Abstract
Background
The global mortality rate of patients with MV is very high, despite a significant variation worldwide. Previous studies conducted in Sub-Saharan Africa among ICU patients focused on the pattern of admission and the incidence of mortality. However, the body of evidence on the clinical outcomes among patients with MV is still uncertain.
Objective
The objective of this study was to investigate the pattern of disease and determinants of mortality among patients receiving mechanical ventilation in Southern Ethiopia.
Methods
Six hundred and thirty patients on mechanical ventilation were followed for 28 days, and multilevel analysis was used to account for the clustering effect of ICU care in the region.
Results
The incidence of 28-day mortality among patients with MV was 49% (95% CI: 36–58). The multilevel multivariate analysis revealed that being diabetic, having GSC < 8, and night time admission (AOR = 7.4; 95% CI: 2.96–18.38), (AOR = 5.9; (5% CI: 3.23, 10.69), and (AOR = 2.5; 95% CI: 1.24, 5.05) were predictors.
Conclusion
The higher 28-day mortality among ICU patients on mechanical ventilation in our study might be attributed to factors such as delayed patient presentation, lack of resources, insufficient healthcare infrastructure, lack of trained staff, and financial constraints.
Trial Registration. The protocol was registered retrospectively on (NCT05303831).
Similar content being viewed by others
Background
The burden of life-threatening conditions requiring mechanical ventilation (MV) in the intensive care unit has grown substantially in the last couple of decades in low- and middle-income countries because of an emerging pandemic, motorization, urbanization, and hospital expansion [1,2,3,4,5,6]. However, the advancement of ICU care is very limited due to the high cost of infrastructure, training, medical staff, failure to incorporate international guidelines for evidence-based care, and inadequate medical supplies [3, 5, 7,8,9,10].
Epidemiological studies revealed that as high as 70% of patients admitted to the intensive care unit (ICU) require mechanical ventilation at some point during their stay in ICU [11, 12].
An international prospective cohort study of 15,757 patients admitted to the ICU found that 5183 (33%) were on mechanical ventilation for more than 12 h, with a third of them suffering from ARDS [12]. Another multicenter study conducted in Poland by Kubler et al. among eighty-three ICUs across the country found that more than seventy percent of patients were on mechanical ventilation with respiratory failure (40%), coma (40%), chronic obstructive pulmonary disease (14%), and neuromuscular disease (5%) [11].
Studies investigating the incidence of MV and determinants of mortality among mechanically ventilated patients in Sub-Saharan African countries are very limited. A few studies in Ethiopia revealed that patients requiring mechanical ventilation and the indication for mechanical ventilation greatly vary from region to region [13,14,15,16,17,18,19,20].
Evidence revealed that the outcomes of patients with MV varied widely from one population to another, which is greatly influenced by ICU infrastructure, patient characteristics, emergent clinical events, ICU staff profile, integrated patient monitors, and medical supplies [11, 21,22,23].
Studies on ICU patients in Sub-Saharan Africa, including Ethiopia, have primarily focused on admission patterns, mortality rates, and their determinants. However, there is still uncertainty in the body of evidence regarding the pattern of disease, the incidence of MV, and the factors influencing clinical outcomes among patients with MV. The objective of this multicenter prospective cohort was to investigate the disease pattern and factors influencing clinical outcomes in patients receiving mechanical ventilation in Southern Ethiopia.
Methods
Study design
This Multi-center prospective cohort study was conducted in Southern Ethiopia teaching referral hospital ICUs from October 2020 to November 2022. Three teaching and referral hospital ICUs were selected randomly from ten teaching hospitals in Southern Ethiopia, namely Hawassa university referral hospital (HURH), Dilla University referral hospital (DURH), and Wolaita Sodo referral hospital (WURH). The ICUs are providing a similar level of care with almost similar staff profiles, monitoring modalities, ICU infrastructure, medical supplies, and admission patterns.
Study inclusion and exclusion criteria
All patients over the age of 12 who received mechanical ventilation at DURH, Wolaita Sodo University Hospital, and Hawassa University Specialized Hospital ICUs and stayed there for longer than 24 h of admission were included; whereas, patients receiving non-invasive oxygen supplementation, patients who were discharged, transferred to, or left against medical advice before 24 h of mechanical ventilation, patients who were admitted to ICU on re-admission, and patients without attendants were excluded.
Study variables
The cumulative incidence of 28-day mortality, duration of a mechanical ventilator, incidence of complications, pattern of disease, and length of stay in ICU were dependent variables, while socio-demographic characteristics: Age, sex, height, weight, BMI; Admission characteristics: date of ICU admission, date of discharge, vital sign, diagnosis, admission category, time of admission, laboratory index, disease severity score; Mechanical ventilation parameters: date of initiation, initial mode, date of tracheostomy, and date of weaning were independent variables.
Data collection
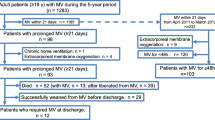
The data were collected prospectively from three hospital ICUs patients in whom mechanical ventilation was initiated. After 2 h of mechanical ventilation, trained ICU nurses followed eligible participants for 28 days. The data were collected with a validated questionnaire and tools adopted from previous studies [11, 21,22,23]. A total of 630 patients were recruited consecutively from each ICU from October 2020 to November 2022 as per proportion allocation to size (Fig. 1).
The data collection included Socio-demographic characteristics: Age, Sex, Height, Weight, BMI); Admission characteristics: date of ICU admission, date of discharge, vital signs, diagnosis, admission category, time of admission, laboratory index, disease severity score; Complications: nosocomial infection, ventilator-associated pneumonia, sepsis, ARDS, aspiration, unplanned extubation, endotracheal tube blockage, tracheostomy loose/stenosis/fistula, cardiac arrest, acute kidney injury, bedsore); comorbidities: hypertension, diabetes mellitus, cardiovascular disease, Asthma/COPD, liver failure, renal failure, others, and clinical outcomes including mortality, duration of a mechanical ventilator, and complications were measured for 28 days. Furthermore, the disease severity scores including sequential organ assessment (SOFA) score, modified SOFA score, Acute Physiology, and Chronic Health Evaluation (APACHE) II score, and modified APACHE II score were recorded at admission and thereafter till discharge every seven days to compare the predicting ability and 28-day mortality of these tools.
Statistical analysis
The data were checked, coded, and entered into Epi-info version 7.0 and imported to SPSS version 22 for analysis. However, STATA version 14 was used to produce some graphs, multilevel analysis and pool the incidence of clinical outcomes. Descriptive statistics were summarized with tables and figures. Categorical variables were reported in frequency and percentage. The numerical data were reported in mean ± SD for symmetric and median (Interquartile range) for asymmetric numeric data. The outlier of the data was checked with standardized residuals while Shapiro–Wilk tests were employed for the normality test. The multicollinearity among independent variables was checked by the Variance inflation factor (VIF), and a VIF of greater than 10 was considered multicollinearity. The association of demographic characteristics, admission category, indications for MV, and complications of MV with mortality were analyzed using multilevel binary logistic regression as there was clustering as depicted with an intraclass correlation coefficient (ICC = 8.5%). All variables showing significance on multilevel bivariate analysis at a p-value less than 0.25 will be taken to multilevel multivariate analysis. In multivariate analysis, a p-value of less than 0.05 was considered for the statistical association. This study was conducted in compliance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies [24].
Study endpoints
The primary endpoints were the incidence of 28-day mortality and duration of mechanical ventilation, while the incidence of complications during MV was the secondary clinical outcome.
Definition incidence of clinical outcomes refers to the occurrence of new clinical events including mortality, morbidity, and prolonged mechanical ventilation in 28 days of ICU stay. Morbidities are defined as any complication developed during Mechanical ventilation which includes nosocomial infection, ventilator-associated pneumonia, sepsis, ARDS, aspiration, unplanned extubation, endotracheal tube blockage, tracheostomy loose/stenosis/fistula, cardiac arrest, acute kidney injury, and bedsore. Prolonged mechanical ventilation refers to the duration of mechanical ventilation for over 21 days [25, 26].
Model building and comparison
The hierarchical nature of the hospital ICU care in which patients are nested within clusters, a multivariable multilevel logistic regression analysis was employed to account for this clustering effect. Thence, four models containing variables of interest were fitted for this study as follows: Model I (Null model) was fitted without explanatory variables to test random variability in the intercept and to estimate the intraclass correlation coefficient (ICC), Model II assessed the effects of individual-level predictors, Model III assessed the effects of hospital-level predictors, and Model IV (Full model) examined the effects of both individual and hospital-level characteristics simultaneously. The Akaike’s Information Criterion (AIC) and Bayesian Information Criterion (BIC) were used to select the model, and the model with low AIC and BIC values was considered the best-fitted model. Based on AIC and BIC, the full (model with individual and hospital-related variables) model had the smallest AIC and BIC value. Therefore, the full model best fits the data.
Ethical statement
This study was reviewed and approved by Dilla University, College of Health Science and Medicine Research Ethics and Review Board (RERB), and a Unique Identification Number (UIN- duirb/001/21-08) was received. Besides, the protocol was registered retrospectively in ClinicalTrials.gov (NCT05303831) on March 30, 2022. The study was conducted in compliance with the Helsinki declaration for human and animal studies [27]. Informed consent was received from all participants’ legal attendants or guardians, and all patient identifiers were kept anonymous at all times. Besides, a formal letter was written to each University hospital ICU director to get permission.
Results
Sociodemographic and baseline characteristics
Out of 648 eligible cohorts, 630 (97.25) completed the 28-day prospective follow-up. The mean (standard deviation) age of the participants was 38.9 ± 17.6 years, where more than two-thirds of them were in the age ranges of 19 to 29 and > 40 years. The majority of participants were male, 426 (67.7%) (Table 1).
Diagnosis and indications for MV
This study showed that acute respiratory syndrome (ARDS) was the commonest diagnosis 178 (28.3%), followed by postoperative events 113 (17.9%), traumatic brain injury (TBI) 92 (14.6%), and stroke 80 (12.7%). The main reason for invasive mechanical ventilation was found to be respiratory failure 393 (62.4%) followed by airway protection 95 (15.1), and postoperative respiratory support 89 (14.1) (Additional file 2: Table S1).
Admission characteristics
Of the 630 patients, medical cases accounted for more than half 356 (56.2) followed by trauma 125 (19.8%), and surgical cases, 89 (14.1%). The majority of patients were admitted to the ICU during day time and nighttime. Overall, 496 (78.7%) of the patients had comorbidities, where hypertension was the highest 151 (245) followed by respiratory (Asthma and COPD) 122 (19.4%), and DM 72 (11.4%). However, in a few patients, 42 (6.7%) had more than one comorbidity, while only 134 (21.2%) had unconfirmed comorbidities (Table 2).
Complications
The majority of patients 456 (71.7%) sustained at least one complication which included ventilator-associated pneumonia (VAP), cardiac arrest, shock, acute kidney injury (AKI), and others, where VAP alone accounted for 198 (31.4%) of the complications. The disease severity scores including Acute Physiologic and Health Evaluation II (APACHE II), Modified Acute Physiologic and Health Evaluation II (APACHE II), Sequential Organ Failure Assessment (SOFA), and Modified Sequential Organ Failure Assessment (MSOFA) were employed during admission of patients, and MAPACHE II) showed a significant association with 28-day survival status with strong predicting probability (Table 2).
Incidence of clinical outcomes
The incidence of 28-day mortality among ICU patients on a mechanical ventilator was 49% (95% CI: 36–58). The overall pooled prevalence of comorbidity among non-survivors was 47% (95% CI: 36–58) (Fig. 2). The histogram and normal distribution curve showed that the majority of patients were on mechanical ventilation for the first fifteen days (Additional file 1: Fig. S1). The duration of MV and baseline Glasgow Coma Scale did not show a significant difference in survival status as depicted on a line graph with error bars (Figs. 3 and 4).
Mechanical ventilation variables
The mode of ventilation in the intensive care unit depends on the admission diagnosis, the severity of the disease, and the presence of other comorbidities. For example, patients with acute respiratory disease distress syndrome benefit from ArdsNet ventilator protocol which includes low tidal volume (4–8 ml/kg) predicted body weight, peak inspiratory pressure < 35 cmH20, and titrated FIO2 as per patient progress while patients with COPD require high peak flow rate with slow respiratory rate. This study tried to investigate the effects of ventilator parameters, duration of mechanical ventilation, and admission disease severity score on survival status and found a significant standardized mean difference in most of the parameters (Fig. 5).
Forest plot for initial ventilator parameters, Deaths severity tools, length of mechanical ventilation among ICU patients on invasive mechanical ventilation: Treatment denotes to Non-survivors; control denotes survivors; TV Tidal volume; MV Minute ventilation; PIP Peak inspiratory pressure; FI02 Fractional inspired oxygen; SPo2 Percutaneous oxygen saturation; APCHE Acute physiologic and chronic health evaluation; MAPACHE Modified acute physiologic and chronic health evaluation; SOFA Sequential organ failure assessment; MSOFA Modified sequential organ failure assessment; LoMV Duration of MV; Los ICU: Length of stay in ICU
Prognostic scores
Several prognostic scores have been employed in the intensive care unit, which includes APACHE I-1 V, SOFA, and biomedical tests. However, the parameters used inquired are blood gas analysis and blood chemistry analysis which is not feasible in a resource-limited setting. In this regard, many studies have been conducted to compare the sensitivity, specificity, and predictability of modified tests that are applicable in a resource-limited environment, but the findings are yet inconsistent. This study was intended to compare the predictability of modified SOFA and modified APACHE II scores. The receiver operating curve showed the area under the curve for APACHE II, modified APACHE II, SOFA, and modified SOFA, revealing a similar prediction of 28-day mortality (Fig. 6 and Additional file 3: Table S2).
Determinants of mortality
This multilevel multivariate analysis revealed that patients with medical causes of ICU admission were approximately 3 times (AOR = 2.9; 95% CI: 1.49–5.49, P value = 0.002) more likely to die compared to surgical (AOR = 1.3; 95% CI: 0.37–2.36), trauma (AOR = 0.9; 95% CI: 0.43–2.13), and other causes of admission (Additional file 4: Table S3 and 3).
Discussion
The discrepancies in sociodemographic, admission characteristics, disease severity, and presence of different comorbidities are considered strongly associated with patient clinical outcomes among patients in the intensive care unit. Therefore, this study has taken into consideration the potential clustering of variation in ICU service among patients on a mechanical ventilator in Southern Ethiopia.
Previous cross-sectional studies conducted in Ethiopia among intensive care patients focused on the overall pattern of admission, determinants, and clinical outcomes in the intensive care unit [13, 14, 19,20,21, 28, 29]. However, this multicenter prospective cohort study tried to investigate the pattern of admission, determinants, and clinical outcomes of patients on a mechanical ventilator.
This study showed that the main indication for initiation of mechanical ventilation was medical cases, followed by postoperative and trauma, which is in line with previous studies conducted in America [30], international cohort study [12], India [22], Poland [11], Ethiopia [13, 20, 21], and Brazil [31]. However, other studies conducted in Tanzania [32], Tunisia [33], the UK [34], and Ethiopia [19] showed that trauma was the main cause of the initiation of mechanical ventilation. These differences might be related to the study area where some ICUs might be specialized in admitting specific patients in the ICU while others admit mixed cases.
Regarding the comorbidity, hypertension was the main comorbidity followed by diabetes mellitus and respiratory disorders, which is consistent with an international cohort study including 16 countries [12], a study by Chiwhane and his colleagues in India [35], and a population-based study by Mehta et al. in the USA [30]. However, DM, cardiovascular, and COPD were the most prevalent comorbidities as per studies conducted by Karthikeyan et al. in India [22], and an international cohort study including 50 countries by Bellani et al., respectively [36]. This discrepancy may be related to the study area, a country where the older population with comorbidities is more prevalent.
The 28-day incidence of mortality in our study was 49% (95% CI: 36–58), which is very high when compared to previous studies conducted among ICU patients on a mechanical ventilator in middle and high-income countries [23, 34]. The disparity in mortality of patients requiring mechanical ventilation might be related to the delayed patient presentation, a lack of resources, insufficient healthcare infrastructure, inadequate trained medical staff, and financial constraints, which entail the stakeholders to buckle down to improve the patient’s clinical outcomes.
Although studies focusing specifically on the incidence of mortality requiring mechanical ventilation in developing countries are lacking, some authors reported cumulative mortality, where evidence from North and Sub-Saharan Africa showed inconsistent findings on the mortality of patients in ICUs receiving mechanical ventilation.
Contrary to the current study, the cumulative incidence of ICU mortality among patients with MV was the highest in Kenya (60.7%) [37], Tanzania (58.7%) [38], Ruanda (68.1%) [39], Tunisia (77.2%) [40], Nigeria (64%) [41], and Ethiopia (80%) [28]. However, other studies in the same Sub-Saharan African region showed a comparable and even lower incidence of mortality to the current study such as in Tanzania (41.4%) [42], Ethiopia (31.5%, 53.5%) [21, 43], and South Africa (24.4%) [44]. This discrepancy might be related to differences in the pattern of admission, sample size, ICU infrastructure, the inadequacy of medical supplies, lack of skilled manpower, and type of hospital and ICU.
The multilevel multivariate analysis revealed that DM comorbidity, baseline respiratory rate > 35 breaths/min, percutaneous arterial oxygen saturation < 80%, and GCS of less than eight were strong independent predictors of 28-day mortality in the intensive care unit among patients on mechanical ventilation. Besides, medical causes of admission, more than one comorbidity, and time of ICU admission were also independent predictors of mortality.
The current study revealed that being diabetic, having GSC < 8 night time admission, and having more than one comorbidity (AOR = 7.4; 95% CI: 2.96–18.38), (AOR = 5.9; (5% CI: 3.23, 10.69), (AOR = 2.5; 95%CI: 1.24, 5.05), and (AOR = 3.9; 95% CI: 1.55, 9.89) were independent predictors of 28-day mortality in patients receiving mechanical ventilation, respectively, which is consistent with previous studies [11, 23, 28, 34]. This calls for special attention to this kind of patient concerning nurse-to-patient ratio, availability of monitoring medication, skilled medical staff, portable diagnostic modalities, and nutritional supplementation.
Strength and limitations
This is the first-ever multicenter prospective cohort study investigating mortality and determinants among patients on mechanical ventilation in sub-Saharan Africa. Besides, the study has taken into account the clustering effect of service variation by conducting a multilevel analysis. However, the study has certain limitations including a lack of arterial and blood chemistry tests to calculate disease severity scores in some patients, and the heterogeneity of cases as the ICUs were general hospitals that admitted a mix of cases.
Implications for practice
This study revealed that the mortality of patients receiving mechanical ventilation in ICU was very high compared to previous studies conducted in western countries, which is strongly associated with the indication for mechanical ventilation, time of admission, baseline vital signs at admission, presence of comorbidities, and complications of mechanical ventilation. This entails mitigating strategies including but not limited to the provision of skilled medical staff, adequate medical supplies, adequate monitoring, and portable diagnostic modalities.
Implications for further study
This is a multicenter prospective cohort study which is the first of its kind in Sub-Saharan Africa with multilevel analysis, but further multicenter prospective studies with a long period of follow-up might be inquired in specialized ICU setups of the homogenous population to investigate the certain impacts of the prolonged mechanical ventilator on patient outcomes.
Conclusion
The higher 28-day mortality among ICU patients on mechanical ventilation might be attributed to factors such as delayed patient presentation, lack of resources, insufficient healthcare infrastructure, lack of trained staff, and financial constraints. The findings of this study could aid in the future improvement in healthcare services among ICU patients with MV in the region.
Availability of data and materials
Data and materials can be available where appropriate.
References
Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339–46.
Baker T. Critical care in low-income countries. Tropical Med Int Health. 2009;14(2):143–8.
Firth P, Ttendo S. Intensive care in low-income countries—a critical need. N Engl J Med. 2012;367(21):1974–6.
Fowler RA, Adhikari NK, Bhagwanjee S. Clinical review: critical care in the global context—disparities in burden of illness, access, and economics. Crit Care. 2008;12(5):225.
Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS ONE. 2015;10(1):e0116949.
Razzak JA, Hyder AA, Akhtar T, Khan M, Khan UR. Assessing emergency medical care in low-income countries: a pilot study from Pakistan. BMC Emerg Med. 2008;8(1):8.
Dondorp A, Dünser M, Schultz M. Infrastructure and organization of adult intensive care units in resource-limited settings--sepsis management in resource-limited settings. 2019.
Papali A, Adhikari NK, Diaz JV, Dondorp AM, Dünser MW, Jacob ST, Phua J, et al. Infrastructure and organization of adult intensive care units in resource-limited settings. Sepsis Manag Resour-Limit Settings. 2019;2019:31–68.
Tumukunde J, Sendagire C, Ttendo SS. Development of intensive care in low-resource regions. Curr Anesthesiol Rep. 2019;9(1):15–7.
Arabi YM, Schultz MJ, Salluh JI. Intensive Care Medicine in 2050: global perspectives. Intens Care Med. 2017;43(11):1695–9.
Kübler A, Maciejewski D, Adamik B, Kaczorowska M. Mechanical ventilation in ICUs in Poland: a multi-center point-prevalence study. Med Sci Monitor: Int Med J Exp Clin Res. 2013;19:424.
Neto AS, Barbas CS, Simonis FD, Artigas-Raventós A, Canet J, Determann RM, et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): an international, multicentre, prospective study. Lancet Respir Med. 2016;4(11):882–93.
Agalu A, Woldie M, Ayele Y, Bedada W. Reasons for admission and mortalities following admissions in the intensive care unit of a specialized hospital, in Ethiopia. Int J Med Med Sci. 2014;6(9):195–200.
Bayisa T, Berhane A, Kedir S, Wuletaw T. Admission patterns and outcomes in the medical intensive care unit of St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. Ethiopian Med J. 2017;55(1):1–8.
Haftu H, Hailu T, Medhaniye A. Assessment of pattern and treatment outcome of patients admitted to pediatric intensive care unit, Ayder Referral Hospital, Tigray, Ethiopia, 2015. BMC Res Notes. 2018;11(1):1–6.
Haile S. One year retrospective review of disease patterns and clinical outcomes of patients admitted in intensive care units of Armed Force General Teaching Hospital in Addis Ababa. Ethiopia: Addis Ababa University; 2014.
Melaku Z, Alemayehu M, Oli K, Tizazu G. Pattern of admissions to the medical intensive care unit of Addis Ababa University Teaching Hospital. Ethiop Med J. 2006;44(1):33–42.
Obsa MS, Adem AO, Gete GB. Clinical outcomes of patients admitted in intensive care units of Nigist Eleni Mohammed Memorial Hospital of Hosanna, Southern Ethiopia. Int J Med Med Sci. 2017;9(6):79–85.
Smith Z, Ayele Y, McDonald P. Outcomes in critical care delivery at Jimma University Specialised Hospital, Ethiopia. Anaesth Intensive Care. 2013;41(3):363–8.
Tesema HG, Lema GF, Mesfin N, Fentie DY, Arefayne NR. Patterns of admission and clinical outcomes among patients admitted to medical intensive care unit of a Teaching and Referral Hospital, Northwest Ethiopia. Global Advances in Health and Medicine. 2021;10:2164956121989258.
Abate SM, Assen S, Yinges M, Basu B. Survival and predictors of mortality among patients admitted to the intensive care units in southern Ethiopia: A multi-center cohort study. Annals Med Surgery. 2021;65:102318.
Karthikeyan B, Kadhiravan T, Deepanjali S, Swaminathan RP. Case-mix, care processes, and outcomes in medically-ill patients receiving mechanical ventilation in a low-resource setting from southern India: a prospective clinical case series. PLoS ONE. 2015;10(8):e0135336.
Sison SM, Sivakumar GK, Caufield-Noll C, Greenough WB III, Oh ES, Galiatsatos P. Mortality outcomes of patients on chronic mechanical ventilation in different care settings: a systematic review. Heliyon. 2021;7(2):e06230.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Rose L, McGinlay M, Amin R, Burns KE, Connolly B, Hart N, et al. Variation in definition of prolonged mechanical ventilation. Respir Care. 2017;62(10):1324–32.
Damuth E, Mitchell JA, Bartock JL, Roberts BW, Trzeciak S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(7):544–53.
Association WM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Wotiye AB, Shimber ET, Ayele BA. Factors Associated with ICU Mortality at Hawassa University Comprehensive Specialized Hospital (HUCSH). Ethiopian Journal of Health Sciences. 2022;32 (3).
Abebe K, Negasa T, Argaw F. Surgical Admissions and Treatment Outcomes at a Tertiary Hospital Intensive Care Unit in Ethiopia: A Two-Year Review. Ethiopian Journal of Health Sciences. 2020. https://doi.org/10.4314/ejhs.v30i5.11.
Mehta AB, Syeda SN, Wiener RS, Walkey AJ. Epidemiological trends in invasive mechanical ventilation in the United States: a population-based study. J Crit Care. 2015;30(6):1217–21.
Fialkow L, Farenzena M, Wawrzeniak IC, Brauner JS, Vieira SRR, Vigo A, et al. Mechanical ventilation in patients in the intensive care unit of a general university hospital in southern Brazil: an epidemiological study. Clinics. 2016;71:144–51.
Sawe HR, Mfinanga JA, Lidenge SJ, Mpondo BC, Msangi S, Lugazia E, et al. Disease patterns and clinical outcomes of patients admitted in intensive care units of tertiary referral hospitals of Tanzania. BMC Int Health Hum Rights. 2014;14(1):1–8.
Bouaziz M, Bahloul M, Kallel H, Samet M, Ksibi H, Dammak H, et al. Epidemiological, clinical characteristics and outcome of severe scorpion envenomation in South Tunisia: multivariate analysis of 951 cases. Toxicon. 2008;52(8):918–26.
Lone NI, Walsh TS. Prolonged mechanical ventilation in critically ill patients: epidemiology, outcomes and modelling the potential cost consequences of establishing a regional weaning unit. Crit Care. 2011;15(2):1–10.
Chiwhane A, Diwan S. Characteristics, outcome of patients on invasive mechanical ventilation: a single center experience from central India. Egypt J Crit Care Med. 2016;4(3):113–8.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800.
Parker RK, Mwachiro EB, Mwachiro MM, Pletcher J, Parker AS, Many HR. Mortality prediction in rural Kenya: a cohort study of mechanical ventilation in critically ill patients. Critical Care Explor. 2019;1(12):e0067.
Nyawale HA. Incidence, bacteria etiology and factors associated with ventilator-associated pneumonia among patients on mechanical ventilator in intensive care units at tertiary hospitals. Dar es Salaam: Muhimbili University of Health and Allied Sciences; 2020.
Riviello ED, Kiviri W, Fowler RA, Mueller A, Novack V, Banner-Goodspeed VM, et al. Predicting mortality in low-income country ICUs: the Rwanda Mortality Probability Model (R-MPM). PLoS ONE. 2016;11(5):e0155858.
Inchai J, Pothirat C, Liwsrisakun C, Deesomchok A, Kositsakulchai W, Chalermpanchai N. Ventilator-associated pneumonia: epidemiology and prognostic indicators of 30-day mortality. Jpn J Infect Dis. 2015;68(3):181–6.
Onyekwulu F, Anya S. Pattern of admission and outcome of patients admitted into the Intensive Care Unit of University of Nigeria Teaching Hospital Enugu: a 5-year review. Niger J Clin Pract. 2015;18(6):775–9.
Sawe HR, Mfinanga JA, Lidenge SJ, Mpondo BCT, Msangi S, Lugazia E, et al. Disease patterns and clinical outcomes of patients admitted in intensive care units of tertiary referral hospitals of Tanzania. BMC Int Health Hum Rights. 2014;14(1):26.
Demass TB, Guadie AG, Mengistu TB, Belay ZA, Melese AA, Berneh AA, et al. The Burden of intensive care unit mortality and the Predictors in Amhara regional state, Northwest Ethiopia. 2022.
De Vasconcellos K, Skinner D, Rodseth R, Gopalan D, Muckart D, Banoof Z, et al. Outcomes 30 days after ICU admission: the 30DOS study. Southern African J Anaesth Analg. 2017;23(6):139–44.
Acknowledgements
The authors would like to acknowledge Dilla University for its financial and technical support and encouragement to carry out the project.
Funding
This project was funded by Dilla University.
Author information
Authors and Affiliations
Contributions
SA conceived the idea and design of the project. SA, BJ, SA, BM, and TT were involved in data cleaning, data entry, analysis, and manuscript preparation. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from the parent/guardian for all eligible participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Figure S3. Duration of mechanical ventilation among patients in the intensive care Unit.
Additional file 2
. Supplemental Table S1: Admission diagnosis and indication of Participants on Mechanical Ventilation in Southern Ethiopia Comprehensive Referral Hospitals (N = 630).
Additional file 3
. Supplemental Table S2: Multilevel bivariate analysis of association between risk factors and 28-day mortality among ICU patients on Mechanical ventilator in Southern Ethiopia (N = 630).
Additional file 4
. Supplemental Table S3. Area Under the curve for APACHE II, modified APACHE II, SOFA, modified SOFA, and albumin.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abate, S.M., Basu, B., Jemal, B. et al. Pattern of disease and determinants of mortality among ICU patients on mechanical ventilator in Sub-Saharan Africa: a multilevel analysis. Crit Care 27, 37 (2023). https://doi.org/10.1186/s13054-023-04316-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04316-w