Abstract
Background
Obstructive sleep apnea (OSA) is a common disorder that is highly associated with postoperative complications. The STOP-Bang questionnaire is a simple screening tool for OSA. The objective of this systematic review and meta-analysis is to evaluate the validity of the STOP-Bang questionnaire for screening OSA in the surgical population cohort.
Methods
A systematic search of the following databases was performed from 2008 to May 2021: MEDLINE, Medline-in-process, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, PsycINFO, Journals @ Ovid, Web of Science, Scopus, and CINAHL. Continued literature surveillance was performed through October 2021.
Results
The systematic search identified 4641 articles, from which 10 studies with 3247 surgical participants were included in the final analysis. The mean age was 57.3 ± 15.2 years, and the mean BMI was 32.5 ± 10.1 kg/m2 with 47.4% male. The prevalence of all, moderate-to-severe, and severe OSA were 65.2, 37.7, and 17.0%, respectively. The pooled sensitivity of the STOP-Bang questionnaire for all, moderate-to-severe, and severe OSA was 85, 88, and 90%, and the pooled specificities were 47, 29, and 27%, respectively. The area under the curve for all, moderate-to-severe, and severe OSA was 0.84, 0.67, and 0.63.
Conclusions
In the preoperative setting, the STOP-Bang questionnaire is a valid screening tool to detect OSA in patients undergoing surgery, with a high sensitivity and a high discriminative power to reasonably exclude severe OSA with a negative predictive value of 93.2%.
Trial registration
PROSPERO registration CRD42021260451.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder, characterized by episodes of apnea and hypopnea [1]. Recognizing OSA in undiagnosed patients preoperatively is particularly important, as many analgesics, anesthetics, and sedatives are respiratory depressants that can exacerbate OSA [1, 2]. Up to 68% of patients undergoing surgery with OSA can be undiagnosed, [2, 3] resulting in increased risk of perioperative cardiovascular and pulmonary complications [2, 4,5,6,7]. Thus, an easy-to-administer screening tool for preoperative assessment of patients undergoing surgery at increased risk for OSA is essential in the armament of perioperative risk stratification.
Polysomnography (PSG) is the diagnostic standard for OSA. However, PSG can be difficult to access as it is expensive, time consuming, and requires overnight laboratory observation [8]. With limited resources for PSG and the high prevalence of OSA in the general population, several screening tools have been developed for clinicians to prioritize diagnosis and treatment in patients with increased risk of OSA. In the surgical population, the STOP-Bang questionnaire, [9] STOP questionnaire, [9] P-SAP score, [10] Berlin questionnaire, [11] and ASA checklist [11] are validated screening tools for OSA.
The STOP-Bang questionnaire is a simple tool for detecting OSA that takes approximately 1 minute to complete. It has been validated in multiple settings [9, 12,13,14,15] and used worldwide in different populations [13,14,15,16]. The STOP-Bang questionnaire consists of four binary (STOP: Snoring, Tiredness, Observed apnea, and high blood Pressure), and four demographic questions (Bang: Body mass index (BMI), age, neck circumference, and gender) [9]. When first developed, the STOP-Bang questionnaire with a cut-off score of 3 or greater had demonstrated a sensitivity of 83.9, 92.9, and 100% in detecting all OSA (Apnea–Hypopnea Index (AHI) ≥5 events per hour), moderate-to-severe OSA (AHI ≥15 events per hour), and severe OSA (AHI ≥30 events per hour), respectively [9]. As a preoperative diagnosis of OSA is associated with higher risk of complications in the perioperative setting, [4, 17,18,19] the predictive parameters of the STOP-Bang questionnaire in the surgical population should be evaluated to determine its utility in predicting perioperative complications associated with OSA. To date, no systematic review and meta-analysis has examined the validity of the STOP-Bang questionnaire to detect OSA specifically in the surgical population. The objective of this systematic review and meta-analysis is to determine the validity of the STOP-Bang questionnaire as a preoperative screening tool in identifying those at increased risk of OSA in the surgical population cohort.
Methods
Study registration
The protocol of this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO; registration CRD42021260451). The study was completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline [20].
Literature search strategy
The literature search was performed by an information specialist (ME) using the Ovid platform for the following databases: MedlineALL, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, APA PsycINFO, and Journals@Ovid. CINAHL, the Web of Science, and Scopus (Elsevier) were also searched. Search components consisted of (“stop-bang” or “stopbang”) AND (perioperative or postoperative or surgery) related terms. Searches were limited to the years 2008 (development of STOP-Bang questionnaire) to May 14, 2021. No other limits were applied. Literature surveillance was performed through November 2021. The Medline search strategy is provided in the supplemental material (Appendix 1).
Study selection and data management
Title and abstract screening, and full text evaluation were independently completed by two reviewers (MH, NG) using Covidence. Full text articles meeting the following inclusion criteria were included: 1) the study screened for OSA using the STOP-Bang questionnaire in adult patients aged ≥18 years undergoing surgery; 2) OSA diagnosis confirmed by PSG or home sleep apnea testing (HSAT); 3) severity of OSA measured by Apnea Hypopnea Index (AHI) or Respiratory Disturbance Index (RDI) cut-offs ≥5, ≥ 15, and ≥ 30 events per hour; and 4) accuracy of the STOP-Bang questionnaire assessed with predictive parameters. The two reviewers extracted data from the included studies with a standardized form. A third reviewer (AS) resolved any discrepancy between the reviewers. Data collection was managed in Excel (Redmond, United States).
Evaluation of methodological quality
Two reviewers (MH, NG) independently evaluated bias of the included studies. The assessment was conducted using criteria for internal and external validity coded using the Cochrane Screening and Diagnostic Tests Methods Group [21]. The result of the evaluation was compared and a third reviewer (AS) resolved any discrepancies. Internal validity was assessed using the following criteria: valid reference standard, definition of disease, blind execution of index and reference tests, interpretation of index test independent of clinical information, and study design. External validity was assessed using the following criteria: disease spectrum, clinical setting, previous screening or referral filter, demographic information, explicit cut-off of index test, percentage of missing participants, management of missing data, and selection of participants for the reference test. Furthermore, the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool was used by the reviewers to rate the quality of individual included study on a scale ranging from 0 to 14 [22].
Statistical analysis
Meta-analysis was performed with Review Manager Version 5.4 and Meta-disc V.1.4. For each of the included studies, 2 × 2 contingency tables were created to obtain predictive parameters with 95% confidence intervals. The following pooled predictive parameters were calculated using a bivariate random-effects model: sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), diagnostic odds ratio (DOR), likelihood ratios, and area under the curve (AUC) to evaluate the validity of the STOP-Bang questionnaire for different OSA severities defined by AHI cut-offs: AHI ≥ 5 (all), AHI ≥ 15 (moderate-to-severe), and AHI ≥ 30 (severe) events per hour. A STOP-Bang score of three or greater was accepted as the threshold and post-test probabilities were calculated as described by Brooks et al. [23] Also, the pooled predictive parameters of additional STOP-Bang score thresholds were calculated for different OSA severities.
Meta-regression and sensitivity analysis were performed for moderate-to-severe and severe OSA using Open Meta Analyst software [24] for categorical variables (validation tools and study type) and continuous variables (age, male gender, BMI, neck circumference, prevalence, and sample size). We focused to measure the association between these variables and the combined estimates of sensitivity, specificity, and log scale diagnostic odds ratio. Leave-one-study-out analysis was performed to examine the effect, if any, of individual study on the reliability of the combined estimates. Level of statistical significance was set at p value < 0.05.
Results
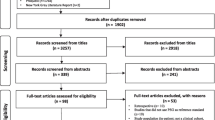
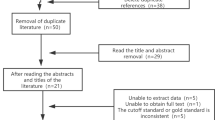
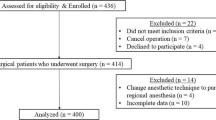
The search of literature identified 4641 articles, from which 2029 duplicates were removed (Fig. 1). Following the review of titles and abstracts, 2586 studies did not meet the inclusion criteria and were excluded. The full text of the remaining 26 studies were reviewed, and 16 full text articles [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] were excluded due to reasons listed in Supplementary Table S1. The review included 10 articles that satisfied the inclusion criteria [41,42,43,44,45,46,47,48,49,50]. Of note, Nunes et al. [42] and Waseem et al. [50] included two and four subgroups, respectively, yielding a total of 14 included study groups. The included studies involved 3247 surgical patients who were preoperatively evaluated for OSA.
The demographic data of the included studies are summarized in Table 1. In surgical patients, the mean age was 57.3 ± 15.2 years, mean BMI was 32.5 ± 10.1 kg/m2, and 47% were male. Seven studies [41,42,43,44, 47, 49, 50] were of prospective design and three studies were retrospective [45, 46, 48]. The characteristics of the included studies are summarized in Table 2. Surgical procedures comprised of non-cardiac elective surgery [41, 44, 50] (n = 3), abdominal surgery [42] (n = 1), coronary artery bypass grafting [42] (n = 1), bariatric surgery [45, 46, 48, 49] (n = 4), and total joint arthroplasty [47] (n = 1). The study by Nunes et al. had two different populations of surgical patients (abdominal surgery and coronary artery bypass grafting) [42]. Among the surgical population, four studies included AHI cut off ≥5 [41, 43, 44, 47], eight included AHI cut off ≥15 [41,42,43, 45, 47,48,49,50], and five included cut off AHI ≥30 events per hour [41, 43, 45, 47, 50] (Figs. 2 and 3).
Forest plot of pooled sensitivity and specificity of STOP-Bang questionnaire for various OSA severities in surgical patients. Values are presented as means with 95% CI in parentheses. Abbreviations: AHI, Apnea–Hypopnea index; Bang, body mass index, age, neck circumference and gender; CABG, coronary artery bypass graft surgery; CI, confidence interval; OSA, obstructive sleep apnea; STOP, snoring, tiredness, observed apnea and high blood pressure
Forest plot of pooled diagnostic odds ratio of STOP-Bang questionnaire for various OSA severities in surgical patients. Values are presented as means with 95% CI in parentheses. Abbreviations: AHI, Apnea–Hypopnea index; Bang, body mass index, age, neck circumference and gender; CABG, coronary artery bypass graft surgery; CI, confidence interval; OR, odds ratio; OSA, obstructive sleep apnea; STOP, snoring, tiredness, observed apnea and high blood pressure
Methodological quality of the included studies
The included studies had QUADAS scores ranging from 9 to 13, denoting a moderate risk of bias (Table 1). PSG or HSAT was used as a reference test in all included studies to determine the accuracy of the STOP-Bang questionnaire (Table 2). Three studies [42, 43, 45] exclusively used PSG, two [41, 48] used a mix of PSG and HSAT, and five [44, 46, 47, 49, 50] used HSAT. Although the standard for the diagnosis of OSA is PSG, there were no significant disparities between studies that used PSG or HSAT regarding prevalence of OSA (Table 2) and accuracy of the STOP-Bang questionnaire (Fig. 2).
The evaluation of internal and external validities of the included studies is summarized in Supplementary Tables S2 and S3. Regarding the internal validity, index and reference tests were blindly executed in five studies [41, 44, 45, 49, 50] and STOP-Bang scores were interpreted independently from clinical data in two studies [44, 50] (Supplementary Table S2). All but one study [43], which had unspecified inclusion criteria, fully described their inclusion and exclusion criteria. In all 10 studies, adequate information was provided to describe the study setting and the demographics of the surgical patients, including age, sex, and BMI. Although one study [43] did not randomly select patients for PSG, all studies applied the STOP-Bang questionnaire without pre-screening for OSA. Overall, there is a low risk of bias in subject selection for the reference test across the 10 studies.
Accuracy of the STOP-Bang questionnaire in surgical patients
For the STOP-Bang questionnaire, the pooled predictive parameters of a score three or greater to screen for OSA in patients undergoing surgery are presented in Table 3 and Figs. 2 and 3. The prevalence of all, moderate-to-severe, and severe OSA was 65, 38, and 17% respectively. The pooled sensitivity of the STOP-Bang questionnaire was high at 85% (95%CI: 82, 88%, I2: 40.9%), 88% (95%CI: 85, 89%, I2: 85.7%), and 90% (95%CI: 87, 93%, I2: 86.9%) in screening for all, moderate-to-severe, and severe OSA, respectively. The pooled specificity was moderate at 47% (95%CI: 42, 52%, I2: 87.2%), 29% (95%CI: 27, 32%, I2: 89.9%), and 27% (95%CI: 25, 29%, I2: 93.1%) for all, moderate-to-severe, and severe OSA, respectively.
The pooled positive predictive value (PPV) was highest at 75% (95%CI: 71.8, 77.7%) in detecting all OSA, and the corresponding PPVs for moderate-to-severe and severe OSA were 43% (95%CI: 40.8, 45.0%) and 20% (95%CI: 18.5, 22.2%), respectively (Table 3). The negative predictive value (NPV) for severe OSA was highest at 93.2% (95%CI: 90.9, 95.1%), indicating that the STOP-Bang questionnaire can reasonably rule-out severe OSA. A negative score of 0–2 would decrease the probability of diagnosing severe OSA from 17.0 to 5.2%. The corresponding NPV values for all and moderate-to-severe OSA were 62.7% (95% CI: 56.9, 68.1%) and 79.6% (95% CI: 76.2, 82.6). The area under the curve (AUC) was 0.84, 0.67, and 0.63 for all, moderate-to-severe, and severe OSA, respectively.
Accuracy of different STOP-Bang score thresholds
The accuracy of different STOP-Bang score cut-offs in surgical patients for all OSA (n = 5722), moderate-to-severe OSA (n = 12,207) and severe OSA (n = 9878) are summarized in Supplementary Table S4. With the increase in the STOP-Bang threshold from 3 to 5, the sensitivity diminished from 88 to 50% for moderate-to-severe OSA and from 90 to 61% for severe OSA. As well, there was an increase in specificity from 29 to 78% for moderate-to-severe and from 27 to 75% for severe OSA. The PPV was highest at 86% with a STOP-Bang threshold of 6 or greater for detecting all OSA. Similarly, the NPV was highest for severe OSA at 94% for a threshold of 4 or greater.
Meta-regression and sensitivity analysis
Meta-regression and sensitivity analysis were conducted for moderate-to-severe OSA with 12 study groups and for severe OSA in eight studies (Supplementary Tables S5 and S6). The analysis revealed that continuous variables marginally altered the combined estimates without significant effect on the results. Similarly, the categorical variables also marginally altered the combined estimates without significance. There was no significant effect on the results by any individual study as shown by leave-one-study-out analysis (Supplementary Fig. S1).
Discussion
To date, our study is the first systematic review and meta-analysis examining the validity of the STOP-Bang questionnaire in the preoperative setting for screening of OSA in the surgical population. We demonstrate that a STOP-Bang score three or greater has excellent AUC of 0.84 to detect OSA in patients undergoing surgery. The high sensitivity and significant diagnostic odds ratio of STOP-Bang score ≥ 3 across the three OSA severities help identify patients undergoing surgery at increased risk for OSA. Similarly, the high NPV of 93.2% can help clinicians to reasonably exclude severe OSA in patients that score 0 to 2.
The prevalence of OSA in our study was high: 65, 38, and 17% for all, moderate-to-severe, and severe OSA, respectively. This is in keeping with previously reported prevalence of OSA in surgical patients [51, 52]. Overall, the high prevalence in the surgical versus the general population [53, 54] could be a consequence of higher burden of comorbidities in patients undergoing surgery, which may be risk factors for OSA.
There may be variations in the predictive accuracy of the STOP-Bang questionnaire within different ethnic groups. Devaraj et al. found a sensitivity of 82.8% and specificity of 65.2% [44]. A recent large prospective cohort study found that the optimal BMI cut-off in Indian population to be > 27.5 kg/m2 and STOP-Bang score 4 or greater as the optimal discrimination score to predict moderate-to-severe and severe OSA [50]. Most importantly, a recent meta-analysis on the performance of STOP-Bang in different geographic regions in 47 studies with 26,547 participants found it to be a valid screening tool worldwide [13]. Our study included patients across different countries and ethnicities, and our findings apply broadly to the surgical population.
In an ideal setting, every patient with undiagnosed OSA should be identified to minimize the risk of perioperative complications. Given limited logistical, financial, and clinical resources, especially in the preoperative setting, clinicians must carefully balance between the missed cases of OSA and the use of healthcare resource to diagnose OSA. In this regard, the predictive parameters of the screening tool are important measures for clinicians to take into consideration when screening patients. Sensitivity and specificity are two parameters that are typically inversely related. We found that an increase in the STOP-Bang cut-off corresponded to increased specificity and a reciprocal decrease in sensitivity in the detection of all, moderate-to-severe, and severe OSA. Surgical patients who score three or greater on STOP-Bang have a high probability of moderate-to-severe OSA [41, 55]. We found that a STOP-Bang threshold of six or greater had the highest PPV of 86% with high specificity of 90% for detecting all OSA (Supplementary Table S4). Our finding is consistent with a recent study that showed a STOP-Bang threshold of 6 has a high specificity of 91% in detecting OSA [56]. Whereas a STOP-Bang score of three or greater can be used to risk stratify patients at increased risk of OSA, a higher threshold may be useful for a patient population with a higher prevalence of OSA to reduce false-positives. In general, surgical patients should be screened with a threshold of three or greater unless a high prevalence of OSA is suspected, in which case a threshold of five or six may be beneficial to identify those at high-risk of undiagnosed OSA and in most need of further evaluation.
Utility of the STOP-Bang questionnaire in patients undergoing surgery
Despite rising awareness and increase in prevalence of OSA in patients undergoing surgery, [53, 57] the vast majority of patients with OSA are unidentified preoperatively [2, 3, 52]. Undiagnosed OSA has been associated with difficult airway management [58] and increased postoperative complications including cardiovascular events, reintubation, respiratory complications, and longer hospital stay [2, 17, 59,60,61]. Notably, preoperative use of the STOP-Bang questionnaire to screen surgical patients to detect undiagnosed OSA has been shown to predict postoperative complications [17, 18, 28, 59, 62]. Of note, several of these studies are non-randomized, observational studies [60,61,62].
An increased severity of OSA may be associated with an increased rate of postoperative complications. Severe OSA was found to be associated with increased risk of postoperative cardiac complications [2]. Similarly, a higher incidence of postoperative complications was associated with higher OSA severity [63]. As higher STOP-Bang score is associated with higher risk of moderate-to-severe and severe OSA, [41] our findings indicate that the STOP-Bang questionnaire is a valid screening tool for preoperative risk stratification.
A recent study found that patients identified by the STOP-Bang questionnaire (score ≥ 3) as at increased risk for OSA had a 4-fold increase in post-operative cardiopulmonary events [59]. Similarly, patients with STOP-Bang score ≥ 3 experienced worse perioperative respiratory outcomes and prolonged hospital stay [62]. As such, missed awareness of OSA in surgical patients can put substantial strain on the healthcare system due to increased consumption of resources in the form of intensive care, increased ventilator support, and longer length of hospitalization [64]. Patients with OSA and compliant with their continuous positive airway pressure (CPAP) therapy were shown to have improved oxygen desaturation index on the night of surgery and were less likely to require oxygen therapy [65]. In addition, surgical patients with OSA and a CPAP prescription were associated with fewer cardiovascular complications, [17] further highlighting the importance of preoperative identification of undiagnosed OSA.
Nevertheless, limited time between preoperative evaluation and surgery, patient hesitance to undergo sleep testing, and long waitlists for sleep clinics are barriers to recognizing undiagnosed OSA. This underscores the importance of access to a robust and easy-to-administer screening tool with a high predictive accuracy. We report that that the STOP-Bang questionnaire is a valid screening tool that addresses this need with a high AUC of 0.84 for clinicians to risk-stratify preoperative patients and to plan mitigation for perioperative complications associated with OSA. Surgical patients at high risk of OSA should be considered for postoperative monitoring such as continuous oximetry and capnography [66, 67].
There are some limitations in our study. First, both PSG and HSAT were used as diagnostic tools for OSA in the included studies. Although the two are often equitable, some heterogeneity may be present as PSG is the diagnostic standard. Secondly, the internal validity was difficult to assess as blinding of the index and reference tests was unclear. Nevertheless, QUADAS tool was used to provide additional evaluation of the quality of the included studies. Lastly, our study population included a variety of surgical procedures, which may limit the applicability of our results to specific surgical populations. The combination of methodological variations in the diagnostic tools, the variability in prevalence of OSA across the studies, and the various surgical procedures likely resulted in high heterogeneity of the predictive parameters. In anticipation of this heterogeneity, a random-effects model was used for the meta-analysis. Nevertheless, our study presents a current review of the literature on the accuracy of the STOP-Bang questionnaire as a preoperative screening tool in the surgical population.
Conclusions
In summary, our systematic review and meta-analysis demonstrates the validity of the STOP-Bang questionnaire for screening of OSA in surgical patients. With a score cut-off of 3 or greater, the STOP-Bang questionnaire has a high sensitivity and NPV, demonstrating its predictive utility to detect OSA in the surgical cohort.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- AHI:
-
apnea–hypopnea index
- AUC:
-
area under the curve
- DOR:
-
diagnostic odds ratio
- HSAT:
-
home sleep apnea testing
- NPV:
-
negative predictive value
- OSA:
-
obstructive sleep apnea
- PPV:
-
positive predictive value
- PSG:
-
polysomnography
- PRISMA:
-
preferred reporting items for systematic reviews and meta-analyses
- PROSPERO:
-
international prospective register of systematic reviews
- QUADAS:
-
quality assessment of diagnostic accuracy studies
- RDI:
-
respiratory disturbance index
References
Subramani Y, Singh M, Wong J, Kushida CA, Malhotra A, Chung F. Understanding phenotypes of obstructive sleep apnea: applications in anesthesia, surgery, and perioperative medicine. Anesth Analg. 2017;124:179–91.
Chan MTV, Wang CY, Seet E, Tam S, Lai HY, Chew EFF, et al. Association of Unrecognized Obstructive Sleep Apnea with Postoperative Cardiovascular Events in patients undergoing major noncardiac surgery. JAMA. 2019;321:1788–98.
Singh M, Liao P, Kobah S, Wijeysundera DN, Shapiro C, Chung F. Proportion of surgical patients with undiagnosed obstructive sleep apnoea. Br J Anaesth. 2013;110:629–36.
Kaw R, Chung F, Pasupuleti V, Mehta J, Gay PC, Hernandez AV. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth. 2012;109:897–906.
Opperer M, Cozowicz C, Bugada D, Mokhlesi B, Kaw R, Auckley D, et al. Does obstructive sleep apnea influence perioperative outcome? A qualitative systematic review for the Society of Anesthesia and Sleep Medicine Task Force on preoperative preparation of patients with sleep-disordered breathing. Anesth Analg. 2016;122:1321–34.
Bolden N, Posner KL, Domino KB, Auckley D, Benumof JL, Herway ST, et al. Postoperative critical events associated with obstructive sleep apnea: results from the Society of Anesthesia and Sleep Medicine Obstructive Sleep Apnea Registry. Anesth Analg. 2020;131:1032–41.
Hai F, Porhomayon J, Vermont L, Frydrych L, Jaoude P, El-Solh AA. Postoperative complications in patients with obstructive sleep apnea: a meta-analysis. J Clin Anesth. 2014;26:591–600.
McNicholas WT. Diagnosis of obstructive sleep apnea in adults. Proc Am Thorac Soc. 2008;5:154–60.
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiol J Am Soc Anesthesiol. 2008;108:812–21.
Ramachandran SK, Kheterpal S, Consens F, Shanks A, Doherty TM, Morris M, et al. Derivation and validation of a simple perioperative sleep apnea prediction score. Anesth Analg. 2010;110:1007–15.
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. Validation of the Berlin questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology. 2008;108:822–30.
Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, et al. Validation of the STOP-bang questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and Meta-analysis. PLoS One. 2015;10:e0143697.
Pivetta B, Chen L, Nagappa M, Saripella A, Waseem R, Englesakis M, et al. Use and performance of the STOP-bang questionnaire for obstructive sleep apnea screening across geographic regions: a systematic review and Meta-analysis. JAMA Netw Open. 2021;4:e211009–9.
Chen L, Pivetta B, Nagappa M, Saripella A, Islam S, Englesakis M, et al. Validation of the STOP-bang questionnaire for screening of obstructive sleep apnea in the general population and commercial drivers: a systematic review and meta-analysis. Sleep Breath. 2021. https://doi.org/10.1007/s11325-021-02299-y.
Hwang M, Zhang K, Nagappa M, Saripella A, Englesakis M, Chung F. Validation of the STOP-bang questionnaire as a screening tool for obstructive sleep apnoea in patients with cardiovascular risk factors: a systematic review and meta-analysis. BMJ Open Respir Res. 2021;8:e000848.
Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-bang, and Epworth sleepiness scales. J Clin Sleep Med. 2011;07:467–72.
Mutter TC, Chateau D, Moffatt M, Ramsey C, Roos LL, Kryger M. A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology. 2014;121:707–18.
Dimitrov L, Macavei V. Can Screening Tools for Obstructive Sleep Apnea Predict Postoperative Complications? A Systematic Review of the Literature. J Clin Sleep Med. 12:1293–300.
Karimi N, Kelava M, Kothari P, Zimmerman NM, Gillinov AM, Duncan AE. Patients at high risk for obstructive sleep apnea are at increased risk for atrial fibrillation after cardiac surgery: a cohort analysis. Anesth Analg. 2018;126:2025–31.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339.
Cochrane Screening and Diagnostic Tests Methods Group. http://srdta.cochrane.org.
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
Brooks Z, Das S, Pliura T. Clinicians’ probability calculator to convert pre-test to post-test probability of SARS-CoV-2 infection based on method validation from each laboratory. EJIFCC. 2021;32:265–79.
Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational Back-end. J Stat Softw. 2012;049.
Vasu TS, Doghramji K, Cavallazzi R, Grewal R, Hirani A, Leiby B, et al. Obstructive sleep apnea syndrome and postoperative complications: clinical use of the STOP-BANG questionnaire. Arch Otolaryngol Head Neck Surg. 2010;136:1020–4.
Lockhart EM, Willingham MD, Abdallah AB, Helsten DL, Bedair BA, Thomas J, et al. Obstructive sleep apnea screening and postoperative mortality in a large surgical cohort. Sleep Med. 2013;14:407–15.
Kulkarni GV, Horst A, Eberhardt JM, Kumar S, Sarker S. Obstructive sleep apnea in general surgery patients: is it more common than we think? Am J Surg. 2014;207:436–40 discussion 439.
Seet E, Chua M, Liaw CM. High STOP-BANG questionnaire scores predict intraoperative and early postoperative adverse events. Singap Med J. 2015;56:212–6.
Dixon SE, Haas SA, Klopp A, Carlson J. A quality improvement project: using the STOP-BANG tool in a military population to improve equity in preoperative screening. J Perianesth Nurs. 2016;31:371–80.
Reed K, Pengo MF, Steier J. Screening for sleep-disordered breathing in a bariatric population. J Thorac Dis. 2016;8:268–75.
Bamgbade OA, Khaw RR, Sawati RS, Holland CM. Obstructive sleep apnea and postoperative complications among patients undergoing gynecologic oncology surgery. Int J Gynaecol Obstet. 2017;138:69–73.
Lakdawala L, Dickey B, Alrawashdeh M. Obstructive sleep apnea screening among surgical patients: a quality improvement project. J Perianesth Nurs. 2018;33:814–21.
Mason M, Hernandez-Sanchez J, Vuylsteke A, Smith I. Usefulness of the STOP-bang questionnaire in a cardiac surgical population. J Cardiothorac Vasc Anesth. 2018;32:2694–9.
Krishnasamy S, Sahid SM, Hashim SA, Singh S, Chung F, Mokhtar RAR, et al. Obstructive sleep apnoea and open heart surgery: a review of its incidence and impact to patients. J Thorac Dis. 2019;11:5453–62.
Sankar A, Beattie WS, Tait G, Wijeysundera DN. Evaluation of validity of the STOP-BANG questionnaire in major elective noncardiac surgery. Br J Anaesth. 2019;122:255–62.
Carr SN, Reinsvold RM, Heering TE, Muckler VC. Integrating the STOP-bang questionnaire into the Preanesthetic assessment at a military hospital. J Perianesth Nurs. 2020;35:368–73.
Duarte RLM, Magalhaes-da-Silveira FJ, Gozal D. Validation of the GOAL questionnaire as an obstructive sleep apnea screening instrument in bariatric surgery candidates: a Brazilian single-center study. Obes Surg. 2020;30:4802–9.
Kara S, Habesoglu MA, Yabanoglu H. Change of respiratory functions, the STOP-bang questionnaire, and Epworth sleepiness scale after bariatric surgery. Ann Ital Chir. 2020;91:633–8.
Sangkum L, Wathanavaha C, Tantrakul V, Pothong M, Karnjanarachata C. Modified STOP-bang for predicting perioperative adverse events in the Thai population. BMC Anesthesiol. 2021;21:132.
Spielmanns M, Pantev S, Turk A, Barthelmes J, Schindler M, Hermann M. Does an undetected obstructive sleep apnea influence the natural course and success of cardiac rehabilitation after cardiac surgery? Eur J Phys Rehabil Med. 2021;57:148–57.
Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108:768–75.
Nunes FS, Danzi-Soares NJ, Genta PR, Drager LF, Cesar LAM, Lorenzi-Filho G. Critical evaluation of screening questionnaires for obstructive sleep apnea in patients undergoing coronary artery bypass grafting and abdominal surgery. Sleep Breath. 2015;19:115–22.
Deflandre E, Degey S, Brichant J-F, Donneau A-F, Frognier R, Poirrier R, et al. Pre-operative ability of clinical scores to predict obstructive sleep apnea (OSA) severity in susceptible surgical patients. Obes Surg. 2017;27:716–29.
Devaraj U, Rajagopala S, Kumar A, Ramachandran P, Devereaux PJ, D’Souza GA. Undiagnosed obstructive sleep apnea and postoperative outcomes: a prospective observational study. Respir Int Rev Thorac Dis. 2017;94:18–25.
Glazer SA, Erickson AL, Crosby RD, Kieda J, Zawisza A, Deitel M. The evaluation of screening questionnaires for obstructive sleep apnea to identify high-risk obese patients undergoing bariatric surgery. Obes Surg. 2018;28:3544–52.
Horvath CM, Jossen J, Kröll D, Nett PC, Baty F, Brill A-K, et al. Prevalence and prediction of obstructive sleep apnea prior to bariatric surgery—gender-specific performance of four sleep questionnaires. Obes Surg. 2018;28:2720–6.
Spence CD, Han CT, Morrison CT, Couture CD. High rate of undiagnosed obstructive sleep apnea in patients undergoing Total joint arthroplasty. AANA J. 2018;86:282–8.
Kreitinger KY, Lui MMS, Owens RL, Schmickl CN, Grunvald E, Horgan S, et al. Screening for obstructive sleep apnea in a diverse bariatric surgery population. Obes Silver Spring Md. 2020;28:2028–34.
Lázaro J, Clavería P, Cabrejas C, Fernando J, Segura S, Marín JM. Sensitivity of a sequential model based on a questionnaire (STOP-bang vs Dixon) and nocturnal pulse oximetry for screening obstructive sleep apnea in patients with morbid obesity candidates for bariatric surgery. Endocrinol Diabetes Nutr. 2020;67:509–16.
Waseem R, Chan MTV, Wang CY, Seet E, Tam S, Loo SY, et al. Diagnostic performance of the STOP-bang questionnaire as a screening tool for obstructive sleep apnea in different ethnic groups. J Clin Sleep Med. 2021. https://doi.org/10.5664/jcsm.8940.
Lopez PP, Stefan B, Schulman CI, Byers PM. Prevalence of sleep apnea in morbidly obese patients who presented for weight loss surgery evaluation: more evidence for routine screening for obstructive sleep apnea before weight loss surgery. Am Surg. 2008;74:834–8.
Finkel KJ, Searleman AC, Tymkew H, Tanaka CY, Saager L, Safer-Zadeh E, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009;10:753–8.
Frey WC, Pilcher J. Obstructive sleep-related breathing disorders in patients evaluated for bariatric surgery. Obes Surg. 2003;13:676–83.
Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84.
Chung F, Abdullah HR, Liao P. STOP-bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016;149:631–8.
Christensson E, Franklin KA, Sahlin C, Palm A, Ulfberg J, Eriksson LI, et al. Can STOP-bang and pulse oximetry detect and exclude obstructive sleep apnea? Anesth Analg. 2018;127:736–43.
Turner K, VanDenKerkhof E, Lam M, Mackillop W. Perioperative care of patients with obstructive sleep apnea—a survey of Canadian anesthesiologists. Can J Anesth. 2006;53:299–304.
Memtsoudis SG, Cozowicz C, Nagappa M, Wong J, Joshi GP, Wong DT, et al. Society of Anesthesia and Sleep Medicine Guideline on intraoperative Management of Adult Patients with Obstructive Sleep Apnea. Anesth Analg. 2018;127:967–87.
Nagappa M, Patra J, Wong J, Subramani Y, Singh M, Ho G, et al. Association of STOP-bang questionnaire as a screening tool for sleep apnea and postoperative complications: a systematic review and Bayesian Meta-analysis of prospective and retrospective cohort studies. Anesth Analg. 2017;125:1301–8.
Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO. Sleep-disordered breathing and postoperative outcomes after bariatric surgery: analysis of the nationwide inpatient sample. Obes Surg. 2013;23:1842–51.
Feng TR, White RS, Ma X, Askin G, Pryor KO. The effect of obstructive sleep apnea on readmissions and atrial fibrillation after cardiac surgery. J Clin Anesth. 2019;56:17–23.
Chudeau N, Raveau T, Carlier L, Leblanc D, Bouhours G, Gagnadoux F, et al. The STOP-BANG questionnaire and the risk of perioperative respiratory complications in urgent surgery patients: a prospective, observational study. Anaesth Crit Care Pain Med. 2016;35:347–53.
Gali B, Whalen FX, Schroeder DR, Gay PC, Plevak DJ. Identification of patients at risk for postoperative respiratory complications using a preoperative obstructive sleep apnea screening tool and Postanesthesia care assessment. Anesthesiology. 2009;110:869–77.
Memtsoudis SG, Stundner O, Rasul R, Chiu Y-L, Sun X, Ramachandran S-K, et al. The impact of sleep apnea on postoperative utilization of resources and adverse outcomes. Anesth Analg. 2014;118:407–18.
Suen C, Wong J, Warsame K, Subramani Y, Panzarella T, Waseem R, et al. Perioperative adherence to continuous positive airway pressure and its effect on postoperative nocturnal hypoxemia in obstructive sleep apnea patients: a prospective cohort study. BMC Anesthesiol. 2021;21:142.
Kor JJ, Sprung J, Khanna AK, Weingarten TN. Continuous Monitoring Detected Respiratory Depressive Episodes in Proximity to Adverse Respiratory Events During the PRODIGY Trial. J Patient Saf. 2022;10:1097.
Lam T, Nagappa M, Wong J, Singh M, Wong D, Chung F. Continuous pulse oximetry and Capnography monitoring for postoperative respiratory depression and adverse events: a systematic review and Meta-analysis. Anesth Analg. 2017;125:2019–29.
Acknowledgements
Not applicable.
Funding
This work was supported by funding from the University Health Network Foundation and the ResMed Research Chair of Anesthesia, Sleep, and Perioperative Medicine.
Author information
Authors and Affiliations
Contributions
Study concept and design: MH, MN, FC. Literature search: ME. Acquisition, analysis, and interpretation of data: MH, NG, AS, FC. Writing of manuscript: all authors. Critical review and approval of manuscript: all authors. FC guarantees the integrity of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Frances Chung reports research support from the University Health Network Foundation, ResMed Foundation, Ontario Ministry of Health Innovation Grant, consultant to Takeda Pharma, Up-to-date royalties, STOP-Bang proprietary to University Health Network. Mahesh Nagappa reports grants from the Academic Medical Organization of South-western Ontario. All other authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table S1.
Excluded studies and reasons for exclusion. Supplementary Table S2. Appraisal of the included studies based on criteria for internal validity. Supplementary Table S3. Appraisal of the included studies based on criteria for external validity. Supplementary Table S4. Predictive parameters of various STOP-Bang cut-offs for different OSA severities in surgical patients. Supplementary Table S5. Meta-regression and sensitivity analysis of various subgroups for AHI ≥ 15. Supplementary Table S6. Meta-regression and sensitivity analysis of various subgroups for AHI ≥ 30. Supplementary Fig. S1. Leave one study out analysis. Appendix 1. MEDLINE Search Strategy
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hwang, M., Nagappa, M., Guluzade, N. et al. Validation of the STOP-Bang questionnaire as a preoperative screening tool for obstructive sleep apnea: a systematic review and meta-analysis. BMC Anesthesiol 22, 366 (2022). https://doi.org/10.1186/s12871-022-01912-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01912-1