Abstract
Background
Red blood cell distribution width (RDW) to platelet ratio (RPR) is a novel inflammatory indicator. It integrates the risk prediction of RDW and platelet, which is associated with adverse outcomes. However, the predictive power of RPR in mortality for patients with acute myocardial infarction (AMI) remains uncertain. Thus, we aimed to explore the association between RPR and 180-day in-hospital mortality in patients with AMI.
Methods
Data on patients with AMI were extracted from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. Patients were divided into two groups according to the optimal RPR cut-off value. The survival curve between high and low RPR groups was plotted via the Kaplan-Meier (KM) method. Univariate and multivariate Cox regression analyses were performed to determine the association between RPR on admission and 180-day in-hospital mortality.
Results
A total of 1266 patients were enrolled, of which 83 (6.8%) died within 180 days during the hospitalization. Compared with the survivor group, the non-survivor group had higher RPR on admission (0.11 ± 0.07 vs. 0.08 ± 0.06, P < 0.001). The KM curve indicated that the survival probability of low RPR group was higher than that of high RPR group. Multivariate Cox regression analysis demonstrated that higher RPR on admission was an independent and effective predictor of 180-day mortality in patients with AMI (hazard ratio [HR]: 2.677, 95% confidence interval [CI]: 1.159–6.188, P = 0.021).
Conclusion
Higher RPR was associated with higher in-hospital 180-day mortality in patients with AMI.
Similar content being viewed by others
Introduction
With the increasing incidence and prevalence of coronary atherosclerosis, over 200,000 hospital visits each year are associated with myocardial infarction [1, 2]. The acute myocardial infarction (AMI) is characterized by the evidence of myocardial necrosis in a clinical setting consistent with acute myocardial ischemia [3]. Although the diagnostic criteria and major treatment strategies for AMI are well defined [4], the mortality rates for such patients remains high. Therefore, how to define high-risk patients is extremely important for the survival of patients with AMI.
Inflammation is one of the main factors contributing to coronary heart disease which leads to plaque instability and rupture [1]. Red blood cell distribution width (RDW) is associated with heterogeneous cell population [5], which can be used as a reliable indicator for anisocytosis [6]. Recent studies had suggested that inflammation, neurohormone and adrenergic system activation may affect erythrocyte maturation by interfering with erythrocyte membrane, resulting in elevated RDW [5, 7, 8]. RDW has been found to be an extremely effective prognostic predictor in patients with AMI [9, 10].
Platelets play a key role in the pathophysiology of AMI, associated with endothelial cell activation and, together with fibrin, form thrombus within coronary arteries [11]. Platelets not only participate in the formation of blood clots, but also release mediators that form and maintain local inflammatory responses. Several previous studies [12, 13] had shown that a decreased platelet count was associated with the severity of MI, death and reinfarction. However, the relationship between platelet counts and the prognosis of MI was controversial [14,15,16,17,18].
The RDW-to-platelets ratio (RPR), a combination of two independent parameters, has been established as a new index to reflect the severity of inflammation [19, 20]. RPR had been proved as a prognostic marker in breast cancer [19, 21], cardiovascular diseases [22, 23], acute pancreatitis [24, 25] and chronic hepatic [26, 27]. While RPR is related to the clinical prognosis of patients with cardiovascular diseases [22, 23], the predictive power of RPR in mortality for AMI patients remains uncertain. The aim of the present study was to investigate the relationship between RPR on admission and short-term mortality within 180 days in patients with AMI.
Method
Study design and patient selection
Data were extracted from the database of Medical Information Mart for Intensive Care IV (MIMIC-IV). The MIMIC-IV database contains clinical data of patients admitted to the Intensive Care Unit (ICU) of Beth Israel Deaconess Medical Center (BIDMC) from 2008 to 2019 inclusive. All patients’ identifiers were removed and patients’ privacy was well protected so that the requirement for informed consent was waived. The MIMIC-IV database is a freely available database, one of the authors who completed the online training course of Data or Specimens Only Research included in Human Research (certification number: 50,765,560) extracted the data. Data extraction was performed using PostgreSQL software (version 6.11).
AMI is defined as being present when blood levels of cardiac troponin (cTn) are increased above the 99th percentile upper reference limit and at least one of the following: 1) Symptoms of MI; 2) New ischaemic electrocardiogram changes; 3) Development of pathological Q waves; 4) Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischaemic aetiology; 5) Identification of a coronary thrombus by angiography or autopsy [28].
Patients who met the diagnosis of AMI were enrolled in the study. Exclusion criteria were as follows: 1) age < 18 years old; 2) patients who were diagnosed with infection, cancer (including hematologic malignancies); 3) RPR on admission records were not available. 4) patients who stayed in the ICU for less than 24 h or without ICU stay record. For patients with multiple admissions, only the first admission data were recorded.
Data collection
Baseline data including gender, age, ethnicity, and concomitant disease (such as hypertension, diabetes mellitus, cardiac arrhythmia) were extracted. Clinical parameters including Troponin T, Creatine Kinase-MB (CK-MB), blood routine examination and other data were also included in the analysis. The RPR, the main factor we intended to study, was calculated as follows: RPR = RDW / platelet count. We also recorded patients’ surgical procedures including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). Missing values greater than 30% of parameters were excluded due to potential bias.
Endpoint event
The endpoint of this study was all-cause in-hospital mortality within 180 days.
Statistical analyses
The normality of continuous variables was analyzed using the skewness kurtosis normality test. Continuous variables were expressed as the mean with standard deviation (for normal distribution) or median with interquartile range (for non-normal distribution), while categorical variables were presented as numbers and percentages. Independent samples t-tests were performed to compare the differences between the group of survivor and non-survivor group. If continuous variables were normally distributed, otherwise, Mann-Whitney test were used. Chi-square test was used for comparison of categorized variables. Receiver operating characteristic (ROC) curves were used to determine the optimal cut-off value of RPR on admission. Patients in this study were separated into a high admission RPR group and a low admission RPR group according to the optimum cut-off value. The Kaplan-Meier (KM) method was used to plot survival curves of two groups with different RPR on admission, with statistical significance examined by the log-rank test. Univariate and multivariate Cox regression analyses were performed to determine the association between RPR on admission and in-hospital mortality. For variables whose P value was less than 0.05 in univariate analysis were considered as potential risk factors and were selected to the multivariate Cox regression model. In addition, the collinearity of variable was tested by variance inflation factors and the equal proportional-hazards assumption also be determined. Interaction analysis was used to determine whether there is an interaction between other variables and RPR. A two-sided P < 0.05 was considered statistically significant.
Results
Baseline characteristics on enrolled patients
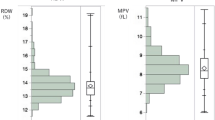
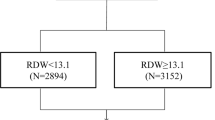
A total of 1269 patients were enrolled in the study (Fig. 1), of which 843 (66.4%) were men. A comparison of baseline characteristics between the survivor and non-survivor groups based on prognosis within 180 days of admission to ICU was shown in Table 1. The average age of the patients was 68.8 ± 12.6 years. 83 patients died within 180 days of admission (mean length of stay: 122.4 ± 57.9 days). We found that patients in the non-survivor group had higher RPR on admission than patients in the survivor group (0.11 ± 0.07 vs. 0.08 ± 0.06, P < 0.001). In addition, other variables such as platelet, RDW, troponin T and creatinine showed significant differences between the two groups. There was no significant difference between the two groups for concomitant disease, such as hypertension, diabetes mellitus, cardiac arrhythmia.
Clinical outcomes
The ROC curve showed the optimal cut-off value of RPR on admission was 0.11. There were 221(17.4%) patients with RPR ≥ 0.11 on admission. Figure 2 showed KM curves for in-hospital mortality among patients stratified by RPR on admission. And we found that compared to the low RPR group, the high RPR group had a significantly higher rate of in-hospital mortality (hazard ratio [HR]: 2.750, 95% confidence interval [CI]: 1.766–4.276, P < 0.001). Figure 3 showed that the rate of in-hospital mortality of patients in high RPR group was about three times higher than that of patients with low RPR group.
Univariate regression analysis demonstrated that many variables were associated with acute phase mortality within 180 days of patients with AMI (Table 2). Clinical characteristics including gender, age, ethnicity and other factors as well as laboratory parameters such as BUN, creatinine and so on were associated with in-hospital mortality in patient with AMI patients. Interestingly, concomitant diseases such as heart failure, hypertension, and diabetes were not shown to be associated with the endpoint event. Multivariate Cox regression analysis revealed that a higher RPR on admission was an independent risk factor for in-hospital mortality in patients with AMI (HR: 2.677,95% CI: 1.159–6.188, P = 0.021), despite confounding factors such as age, ethnicity other factors. We also observed that the older age (HR: 1.031, 95% CI: 1.005–1.507, P = 0.019), higher CK-MB (HR: 1.003, 95% CI: 1.000–1.006, P = 0.04), and higher blood glucose (HR: 1.004, 95 CI%: 1.002–1.006, P < 0.001), were associated with higher acute mortality, while white patients (HR: 0.403, 95% CI: 0.230–0.705, P = 0.001) and patients undergoing CABG (HR: 0.084, 95% CI: 0.011–0.623, P = 0.015) had a lower risk of death.
Discussion
For the first time, the relationship between RPR and mortality in patients with AMI was evaluated. We compared the survivor and non-survivor groups of patients admitted to the ICU with AMI. The main findings of this study are as follows: 1) patients with AMI who died within 180 days had higher RPR on admission; 2) the rate of in-hospital mortality was significantly higher in patients with high RPR than in those with low RPR; 3) RPR on admission was an independent predictor of in-hospital mortality within 180 days in patients with AMI.
Recent studies had shown that elevated RDW was related to higher mortality in patients with AMI [29, 30]. A study of 3100 patients from the MIMIC-IV database showed that a higher RDW was associated with increased risks of in-hospital mortality in patients with AMI [31]. Another study enrolling 763 patients with AMI undergoing a primary PCI proved that a high RDW level on admission was associated with an increased risk for intrahospital cardiovascular mortality [32]. Coronary atherosclerosis is a chronic disease with stable and unstable periods. If the blood vessel wall is irritated by inflammation, a patient who in an unstable period may deteriorate to MI. Increased systemic and local inflammation play a key role in the pathophysiology of Acute coronary syndrome (ACS) [33]. Elevated RDW has been shown to be associated with severe inflammation [34]. Inflammatory factors desensitize bone marrow erythroid progenitor cells, blocking the anti-apoptotic and pro-maturation effects of erythropoietin. Resulting in a large number of reticulocytes to enter the peripheral blood and an increase in RDW [35]. It also led to the change of red blood cells (RBCs) lipid structure, and the destruction of RBCs degeneration ability. As a result, the oxygen carrying capacity of RBCs decreases and the viscosity of whole blood increases, which increases the risk of death in patients with MI [36, 37].
Platelet was associated with the activation of endothelial cells and was important in the pathogenesis of ACS [33]. Several studies had reported the evidence that decreased platelet counts were related to increased MI size and severity and mortality or reinfarction rates [12, 13]. A study demonstrated that decreased platelet counts at hospital admission in post-ACS patients had relation to a significant almost two times higher 5-year mortality rate [38]. Another study including 10,793 patients with ST-segment elevation myocardial infarction (STEMI) from the Thrombolysis In Myocardial Infarction trials database demonstrated that compared with baseline values, a greater decrease in follow-up platelet counts was independently associated with an increased risk of reinfarction at 30 days (OR: 1.44, 95% CI:1.13–1.82, P = 0.03) [39] These results were consistent with our findings, that the non-survivor group had lower platelet counts on admission compared with the survivor group.
RPR, as a potential indicator of inflammatory processes, is calculated as the ratio of RDW to platelet count. RPR was considered to be an effective prognostic factor for many diseases [19, 20, 40,41,42,43]. One study performed by Lehmann et al. proved that patients after deep-seated intracerebral hemorrhage (ICH) with a low baseline RPR were distinguished by significantly lower case-fatality at 90 days compared to patients with a high baseline RPR (27 vs. 57%; P = 0.003, OR: 3.6, 95% CI: 1.6–8.3) [20]. Zhu et al. demonstrated that RPR was an effective predictor of cardiovascular events in hemodialysis patients, with the areas under the ROC curves of 0.88 [41]. Another study including 470 STEMI patients with PCI, demonstrated that higher RPR was associated with an increased risk for in-hospital and long-term major adverse cardiovascular events (MACE), all-cause mortality and cardiovascular mortality [23]. In the development of atherosclerosis, unstable atherosclerotic plaque and formation of clots on the plaque surface, the inflammatory process plays an important role [44]. RPR was a combination of two inflammatory parameters that had been proved have a better ability to predict the prognosis of the disease. A study conducted by Xi et al. confirmed that compared with RDW, RPR presented better diagnostic value of hemophagocytic lymphohistiocytosis (HLH). Moreover, RPR had a better ability to monitor the effects of treatment on HLH [43]. Studies have shown that Troponin T and CKMB are positively correlated with AMI extent [45], which was consistent with our study. In our study, Troponin T and CKMB were both higher in the non-survivor group than in the survivor group, accompanied by higher RPR, suggesting that RPR may also be a predictor of poor outcomes in patients with AMI. RPR, as a readily available and economical blood routine parameter, has been neglected in clinical practice. Our study demonstrated the importance of RPR, as a potential indicator of inflammation, in predicting in-hospital mortality within 180 days in patients with AMI. After adjusting sex, age, concomitant disease, and treatment, RPR remained an independent predictor of mortality in patients with AMI. However, there are few studies on RPR at present. In the current practical application, RPR should be combined with other clinical indicators to better verify the clinical prognosis of AMI.
Limitations
As a single center, retrospective, small cohort study, there may still be uncontrollable factors affecting the outcome even if adjusted by analysis. We did not conduct subgroup analysis according to the severity of MI, but only analyzed and discussed according to the survival status of patients. A piece of missing data, such as leukocytes and neutrophils, were deleted in this study, these values may affect the outcome. Meanwhile, indicators such as smoking, drinking, and patient medication history, which may have a significant impact on patient outcomes, were not available in the database. The predictive role of RPR for all-cause mortality in patients with AMI in long-term follow-up could not be demonstrated for unavailable follow-up data in the MIMIC-IV database.
Conclusion
Based on the findings of this study, RPR, as a potential indicator of inflammatory processes, could effectively and independently predict 180-day in-hospital mortality in patients with AMI. More prospective randomized controlled studies are needed for further investigation on the effect of RPR in patients with AMI.
Data availability
The data that support the findings of this study are available from MIMIC-IV (Published: March 16th, 2021. Version: 1.0) public database. But restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA).
Abbreviations
- RDW:
-
Red blood cell distribution width
- RPR:
-
RDW to platelet ratio
- AMI:
-
Acute myocardial infarction
- MIMIC-IV:
-
Medical Information Mart for Intensive Care IV
- KM:
-
Kaplan-Meier
- HR:
-
hazard ratio
- CI:
-
confidence interval
- ICU:
-
Intensive Care Unit
- BIDMC:
-
Beth Israel Deaconess Medical Center
- CK-MB:
-
Creatine Kinase-MB
- PCI:
-
percutaneous coronary intervention
- CABG:
-
coronary artery bypass grafting
- ROC:
-
Receiver operating characteristic
- RBCs:
-
red blood cells
- ICH:
-
intracerebral hemorrhage
- MACE:
-
cardiovascular events
- HLH:
-
lymphohistiocytosis
- STEMI:
-
ST-segment elevation myocardial infarction
- ACS:
-
Acute coronary syndrome
- BUN:
-
blood urea nitrogen
- MCH:
-
mean corpuscular hemoglobin
- MCHC:
-
mean corpuscular hemoglobin concentration
- MCV:
-
mean corpuscular volume
- cTn:
-
cardiac troponin
References
Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet (London England). 2017;389(10065):197–210.
Núñez-Gil IJ, Riha H, Ramakrishna H. Review of the 2017 european Society of Cardiology’s Guidelines for the management of Acute myocardial infarction in patients presenting with ST-Segment Elevation and focused Update on Dual Antiplatelet Therapy in Coronary Artery Disease developed in collaboration with the European Association for Cardio-Thoracic surgery. J Cardiothorac Vasc Anesth. 2019;33(8):2334–43.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Third universal definition of myocardial infarction. Nat Rev Cardiol. 2012;9(11):620–33.
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, ACC/AHA/ACP/AATS et al. /PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation. 2016;134(10):e123-55.
Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. 2015;52(2):86–105.
Hoffmann JJ, Nabbe KC, van den Broek NM. Effect of age and gender on reference intervals of red blood cell distribution width (RDW) and mean red cell volume (MCV). Clin Chem Lab Med. 2015;53(12):2015–9.
Cole J, Ertoy D, Lin H, Sutliff RL, Ezan E, Guyene TT, et al. Lack of angiotensin II-facilitated erythropoiesis causes anemia in angiotensin-converting enzyme-deficient mice. J Clin Investig. 2000;106(11):1391–8.
Förhécz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohászka Z, Jánoskuti L. Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am Heart J. 2009;158(4):659–66.
Tonelli M, Sacks F, Arnold M, Moye L, Davis B, Pfeffer M. Relation between red blood cell distribution Width and Cardiovascular Event Rate in People with Coronary Disease. Circulation. 2008;117(2):163–8.
Anderson JL, Ronnow BS, Horne BD, Carlquist JF, May HT, Bair TL, et al. Usefulness of a complete blood count-derived risk score to predict incident mortality in patients with suspected cardiovascular disease. Am J Cardiol. 2007;99(2):169–74.
Falk E, Nakano M, Bentzon JF, Finn AV, Virmani R. Update on acute coronary syndromes: the pathologists’ view. Eur Heart J. 2013;34(10):719–28.
Roh JW, Lim S, Hwang Y, Lee KY, Choo EH, Choi IJ et al. Ischemic and Bleeding Events Associated with Thrombocytopenia and Thrombocytosis after Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction. J Clin Med. 2020;9(10).
Patel SJ, Ajebo G, Kota V, Guddati AK. Outcomes of hospitalized patients with myocardial infarction and immune thrombocytopenic purpura: a cross sectional study over 15 years. Am J blood Res. 2020;10(5):210–6.
Quan XQ, Ji HY, Jiang J, Huang JB, Zhang CT. Prognostic utility of the combination of platelet count with neutrophil-to-lymphocyte ratio in aged patients with Acute Myocardial Infarction undergoing percutaneous coronary intervention. Emerg Med Int. 2021;2021:4023472.
Fawzy A, Anderson JA, Cowans NJ, Crim C, Wise R, Yates JC, et al. Association of platelet count with all-cause mortality and risk of cardiovascular and respiratory morbidity in stable COPD. Respir Res. 2019;20(1):86.
Patti G, Di Martino G, Ricci F, Renda G, Gallina S, Hamrefors V, et al. Platelet indices and risk of Death and Cardiovascular events: results from a large Population-Based Cohort Study. Thromb Haemost. 2019;119(11):1773–84.
Song PS, Ahn KT, Jeong JO, Jeon KH, Song YB, Gwon HC et al. Association of baseline platelet count with all-cause mortality after acute myocardial infarction. European heart journal Acute cardiovascular care. 2020:2048872620925257.
Sharif D, Abu-Salem M, Sharif-Rasslan A, Rosenschein U. Platelet counts on admission affect coronary flow, myocardial perfusion and left ventricular systolic function after primary percutaneous coronary intervention. Eur heart J Acute Cardiovasc care. 2017;6(7):632–9.
Takeuchi H, Abe M, Takumi Y, Hashimoto T, Miyawaki M, Okamoto T, et al. Elevated red cell distribution width to platelet count ratio predicts poor prognosis in patients with breast cancer. Sci Rep. 2019;9(1):3033.
Lehmann F, Schenk LM, Bernstock JD, Bode C, Borger V, Gessler FA, et al. Elevated red cell distribution width to platelet ratio is Associated with poor prognosis in patients with spontaneous, deep-seated Intracerebral Hemorrhage. Front Neurol. 2021;12:751510.
Takeuchi H, Abe M, Takumi Y, Hashimoto T, Kobayashi R, Osoegawa A, et al. The prognostic impact of the platelet distribution width-to-platelet count ratio in patients with breast cancer. PLoS ONE. 2017;12(12):e0189166.
Celık T, Balta S, Demır M, Yıldırım AO, Kaya MG, Ozturk C, et al. Predictive value of admission red cell distribution width-platelet ratio for no-reflow phenomenon in acute ST segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Cardiol J. 2016;23(1):84–92.
Pusuroglu H, Cakmak HA, Akgul O, Erturk M, Surgit O, Akkaya E, et al. The prognostic value of admission red cell distribution width-to-platelet ratio in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Revista portuguesa de cardiologia: orgao oficial da sociedade portuguesa de cardiologia = portuguese. J Cardiol : official J Portuguese Soc Cardiol. 2015;34(10):597–606.
İlhan M, İlhan G, Gök AF, Bademler S, Verit Atmaca F, Ertekin C. Evaluation of neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and red blood cell distribution width-platelet ratio as early predictor of acute pancreatitis in pregnancy. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies. Int Soc Perinat Obstet. 2016;29(9):1476–80.
Cetinkaya E, Senol K, Saylam B, Tez M. Red cell distribution width to platelet ratio: new and promising prognostic marker in acute pancreatitis. World J Gastroenterol. 2014;20(39):14450–4.
Karagöz E, Tanoğlu A, Ülçay A, Erdem H, Turhan V, Kara M, et al. Mean platelet volume and red cell distribution width to platelet ratio for predicting the severity of hepatic fibrosis in patients with chronic hepatitis C. Eur J Gastroenterol Hepatol. 2016;28(7):744–8.
Taefi A, Huang CC, Kolli K, Ebrahimi S, Patel M. Red cell distribution width to platelet ratio, a useful indicator of liver fibrosis in chronic hepatitis patients. Hep Intl. 2015;9(3):454–60.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237–69.
Ferreira JP, Lamiral Z, Bakris G, Mehta C, White WB, Zannad F. Red cell distribution width in patients with diabetes and myocardial infarction: an analysis from the EXAMINE trial. Diabetes Obes Metab. 2021;23(7):1580–7.
Lin G, Dai C, Xu K, Wu M. Predictive value of neutrophil to lymphocyte ratio and red cell distribution width on death for ST segment elevation myocardial infarction. Sci Rep. 2021;11(1):11506.
Huang S, Zhou Q, Guo N, Zhang Z, Luo L, Luo Y, et al. Association between red blood cell distribution width and in-hospital mortality in acute myocardial infarction. Medicine. 2021;100(15):e25404.
İlhan E, Güvenç TS, Altay S, Çağdaş M, Çalik AN, Karaca M, et al. Predictive value of red cell distribution width in intrahospital mortality and postintervention thrombolysis in myocardial infarction flow in patients with acute anterior myocardial infarction. Coron Artery Dis. 2012;23(7):450–4.
Budzianowski J, Pieszko K, Burchardt P, Rzeźniczak J, Hiczkiewicz J. The role of hematological indices in patients with Acute Coronary Syndrome. Dis Markers. 2017;2017:3041565.
Tsimikas S, Willerson JT, Ridker PM. C-reactive protein and other emerging blood biomarkers to optimize risk stratification of vulnerable patients. J Am Coll Cardiol. 2006;47(8 Suppl):C19–31.
Afsar B, Saglam M, Yuceturk C, Agca E. The relationship between red cell distribution width with erythropoietin resistance in iron replete hemodialysis patients. Eur J Intern Med. 2013;24(3):e25–9.
Xanthopoulos A, Giamouzis G, Dimos A, Skoularigki E, Starling RC, Skoularigis J et al. Red Blood Cell Distribution Width in Heart Failure: Pathophysiology, Prognostic Role, Controversies and Dilemmas. J Clin Med. 2022;11(7).
Pernow J, Mahdi A, Yang J, Zhou Z. Red blood cell dysfunction: a new player in cardiovascular disease. Cardiovascular Res. 2019;115(11):1596–605.
Małyszczak A, Łukawska A, Dyląg I, Lis W, Mysiak A, Kuliczkowski W. Blood platelet count at Hospital Admission Impacts Long-Term Mortality in patients with Acute Coronary Syndrome. Cardiology. 2020;145(3):148–54.
Ly HQ, Kirtane AJ, Murphy SA, Buros J, Cannon CP, Braunwald E, et al. Association of platelet counts on presentation and clinical outcomes in ST-elevation myocardial infarction (from the TIMI trials). Am J Cardiol. 2006;98(1):1–5.
Chen B, Ye B, Zhang J, Ying L, Chen Y. RDW to platelet ratio: a novel noninvasive index for predicting hepatic fibrosis and cirrhosis in chronic hepatitis B. PLoS ONE. 2013;8(7):e68780.
Zhu X, Li G, Li S, Gong Z, Liu J, Song S. Neutrophil-to-lymphocyte ratio and red blood cell distribution width-to-platelet ratio predict cardiovascular events in hemodialysis patients. Experimental and therapeutic medicine. 2020;20(2):1105–14.
Qiu L, Chen C, Li SJ, Wang C, Guo F, Peszel A, et al. Prognostic values of red blood cell distribution width, platelet count, and red cell distribution width-to-platelet ratio for severe burn injury. Sci Rep. 2017;7(1):13720.
Xi Y, Bai Y. Diagnostic value of red blood cell distribution width, platelet distribution width, and red blood cell distribution width to platelet ratio in children with hemophagocytic lymphohistiocytosis. J Clin Lab Anal. 2021;35(9):e23909.
Meng LB, Yu ZM, Guo P, Wang QQ, Qi RM, Shan MJ, et al. Neutrophils and neutrophil-lymphocyte ratio: inflammatory markers associated with intimal-media thickness of atherosclerosis. Thromb Res. 2018;170:45–52.
Byrne RA, Ndrepepa G, Braun S, Tiroch K, Mehilli J, Schulz S, et al. Peak cardiac troponin-T level, scintigraphic myocardial infarct size and one-year prognosis in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2010;106(9):1212–7.
Acknowledgements
We would like to thank the Massachusetts Institute of Technology and the Beth Israel Deaconess Medical Center for the MIMIC project.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Chen C created the concept and designed the study, Li L extracted the data from the database, Hong Y, RZ analyzed the data. Hong Y drafted the manuscript. Chen C revised the manuscript. All the authors had full access to all the data in the study, and took responsibility for the integrity and accuracy of the data.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Institutional Review Boards of the Beth Israel Deaconess Medical Center (BIDMC) and the Massachusetts Institute of Technology (MIT). Therefore, the First Affiliated Hospital of Wenzhou Medical University ethics committee waived the informed consent for the present study. The study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yao, H., Lian, L., Zheng, R. et al. Red blood cell distribution width/platelet ratio on admission as a predictor for in-hospital mortality in patients with acute myocardial infarction: a retrospective analysis from MIMIC-IV Database. BMC Anesthesiol 23, 113 (2023). https://doi.org/10.1186/s12871-023-02071-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02071-7