Abstract
Salmonellosis, a zoonotic disease, is one of the leading causes of foodborne illness worldwide. It is responsible for most infections caused by consumption of contaminated food. In recent years, a significant increase in the resistance of these bacteria to common antibiotics has been observed, posing a serious threat to global public health. The aim of this study was to investigate the prevalence of virulent antibiotic-resistant Salmonella spp. strains in Iranian poultry markets. A total of 440 chicken meat samples were randomly selected from meat supply and distribution facilities in Shahrekord and tested for bacteriological contamination. After culturing and isolating the strains, identification was performed using the classical bacteriological method and PCR. To determine antibiotic resistance, a disc diffusion test was performed according to the recommendations of the French Society of Microbiology. PCR was used to detect resistance and virulence genes. Only 9% of the samples were positive for Salmonella. These were Salmonella typhimurium isolates. All Salmonella typhimurium serotypes tested positive for the rfbJ, fljB, invA and fliC genes. Resistance to TET, cotrimoxazole, NA, NIT, piperacillin/tazobactam and other antibiotics was found in 26 (72.2%), 24 (66.7%), 22 (61.1%) and 21 (58.3%) isolates, respectively. The sul1, sul2 and sul3 genes were present in 20, 12 and 4 of 24 cotrimoxazole-resistant bacteria, respectively. Chloramphenicol resistance was found in six isolates, but more isolates tested positive for the floR and cat two genes. In contrast, 2 (33%) of the cat three genes, 3 (50%) of the cmlA genes and 2 (34%) of the cmlB genes were all positive. The results of this investigation showed that Salmonella typhimurium is the most common serotype of the bacterium. This means that most of the antibiotics commonly used in the livestock and poultry industries are ineffective against most Salmonella isolates, which is important for public health.
Similar content being viewed by others
Introduction
An important foodborne pathogen known as non-typhoidal Salmonella has been linked to the intestinal system of animals that produce food [1]. Salmonella is a common foodborne disease associated with the intestinal system of food-producing animals. It is a gram-negative, facultatively anaerobic, flagellated bacteria [2]. Non-typhoidal Salmonella causes approximately 153 million cases of gastroenteritis and 57,000 deaths annually worldwide. Typhimurium is one of the most common Salmonella serovars [3]. Humans and animals are often colonized by Salmonella microorganisms, which can proliferate in the intestinal tract and result in a range of gastrointestinal disorders. In some cases, these infections can lead to severe illness or even mortality [4]. Enteritidis, one of the most important Salmonella serovars, is a major cause of human illness with symptoms commonly including fever, vomiting, diarrhoea, and abdominal cramps 12–72 h after ingestion of the bacterium [5].
The most prevalent Salmonella serotypes causing human gastroenteritis worldwide are Salmonella Typhimurium and Salmonella Enteritidis [6]. The virulence of Salmonella depends on many factors. It is determined by its ability to adhere to cells, to invade them, to survive and to multiply inside epithelial cells and macrophages thanks to the involvement of several virulence factors often carried by plasmids [7]. A significant proportion of these virulence genes are clustered together in specific genomic regions known as “Islands of pathogenicity of Salmonella” (SPIs), acquired by horizontal transfer. In general, different virulence factors that are important for a variety of pathogenic mechanisms, including adhesion, invasion, intracellular survival, systemic infection, toxin generation, and iron acquisition, determine how pathogenic Salmonella is [8]. An essential feature of the pathogenesis of Salmonella is its ability to enter host cells and remain there as an optional intracellular parasite. Another possible risk to human health is the existence of virulence genes that are frequently carried by plasmids, prophages, and Salmonella pathogenicity islands (SPIs), which can be transmitted between these bacteria. Several severe Salmonella infections associated with these virulent components have been reported [8, 9].
A common source is poultry, and in recent years, much attention has been paid to understanding out how widespread Salmonella is at various points in the poultry production chain [10]. In addition, contamination of meat can occur during loading, unloading, and storage. To ensure both meat quality and consumer protection, strict good hygiene and moral slaughter methods must be combined coupled with risk-based preventive actions [11]. The prevalence of drug-resistant strains, which pose serious risks to the public’s health, is another epidemiological issue [12]. Antibiotic resistance has increased, and genes conferring antimicrobial resistance to Salmonella are now present because of the selective pressure exerted using antibiotics in poultry production and veterinary medicine for growth promotion and prevention [13,14,15].
In Iran, numerous studies have been conducted on the incidence of Salmonella resistance in humans [16, 17], the factors associated with this infection [18], salmonellosis in eggs [19] and in cattle [20], but no study has considered the virulence and resistance of Salmonella enteritidis and Salmonella typhimurium strains in Iran. Therefore, this study was carried out to investigate the frequency of virulent strains of Salmonella enteritidis and Salmonella typhimurium that are resistant to antibiotics in the chicken meat markets of Iran. This study was conducted to determine the frequency of Salmonella in poultry meat shops in Iran. The antibiotic resistance patterns of the Salmonella isolates and the location of their virulence genes were also identified.
Methods
Study framework and sampling
This study was conducted in the city of Shahrekord. The sampling area was selected based on the availability of meat, and shops were randomly selected, along with poultry meat taken tissue samples from each store. The meat sampled was factory farmed. A total of 80 chicken, 80 quail, 80 from grocery stores in Quebec, 80 turkeys, 60 duck and 60 goose were randomly sampled from stores. All samples were collected aseptically, placed in sterile bags and delivered to the Food Microbiology Laboratory of Islamic Azad University of Shahrekord.
Microbiological analysis
The samples were examined according to the procedure described by Mir-Hassan Moosavy et al. in 2015. Using a sterile scalpel, each tissue sample was cut into pieces weighing approximately 25 g. The pieces were then placed in a sterile mortar and pestle where they were homogenised with 225 ml of buffered peptone water (BPW) before being placed in a 250 ml tube and incubated at 37 °C for 24 to 48 h. The swab samples were then grown on Salmonella-Shigella solid agar medium (containing proteins, lactose and iron) and incubated at 37 °C for 24 h. The suspected Salmonella colonies were then examined. In the case of a negative result (Salmonella that has lost all colour by this time), the incubation process was extended for a further 24 h. Colonies that were light in colour or had a grey or black centre were considered negative. Questionable colonies on the Salmonella-Shigella agar medium were removed and complementary assays and differentiating microbiological tests were performed, such as urease and IMViC [methyl red (MR) and Voges-Proskauer (VP) broth] [21].
Detection of virulence genes and Salmonella’s detection
Salmonella isolates were grown on Luria Bertani (LB) agar plates and incubated at 37 °C for 24 h prior to DNA extraction. Following to the procedure of Mir-Hassan Moosavy et al. 2015, one loop of each LB agar sample was suspended in 250 µl of sterile distilled water for DNA extraction. Samples were vortexed, boiled for 10 min, and then centrifuged at 6000 x g for 7 min to achieve uniform turbidity. DNA-containing supernatants were collected and stored for multiplex PCR analysis. For DNA amplification of two serovars, Typhimurium and Enteritidis, multiplex PCR was performed out [16] with two independent sets as previously described. In the case of Salmonella typhimurium (Table 1) [20], four sets of primer pairs specific for rfbJ (663 bp), fljB (526 bp), invA (284 bp) and fliC (183 bp), and three sets of primer pairs designed for a random sequence specific to the Salmonella enteritidis genus Salmonella (429 bp), sefA (310 bp) and spv (250 bp) [22]. Agar gel electrophoresis was used to verify the amplification results. For Salmonella typhimurium and Salmonella enteritidis, the amplification products were electrophoresed on 1.2% and 1.8% agarose gels, respectively. A 100 bp ladder was used as a molecular weight marker in both methods. When UV was used in the gel documentation system, the gels were stained with ethidium bromide (2 g/mL) to visualise fluorescent bands (BIORAD). For each PCR reaction, positive controls were performed using the reference strains.
Antimicrobial susceptibility testing (AST)
The disc diffusion method was used to perform the AST [24, 25]. Incubation was performed at 37 °C for 16–18 h. After incubation, the zones of inhibition by each antibiotic were measured. The reference strain Salmonella Typhimurium ATCC 14,028 was used as an internal quality control for AST. The data were interpreted according to the recommendations of the Clinical and Laboratory Standards Institute (CLSI) (CLSI 2018) [24]. Ampicillin (AMP, 20 lg), cefotaxime (CTX, 300 lg), chloramphenicol (C, 30 lg), tetracycline (TET, 30 lg), ciprofloxacin (CIP, 5 lg), gentamicin (GEN, 10 lg), nalidixic acid (NA, 30 lg), cotrimazole (COT, 25 lg), tetracycline (TET, 30 lg), ciprofloxacin (CIP, 5 lg), gentamicin (GEN, 10 lg), nalidixic acid (NA, 30 lg), cotrimazole (COT, 25 lg), tetracycline (TET), nitrofurantion (NIT, 30 lg), imepenem (IPM, 10 lg), meropanem (MRP, 10 lg), piperacillin/tazobactin (PIT, 100/10).
Antimicrobial resistance gene detection
Target genes conferring resistance to tetracyclines (tetA, tetB), sulfonamides (sul1, sul2, and sul3), chloramphenicol (cat1, cat2, and cat3, cmlA, cmlB, floR), and aminoglycosides (aph(3)11a, aac(3)11a, and aac6) were screened by PCR using the corresponding primers in order to The cycle parameters and primer combinations followed the guidelines of Ma et al. (2017) (Table 2) [27]. PCR was performed using 2.0 l of template DNA and 30 l containers containing 3 l of buffer (100 mmol/L Tris-HCl [pH 9], 1.5 mmol/L MgCl2, 500 mmol/L KCl, 0.1% gelatin), 100 lmol/L concentrations of dATP, dTTP, dGTP, and dCTP, 10 pmol of each primer, and 0.9 A thermal cycler (MJ Research, Bio-Rad, Hercules, CA) was used to perform the reactions. Table 3 summarises the cycling conditions and primer sequences [27].
Statistical analysis
For analysis, the data were transferred to a Microsoft Excel spreadsheet (Microsoft Corp., Redmond, Washington). Statistical tests were performed using SPSS (Statistical Package for the Social Sciences) 18.0 (SPSS Inc., Chicago, IL, USA). P values below 0.05 were considered significant.
Results
Salmonella prevalence
Salmonella-Shigella solid agar medium was used and differential microbiological tests were conducted, such as urease and IMViC [methyl red broth (MR) and Voges-Proskauer (VP) to isolate and identify Salmonella. Out of the 400 samples analyzed, 36 were found to be positive for the culture of Salmonella, indicating a contamination rate of 9% (36/400). The prevalence of Salmonella in Quebec meat samples (11.25%, 9/80) was significantly higher than in other poultry (Table 3).
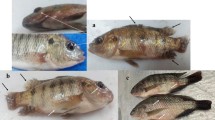
Salmonella serovars’s detection
The detection of Salmonella serovars was carried out through multiplex PCR using four sets of primer pairs specific for rfbJ, fljB, invA, and fliC in the case of Salmonella typhimurium (Table 1) [23] and three sets of primer pairs designed for a 429 bp fragment specific to the genus Salmonella enteritidis, sefA, and spv. After PCR amplification, all isolates were identified as positive for the invA gene. Salmonella typhimurium was found to be present in all isolates. The RfbJ, fljB, invA and fliC genes were observed in all typhimurium serotypes (Table 4).
Antibiotic sensitivity
The antibiotic sensitivity of each strain was determined by the disk diffusion method. The measured zones of inhibition were interpreted according to the Clinical and Laboratory Standards Institute recommendations. Of the isolates tested, 26 (72.2%), 24 (66.7%), 22 (61.1%), 21 (58.3%), and 21 (58.3%) isolates were resistant to TET, cotrimoxazole, NA, NIT, and piperacillin/tazobactin, respectively. Moreover, resistance to CTX, AMP, GEN, and chloramphenicol was detected in 10–20% of the isolates. A majority (50.5%) of the isolates were at least partially antibiotic resistant (Table 5).
Detection of resistance genes
To detect the resistance genes to the antibiotics used, a screening of target genes was conducted using PCR. Target genes conferring resistance to tetracyclines (tetA, tetB), sulfonamides (sul1, sul2 and sul3), chloramphenicol (cat1, cat2 and cat3, cmlA, cmlB, floR) and aminoglycosides (aph(3)11a, aac( 3)11a and aac6) were used. After amplification, the tetA gene was present in all 36 TET-resistant isolates, and the tetB, tetC, and tetG genes were present in 23% (6), 27% (7), and 39% (10) of the isolates, respectively. Additionally, 20 (84%), 12 (50%), and 4 (17%) of the 24 cotrimoxazole-resistant bacteria were detected to possess the sul1, sul2, and sul3 genes, respectively (Table 6). Six isolates were resistant to chloramphenicol, although more isolates were positive for the floR and cat two genes, while only two isolates (33%) were positive for the cat three genes, three (50%) were positive for the cmlA gene, and two isolates (34%) were positive for the cmlB gene.
Discussion
Salmonella Typhimurium and Salmonella Enteritidis are common causes of foodborne illness and death. With increasing antibiotic resistance, these pathogens have become more prevalent over the years, posing a serious public health problem. The objective of this study was to investigate the frequency of antibiotic-resistant virulent strains of Salmonella Enteritidis and Salmonella Typhimurium in chicken meat markets in Iran.
In this study, 400 samples were used, among which 36 (9%) samples tested positive for Salmonella. This level of contamination is similar to what has been observed in previous investigations in Iran and other countries on various types of meat. A range of Salmonella prevalence has been reported in Iran previously. In this study, compared to the figures reported in other Asian countries such as India (14.8%) [28] and Vietnam (48.9%) [29], China (52.2% [30], Malaysia (48%) [31], Pakistan (38%) [32], and Singapore (18.1%) [33], the prevalence of Salmonella in chicken meat was less than 9%. After detecting serovars, we found 36 (9%) positive samples for S. Typhimurium. In a similar study, 36 (9%) positive samples for S. Typhimurium were reported [34]. In a related survey, Salmonella Enteritidis, Salmonella Typhimurium, and Salmonella Thompson were the three Salmonella serotypes identified by Kumar et al., 2019 [28].
The AST conducted in this study showed that 72.2%, 66.7%, and 61.2% of the identified Salmonella isolates had significant levels of resistance to tetracycline (TET), COT, and NA, respectively. A comparative study conducted in Ibadan, Nigeria, reported a high frequency of isolates resistant to TET (93%), NA (81%), and sulfamethoxazole (87%). However, human isolates showed resistance to trimethoprim, sulfamethoxazole, AMP, and chloramphenicol ranging from 36 to 59%. The diversity of high levels of drug resistance in different locations could be explained by the numerous discoveries on Salmonella antibiotic resistance in various countries. According to Zhao et al. (2017), Salmonella obtained from chickens had considerable resistance to tetracycline (93.1%), but resistance to ampicillin was only 47% [35]. Clinical isolates from the northern region of Nigeria were reported to have 100% resistance to fluoroquinolones in another survey. Kumar (2019) identified high resistance to tetracycline (100%), erythromycin (100%), nalidixic acid (98.57%), ampicillin (95.71%), and ciprofloxacin (82.86%) [28]. Particularly in developing countries, resistance to ciprofloxacin and higher-generation cephalosporins is a serious problem, and chicken-based products may be directly responsible for its establishment [29, 30].
Studies in several parts of Iran show the introduction and growth of antibiotic resistance in Salmonella isolates. Tetracycline (66.6%), furazolidone (52.8%), nalidixic acid (43.8%), lincomycin-spectinomycin (42.3%), flumequine (40.6%), and streptomycin (39.1%) had the highest rates of resistance, according to Peighambari et al. (2011), while ciprofloxacin and imipenem had a sensitivity of 100% [38]. The highest rates of drug resistance were reported during the use of nitrofurantoin (92.6%), nalidixic acid (86.7%), cloxacillin (64%), tetracycline (54%), furazolidone (49.3%), and amoxicillin (45.3%), according to Ezzatpanah et al. (2013) [39]. All isolates were found to be resistant to tetracycline, streptomycin, nalidixic acid, cefazolin, and sulfamethoxazole + trimethoprim by Asadpour et al. (2013) [40]. Drugs with the highest rates of resistance were streptomycin and nalidixic acid (100%), tetracycline (92.3%), neomycin and furazolidone (84.6%), and chloramphenicol (73.3%), according to Raeisi and Ghiyami (2015). Furthermore, amoxicillin and ampicillin (11.5%), ciprofloxacin (7.7%), and gentamicin (3.7%) had the lowest rates of resistance [41]. Tetracycline was first introduced as the most effective antibiotic against Salmonella in poultry by Sodagari et al. (2015) in the Alborz province [42]. The need to improve coordination between the veterinary and public health sectors on appropriate diagnosis and notification of foodborne zoonotic pathogens is reinforced by the high level of resistance to NA 22 (61.2%) that was observed in this study, especially in food animals [43]. The result of this study is also highly significant as the effective management of severe or invasive human salmonellosis depends on the use of antibiotics.
In this study, TET-resistant genes were most frequently found in isolates with tetA gene, followed by tetB, tetC, and tetG genes in 23%, 27%, and 39% of TET-resistant isolates, respectively. The cat 1 gene was found in all six resistance genes in the current analysis. Various antibiotic resistance genes are present in Salmonella on mobile genetic components, facilitating rapid spread of resistance characteristics to other serotypes or even bacteria of different genera. In line with this, Ahmed and Shimamoto (2012) showed that only tetA gene was found in S. Typhimurium [44] out of the six examined genes (tetA, tetB, tetC, tetD, tetE, and tetG). Additionally, studies by Adesiji et al. (2014) showed that tetA was the most prevalent (100%) [45]. TetA is predominantly present in non-typhoidal Salmonella, highlighting the contribution of the gene to tetracycline resistance. Sul1 and sul2 genes code for sulfonamide resistance. Sul1 gene was found in 82.35% of isolates while sul2 gene was only found in 8.82% of isolates. The predominance of sul1 gene in S. Typhimurium was described by Randall et al. (2004) [46]. Ahmed et al. (2016) also discovered sul1 gene in Salmonella species resistant to 96.7% of sulfonamides.
Different prevalences of resistance genes were noted; the most prevalent gene among poultry strains was floR. The results of this analysis show that S. typhimurium is the most common serotype. Most antimicrobial drugs under investigation are not effective against poultry Salmonella isolates, posing a public health problem. This problem can be exacerbated by the continued use of drugs in chicken farming. Therefore, prudent use of antibiotics appears necessary to prevent the formation of resistant Salmonella strains.
The results of this study provide current data on the frequency of S. typhimurium in poultry meat sold in retail establishments in the Iranian city of Shahrekord. These Salmonella typhimurium isolates recovered from poultry meat exhibited serovar-specific pathogenicity genes as well as various important resistance genes. It is crucial to keep in mind that control is necessary at every stage of the food chain.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Hunter JC, Watkins LKF. Salmonellosis (nontyphoidal) In Centers for Disease Control and Prevention, ed. CDC Health Information for International Travel, Chap. 3: Infectious Diseases Related to Travel. https://wwwnc.cdc.gov/travel/yellowbook/2018/infectious-diseases-related-to-travel/salmonellosis-nontyphoidal. Accessed March21, 2018.
Hadjinicolaou AV, Demetriou VL, Emmanuel MA, Kakoyiannis CK, Kostrikis LG. Molecular beacon-based real-time PCR detection of primary isolates of Salmonella Typhimurium and Salmonella Enteritidis in environmental and clinical samples. BMC Microbiol. 2009;9:97. https://doi.org/10.1186/1471-2180-9-97. Published 2009 May 19.
Mezal EH, Sabol A, Khan MA, Ali N, Stefanova R, Khan AA. Isolation and molecular characterization of Salmonella enterica serovar enteritidis from poultry house and clinical samples during 2010. Food Microbiol. 2014;38:67–74. https://doi.org/10.1016/j.fm.2013.08.003.
Frederick A, Ayum TG, Gifty AA, Samuel A. Microbial quality of chevon and mutton sold in Tamale Metropolis of Northern Ghana. J Appl Sci Environ Manage. 2010;14(4):53–5.
Mezal EH, Stefanova R, Khan AA. Isolation and molecular characterization of Salmonella enterica serovar Javiana from food, environmental and clinical samples. Int J Food Microbiol. 2013;164(1):113–8. https://doi.org/10.1016/j.ijfoodmicro.2013.03.021.
Edris A, Hassan M, Shaltout F, El-Hosseny S. Detection of E.Coli and Salmonella organisms in cattle and camel meat. BVMJ. 2013;25:2:198–204.
Kaur J, Jain SK, Malik RK. Salmonella pathogenesis: where do we stand and what do we aim to achieve? Reviews in Medical Microbiology. 2021;32(2):71–84.
Tamang MD, Gurung M, Nam HM, Moon DC, Jang GC, Jung SC. Antimicrobial susceptibility and virulence characteristics of Salmonella enterica typhimurium isolates from healthy and diseased pigs in Korea. JFP. 2014;77(9):1481–6.
Litrup E, Torpdahl M, Malorny B, Huehn S, Christensen H, Nielsen EM. Association between phylogeny, virulence potential and serovars of Salmonella enterica. Infect Genet Evol. 2010;10(7):1132–9.
Luu QH, Fries R, Padungtod P, Tran TH, Kyule MN, Baumann MP, Zessin KH. Prevalence of Salmonella in retail chicken meat in Hanoi, Vietnam. Ann N Y Acad Sci. 2006;1081:257–61.
FestusJaja I, LondiweBhembe N, Green E, Oguttu J, Muchenje V. Molecular characterisation of antibiotic-resistant Salmonella enterica isolates recovered from meat in South Africa.2019. Acta Trop 190: 129–36.
Ćwiek K, Korzekwa K, Tabiś A, Bania J, Bugla-Płoskońska G, Wieliczko A. Antimicrobial Resistance and Biofilm formation capacity of Salmonella enterica Serovar Enteritidis strains isolated from Poultry and humans in Poland.2020. Pathogens. 2020;9(8):643.
Zishiri OT, Mkhize N, Mukaratirwa S. Prevalence of virulence and antimicrobial resistance genes in Salmonella spp isolated from commercial chickens and human clinical isolates from South Africa and Brazil. Onderstepoort J Vet Res. 2016;83:a1067.
Alduhaidhawi AHM, AlHuchaimi SN, Al-Mayah TA, Al-Ouqaili MTS, Alkafaas SS, Muthupandian S, Saki M. Prevalence of CRISPR-Cas Systems and their possible Association with Antibiotic Resistance in Enterococcus faecalis and Enterococcus faecium collected from Hospital Wastewater. Infect Drug Resist 2022 Mar 19;15:1143–54. doi: https://doi.org/10.2147/IDR.S358248. PMID: 35340673; PMCID: PMC8942119.
Chinemerem Nwobodo D, Ugwu MC, Oliseloke Anie C, Al-Ouqaili MTS, Chinedu Ikem J, Victor Chigozie U, Saki M. Antibiotic resistance: the challenges and some emerging strategies for tackling a global menace. J Clin Lab Anal. 2022 Sep;36(9):e24655. https://doi.org/10.1002/jcla.24655. Epub 2022 Aug 10. PMID: 35949048; PMCID: PMC9459344.
Dallal MMehdiS, Motalebi S, Asl HM. Mohammad Kazem Sharifi Yazdi et Abbas Rahimi Forushani,2020. Antimicrobial investigation on the multi-state outbreak of salmonellosis and shigellosis in Iran. Med J Islam Repub Iran 2020 May 18;34:49. doi: https://doi.org/10.34171/mjiri.34.49. eCollection 2020.
Farzad Khademi H, Vaez F, Ghanbari M, Arzanlou J, Mohammadshahi AS. 2020. Prevalence of fluoroquinolone-resistant Salmonella serotypes in Iran: a meta-analysis. Pathog Glob Health. 2020 Feb;114(1):16–29. doi: 10.1080/20477724.2020.1719701. Epub 2020 Feb 4.
Chen HM, Wang Y, Su LH, Chiu CH. Nontyphoid Salmonella infection: Microbiology, clinical features, and antimicrobial therapy. Pediatr Neonatol. 2013;54:147–52.
Moosavy M-H, Esmaeili S, Amiri FB, Mostafavi E, Salehi TZ. 2015. Detection of Salmonella spp in commercial eggs in Iran. Iran J Microbiol. 2015 Feb;7(1):50 – 4.
Hessam A, Halimi HA, Seifi R, Mehrnaz. Bovine salmonellosis in northeast of Iran: frequency, genetic fingerprinting and antimicrobial resistance patterns of Salmonella spp. Asian Pac J Trop Biomed 2014 Jan. 2014;4(1):1–7. https://doi.org/10.1016/S2221-1691(14)60199-4.
Ranjbar R, Safarpoor Dehkordi F, Heiat M. The frequency of resistance genes in Salmonella enteritidis strains isolated from cattle. Iran J Public Health 2020 May;49(5):968–74. PMID: 32953685; PMCID: PMC7475613.
Jamshidi A, Bassami MR, Afshari-Nic S. Identification of Salmonella spp. and Salmonella Typhimurium by a multiplex PCR-based assay from poultry carcasses in Mashhad- Iran. Iran J Vet Res. 2009;3:43–8.
Hassanzadeh SH, Emaddi Chashni M, Bozorgmehri Fard MH, Mirzaie S. 2009. Characterization of the Salmonella isolates from backyard chickens in North of Iran, by Serotyping, Multiplex PCR and antibiotic resistance analysis. Arch Razi Inst, Vol. 64, No. 2.77-83.
Shakerian A, Rahimi E, Emad P. Vegetables and restaurant salads as a reservoir for Shiga toxigenic Escherichia coli: distribution of virulence factors, O-serogroups, and antibiotic resistance properties. J Food Prot. 2016;79(7):1154–60.
Shakerian A, Barton MD, Akinbowale OL, Khamesipour F. Antimicrobial resistance profile and resistance genes of Vibrio species isolated from giant freshwater prawn (Macrobrachium rosenbergii) raised in Iran. J Hellenic Veterinary Med Soc. 2017;68(1):79–88.
Proroga YTR, Mancusi A, Peruzy MF, Carullo MR, Montone AMI, Fulgione A, Capuano F. Characterization of Salmonella Typhimurium and its monophasic variant 1,4, [5],12:i:-isolated from different sources. Folia Microbiol. 2019;64:711–8. https://doi.org/10.1007/s12223-019-00683-6.
Ma M, Wang HI, Yu Y, Yong D, Zhang, Liu S. Detection of antimicrobial resistance genes of pathogenic Salmonella from swine with DNA microarray. J Vet Diagn Invest. 2007;19:161–7.
Kumar M, Dahiya S, Sharma P, Sharma S, Singh TP, Kapil A, et al. Structure based in silico analysis of quinolone resistance in clinical isolates of Salmonella Typhi from India. PLoS ONE. 2015;10(5):e0126560.
Hussein RA, Al-Ouqaili MTS, Majeed YH. (2021). Detection of Helicobacter Pylori infection by invasive and non-invasive techniques in patients with gastrointestinal diseases from Iraq: A validation study. PLoS One. 23;16(8):e0256393. doi https://doi.org/10.1371/journal.pone.0256393. PMID: 34424925; PMCID: PMC8382163.
Al-Ouqaili MTS, Khalaf EA, Al-Kubaisy SH. DNA sequence analysis of BlaVEB Gene Encoding Multi-drug Resistant and extended-spectrum β-lactamases producer isolates of Enterobacteriaceae and Pseudomonas aeruginosa. Open Microbiol J. 2020;4:40–7.
Huong LQ, Reinhard F, Padungtod P, Hanh TT, Kyule MN, Baumann MP, et al. Prevalence of Salmonella in retail chicken meat in Hanoi, Vietnam. Volume 1081. Annals of the New York Academy of Sciences; 2006. pp. 257–61.
Yang B, Xi M, Wang X, Cui S, Yue T, Hao H, et al. Prevalence of Salmonella on raw poultry at retail markets in China. J Food Prot. 2011;74(10):1724–8.
Abatcha MG, Effarizah ME, Rusul G. Prevalence, antimicrobial resistance, resistance genes and class 1 integrons of Salmonella serotypes in leafy vegetables, chicken carcasses and related processing environments in malaysian fresh food markets. Food Control. 2018;91:170–80.
Soomro AH, Khaskheli MS, Bhutto MB, Shah G, Memon A, Dewani P. Prevalence and antimicrobial resistance of Salmonella serotypes isolated from poultry meat in Hyderabad, Pakistan. Turkish J Vet Anim Sci. 2010;34:455–60.
Zwe YH, Tang VC, Aung KT, Gutiérrez RA, Ng LC, Yuk H. Prevalence, sequence types, antibiotic resistance and, gyrA mutations of Salmonella isolated from retail fresh chicken meat in Singapore. Food Control. 2018;90:233–40.
Azizpour. 2021. Prevalence and Antibiotic Resistance of Salmonella Serotypes in Chicken Meat of Ardabil, Northwestern Iran. Iran J Med Microbiol. 2021; 15(2): 232–246.
Zhao X, Ye C, Chang W, Sun S, Qian Y. Antibiotic resistance of Salmonella isolated from food animals: a review. Front veterinary Sci. 2017;4:126. https://doi.org/10.3389/fvets.2017.00126.
Peighambari SM, Akbarian R, Morshed R, Yazdani A. Characterization of Salmonella isolates from poultry sources in Iran. Iran J Vet Med. 2013;7:35–41.
Ezzatpanah A, Moradi BS, Khaki P, Ghaderi R, Seyedan Jasbi SIsolation. Determination of serotype and pattern of Antibiotic Resistance of isolated Salmonella from Poultry in Arak. Iran Vet J. 2013;9(2):88–96.
Asadpour Y, Mohammadi M, Pourbakhsh SA, Rasa M. Isolation, serotyping and antibiotic resistance of Salmonella isolated from chicken carcasses in Guilan province. Iran Vet J. 2013;9(4):5–13.
Raeisi A, Ghiyami RM. Survey on Prevalence of Salmonella Serogroups and Antibiotics Susceptibility Pattern in Chicken meat in Ardabil. Iran J Ardabil Uni Med Scie. 2015;15(3):320–9.
Sodagari HR, Mashak Z, Ghadimianazar A. Prevalence and antimicrobial resistance of Salmonella serotypes isolated from retail chicken meat and giblets in Iran. J Infect Dev Count. 2015;9(5):463–9.
Adesiji YO, Fagbami AH. Epidemiology of bacterial zoonosis in Nigeria. Niger J Health Biomed Sci. 2006;5:20–5.
Ahmed AM, Shimamoto T. Genetic analysis of multiple antimicrobial resistance in Salmonella isolated from diseased broilers in Egypt. Microbiol Immunol. 2012;56:254–61.
Adesiji YO, Deekshit VK, Karunasagar I. Antimicrobial-resistant genes associated with Salmonella spp. isolated from human, poultry, and seafood sources. Food Sci Nutr. 2014;2:436–42.
Ahmed HA, El-Hofy FI, Shafik SM, Abdelrahman MA, Elsaid GA. Characterization of virulence-associated genes, antimicrobial resistance genes, and class 1 integrons in Salmonella enterica serotype typhimurium isolates from chicken meat and humans in Egypt. Foodborne Pathog Dis. 2016;13(6):281–8.
Acknowledgements
The authors would like to thank Dr. M. Momeni Shahraki for his assistance in sample collection.
Funding
Not applicated.
Author information
Authors and Affiliations
Contributions
ER, and MN carried out the molecular genetic studies, participated in the primers sequence alignment, and drafted the manuscript. MN and AS carried out the sampling and culture method. ER, HM, and AS participated in the study’s design, performed the statistical analysis, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research was ethically approved by the Council of Research of the Faculty of Veterinary Medicine, Shahrekord Branch, Islamic Azad University, Shahrekord, Iran. Verification of this research project and the licenses related to sampling process were approved by the Prof. Ebrahim Rahimi (Approval Ref Number MIC19818).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nazari Moghadam, M., Rahimi, E., Shakerian, A. et al. Prevalence of Salmonella Typhimurium and Salmonella Enteritidis isolated from poultry meat: virulence and antimicrobial-resistant genes. BMC Microbiol 23, 168 (2023). https://doi.org/10.1186/s12866-023-02908-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-023-02908-8