMT and TPA was associated with Mets only in those younger than 50 years (Table 2, Figures1 and2).
In stepwise multiple regression analysis, MetS was independently associated with follow-up IMT (β = 0.051 mm, p < 0.0001) and TPA (β = 0.372 mm2, p = 0.009) in men. MetS predicted follow-up IMT (β = 0.045 mm, p = 0.001) in women only (Table 3). In analyses stratified by age, MetS predicted progression of IMT (β = 0.043 mm, p = 0.046) and TPA (β = 1.02 mm2, p = 0.002) in men below 50 years of age, but not in the total population.
Uric acid level (log-transformed) was not independently associated with IMT or TPA in multivariable analyses, and further adjustment for uric acid did not change did not change the estimates. Adjustment for lipid-lowering, antiplatelet and antihypertensive treatment at follow-up weakened the relationship between MetS and follow-up levels of IMT and TPA, but not substantially.
In stepwise multivariable analyses with each component of the MetS entered separately and adjusted for age, LDL-cholesterol and smoking, hypertension was consistently associated with follow-up levels of TPA and IMT in both sexes and with progression of TPA in women (Table 4). Low HDL-cholesterol levels were associated with follow-up levels of IMT women. Impaired glucose tolerance was associated with follow-up levels of IMT and TPA and with progression of IMT in men. Hypertriglyceridemia was associated with follow up levels of IMT in both men and women, but not with progression. We found no association between abdominal obesity and IMT or TPA.
Discussion
The main finding of our study was that MetS was an independent predictor of follow-up IMT and TPA in men and women. MetS was an independent predictor of progression of IMT and TPA in subjects below 50 years of age, but not in other age groups.
Our finding of increased IMT in subjects with MetS after 13 years of follow-up is in line with results from previous cross-sectional studies[1, 3, 8, 9]. Longitudinal data are scarce. In a posthoc analysis on 2334 hypertensive patients in the European Lacidipine Study on Atherosclerosis (ELSA), progression of IMT was slightly greater in patients with MetS, but this was not significant after adjustment for other cardiovascular risk factors[20]. In our study, change in IMT and TPA was most pronounced in younger age groups. This is in line with the results from a population-based study of 1809 young Finns aged 32 ± 5 years, where MetS was associated with progression of IMT in subjects aged 24–39 years[10]. We found no association in the older age groups. This may indicate that MetS is more important for the early stages of the atherosclerotic process, a process which accelerates in the 4th to 5th decade. However, in a study on 102 elderly women, incident MetS predicted progression of IMT after 12-years follow-up[21].
Few studies have assessed the relationship between MetS and plaque measurements[6, 9, 11, 22]. In a multi-ethnic cross-sectional study, MetS and the number of MetS components was independently associated with plaque presence[22]. A prospective study on 166 Cree-Indians showed that MetS at baseline predicted follow-up levels of IMT, but not total plaque volume, a measure which is strongly correlated with TPA. However, change in IMT and total plaque volume was not assessed. In the Bruneck study, MetS was associated with 5-year change in atherosclerosis as assessed by novel plaque and stenosis formation[11].
Previous studies found no clear evidence that MetS predicted IMT progression better than expected from the sum of the individual components[10]. In our study, hypertension was the one component most consistently associated with follow-up levels of carotid atherosclerosis among men and women. Hypertension was also independently associated with progression of TPA in women. Impaired glucose tolerance was associated with follow up IMT and progression of IMT in men. In a systematic review, three of nine of cross-sectional studies found significantly larger IMT in subjects with impaired glucose tolerance[23]. Both low HDL-levels and hypertriglyceridemia were associated with follow-up levels of IMT and TPA, but not with progression of atherosclerosis.
Increased use of medication that may influence the atherosclerotic process during follow-up could have confounded our results. Use of lipid-lowering, antiplatelet and antihypertensive drugs increased during follow-up, most pronounced for use of lipid-lowering drugs (from 1.9% to 26.9%). The association between MetS and IMT and TPA was somewhat weakened with adjustment for use of medication at follow-up, but not substantially, and this could not explain the lack of association between MetS and progression of atherosclerosis.
In a previous study, serum uric acid level was associated with MetS and carotid atherosclerosis in patients diagnosed with diabetes mellitus type 2[24]. We found no independent association between serum uric acid and carotid atherosclerosis in our population-based study. Possible links between metabolic dysfunction and atherosclerosis may be secretion of adipokines by adipose tissue. Several adipokines have been reported to promote arterial stiffness, inflammation and atherosclerosis in subjects with diabetes and coronary heart disease[25–27]. Adipokines were not measured in the Tromsø Study.
In general, it is more difficult to detect associations between risk factors and change in atherosclerosis as opposed to single measurements[15, 28]. Measurements of progression of atherosclerosis are more prone to errors than single measurements because random measurement errors at baseline and follow-up are accumulated. This can attenuate the differences aimed to be detected, and may preclude the detection of a positive relationships between MetS and change in atherosclerosis as opposed to single measurement of atherosclerosis at follow-up.
Our study has some important limitations. As observed in many other large population-based epidemiological studies, the overall attendance rates of the Tromsø Study fell from 77% in 1994–1995 to 64% in 2007–8[12]. The attendance at follow-up was lower in those with MetS at baseline. During follow-up, the proportion that moved from Tromsø was lower in the MetS group compared to the non-MetS group (5.9% vs. 7.9%, p = 000.4), but this was by far outweighed by selection bias due to higher mortality in those with than without MetS (28.8% vs 19.6%, p <0.0001). Further selection bias may have occurred due to higher morbidity in the MetS group[12]. Furthermore, the attendance rates at follow-up were low in subjects ≥70 years, which calls for caution in making inferences about this group.
Conclusion
In conclusion, we found that MetS was associated with IMT and TPA levels at follow up. In analyses of the different components of MetS, hypertension showed the most consistent positive association with carotid atherosclerosis. MetS was associated with progression of IMT and TPA only in those below 50 years of age. The results may indicate that MetS may be involved in the initiation of the atherosclerotic process.
Abbreviations
- MetS:
-
Metabolic syndrome
- NCEP:
-
ATPIII (National Cholesterol Education Programme, Adult Treatment Panel III)
- TPA:
-
Total plaque area
- IMT:
-
Intima-media thickness
- HDL:
-
Serum high density lipoprotein
- HbA1C:
-
Glycosylated haemoglobin
- CCA:
-
Common carotid artery
- ICA:
-
Internal carotid artery
- CVD:
-
Cardiovascular disease
- CCA-FW-IMT:
-
Common carotid far wall intima-media thickness
- CCA-NW-IMT:
-
Common carotid near wall intima-media thickness
- AMS:
-
artery measurement system
- CV:
-
Coefficient of variation.
References
Ballantyne CM, Hoogeveen RC, McNeill AM, Heiss G, Schmidt MI, Duncan BB, Pankow JS: Metabolic syndrome risk for cardiovascular disease and diabetes in the ARIC study. Int J Obes. 2008, 32 (Suppl 2): S21-S24.
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT: The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002, 288 (21): 2709-2716. 10.1001/jama.288.21.2709.
Sipila K, Moilanen L, Nieminen T, Reunanen A, Jula A, Salomaa V, Kaaja R, Kukkonen-Harjula K, Lehtimaki T, Kesaniemi YA, et al: Metabolic syndrome and carotid intima media thickness in the Health 2000 Survey. Atherosclerosis. 2009, 204 (1): 276-281. 10.1016/j.atherosclerosis.2008.08.029.
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ: The metabolic syndrome. Lancet. 2010, 375 (9710): 181-183. 10.1016/S0140-6736(09)61794-3.
Guize L, Pannier B, Thomas F, Bean K, Jego B, Benetos A: Recent advances in metabolic syndrome and cardiovascular disease. Arch Cardiovasc Dis. 2008, 101 (9): 577-583. 10.1016/j.acvd.2008.06.011.
Iglseder B, Cip P, Malaimare L, Ladurner G, Paulweber B: The metabolic syndrome is a stronger risk factor for early carotid atherosclerosis in women than in men. Stroke. 2005, 36 (6): 1212-1217. 10.1161/01.STR.0000166196.31227.91.
Galassi A, Reynolds K, He J: Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. American J Med. 2006, 119 (10): 812-819. 10.1016/j.amjmed.2006.02.031.
Kawamoto R, Tomita H, Inoue A, Ohtsuka N, Kamitani A: Metabolic syndrome may be a risk factor for early carotid atherosclerosis in women but not in men. J of Atheroscl Thromb. 2007, 14 (1): 36-43. 10.5551/jat.14.36.
Pollex RL, Al-Shali KZ, House AA, Spence JD, Fenster A, Mamakeesick M, Zinman B, Harris SB, Hanley AJ, Hegele RA: Relationship of the metabolic syndrome to carotid ultrasound traits. Cardiovasc Ultrasound. 2006, 4: 28-10.1186/1476-7120-4-28.
Koskinen J, Kahonen M, Viikari JS, Taittonen L, Laitinen T, Ronnemaa T, Lehtimaki T, Hutri-Kahonen N, Pietikainen M, Jokinen E, et al: Conventional cardiovascular risk factors and metabolic syndrome in predicting carotid intima-media thickness progression in young adults: the cardiovascular risk in young Finns study. Circulation. 2009, 120 (3): 229-236. 10.1161/CIRCULATIONAHA.108.845065.
Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Bonadonna RC, Muggeo M: Carotid atherosclerosis and coronary heart disease in the metabolic syndrome: prospective data from the Bruneck study. Diabetes Care. 2003, 26 (4): 1251-1257. 10.2337/diacare.26.4.1251.
Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njølstad I: Cohort profile: The Tromsø Study. IntJ Epidemiol. 2011, e-pub ahead of print: 10.1093/ije/dyr049
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, et al: Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Curr Opin Cardiol. 2006, 21 (1): 1-6. 10.1097/01.hco.0000200416.65370.a0.
Borch KH, Braekkan SK, Mathiesen EB, Njølstad I, Wilsgaard T, Størmer J, Hansen JB: Abdominal obesity is essential for the risk of venous thromboembolism in the metabolic syndrome: the Tromsø Study. J Tromb Haemost . 2009, 7 (5): 739-745. 10.1111/j.1538-7836.2008.03234.x.
Herder M, Johnsen SH, Arntzen KA, Mathiesen EB: Risk factors for progression of carotid intima-media thickness and total plaque area. A 13-year follow-up study. The Tromsø Study. Stroke. 2012, 43 (7): 1818-1823. 10.1161/STROKEAHA.111.646596.
Liang Q, Wendelhag I, Wikstrand J, Gustavsson T: A multiscale dynamic programming procedure for boundary detection in ultrasonic artery images. Trans Med Imaging. 2000, 19 (2): 127-142. 10.1109/42.836372.
Joakimsen O, Bønaa KH, Stensland-Bugge E: Reproducibility of ultrasound assessment of carotid plaque occurrence, thickness, and morphology. The Tromsø Study. Stroke. 1997, 28 (11): 2201-2207.
Stensland-Bugge E, Bønaa KH, Joakimsen O: Reproducibility of ultrasonographically determined intima-media thickness is dependent on arterial wall thickness. The Tromsø Study. Stroke. 1997, 28 (10): 1972-1980. 10.1161/01.STR.28.10.1972.
Fosse E, Johnsen SH, Stensland-Bugge E, Joakimsen O, Mathiesen EB, Arnesen E, Njølstad I: Repeated visual and computer-assisted carotid plaque characterization in a longitudinal population-based ultrasound study: the Tromso study. Ultrasound Med Biol. 2006, 32 (1): 3-11. 10.1016/j.ultrasmedbio.2005.09.006.
Zanchetti A, Hennig M, Baurecht H, Tang R, Cuspidi C, Carugo S, Mancia G: Prevalence and incidence of the metabolic syndrome in the European Lacidipine Study on Atherosclerosis (ELSA) and its relation with carotid intima-media thickness. Hypertens. 2007, 25 (12): 2463-2470. 10.1097/HJH.0b013e3282f063d5.
Hassinen M, Komulainen P, Lakka TA, Vaisanen SB, Haapala I, Gylling H, Alen M, Schmidt-Trucksass A, Nissinen A, Rauramaa R: Metabolic syndrome and the progression of carotid intima-media thickness in elderly women. Arch Intern Med. 2006, 166 (4): 444-449.
Rundek T, White H, Boden-Albala B, Jin Z, Elkind MS, Sacco RL: The metabolic syndrome and subclinical carotid atherosclerosis: the Northern Manhattan Study. J Cardiometab Syndr. 2007, 2 (1): 24-29. 10.1111/j.1559-4564.2007.06358.x.
Brohall G, Oden A, Fagerberg B: Carotid artery intima-media thickness in patients with Type 2 diabetes mellitus and impaired glucose tolerance: a systematic review. Diabet Med. 2006, 23 (6): 609-616. 10.1111/j.1464-5491.2005.01725.x.
Li Q, Yang Z, Lu B, Wen J, Ye Z, Chen L, He M, Tao X, Zhang W, Huang Y, et al: Serum uric acid level and its association with metabolic syndrome and carotid atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol. 2011, 10: 72-10.1186/1475-2840-10-72.
Ikonomidis I, Kadoglou N, Tsiotra PC, Kollias A, Palios I, Fountoulaki K, Halvatsiotis I, Maratou E, Dimitriadis G, Kremastinos DT, et al: Arterial Stiffness Is Associated With Increased Monocyte Expression of Adiponectin Receptor mRNA and Protein in Patients With Coronary Artery Disease. Am J Hypertens. 2012, 10.1038/ajh.2012.42. e-pub ahead of print.
Yoo HJ, Hwang SY, Hong HC, Choi HY, Yang SJ, Seo JA, Kim SG, Kim NH, Choi KM, Choi DS, et al: Association of circulating omentin-1 level with arterial stiffness and carotid plaque in type 2 diabetes. Cardiovasc Diabetol. 2011, 10: 103-10.1186/1475-2840-10-103.
Fantuzzi G, Mazzone T: Adipose tissue and atherosclerosis: exploring the connection. Arterioscler Thromb Vasc Biol. 2007, 27 (5): 996-1003. 10.1161/ATVBAHA.106.131755.
Chambless LE, Folsom AR, Davis V, Sharrett R, Heiss G, Sorlie P, Szklo M, Howard G, Evans GW: Risk factors for progression of common carotid atherosclerosis: the Atherosclerosis Risk in Communities Study, 1987–1998. Am J Epidemiol. 2002, 155 (1): 38-47. 10.1093/aje/155.1.38.
Acknowledgements
The present work was supported by unconditional grants from The North Norway Regional Health Authority and from the Simon Fougner Hartmann’s Family Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
We declare that we have no competing interests.
Authors’ contributions
MH acquired the carotid ultrasound data, performed the statistical analysis, and drafted the manuscript. KAA acquired the carotid ultrasound data, and made critical revision of the manuscript. SHJ participated in the design of the study, and made critical revision of the manuscript. EBM designed and coordinated the study, acquired the carotid ultrasound data, handled funding, and helped to draft the manuscript. All authors read and approved the final manuscript.
An erratum to this article is available at http://dx.doi.org/10.1186/1475-2840-12-144.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Herder, M., Arntzen, K.A., Johnsen, S.H. et al. The metabolic syndrome and progression of carotid atherosclerosis over 13 years. The Tromsø study. Cardiovasc Diabetol 11, 77 (2012). https://doi.org/10.1186/1475-2840-11-77
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-11-77