Abstract
Introduction
Mechanical ventilation is the most common intervention for patients with respiratory failure in the intensive care unit. There is limited data from African countries, including Ethiopia on time to death and its predictors among patients on mechanical ventilators. Therefore, this study aimed to assess time to death and its predictors among adult patients on mechanical ventilation admitted in comprehensive specialized hospitals in West Amhara, Ethiopia.
Methods
An institutional-based retrospective follow-up study was conducted from January 1, 2020, to December 31, 2022. A simple random sampling was used to select a total of 391 patients’ charts. Data were collected using data the extraction tool, entered into Epi-data version 4.6.0, and exported to STATA version 14 for analysis. Kaplan–Meier failure curve and the log-rank test were fitted to explore the survival difference among groups. The Cox regression model was fitted, and variables with a p-value < 0.25 in the bivariable Cox regression were candidates for the multivariable analysis. In the multivariable Cox proportional hazard regression, an adjusted hazard ratio with 95% confidence intervals were reported to declare the strength of association between mortality and predictors when a p value is < 0.05.
Results
A total of 391 mechanically ventilated patients were followed for 4098 days at risk. The overall mortality of patients on mechanical ventilation admitted to the intensive care units was 62.2%, with a median time to death of 16 days (95% CI: 11, 22). Those patients who underwent tracheostomy procedure (AHR = 0.40, 95% CI: 0.20, 0.80), received cardio-pulmonary resuscitation (AHR = 8.78, 95% CI: 5.38, 14.35), being hypotensive (AHR = 2.96, 95% CI: 1.11, 7.87), and had a respiratory rate less than 12 (AHR = 2.74, 95% CI: 1.48, 5.07) were statistically significant predictors of time to death among mechanically ventilated patients.
Conclusion
The mortality rate of patients on mechanical ventilation was found to be high and the time to death was short. Being cardiopulmonary resuscitated, hypotensive, and had lower respiratory rate were significant predictors of time to death, whereas patients who underwent tracheostomy was negatively associated with time to death. Tracheostomy is needed for patients who received longer mechanical ventilation, and healthcare providers should give a special attention for patients who are cardiopulmonary resuscitated, hypotensive, and have lower respiratory rate.
Similar content being viewed by others
Introduction
Mechanical ventilation (MV) is a lifesaving treatment modality considered a cornerstone to support critically ill patients and is used most commonly in Intensive Care Units (ICU) [1,2,3,4,5]. Globally, the number of patients requiring mechanical ventilation is increasing, specifically patients with Acute Respiratory Failure (ARF). It is provided for over 20 million patients worldwide [6], and among ICU-admitted patients, 35–50% require MV during their admission [7]. Millions of patients are discharged from hospitals after surviving critical illnesses each year. However, patients with ARF had a low survival rate, with a death rate of 67.2%. As a result, these patients are often supported with MV to improve gas exchange, reduce the work of breathing, prevent complications, and improve their outcome [8]. On the contrary, due to complications resulting from mechanical ventilation, up to 40% of patients died in the hospital because of its harmful effect on the patients’ lungs [9].
Despite the advancement in technology to support medical practices in the ICU, the death rate among mechanically ventilated patients remains high [2]. This mortality might be due to factors existed prior to the initiation of MV or developed during the course of treatment, as well as its complications [10]. Moreover, survivors of mechanically ventilated critically ill patients had short-term survival and a poor quality of life [11]. In addition to the high mortality rate, mechanically ventilated patients had faced various health-related problems [12, 13], such as emotional signs when they are stressed, mental health problems [14], physiological disturbances, and physical changes [15]. Besides, these critically ill patients on MV had increased healthcare expenditures since these patients consume extensive medical resources [16, 17], such as medical equipment, supplies, and personnel costs required to provide care [18].
In Ethiopia, many studies have been conducted to determine the mortality outcome of patients admitted to the ICU. However, studies on the survival of patients on mechanical ventilation admitted to the ICU were scarce. Furthermore, even available studies are not specific and cross-sectional in nature, which couldn’t consider the time variable and other clinically significant variables. In this regard, evidence about the time to death and its predictors helps to improve patient outcomes, assist clinicians in designing evidence-based strategies, decision-making process, and better resource allocation, and is used as an input for future studies. Therefore, this study aimed to determine the time to death and its predictors among mechanically ventilated patients admitted to the ICU.
Methods and materials
Study area
The study was conducted in West Amhara comprehensive specialized hospitals. There are five comprehensive specialized hospitals found in West Amhara. Among these, Felege-Hiwot, Tibebe Ghion, and Debre Markos comprehensive specialized hospitals were included in the study. Felege-Hiwot and Tibebe Gion comprehensive specialized hospitals are found in Bahir Dar, which is located 565 km northwest of Addis Ababa, the capital city of Ethiopia, whereas Debre Markos comprehensive specialized hospital is found in Debre Markos town, 299 km away from Addis Ababa. These hospitals provide inpatient and outpatient healthcare services for more than 15 million people. The ICUs are providing similar level of care equipped with mechanical ventilators, noninvasive hemodynamic monitoring devices, portable ultrasounds, Electrocardiograms (ECG), defibrillators, and infusion pumps. The total number of ICU beds in Felege Hiwot, Tibebe Ghion, and Debre Markos is 12, 9, and 4, respectively.
Study design and period
The institutional-based retrospective follow-up study design was conducted from January 1, 2020, to December 31, 2022, and the actual data collection period was December 1–31, 2022.
Population
All adult patients who were admitted to the ICU in West Amhara comprehensive specialized hospitals and received MV were the source population. All adult patients on MV who were admitted to the ICU in selected comprehensive specialized hospitals during the study period were the study population. Records of patients on MV during the study period and whose age ≥ 18 years were included. However, records of patients on MV without the outcome variable were excluded from the study.
Sample size determination
A survival sample size calculation power approach using Stata 14 software with cox proportional assumptions was used.
Where: N = total number of sample size, E = total number of events required, p(E) = probability of event,ρ=proportion of subjects under exposure variable,HR=hazard ratio,\(\frac{{z\alpha }}{2}\) =critical value at 95% confidence level, which 1.96 and \(Z\beta\)= 0.842, standard deviation and correlation of covariate 0.5 and 0, respectively, and 0.1 for probability of withdrawal.
Therefore, the sample size was calculated for the four predictor variables, i.e., use of vasopressors, neuromuscular blockers, hemodialysis, and body mass index ≤ 21 kg/m2 based on the study done in Korea [11] (Table 1).
Accordingly, the largest sample size obtained was 355. Thus, by adding 10% for possible incomplete charts and lost medical records, the total sample size was 391.
Sampling techniques and procedures
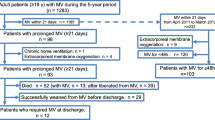
A simple random sampling was employed to select three hospitals from a total of five comprehensive specialized hospitals. Moreover, after the sample size was proportionally allocated for each hospital, a simple random sampling technique using the computer generation method was used to select the patients’ charts. The list of patients who were admitted to the ICU and received MV was used as a sampling frame. The total number of patients who received MV and were admitted to the ICU in two years was 688 (Fig. 1).
Operational definitions
Prolonged use of mechanical ventilation
when patients experience difficulty of weaning from MV after 21 days (the use of mechanical ventilation for ≥ 21 days) [19].
Incomplete card
patient chart in which the outcome of the patient and the duration of mechanical ventilation were not registered.
Comorbidity
presence of disease conditions according to the Carlson comorbidity index. A “yes” to these disease conditions indicates comorbidity, and “no” answer was taken as the absence of comorbidity [20].
Event
mechanically ventilated adult patients who died in the hospital during the follow-up period.
Censored
patients who did not develop the outcome of interest (death) such as Left Against Medical Advice (LAMA), transferred out, and recovered during the follow-up period.
Time to death
The number of days starting from the initiation of the mechanical ventilator to the occurrence of an event (death) within the follow-up period.
Data collection tool and procedures
Data was collected using a data extraction tool adapted from different literature [2, 4, 11, 21, 22]. The questionnaire has five sections: factors related to socio-demographic characteristics, factors present at the initiation of mechanical ventilation, factors related to the patient’s clinical condition, factors related to the management of patients, and factors related to vital signs at admission (Supplementary material 1). The data were obtained from the ICU registration book and patients’ charts. Data collection was done by four BSc nurses, and one MSc nurse supervised the collection period process.
Data quality control
A one-day training was provided to data collectors and supervisor on the data collection process. Preliminary chart review was conducted in Debre Markos comprehensive specialized hospital to ensure the availability of variables on the patient’s chart. Moreover, the data were cross-checked for consistency, completeness, clarity, and accuracy by the supervisor and the principal investigator before analysis.
Data processing and analysis
Data were entered into Epi Data Version 4.6 and exported into Stata Version 14 statistical software for analysis. Descriptive statistics of numeric variables are presented using the median with Inter Quartile Range (IQR) and categorical variables expressed in frequency with percentages. The incomplete data were managed with the assumption of multiple imputations, after which it was ascertained that the missing data was completely at random and less than 15% of the records. The outcome of each participant was dichotomized into censored or event. The Kaplan-Meier failure curve was used to estimate failure time. The Kaplan-Meier failure curve and the log-rank test were fitted to test the presence of differences between different categories of explanatory variables. The proportional hazard assumption was checked both graphically and statistically by using the log (-log) plot and Schoenfeld residual test, respectively, and it was satisfied. Multicollinearity for independent variables was checked by using Variance Inflation Factor (VIF) and the mean VIF was 1.37. The Cox proportional hazard regression was used to explore the association between each independent variable and the outcome variable. The model’s fitness was tested using the Cox–Snell residual test. Variables having a p-value < 0.25 in the bivariable analysis were candidates for the multivariable analysis. An Adjusted Hazard Ratio (AHR) with 95% Confidence Intervals (CI) was computed to explore the strength of the association, and variables with a p-value less than 0.05 were considered statistically significant with time to death.
Result
Socio-demographic characteristics of the study participants
During the study period, 688 patients were treated with invasive mechanical ventilation. From these, 391 patients’ charts were reviewed (Supplementary material 2). About 159 (40.7%) of the participants were less than 45 years old, with a median age of 50 years (IQR: 18–90). Nearly two-thirds (63.4%) were males, and more than half (54.5%) were rural residents (Table 2).
Vital signs of mechanically ventilated patients during admission
Nearly half (45.5%) and three-fourths (73.40%) of study participants were hypotensive and hypoxic during admission, respectively (Table 3).
Clinical-related characteristics of the study participants
More than a quarter (28.6%) of patients were admitted to the ICU with the diagnosis of respiratory failure, followed by neurological disorder (16.4%). Nearly half (48.3) of the study participants had a Glasgow Coma Scale (GCS) score of 3–8 (Table 4).
Management-related characteristics of patients on MV
More than one-fourth (27.62%) of the study participants were received vasopressors during their ICU admission. Tracheostomy procedure is performed for only (8.4%) of the mechanically ventilated patients (Table 5).
Ventilation-related characteristics of the study participants
The majority of patients (90.0%) were received Synchronized Intermittent Mandatory Ventilation (SIMV) mode of mechanical ventilation. From the total mechanical ventilated patients, (15.5%) were developed ventilated associated complications (Table 6).
Assessing the proportional hazard assumption
The Cox proportional hazard assumptions were checked statistically and graphically using the global test and log (-log) plot, respectively. All the covariates met the proportional hazard assumptions, and the p-value overall Schoenfeld global test was 0.0795 (Table 7).
Model goodness of fit test
Cox Snell residuals were used to check the goodness of fit test. The hazard function follows 45˚ closest to the baseline hazard, which showed that the model was well fitted (Fig. 2).
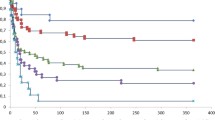
Time to death among mechanically ventilated patients
This study found that the overall mortality of patients on mechanical ventilation admitted to the ICU was 62.2%, with a median time to death of 16 days (95% CI: 11, 22). Patients were followed for a minimum of 1 day and a maximum of 36 days, with a total person-time at risk of 4098 days. The overall incidence density rate of mortality among mechanically ventilated patients admitted to the ICU was 5.93 per 100 person-day observations (95% CI: 5.23, 6.72). According to the Kaplan-Meier failure curve, the cumulative probability of death at the end of 8, 16, 24, 32 and 36 days was 5.8%, 3.6%, 7.3%, 23%, and 25.0%, respectively (Fig. 3).
Test for equality of failure function
A Kaplan-Meier failure curve together with the log-rank test was done to test the presence of a difference in the time to death among predictor variables. According to the current study, those patients without a tracheostomy procedure had a shorter time to death with a median survival time of 12 days (95% CI: 10, 18) as compared to their counterparts (23 days, 95% CI: 22, 25) (Fig. 4).
In addition, those patients who received CPR had a shorter time to death with a median survival time of 5 days (95% CI: 3, 7) as compared to their counterparts (24 days, 95% CI: 23, 25) (Fig. 5).
Patients who had a respiratory rate less than 12 had a shorter time to death with a median survival time of 3 days (95% CI: 3, 8), as compared to those who had 12–20 breaths/minutes (23 days, 95% CI: 23, 24). Similarly, those patients with a respiratory rate greater than 20 breaths/ min had a shorter time to death with a median survival time of 12 days (95% CI: 9, 15) compared to those who had a respiratory rate of 12–20 breaths/min (Fig. 6).
Moreover, those hypotensive patients at admission had a shorter time to death with a median survival time of 3 days (95% CI: 2, 6) as compared to normotensive patients (23 days, 95% CI: 15, 24). Similarly, patients having a higher systolic blood pressure (> 140mmHg) had also a shorter time to death with a median survival time of 12 days (95% CI: 10, 22) compared to normotensive patients (Fig. 7).
Predictors of time to death among mechanically ventilated patients admitted to the ICU
Based on the multivariable Cox proportional hazard regression analysis, patients who underwent tracheostomy, CPR, SBP < 90 mmHg, and respiratory rate < 12 rate/min were significant predictors of time to death among mechanically ventilated patients admitted to the ICU.
Keeping other variables constant, underwent tracheostomy procedure among mechanically ventilated patients decreased the hazard of death by 60% as compared to their counterparts (AHR: 0.40, 95% CI: 0.20, 0.80). The hazard of death among those cardiopulmonary resuscitated patients was 8.8 times higher as compared to their counterparts (AHR: 8.78, 95% CI: 5.38, 14.35). Moreover, those mechanically ventilated patients who had hypotension at admission had 2.96 times a higher hazard of death as compared to those patients who were normotensive (AHR: 2.96, 95% CI: (1.11–7.87). Similarly, those patients who had a respiratory rate of < 12 breath/min had 2.7 times higher hazard of death as compared to those who had a respiratory rate of 12–20 breath/min (AHR: 2.74, 95% CI: (1.48–5.07)) (Table 8).
Discussion
This study aimed to determine the time to death and identify its predictors among patients on MV admitted to the ICU. According to the current study, the median time to death among patients on mechanical ventilator was 16 days. Those mechanically ventilated patients who underwent tracheostomy, received CPR, having a respiratory rate less than 12 breaths per minute, and were hypotensive were significant predictors for time to death.
This study found that the median time to death of mechanically ventilated ICU patients was 16 days (95% CI: 11–22). This finding is in line with the studies done in Saudi Arabia, Spain, and Ethiopia [5, 23, 24]. However, it is lower than the study conducted in Southern Brazil [2]. The reason for this discrepancy might be due to the difference in the quality of the health care delivery system [2, 25]. Additionally, it might also be due to the patients’ clinical status during admission to the ICU, which can increase the hazard of death [9, 25].
This study also showed that the overall incidence density rate of death among mechanically ventilated patients admitted to the ICU was 5.93 per 100-day observations (95% CI: 5.23–6.72), which is in line with the study conducted in Ethiopia [26]. The overall mortality of patients on mechanical ventilation was 62.2%, which is consistent with the previous study conducted in Ethiopia (60.7%) [27]. However, this finding is higher than the studies conducted in Ethiopia [24] Sub-Saharan Africa [28], and Brazil [2], which reported that the prevalence of mortality among mechanically ventilated patients admitted to the ICU was 33.78%, 49%, and 51%, respectively. The reason for this discrepancy might be due to the difference in the level of ICU organization and duration of follow-up.
Mechanically ventilated patients who underwent tracheostomy procedure had decreased the hazard of death by 60% as compared to their counterparts. This finding is supported by studies done in Nigeria and Taiwan [9, 29]. This might be due to the protective effects of tracheostomy procedure such as improved patient comfort, better oral hygiene, less dental damage and tracheal injury, easier and faster nursing care, and lower airway resistance, which may facilitate the weaning process and avoid ventilator-associated pneumonia [30].
This study also found that the hazard of death among those cardiopulmonary resuscitated patients was 8.8 times higher as compared to their counterparts. This finding is supported by the studies conducted in Ethiopia, Berlin, and France [24, 31, 32]. This might be due to the fact that those patients who were cardiopulmonary resuscitated had the problems of hemodynamic failure, lack of oxygenation [32], and a higher severity of illness [31], which facilitates patient mortality. The time of CPR initiation could be another possible reason since the chance of survival would be low if CPR couldn’t be initiated immediately after cardiac arrest due to severe and permanent brain damage [31, 33].
Mechanically ventilated patients who were hypotensive at admission had 2.96 times a higher hazard of death as compared to those who were normotensive. This is supported by studies done in France and China [32, 34]. This might be due to the scientific evidence that hypotension decreases tissue perfusion, which leads to multi-organ failure such as renal failure, cardiac failure, and brain death [35, 36]. Therefore, a healthcare provider should focus on maintaining the blood pressure of critically ill patients who have received mechanical ventilation.
Moreover, this study revealed that those patients who had a respiratory rate less than 12 breaths per minute had 2.7 times higher hazard of death as compared with those who had a respiratory rate of 12–20 breaths per minute. This is supported by the studies done in Denmark and Sweden [37, 38]. The possible reason for this might be attributed to the decreasing respiratory rate, which is an indicator of brain dysfunction from many causes, like structural or non-structural processes affecting the central nervous system, which leads to death [37, 38]. Therefore, measuring the respiratory rate is important for early identification of high-risk patients because the respiratory rate is a superior indicator to other physiologic parameters.
Strengths and limitations of the study
This is a multi-center follow-up study, which increases its generalizability to the target population. However, this study has some limitations. Since it was institutional-based and the data were obtained from patients’ medical records, mortality-predicting variables such as the Acute Physiology and Chronic Health Evaluation (APACHE) and Sequential Organ Failure Assessment (SOFA) scores couldn’t be addressed.
Conclusion
Patients treated with mechanical ventilation had a shorter time to death. Being cardiopulmonary resuscitated, hypotensive, and had lower respiratory rate were significant predictors of time to death, whereas patients who underwent tracheostomy was negatively associated with time to death. Therefore, we strongly recommended that the healthcare provider should perform a tracheostomy procedure early for critically ill patients who need prolonged ventilation, and a special attention should be given for patients who had lower systolic blood pressure and respiratory rate. Furthermore, a prospective follow up study is required by incorporating the Acute Physiology and Chronic Health Evaluation (APACHE) and Sequential Organ Failure Assessment (SOFA) scores to predict the mortality of mechanically ventilated patients.
Data availability
Data will be available upon request from the corresponding author.
Abbreviations
- AHR:
-
Adjusted Hazard Ratio
- ARDS:
-
Acute Respiratory Distress Syndrome
- CHR:
-
Crude Hazard Ratio
- COPD:
-
Chronic Obstructive Pulmonary Diseases
- CI:
-
Confidence Interval
- GCS:
-
Glasgow Coma Scale
- IDR:
-
Incidence Density Rate
- KM:
-
Kaplan Meier
- LOS:
-
Length Of Stay
- MOF:
-
Multi-Organ Failure
- MV:
-
Mechanical Ventilation
- WHO:
-
World Health Organization
References
Esteban A, Frutos-Vivar F, Muriel A, Ferguson ND, Peñuelas O, Abraira V, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188(2):220–30.
Fialkow L, Farenzena M, Wawrzeniak IC, Brauner JS, Vieira SRR, Vigo A, et al. Mechanical ventilation in patients in the intensive care unit of a general university hospital in southern Brazil: an epidemiological study. Clinics. 2016;71:144–51.
Damuth E, Mitchell JA, Bartock JL, Roberts BW, Trzeciak S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respiratory Med. 2015;3(7):544–53.
Liang J, Li Z, Dong H, Xu C. Prognostic factors associated with mortality in mechanically ventilated patients in the intensive care unit: a single-center, retrospective cohort study of 905 patients. Medicine. 2019;98(42).
Ismaeil T, Almutairi J, Alshaikh R, Althobaiti Z, Ismaiel Y, Othman F. Survival of mechanically ventilated patients admitted to intensive care units: results from a tertiary care center between 2016–2018. Saudi Med J. 2019;40(8):781.
Urner M, Jüni P, Hansen B, Wettstein MS, Ferguson ND, Fan E. Time-varying intensity of mechanical ventilation and mortality in patients with acute respiratory failure: a registry-based, prospective cohort study. Lancet Respiratory Med. 2020;8(9):905–13.
Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345–55.
Stefan MS, Priya A, Pekow PS, Lagu T, Steingrub JS, Hill NS, et al. The comparative effectiveness of noninvasive and invasive ventilation in patients with pneumonia. J Crit Care. 2018;43:190–6.
Tobi K, Ekwere I, Ochukpe C. Mechanical ventilation in the Intensive Care Unit: a prospective study of indications and factors that affect outcome in a Tertiary Hospital in Nigeria. J Anesth Clin Res. 2017;8(718):2.
Esteban A, Anzueto A, Alia I, Gordo F, Apezteguia C, Palizas F, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med. 2000;161(5):1450–8.
Lee SH, Kim MJ, Jeong ES, Jo E-J, Eom JS, Mok JH, et al. Outcomes and prognostic factors in patients with prolonged acute mechanical ventilation: a single-center study in Korea. J Crit Care. 2015;30(5):1016–20.
Engström Å, Nyström N, Sundelin G, Rattray J. People’s experiences of being mechanically ventilated in an ICU: a qualitative study. Intensive Crit care Nurs. 2013;29(2):88–95.
Ten Hoorn S, Elbers P, Girbes A, Tuinman P. Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Crit Care. 2016;20(1):1–14.
edu TSIchm. Early mobilization and recovery in mechanically ventilated patients in the ICU: a bi-national, multi-centre, prospective cohort study. Crit Care. 2015;19:1–10.
Dehghani A, Abdeyazdan G, Davaridolatabadi E. An overview of the predictor standard tools for patient weaning from mechanical ventilation. Electron Physician. 2016;8(2):1955.
Wunsch H, Linde-Zwirble WT, Angus DC, Hartman ME, Milbrandt EB, Kahn JM. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38(10):1947–53.
Fernando SM, McIsaac DI, Rochwerg B, Bagshaw SM, Muscedere J, Munshi L, et al. Frailty and invasive mechanical ventilation: association with outcomes, extubation failure, and tracheostomy. Intensive Care Med. 2019;45(12):1742–52.
Jacobs P, Edbrooke D, Hibbert C, Fassbender K, Corcoran M. Descriptive patient data as an explanation for the variation in average daily costs in intensive care. Anaesthesia. 2001;56(7):643–7.
Hill AD, Fowler RA, Burns KE, Rose L, Pinto RL, Scales DC. Long-term outcomes and health care utilization after prolonged mechanical ventilation. Annals Am Thorac Soc. 2017;14(3):355–62.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Wang C-H, Lin H-C, Chang Y-C, Maa S-H, Wang J-S, Tang W-R. Predictive factors of in-hospital mortality in ventilated intensive care unit: a prospective cohort study. Medicine. 2017;96(51).
Lai C-C, Shieh J-M, Chiang S-R, Chiang K-H, Weng S-F, Ho C-H, et al. The outcomes and prognostic factors of patients requiring prolonged mechanical ventilation. Sci Rep. 2016;6(1):1–6.
Rodriguez JS, Cortés JM. Mortality study in patients at weaning from mechanical ventilation. Med Intensiva (English Edition). 2020;44(8):485–92.
Tilahun L, Molla A, Ayele FY, Nega A, Dagnaw K. Time to recovery and its predictors among critically ill patients on mechanical ventilation from intensive care unit in Ethiopia: a retrospective follow up study. BMC Emerg Med. 2022;22(1):1–11.
Machado–Alba JE. AFUV, Nicolás Sánchez–Ramírez, Luis Fernando Valladales–Restrepo, Manuel Machado–Duque, Andrés Gaviria–Mendoza. Factors Associated with Survival in patients undergoing invasive mechanical ventilation in an Intensive Care Unit in Colombia. Real world outcome; 2021.
Endeshaw AS, Fekede MS, Gesso AS, Aligaz EM, Aweke S. Survival status and predictors of mortality among patients admitted to surgical intensive care units of Addis Ababa governmental hospitals, Ethiopia: a multicenter retrospective cohort study. Front Med. 2023;9:1085932.
Debebe F, Goffi A, Haile T, Alferid F, Estifanos H, Adhikari NK. Predictors of ICU Mortality among Mechanically Ventilated Patients: An Inception Cohort Study from a Tertiary Care Center in Addis Ababa, Ethiopia. Critical Care Research and Practice. 2022;2022.
Abate SM, Basu B, Jemal B, Ahmed S, Mantefardo B, Taye T. Pattern of disease and determinants of mortality among ICU patients on mechanical ventilator in Sub-saharan Africa: a multilevel analysis. Crit Care. 2023;27(1):1–13.
Wei-Chieh Lin1 C-WC, Wang J-D, Liang-Miin, Tsai. Is tracheostomy a better choice than translaryngeal intubation for critically ill patients requiring mechanical ventilation for more than 14 days? A comparison of short-term outcomes. BMC. 2015.
Prin M, Kaizer A, Cardenas J, Mtalimanja O, Kadyaudzu C, Charles A, et al. Tracheostomy practices for mechanically ventilated patients in Malawi. World J Surg. 2021;45(9):2638–42.
Al-Alwan A, Ehlenbach WJ, Menon PR, Young MP, Stapleton RD. Cardiopulmonary resuscitation among mechanically ventilated patients. Intensive Care Med. 2014;40(4):556–63.
De Jong A, Rolle A, Molinari N, Paugam-Burtz C, Constantin J-M, Lefrant J-Y, et al. Cardiac arrest and mortality related to intubation procedure in critically ill adult patients: a multicenter cohort study. Crit Care Med. 2018;46(4):532–9.
Kaldırım U, Toygar M, Karbeyaz K, Arzıman I, Tuncer SK, Eyi YE, et al. Complications of cardiopulmonary resuscitation in non-traumatic cases and factors affecting complications. Egypt J Forensic Sci. 2016;6(3):270–4.
Li C, Chen Y, Zheng Q, Wu W, Chen Z, Song L, et al. Relationship between systolic blood pressure and all-cause mortality: a prospective study in a cohort of Chinese adults. BMC Public Health. 2018;18(1):1–9.
Smischney NJ, Demirci O, Diedrich DA, Barbara DW, Sandefur BJ, Trivedi S, et al. Incidence of and risk factors for post-intubation hypotension in the critically ill. Med Sci Monitor: Int Med J Experimental Clin Res. 2016;22:346.
Messelu MA, Tilahun AD, Beko ZW, Endris H, Belayneh AG, Tesema GA. Incidence and predictors of mortality among adult trauma patients admitted to the intensive care units of comprehensive specialized hospitals in Northwest Ethiopia. Eur J Med Res. 2023;28(1):1–12.
Barfod C, Lauritzen MMP, Danker JK, Sölétormos G, Forberg JL, Berlac PA, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department-a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2012;20(1):1–10.
Ljunggren M, Castrén M, Nordberg M, Kurland L. The association between vital signs and mortality in a retrospective cohort study of an unselected emergency department population. Scand J Trauma Resusc Emerg Med. 2016;24(1):1–11.
Acknowledgements
We would like expressed our heartfelt thanks to Flege Hiwot, Tibe Ghion, and Debre Markos hospitals for their cooperation and giving permission for the data access. Moreover, we would like to give our special appreciation to the data collectors and supervisor. Finally, thanks to all with significant contribution to the success of this study.
Funding
Funding not applicable.
Author information
Authors and Affiliations
Contributions
KD conceptualized the study and Dr. ET and FN were involved in design, analysis, interpretation, report and manuscript writing. AT, TA and MA made substantial contribution to conception, analysis and interpretation of data, drafting the manuscript and critical revision for important intellectual content. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by Ethical Review Committee of school of nursing on the behalf of Debre Birhan University with ethical approval number IRB 70/09/2014. The need for informed consent was waived by Ethical Review Committee of school of nursing. Amhara Public Health Institute (APHI) wrote a cooperation letter to each study hospital with the reference number APHI/422/2014. Data was kept anonymously by coding and the data recorded on mobile was locked with password to keep confidentiality. Information about specific personal identifiers like the patient’s name were not collected, so it didn’t inflict any harm on the patients. All the processes of the research were performed and secured in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Demem, K., Tesfahun, E., Nigussie, F. et al. Time to death and its predictors among adult patients on mechanical ventilation admitted to intensive care units in West Amhara comprehensive specialized hospitals, Ethiopia: a retrospective follow-up study. BMC Anesthesiol 24, 114 (2024). https://doi.org/10.1186/s12871-024-02495-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-024-02495-9