Abstract
Background
Laryngeal mask airways (LMA) are commonly used for airway management. Complications with this device are rare. However, when they do occur, there is a high risk for respiratory problems, necessitating early diagnosis and treatment. We present the first case of a life-threatening abscess spreading in the visceral space caused by a penicillin and metronidazole resistant Prevotella Denticola after the use of an LMA.
Case presentation
A female patient was admitted to our day care centre for bunion surgery. A single use LMA size 3 (Solus®, intersurgical, Wokingham, Berkshire, United Kingdom) was successfully inserted. After surgery, the patient complained of a sore throat and amoxicillin was prescribed by the general practitioner. Three days after surgery the patient was admitted to the Intensive Care Unit (ICU) for obstructive breathing, due to an abscess in the visceral space. Retropharyngeal and certainly parapharyngeal abscesses in adults are already rare. This case however, is unique because it is the first case of abscess spreading into the visceral space after the use of an LMA. Amoxicillin/clavulanate and vancomycin were started. The abscess was incised 5 days later and microbiology showed 3 positive cultures of the anaerobe Prevotella denticola, resistant for penicillin and metronidazole, but sensitive for amoxicillin/clavulanate. The patient fully recovered.
Conclusion
LMA’s are easy to use and are established, safe tools to support ventilation of the airway. In this case, the authors hypothesise a small wound in the lateral pharyngeal wall probably created an opening into the visceral space causing infection with Prevotella denticola, supporting the idea that the pharyngeal mucosal space must be part of the visceral space. Additionally, early recognition and treatment of an LMA induced abscess is necessary to prevent evolution of complications leading to airway obstruction.
Similar content being viewed by others
Background
The laryngeal mask airway was developed by Doctor Archie Brain in 1980 as a safe alternative to endotracheal intubation and was introduced into clinical practice in 1988 in the United States [1]. This device can be placed without a laryngoscope or muscle relaxation and can be used for both spontaneous breathing and controlled mechanical ventilation. The mask was designed to adapt to the contours of the hypopharynx with its lumen facing the laryngeal opening. The distal tip of the LMA cuff presses against the upper oesophageal sphincter, its sides face into the pyriform fossae and the upper border rests against the base of the tongue. The formation of a low-pressure seal around the glottis provides a safe and effective artificial airway. Different comparison studies between the laryngeal mask airway and tracheal intubation were performed [2, 3]. The LMA became adopted into worldwide practice because of the easy and successful insertion (99,81%) and the low rate of critical incidents (0,15%) [4]. The 4TH national audit project (NAP4) in 2011 estimated that 56% of general anesthetics performed were carried out using supraglottic airway devices (SGAs). Anaesthesia events led to 16 deaths and three episodes of persistent brain damage: a mortality rate of 5.6 per million general anaesthetics, one per 180,000. Rates of death and brain damage for different airway devices (facemask, supraglottic airway, tracheal tube) varied little [5].
Indications and contra-indications for the use of laryngeal mask airway [6] are listed in Table 1.
The most commonly reported complications include: sore throat, laryngospasm, coughing, gagging, retching, vomiting, glottis closure, arytenoid dislocation and vocal cord paralysis. There is still discussion about the advantages of the LMA for reducing respiratory complications compared to the endotracheal tube. A systematic review performed by Yu in 2010 showed that, for the patients receiving general anaesthesia, the use of the LMA resulted in a statistically and clinically significant lower incidence of laryngospasm during emergence, postoperative hoarseness and coughing in comparison to an endotracheal tube (ETT) [7]. However, a recent systematic review showed no clear advantage of the LMA over ETT in incidence of postoperative airway complications. Only the LMA Supreme® (Teleflex, Westmeath, Ireland) may reduce this risk [8]. This indicates that this could also be the best choice of LMA. However, there are controversial reports about the benefits of one specific LMA over others regarding the incidence and severity of pharyngolaryngeal complications and more studies need to be done to prove this hypothesis. The i-gel (Intersurgical), invented by Chang is reported to cause less oropharyngeal mucosal injury than the LMA Protector. It is an anatomically preshaped LMA with a soft, gel-like noninflating cuff. However, the incidence of postoperative sore throat in this comparative study between the i-gel and the LMA Protector remained the same. The oropharyngeal mucosal injury in this study was evaluated by checking for presence of blood on the LMA’s surface after its removal [9]. Furthermore, in another study, one day postoperatively after general anesthesia lasting less than two hours, the i-gel, the LMA Unique and LMA Supreme were reported to cause a similar incidence of sore throat [10].
Severe respiratory complications due to retropharyngeal abscesses following injuries caused by LMA are rare [11,12,13,14,15,16]. The extension of the abscess into the parapharyngeal space is even more rare. Only two of these cases have been reported [17, 18]. We report the first patient with an abscess in the visceral space following the use of an LMA. This case is unique because of the localisation of the infection, supporting a hypothesis that the pharyngeal mucosal space must be part of the visceral space [19,20,21]. Secondly, the infection became life-threatening despite timely treatment with antibiotics due to an infection with a penicillin and metronidazole resistant Prevotella denticola.
Case presentation
Patient information
A 61-year-old female patient with a body weight of 67 kg was admitted in our day care centre for bunion surgery. Her medical history included hypertension, hypercholesterolemia, a surgical history of appendicectomy and she smoked 5 cigarettes a day. She was compliant with her medication intake (amlodipine, simvastatin, prazosin, acetylsalicylic acid) and in a healthy condition. The patient had fixed dentures. Anaesthetic care was provided by an anaesthetist with a broad clinical experience of over 30 years. Anaesthesia was induced with 120 mg propolipid, 20 mcg sufentanyl and maintained with sevoflurane 2% in an oxygen-air mixture via spontaneous ventilation. A single use LMA size 3 (Solus®, intersurgical, Wokingham, Berkshire, United Kingdom) was successfully inserted after one attempt and the cuff was inflated with 20 ml of air. There was no documentation of difficult insertion, no complications during surgery and the duration of the procedure was 80 min.
Clinical findings
The LMA was removed on recovery from general anaesthesia with the cuff deflated with evidence of a little blood on the LMA cuff. At discharge from day care centre the patient complained of a sore throat and a small amount of bloodstained sputum. This was not investigated any further and she was discharged with simple analgesics. The following day the pain in her throat became progressively worse and she presented to her general practitioner with fever, dysphagia and throat pain. Amoxicillin (500 mg (mg) 4x/day) and analgesics were prescribed as treatment for laryngitis. After three days symptoms persisted and the patient started to experience respiratory difficulty and worsening pain. The skin from the sternum bilaterally to both ears was swollen, red and warm and she was admitted to the emergency department.
Diagnostic assessment
A contrast-enhanced computer tomography (CECT) scan of the neck and upper chest showed a large collection in the visceral space, with a mass effect leading to a deviation of the trachea to the left.
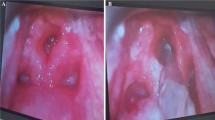
Therapeutic interventions
The patient was referred to the ICU with dyspnoea. Oxygen therapy was started and the patient was initially treated with amoxicillin/clavulanate (1000 mg 4x/day) and vancomycin (1000 mg 4x/day) followed by surgical drainage under general anaesthesia 5 days later. After thorough examination by an otolaryngologist during surgery, a minor wound was found on the lateral pharyngeal wall. Microbiology showed 3 positive cultures of the anaerobe Prevotella denticola, resistant for penicillin and metronidazole, but sensitive for amoxicillin/clavulanate. After surgery, the patient had an uneventful recovery and was discharged a few days later. The patient fully recovered following discharge. The time-line regarding the evolution of this case is found in Table 2.
Discussion and conclusion
This is a case of an abscess in the visceral space following LMA insertion for elective surgery, evolving into respiratory distress despite antibiotic therapy, with the need for admission to the ICU and incision and drainage of the abscess.
The wound
Necrotic mucosal tissue and defects in the posterior wall after use of LMA have already been reported [22]. Soft tissue necrosis could have different causes such as: over-inflation, bad positioning, incorrect sizing of the LMA, prolonged direct pressure effects due to long procedural duration and direct trauma [23]. Direct trauma had even been reported to cause bleeding, uvular damage [24], tearing of the lingual frenulum [25] and ulceration of the soft palate [26]. Even with apparent easy insertion of an LMA such complications can occur. However they may be more likely if repeated attempts at insertion are needed or excessive force is used. Table 3 shows the possible sites, types and mechanisms of traumatic injuries caused by LMA [27].
Since the patient complained of sore throat with bloodstained sputum on the day of surgery, we believe that blunt trauma to the lateral pharyngeal wall was caused by the tip of the laryngeal mask during insertion. This pharyngeal tear created a entrance for the Prevotella into the visceral space, leading to abscess formation.
Another cause in our case could have been over-inflation or bad positioning. Unfortunately, cuff pressures are not routinely measured in our institution. Therefore, relative over-inflation cannot be excluded as a cause of pharyngeal mucosal injury. However, the limit of 20 ml (milliliter) for the cuff for a size 3 as suggested by the product instruction leaflet was not exceeded. Nevertheless, routine manometry for LMA should be the standard of care [28]. We do not believe that the injury was caused by a larger than necessary LMA [29] because a size 3 was used for a female of 67 kg. Bad positioning is difficult to exclude, but there was no recorded ventilatory problem during anesthesia and there was no notification of bad positioning at removal of the LMA. However, it has already been described that 40–60% of LMA are not correctly positioned [30]. It is our belief that using a manometer should be mandatory to avoid excessive pressure, certainly in operations with a longer duration (> 1 h). Seet et al. showed that the incidence of postoperative pharyngolaryngeal adverse events could reduce by 70% while using intraoperative manometry to measure and adjust the intracuff pressure to less than 44 mmHg (millimeters of mercury) or 60 cm H2O (centimeters of water) in spontaneously breathing patients [31]. However, with the knowledge that the correct position of the LMA is only achieved 50–60% of the time [30] and that various reasons for trauma have been pointed out [27], the outcome of the patient would probably not have changed.
The infection
The patient was otherwise healthy and immunocompetent.
Retropharyngeal abscesses in adults are rare. Tennebaum reported 51 cases in 1996 in his review. Forty one percent of these cases involved patients with a recent history of pharyngeal tear by a preceding procedure or impacted foreign body [32]. Harkani reported 5 case reports in a review in 2011 which occurred mostly due to local trauma due to foreign body ingestion or in immunocompromised patients [33].
Parapharyngeal abscesses in adults are even more uncommon. Sethi found only 9 patients in his review [34]. All the patients in this study presented with fever and swelling of the upper neck and all needed exploration, incision and drainage. Infection in the parapharyngeal space can spread to the retropharyngeal space and the mediastinum [35], requiring urgent diagnosis and treatment. Immunocompromised patients and diabetics are also more prone for this kind of infections [36]. However, our patient had an abscess in the visceral space. How could this deep abscess originate from the insertion of a LMA? As discussed earlier, the otolaryngologist found a small wound in the lateral wall on the right side. The spread to the visceral space can be explained by the anatomical boundaries of the visceral space. The visceral space has a controversial terminology with the main difference being the superior limit. Some authors consider the entire pharyngeal mucosal space, including nasopharynx and oropharynx, as a subcomponent of the visceral space [19,20,21] extending the superior border to the skull base, while others restrict the visceral space to the infra-hyoid neck, with the superior border at the level of the hyoid bone [37]. Our case report would support the first hypothesis. The pharyngeal mucosal space must be part of the visceral space, otherwise this type of abscess could not have occurred. Apart from this discussion, there is consensus that the visceral space extends to the superior mediastinum: this consensus is supported by our case report, as the superior mediastinum represented the inferior border of the abscess.
The strength of this case presentation is the combination of the chronology of events, the diagnosis on CECT of the visceral abscess and the positive microbiology. Limitations are the paucity of data to be found in the literature about the anatomical extension of the visceral space.
The diagnosis
In our case the patient had a sore throat postoperatively. However, this is not uncommon after airway manipulation. A sore throat occurs in 12% after airway manipulation with 45% due to endotracheal intubation and only 18% attributed to LMA [38]. The cuff pressure has also an effect on the degree of pain [39]. Therefore, measurement of cuff pressure should be the standard of care in LMA use.
The evidence of some blood on the LMA at the time of removal could have alerted medical staff to the possibility of trauma caused by the LMA. Evidence exists that patients with a postoperative sore throat and bloodstained sputum should undergo more thorough clinical investigations [11]. In this patient, because only a small amount of bloodstained sputum was observed, no further investigation was initiated.
The patient presented to her general practitioner the following day with fever, dysphagia and throat pain. A common diagnosis of laryngitis was made and she was treated accordingly. After three days, the fever and pain persisted and the skin was swollen, red and warm from the sternum bilaterally to both ears. The patient was admitted to the emergency room where an abscess in the visceral space was confirmed after CECT scan before she was transferred to the ICU.
The CECT scan of the neck and upper chest was performed 5 days after insertion of the LMA. The initial CECT scan shows a large collection of fluid and air bubbles (which proved to be an abscess) in a rather unusual location, called the visceral space. The collection pushes the right thyroid lobe and the right internal jugular vein posteriorly. The collection is therefore draped over the thyroid gland and contained by the overlying sternocleidomastoid muscle (Fig. 1, red arrow). Part of the abscess is located adjacent to the trachea on the right side, deep from the right thyroid gland lobe (Fig. 1, green arrow).
There is inferior extension of the abscess into the border of the upper mediastinum, posterior from the manubrium of the sternum. The platysma is slightly thickened at the right side. Several bilateral jugulodigastric lymph nodes are reactively enlarged. Although some inflammation around the right external jugular vein is noted, this does not result in a frank thrombophlebitis. Tracheal deviation to the left can be seen on the coronal reconstructions due to mass effect of the abscess (Fig. 2).
CECT, coronal image. Inferior extension of the deep neck abscess (largest part on the right side) into the border of the upper mediastinum with mass effect, leading to a leftward deviation of the trachea (a). Bilateral reactively enlarged jugulodigastric lymph nodes (b) without signs of intranodal abscess
Control CECT scan (not shown), obtained five days after the initial CECT scan, showed a decrease in diameters of the deep neck abscess.
The treatment
In the day care centre only analgesics were prescribed. The general practitioner added amoxicillin 24 h later following national guidelines for the treatment of laryngitis. Unfortunately, the Prevotella spp. which caused the infection was resistant to amoxicillin. This made it possible for the infection to spread further causing pain, dysphagia and respiratory problems. Fortunately, the patient recovered well on therapy with amoxicillin/clavulanate and vancomycin. Respiratory distress improved over the following 24 h and the swelling diminished. Subsequently, the abscess was incised 5 days later under general anaesthesia. The treatment given, of antibiotics and surgical treatment for deep neck abscess was in accordance with international guidelines [40].
Prevotella is a genus of Gram-negative bacteria. They are non-motile, singular cells that thrive in anaerobic growth conditions. They thrive on tissues with decreased oxidation-reduction potentials, such as those with limited blood supply or tissue necrosis. Prevotella spp. are found in the oral cavity, the gastrointestinal tract and the vagina. They can act as an opportunistic pathogen, often penetrating tissues and establishing an infection at mucosal surfaces causing periodontal and tooth problems such as gingivitis and periodontitis. They predominate in periodontal disease and periodontal abscesses. Some Prevotella spp. are resistant to Beta-lactam antibiotics [41]. Effective antibiotic treatments are metronidazole, amoxicillin/clavulanate, ureidopenicilins, carbapenems, cephalosporins, clindamycin and chloramphenicol. This patient had extensive spread of the infection due to a late diagnosis of an abscess in the visceral space with a penicillin resistant Prevotella treated with amoxicillin.
Patient perspective on the received treatment
“I recovered from anesthesia of the first operation and was very pleased with the results of the operation. However, I had a sore throat when leaving the day care centre. One day later I was in so much pain that I had to call the general practitioner. I was thankful for the painkillers and I was well informed why antibiotics were prescribed. 24 hours later the pain and swelling was getting worse and I started to panic because I thought I would die. The treatment with oxygen and antibiotics started on intensive care and I was overwhelmed by all the actions the caregivers had to do to stabilise my situation. I am so glad I didn’t have to get a tracheotomy. Luckily, I have fully recovered and I am very thankful for the good treatment I have been given.”
Conclusion
Laryngeal mask airways are easy to use and are established safe tools to support the airway. This is the first case report with a penicillin and metronidazole resistant Prevotella denticola as the documented bacterial cause of a deep neck abscess after LMA and the first case report of such an abscess in the visceral space.
In this case a small wound in the lateral pharyngeal wall potentially created an access from the pharyngeal cavity into the otherwise sterile visceral space causing infection with Prevotella denticola. The infection spread rapidly because of resistance to penicillin and metronidazole and caused respiratory problems necessitating admittance to ICU for respiratory failure. Early recognition and treatment of LMA induced abscess is necessary to prevent evolution to airway obstruction. If the patient complains of a sore throat and bloodstained sputum after evidence of blood on removal of the LMA, antibiotics should be considered and close monitoring of the patient’s ongoing condition should be mandatory.
Furthermore, we advise the routine use of a manometer when using LMA’s to obtain a cuff pressure of less then 44 mmHg to prevent soft tissue necrosis.
A randomised controlled trial to compare the incidence of infection and sore throat after findings of blood stains after LMA removal could be beneficial. Also because the LMA is usually inserted blindly, its exact position cannot be assured. Therefore, to place the device into the correct position, we need to understand the possible types of misplacement and have indirect detection methods of misplacement, and to master techniques to place the device correctly.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LMA:
-
Laryngeal mask airway
- ICU:
-
Intensive Care Unit
- ETT:
-
Endotracheal tube
- Ml:
-
Milliliter
- Mg:
-
Milligrams
- MmHg:
-
Milliliters of mercury
- Cm H2O:
-
Centimeters of water
- CECT:
-
Contrast-enhanced computed tomography scan
References
Brain AL. The laryngeal mask-a new concept in airway management. Br J Anaesth. 1983;55(8):801–5. https://doi.org/10.1093/bja/55.8.801.
Brimamcombe J. The advantages of the LMA over the tracheal tube or facemask: a meta-analysis. Can J Anaesth. 1955;42:1017–23.
Springer D, Jahr JS. The laryngeal mask airway. Safety, efficacy and current use. Am J Anesthesiol. 1995;22(2):65–9.
Verghese C, Smith TGC, Young E. Prospective survey of the use of the laryngeal mask airway in 2359 patients. Anaesthesia. 1933;48:58–60.
Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the fourth National Audit Project of the Royal College of Anaesthetists and the difficult airway society. Part 1: anaesthesia, Fourth National Audit Project. Br J Anaesth. 2011;106(5):617–31.
Simon LV, Torp KD. Laryngeal Mask Airway. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. PMID: 29489214.
Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review. J Oral Maxillofac Surg. 2010;68(10):2359–76. https://doi.org/10.1016/j.joms.2010.04.017.
Van Esch B, Stegeman I, Smit A. Comparison of laryngeal mask airway vs tracheal intubation: a systematic review on airway complications. J Clin Anesth. 2017;36:142–50. https://doi.org/10.1016/j.jclinane.2016.10.004.
Chang JE, Kim H, Lee J-M, Min SW, Won D, Jun K, et al. A prospective, randomized comparison of the LMA-protector™ and i-gel™ in paralyzed, anesthetized patients. BMC Anesthesiol. 2019;19(1):118. https://doi.org/10.1186/s12871-019-0785-8.
L’Hermite J, Dubout E, Bouvet S, Bracoud LH, Cuvillon P, Coussaye JEL, et al. Sore throat following three adult supraglottic airway devices: a randomised controlled trial. Eur J Anaesthesiol. 2017;34(7):417–24. https://doi.org/10.1097/EJA.0000000000000539.
Lynn E, et al. Retropharyngeal abscess – a complication of laryngeal mask airway. J Surg Case Rep. 2012;10:7.
Casey SED, Donolly M, McCaul CL. Severe retropharyngeal abscess after the use of a reinforced laryngeal mask with a basworth introducer. Anetshesiology. 2009;110(4):943–5.
Furst I, Ellis D, Winton T. Unusual complication of endotracheal intubation: retropharyngeal space abscess, mediastinitis and empyema. J Otolaryngol. 2000;29(5):309–11. 11108491.
Stein S, Daud AS. Retropharyngeal abscess: an unusual complication of tracheal intubation. Eur J Anaesthesiol. 1999;16(2):133–6. https://doi.org/10.1046/j.1365-2346.1999.00438.x.
Paciui M. Deep neck abscess and mediastinitis after laryngeal mask anesthesia. Anesth Analg. 2009;108(4):1356–7. https://doi.org/10.1213/ane.0b013e31819543d8.
Yegappan C, Redmond E, LeDEz K. Anterior mediastinitis following traumatic laryngeal mask placement. Can J Anaesth. 2007;54(S1):44568. https://doi.org/10.1007/BF03019996.
Van der Woerd B, Robichaud J, Gupta M. Parapharyngeal abscess following use of a laryngeal mask airway during open revision septorinoplasty. Int J Surg Case Rep. 2015;16:198–201. https://doi.org/10.1016/j.ijscr.2015.10.003.
Balasubramanian A, Shah JR, Gazali N, Rajan P. Life-threatening parapharyngeal and retropharyngeal abscess in an infant. BMJ Case Rep. 2017:bcr-2017-221269. https://doi.org/10.1136/bcr-2017-221269.
Guidera AK, Dawes PJ, Fong A, Stringer MD. Head and neck fascia and compartments: no space for spaces. Head Neck. 2014;36(7):1058–68. https://doi.org/10.1002/hed.23442-pubmed.
Som PM, Curtin HD. Head and Neck Imaging – 2 Volume Set. 5th edition (2011) hardcover ISBN: 9780323053556, eBook ISBN: 9780323248938.
Mukherji SK, Castillo M. A simplified approach to the spaces of the suprahyoid neck. Radiol Clin North Am. 1998;36(5):761–80.
Noma U, et al. Progressive Dysphagia post Laryngeal Mask Airway Intubation. J Surg Technique Case Rep. 2009;1(1):23–4 eISSN: 2006–8808.
Weber S. Traumatic complications of airway management. Anesthesiol Clin North Am. 2002;20(3):503–12. https://doi.org/10.1016/S0889-8537(02)00014-7.
Lee JJ. Laryngeal mask and trauma to uvula. Anaesthesia. 1989;44(12):1014–5. https://doi.org/10.1111/j.1365-2044.1989.tb09242.x.
Mj P, et al. Tearing of the lingual frenulum caused by insertion of the proSeal LMA IN A CHILS. Korean J Anaesthesiol. 2009;57(5):644–6.
Van Dongen VC, Langemeijer JJ. An unusual complication of the laryngeal mask airway? Anaesthesia. 1994;49(12):1097–8. https://doi.org/10.1111/j.1365-2044.1994.tb04370.x PMID: 7864335.
Michalek P, Donaldson W, Vobrubova E, Hakl M. Complications Associated with the Use of Supraglottic Airway Devices in Perioperative Medicine. BioMed Res Int. 2015;746560:13.
Bick E, Balies I, Patel A, Brain AIJ. Fewer sore throats and a better seal: why routine manometry for laryngeal mask airways must become the standard of care. Anaesthesia. 2014;69(12):1304–8. https://doi.org/10.1111/anae.12902.
Jonathan L. Benumof; laryngeal mask airway: indications and contraindications. Anesthesiology. 1992;77(5):843–6.
Seet E, Youssaf F, Gupta S, et al. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: a prospective randomized trial. Anesthesiology. 2010;112(3):652–7. https://doi.org/10.1097/ALN.0b013e3181cf4346.
Grady DM, McHardy F, Wong J, Lin F, Tong D, Chung F. Pharyngolaryngeal morbidity with the laryngeal mask airway in spontaneously breathing patients: does size matter? Anesthesiology. 2001;94(5):760–6. https://doi.org/10.1097/00000542-200105000-00012.
Tannebaum RD. Adult retropharyngeal abscess: a case report and review of the literature. J Emerg Med. 1996;14(2):147–58. 8740744. https://doi.org/10.1016/0736-4679(95)02113-2.
Harkani A, Hassani R, Ziad T, Aderdour L, Nouri H, Rochdi Y, et al. Retropharyngeal abscess in adults: five case reports and review of the literature. Sci World J. 2011;11:1623–9. https://doi.org/10.1100/2011/915163.
Sethi DS, Stanley RE. Parapharyngeal abscesses. J.Laryngol.Otol. 1991;105(12):1025–30.
Salam A, Khan I, Sonawalla A, Fatimi S. Rare mycotic aneurysm of internal jugular vein and innominate vein secondary to untreated parapharyngeal abscess: a case report. Ann Med Surg. 2017;19:62–4. https://doi.org/10.1016/j.amsu.2017.05.011.
Mahfoudhi M, Khaled K. Abcès para-pharyngé survenant chez un diabétique [Parapharyngeal abscess occurring in a diabetic]. Pan Afr Med J. 2015;20:114. https://doi.org/10.11604/pamj.2015.20.114.6130 PMID: 26090062; PMCID: PMC4458320.
Koch BL, Hamilton BE, Hudgins PA, Harnsberger HR. Diagnostic Imaging: Head and Neck E-Book 3th edition. Elsevier: Hardcover; 2016. ISBN: 9780323443012, eBook ISBN: 9780323443142
Higgins PP, et al. Postoperative sore throat after ambulatory surgery. Br J Anaesthesia. 2002;88(4):5825–584.
Joe HB, Kim DH, Chae YJ, Kim JY, Kang M, Park KS. The effect of cuff pressure on postoperative sore throat after cobra perilaryngeal airway. J Anesth. 2012;26(2):225–9. https://doi.org/10.1007/s00540-011-1293-2.
Herzon FS, Martin AD. Medical and surgical treatment of peritonsillar, retropharyngeal and parapharyngeal abscesses. Curr Infect Dis Rep. 2006;8(3):196–202. https://doi.org/10.1007/s11908-006-0059-8.
Finegold SM. Anaerobic gram-negative bacilli. In: Baron S, editor. Medical Microbiology. 4th ed. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 20. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8438/.
Acknowledgements
None.
Funding
The authors declare that there is no funding.
Author information
Authors and Affiliations
Contributions
V.H. wrote the case report, V.O. was a major contributor in rewriting the manuscript, N.E. was also a contributor in rewriting the manuscript, T.M. was a major contributor for the radiologic and anatomic explanation of this case report. All authors read and approved the final manuscript. N.E. reviewed the manuscript for English grammatical corrections and advice.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and consent to participate are not applicable.
Consent for publication
The patient gave a written consent for publication..
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vanden Eede, H., Norris, E., Torfs, M. et al. Life threatening abscess in the visceral space with penicillin and metronidazole resistant Prevotella Denticola following use of a laryngeal mask airway: case report. BMC Anesthesiol 21, 102 (2021). https://doi.org/10.1186/s12871-021-01322-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-021-01322-9