Abstract
Background
The food industry is increasingly becoming more scrutinized, given the frequency and intensity with which zoonotic diseases are being reported. Pathogen tracking has become more applicable with regards food safety. It is in this regard that the present study was formulated to track Listeria species. in freshly slaughtered cattle carcasses by utilizing standard and molecular biological techniques.
Methods
A cross-sectional study design was conducted from March to December 2020 with 200 samples being equally collected in the rainy and dry seasons. A total of 180 and 20 swabs were aseptically collected from carcasses and the environment respectively. Samples were first subjected to pre-enrichment in half-strength Fraser broth followed by enrichment in full strength Fraser broth and subsequent plating on Listeria agar. Listeria growth characteristics were identified up to species level based on their morphological and biochemical characteristics. Further, molecular detection and phylogenetic analysis was conducted. Quantitative proportionate survey data were analyzed using Stata Version 15 software to estimate crude prevalence taking into account complex design at abattoir level. Factors associated with contamination were characterized using logistic regression. Sequences were analyzed using, Genetyyx version 12 and phylogenetic Mega.
Results
Of the 200 samples, 19 were positive for Listeria species identified as L.innocua 14/19 (73.7%) and L. monocytogenes 5/19 (26.3%). All isolates were from freshly slaughtered carcasses, and none from environment. Siginificant differences in contamination levels were observed based on season: rainy season yielded 14 (73.6%) whilst the dry season 5 (26.3%). The L. monocytogenes strains showed a high degree of homogeneity on phylogenetic analysis and clustered based on abattoir. Seasonality was identified as a major determinant influencing contamination based on the final logistic regression model.
Conclusion
This study found evidence of L. monocytogenes contamination on traditionally raised beef carcasses across various abattoirs surveyed. The failure to find Listeria contamination on the abattoir environment may to a greater extent intimate cattle carccases as primary sources of contamination. However, a more comprerehnsive study incorporating different geographical regions is needed to conclusively ascertain these present findings.
Similar content being viewed by others
Introduction
Listeriosis infection is caused by Listeria monocytogenes (L. monocytogenes) bacteria of the genus Listeria. L. monocytogenes is a major pathogen that primarily affects pregnant women, newborns, older adults, and people with weakened immune systems [1]. People usually get infected with Listeria after eating contaminated food [2]. Cattle farms are an important array in spreading Listeria pathogens in food animals compared to small ruminant farms [3, 4]. The ruminant farm animals perpetuate the persistence of Listeria species in the rural environment via a continuous faecal-oral cycle [5, 6]. Moreover, the risk of Listeriosis in cattle increases when ensilage foods are provided or if animals graze on contaminated pasture [4, 7]. Although, other parameters such as good herd health management play a pivotal role in ensuring the microbiological quality of beef [8]. Listeriosis is an uncommon to cause of illness in the general population. The annual incidence of the European Union countries is 2–10 cases per million people [9].In the U.K., an outbreak of Listeriosis occurred, which affected pregnant women who purchased sandwiches from hospital-based retail shops [10]. A report in the United States indicates the incidence rates of 0.3 cases per 100,000 of Listeriosis in recent years transmitted via food [11]. Africa has a record of about 91 million people who have foodborne related diseases in 2015, while South Africa in 2019 recorded an outbreak of Listeriosis which was confirmed to come from a food source [12, 13]. While in Zambia, Listeria species, more specifically L. monocytogenes contamination, was detected in freshly cut organic vegetables sampled on farms grown for exportation [14]. Incidentally, Listeria species are reported to colonize a wide array of food products because of their ubiquitous nature in the environment [15]. The prevalence reports of Listeria species, including L. monocytogenes, in meat and raw meat products have been investigated in several countries [16, 17]. Additionally, Listeria species are post-processing contaminants that may arise due to inadequate cleaning and poor separation techniques between the ready to get foods and the raw foods [18].
Beef is among the known high-risk foods for pathogenic and non-pathogenic bacteria [16, 17]. Traditional meat inspections, lacking Good Manufacturing Practices (G.M.P.s), cannot assure the attainment and maintenance of high hygienic standards for meat regarding contamination with pathogenic bacteria such as L. monocytogenes [19]. The establishment of Hazard Analysis Critical Control Points (HACCP) is also important to ensure systematic control of meat slaughter processes regarding microbiological safety, spoilage, and storage stability [20]. Consequently, regulatory authorities are now moving towards the requirement for such systems in the meat industry [21]. Mostly, the traditional approach to assuring product quality involves inspections of sampled products from each batch and determining the proportion of samples that fail to meet the expected quality. Although this quality assurance method is usually feasible when throughputs are small, it becomes increasingly impractical as volumes increase [22].
The major contamination concerns in high-risk foods like beef are pathogens such as parasites, viruses, and most common bacteria [23]. Recently, several bacteria such as Salmonella and Escherichia coli that contaminate food origins have been documented in Zambia [24]. Listeria, more importantly, L. monocytogenes, is also among the group of bacteria of public health significance that is known to contaminate food. Listeria is ubiquitous in the environment, such as soil, manure, and grass [15]. Listeria species are facultatively anaerobic, non-spore-forming, a motile intracellular pathogen that comprises seventeen recognized species [25, 26]. Among the species of Listeria, the only one implicated in human infections is L. monocytogenes while Listeria ivanovii mainly affects ruminants [27]. More importantly is L. monocytogenes with a reported fatality of about 30%, while other species like Listeria innocua (L.innocua) and Listeria seeligeri are rarely pathogenic to humans. Listeria, by nature, maybe persistent in most food processing environments; once introduced in slaughter facilities may survive for years [28, 29]. Isolation of other Listeria species may indicate the absence of L. monocytogenes because it can be suppressed, especially in the presence of L.innocua; thus, this may increase the high rate of negativity for L. monocytogenes [30].
A study titled abattoirs, butcheries, and restaurants revealed high contamination in the dry season than wet season [31]. They attributed this difference to be because more samples were collected in the dry season than the wet season [32]. Other risks of Listeria contamination may be farm-specific such as the hygienic status of where the animals are kept, source of water, and feed [33]. In the same study, genetic relatedness of strains sampled from different farms was observed. The finding suggested, among others, carcass contamination originating from both incoming animals as well as transmission due to slaughter practices and persistent contamination coming from slaughterhouses [33].
The standard known microbiological methods routinely used for isolating Listeria species including L. monocytogenes in different samples usually require two enrichment steps (enriched with Listeria selective supplements) which are later inoculated on the surface of the Listeria selective agar [34]. The prs is a general marker gene present in all Listeria species, which encodes the enzyme phosphoribosyl pyrophosphate synthetase to determine the genus [35]. Other authors have also used prs to screen the presence of Listeria species because it is known as the housekeeping gene [35, 36]. In Zambia, molecular studies on Listeria are non-existent. It lacks information regarding the prevailing Listeria species; thus, this study incorporates culture and phylogenetic analysis to determine the prevalence, species, and strains of Listeria in the Namwala district of Zambia. Furthermore, the study aimed to determine the relationship and relatedness of the Listeria strains isolated in different seasons from different abattoirs in the Namwala district by analysing the prs gene.
Methods
Study design
A cross-sectional study design was conducted from March to December 2020 with 200 samples being equally collected in the rainy and dry seasons. The swabs were collected from the surfaces of carcass including cold room and storage environments in the abattoirs.
Study site
Administratively, Zambia is divided into ten provinces, and among these provinces is the Southern province, which has the highest livestock-raising households accounting for 16%, with the majority residing in the Namwala district [37]. Namwala, which is located between the latitudes 15 and 170 South of the equator and longitude 25 and 270 East, has the greatest stretch of its traditional land covered by the Kafue flood plains, which offers nutritious varieties of green grass for wildlife, and approximately 300,000 cattle it houses [38]. It is also known to be the natural hub of traditionally reared beef produce supplied in most parts of Zambia [39]. As a result, several beef abattoirs are being constructed to answer the call of production [39]. Furthermore, most of the beef slaughtered in Namwala is not only consumed within but also supplied to all parts of Zambia [39].
Namwala District has six beef processing abattoirs [39], of which all were incorporated in this study except for one that was waiting to be commissioned for opening. The district was selected because it houses the largest number of abattoirs that supply beef on a small scale and commercial bases throughout the country [38]. Furthermore, Southern Province is reported to contribute the highest number of cattle compared to other Provinces [37]. The abattoirs involved were identified as one, two, three, four, and five.
Sample size and sampling
One hundred eighty carcass swabs and 20 environmental swabs were collected from five beef abattoirs. Sample size estimatation was based on an assumed prevalence of 27.5% [40] at 80% power and a 5% significance level. The two hundred samples were divided equally as one hundred each for exterior and interior carcass swabs, including sampling season. All swabs were collected immediately after evisceration and hide removal. The total maximum throughput for all the abattoirs for a day was reported to be 150 carcasses, the stated sample size was equally allocated to the abattoirs, and a total of 36 carcass swabs and four environmental samples per site were collected. The abattoirs, having the same maximum capacity throughput, slaughtered an average of 30 carcasses per day, with only one recording slaughters of 90 per day as a maximum. Complex design was employed to account for bias brought about by oversampling and under-sampling of certain abattoirs. Simple random sampling was the technique that was used to pick the carcass for swabbing through shuffling before the next pick was done.
Sample collection and processing
Bacteriological standard sample collection for Listeria contamination was used on samples collected from five abattoirs [41]. A template metal that was sterile was used to outline 5 × 5cm2 area parts marked for swabbing, including environmental swabs [42]. Surface swabs were collected from the interior and exterior parts of the carcasses. The outlined areas by the metal template were swabbed with a sterile moist cotton gauze which was wrapped around the end of a flat swab stick. Swab samples were placed in screw-cap tubes containing Amies transport media [41]. The swab samples were identified according to date, ingredient samples (e.g. Beef carcass), batch code, and site name, including comments specific to the sample (e.g. interior or exterior), were recorded. All samples were given codes for easy identification according to sampling site/product or ingredient type, date, and site further, and these samples were all kept at -4ºC before being transported within 72 h at the Microbiology laboratory at the School of the Veterinary Medicine University of Zambia. The samples were immediately transferred in 9 ml of pre-enrichment broth and later incubated at 37 ºC for 48 h. Before isolation from swab diluents, samples were vortexed for 30 s and then plated on selective media to detect the target micro-organisms [42] in both environmental and carcass swab samples.
Isolation and identification of Listeria species
The beef carcass swabs were tested for the presence of Listeria species using Standard international methods which were recommended by the International Organization for Standardization (ISO g11290 -1: 1996, 2004) procedure. First, a 1 g of the sample representative portion from each was inoculated in 9 ml of pre-enriched broth and incubated at 37 ºC for 24 h, then 1 ml of pre-enriched broth was transferred into 9 ml of Fraser broth (Oxoid) (enriched with Listeria selective supplement) and vortexed for 1 min, followed by incubation at 37 ºC for 48 h. A loop-full of pre-enrichment broth (Oxoid) culture was inoculated on the surface of Listeria selective agar (Oxoid), incubated at 37 ºC for 48 h, and observed for colonies showing growth typical greenish sheen morphology or green–blue colonies' colour of Listeria. The suspected colonies were then sub-cultured onto Nutrient Agar (Oxoid) and later incubated at 37 ºC for 24 h to obtain pure colonies. Some standard biochemical tests were done on the purified cultures, namely, Gram's staining, citrate, urea, indole, motility, oxidase, catalase, and methyl-red tests to obtain a presumptive diagnosis of Listeria.
DNA extraction and PCR Identification of Listeria
Following biochemical tests, polymerase chain reaction (PCR) assays were performed to confirm the presumptive isolates of Listeria species. D.N.A. was extracted from the pure culture of the suspected isolates, grown on nutrient agar using a commercial genomic D.N.A. extraction kit (ZYMO Research quick D.N.A. miniprep kit) as per the manufacturer's instructions. The primer pairs designated as prs -F (5'- GCT GAA GAG ATT GCG AAA GAA G – 3') and prs-R (5’-CAA AGA AAC CTT GGA TTT GCG G- 3') were used to amplify a 370 bp fragment of the Listeria prs gene [43]. A 50 µl PCR master mixture, consisting of 5 ul of 10 × PCR buffer, 1.5 ul of 0.5 ul of Taq D.N.A. polymerase, 1 ul of 10 mM dNTP5 mix (10 Mm l µl), 100 ng of template and Nuclease. The thermal cycler conditions were: initial denaturation at 94 ºC for 2 min followed by 35 cycles, denaturation at 94 ºC for 45 s, annealing at 53 ºC for 45 s, and extension at 72 ºC for 2 min with a final extension, at 72 ºC for 7 min. The amplified PCR products were visualized on 1% agarose gel coated with ethidium bromide.
Purification of PCR products and cycle sequencing
The amplified PCR products were purified using a Promega purification kit (Wizard S.V. Gel & PCR Promega clean-up System) per the manufacturer's instructions [44]. According to the manufacturer's instructions, the Purified PCR products were then subjected to sequencing PCR reaction using brilliant dye terminator ver.3.1 kits according to the manufacturer's instructions. The sequence products were precipitated as described by [45] after denaturation with formamide were then subjected to capillary electrophoresis on the ABI 3500 Genetic Analyzer [46].
Data analysis
The obtained data from the beef carcasses and the storage environment was entered in the Excel sheet and imported to Stata version 15 (Stata cop, college station, Texas, U.S.A.) for all analyses. The primary outcome was Listeria or Listeria species (i.e. L. innocua and L. monocytogenes) contamination from various beef carcass swabs, including environmental swabs. The prevalence of Listeria contamination was calculated as the proportion of the total beef carcasses collected that were contaminated, taking into account proportional weights for abattoir throughputs. Factors associated with Listeria contamination such as seasons, part swabbed, and abattoir name were investigated, considering complex design at abattoir level (clusters). To account for confounders, forward stepwise model building was used by conducting univariate logistic regression, and all factors that were significant inclusion in the multivariable logistic model was considered. Complex design was used to account for intra –cluster correlation in this study. All analyses in this study were stratified by site, and a p-value of 0.05 was used to determine statistical significance using a likelihood ratio test.
Sequence analysis
Nucleotide sequences obtained in this study were first subjected to blast analysis on the NCBI website (https://blast.ncbi.nlm.nih.gov/Blast.cgi) to verify the species of bacteria or Listeria obtained, followed by assembly and editing using the ATGC plug-in Genetyx ver. 12. Using the obtained sequences and reference sequences downloaded from the GenBank, a multiple sequence alignment was constructed using clustalW1.6 (Supplementary Fig. 1). Furthermore, a fasta file of the multiple alignments was generated using MEGA 6 [47, 48] and utilized to construct a neighbour-joining phylogenetic tree with 1000 bootstrap replicates as a measure of the confidence interval [47, 48]. All the generated sequences in this study have been deposited in the DNA Data Base of Japan with accession numbers LC629080 to LC629098 (Supplementary Table 1).
Results
Descriptors of Listeria prevalence
Of the 200 environmental and beef carcasses collected,19 had Listeria species of which 20 came from environmental swabs and 180 from carcass swabs. When specific Listeria contamination in the abattoirs was considered, L. innocua accounted for 14 (73.7%) and L. monocytogenes 5 (26.3%).
Furthermore, when specific establishment contamination was considered abattoir one, showed the highest contamination of both L. innocua 8 (42.1%) and L. monocytogenes 4 (21.1%). Meanwhile, no Listeria species were isolated from the environmental samples collected in this study. (Table 1).
Phylogenetic analysis
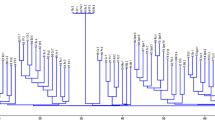
Phylogenetic analysis of the obtained sequences as well as the reference sequences showed the presence of three clusters, namely clusters A, B and C (Fig. 1). Cluster A comprised of both L. monocytogenes and L.innocua reference sequences as well as study sequences collected in both the dry and wet season from abattoir 1 and 2, with the majority originating from abattoir 1. On the other hand, clusters B and C exclusively comprised of L. innocua isolated from this study. In cluster B, sequences from abattoir 1, 2 and 3 collected both during the dry and wet season formed a cluster while in cluster C, sequences from abattoir 1 and 5 were present. Sequence LC629081 from this study did not cluster in any of the above clusters, however it was closely related with sequences from C (Fig. 1). Overall, phylogenetic analysis revealed that sequences collected in both the dry and wet season from abattoir 1 were represented in all clusters, while sequences from abattoir 5 were only present in cluster C. Clustering according to seasonality was not observed.
Phylogenetic tree. Comprising of 35 sequences (19 obtained in this study and 16 downloaded sequences from (GenBank) based on 370 bp partial nucleotide sequences of the prs gene of Listeria. The tree was inferred using the Neighbor-joining method with 1000 bootstrap replicates as a confidence interval. The Maximum Composite likelihood method was used to compute the evolutionary distances with all ambiguous positions for each sequence pair removed. The color codes and number at the end of the study sequences represent the abattoir of origin and the season of sampling is designated as D; dry season and W; wet season
Univariate analysis of Listeria species and L.innocua indicated season of sampling to be significantly related to contamination level (p < 0.0032) and (p < 0.0101), respectively; (Tables 2 and 3).
A logistic regression analysis was carried out to determine the strength of the association of factors that were likely to influence Listeria contamination in abattoirs. The season in which the sampling was done was significant for Listeria, with samples collected during the wet seasons having (OR = 3.31; 95% CI: 1.27–5.35) odds of contamination compared to the dry season. Similarly, the parts swabbed were equally significant, with the internal parts having (OR -1.17; 95% CI: -2.49 -1.59) odds of contamination compared to the external parts (Table 4).
A logistic regression analysis was used to determine the strength of the association of factors that were likely to influence L. innocua contamination in abattoirs. The season in which the sampling was done was found significant for L. innocua, with samples collected during the wet seasons having (OR 24.59; 95% CI: 1.64 – 368.8.7) odds of contamination compared to the dry season. Similarly, the parts swabbed were equally significant, with the internal parts having (OR 0.12; 95% CI: 0.09 – 1.67) odds of contamination compared to the external parts (Table 5).
Discussions
To the best of our knowledge, this study is the first in Zambia to isolate, determine and characterize Listeria from traditionally raised cattle carcasses from abattoirs. The unique ability of Listeria to survive food preservation or hostile environments, coupled with its long incubation period, makes it a serious threat to food safety and may potentially result in it being missed by diagnosticians and clinicians. In this study, we utilized molecular phylogenetic analysis to determine the relatedness of the isolated Listeria species and determine the proportion of different strains of Listeria. From this analysis, we identified two species of Listeria based on culture, biochemical tests, and finally, through gene sequencing of prs as L. monocytogenes and L. innocua. These present findings of 26.3% as L. monocytogenes is slightly higher than what was reported by Nguz et al. in (2005) who reported a prevalence of 20% in freshly cut vegetables harbouring L. monocytogenes [14]. Despite that their study was in vegetables, compared to this present study in meat, their findings presented a much lower percentage prevalence variance. Apart from the difference in sample sources, to some extent, the inconsistency in prevalence may conservatively be attributed to differences in the identification methods used between the two studies; Nguz et al. (2005) only utilized differential and selective agars (PALCAM and OXFORD agars) without any definitive molecular methods while in the current study, molecular techniques were utilized through PCR and sequencing of prs gene.
Molecular techniques are more reliable and have high differentiation power within and between organisms that exhibit similar characteristics compared to cultural methods [49]. To this regard, the present study attempted to further confirm the identity of Listeria species using PCR and sequencing of the prs gene. Blast analysis of the obtained sequences showed a similarity score ranging from 89% to 99.9% (Supplementary Table 1) and phylogenetic analysis revealed clustering of sequences under study (mainly from abattoir 1) with L. monocytogenes and L. innocua reference sequences in cluster A while other sequences under study formed exclusive clusters B and C (Fig. 1). Thus, despite the prs gene not being entirely able to disciminate Listeria to species level [43], through PCR and sequencing of the prs gene coupled with culture and biochemical tests, this study was able to ascertain the different types of Listeria species as L. innocua and L. monocytogenes based on Blast analysis (https://blast.ncbi.nlm.nih.gov/Blast.cgi) and the pattern of clustering on phylogenetic analysis (Fig. 1) [49]. One of the sequences (LC629092), despite showing a similarity score of 98.75% with L. monocytogenes, closely clustered with L. innocua in cluster A (Fig. 1). This observation can be attributed to the biological relatedness that exist between L. monocytogenes and L.innocua [50]. Furthermore, sequences from different abattoirs clustered together irrespective of the sample origin or season (Fig. 1) implying that the abattoir could be the source of contamination and not necessarily the farms because Listeria contamination was linked only to specific abattoirs with others ( i.e. abattoir 4) recording zero contamination. In addition, all sequences from abattoir 5 clustered together, further ascertaining the notion that the abattoir was the primary source of contamination. The data presented in this study is thus in agreement with previous studies were L. monocytogenes was observed to be endemic in specific abattoirs [51, 52].
In the recent past, L. monocytogenes caused a major outbreak in other African countries like South Africa [13], Zambia’s major trading partner, especially regarding the food of both animal and plant origin. During the same outbreak, the isolation of L. monocytogenes was reported mostly in cold meats, i.e. polonies [13]. Wieizorek's and others reported 19.4% of L. monocytogenes in beef meat samples [53]; in Malaysia, L. monocytogenes in meat samples was 8.6% [16], in Poland, bovine carcasses were found positive with L. monocytogenes at 2.5% attribution. While, in Iran, a lower prevalence was detected with only a single sample found contaminated with L. monocytogenes 2.7% [54], in the same country R.T.E. food samples were found contaminated with L. monocytogenes 19.1% [50]. This contamination difference can be linked to the handling processes that the R.T.E. foods undergo compared to the raw beef.
Furthermore, the above prevalence disparities recorded in other studies compared to the results of this current study can mainly be ascribed to methodological differences of isolation of the micro-organism in question [49]. The other important aspect can be aligned to the differences in the sampled foods and the ability of Listeria to survive in the same foods [55]. More importantly, Listeria is an ubiquitous bacteria in the environment and it is mainly introduced in the food due to inadequate hygienic practices were stringent measures are not employed this can also bring about differences in prevalence contamination in different studies reported [56].
This study also showed that L. innocua was the major contaminant.This is an important finding, because other studies have long suggested its usefulness as an indicator of the presence of L. monocytogenes [30]. Mostly L. innocua, although non-pathogenic to humans, may indicate lapses in food control systems in processing abattoirs. Mainly, contaminating bacteria are associated with the absence of prerequisite programs that help in ensuring food safety quality. In this present study, most contaminating bacteria were isolated in abattoirs that were observed to lack proper food management systems such as the implementation of Standard Operating Systems (SOSs) including HACCP. HACCP is a scientific tool that helps in the identification of hazards systematically [20, 27]. L. monocytogenes and L. innocua are common species in food processing plants, with the latter being prevalent; therefore, continuous monitoring is needed to avoid there existence [30, 57]. Therefore, when investigating the sources of L. monocytogenes, the isolation of L.innocua is equally high because it is commonly known to colonize food premises [30]. L. innocua has been reported by others to be more prevalent in food processing environments than L. monocytogenes [58]. Although the adaptive nature of L.innocua in the food processing environment is not fully understood, this is helpful information in controlling food pathogens [58]. Additionally, further studies are needed to ascertain the presence of L. monocytogenes and L. innocua if they are influenced by the respective environment (i.e. farms, food processing facilities, or foods). This could indicate whether one or more species is more likely to persist through the farm to fork continuum.
Meanwhile, no Listeria species were isolated from environmental swabs collected from storage cold-rooms in this study. The sample size allocated to the environmental swabs could have partly influenced the none isolation of Listeria species as only 20 swabs were collected from each abattoir. The other factor could be linked to the short storage of carcasses in the studied abattoirs after slaughter. Normally the carcasses from these abattoirs are only kept in the cold rooms for a maximum of two days and are later dispatched to their final destination. This, to a greater extent could have facilitated adequate cleaning, which could have been prevented if carcasses were stocked in the abattoir longer [59].
Contrary to this result, the finding in another study reported having isolated Listeria species on environmental samples 54.7% [60]. These variances in isolation can probably be explained by differences in the sampled environment concerning the storage system of carcasses and the length of storage from the two studies. The other differences can also be drawn from the hygienic conditions of specific abattoir facilities because Listeria is known to form biofilms that are resistant to most disinfectants commonly used in processing abattoirs [61].
From the total average number of contamination, the majority were recorded in the wet and dry seasons. Listeria is ubiquitous in the environments like soil, manure, and grass; this is comparable to free-range grazing of pasture in the dry season, which reduces the chances of cross-contamination because the feeding is off-site where animals are sheltered [15]. Other reports concluded the same with this current study with the highest number of L. monocytogenes recorded in the rainy season 3%, while dry 0.8% [62]. The rainy season in most parts of Zambia is cooler compared to the dry, hot season when the sampling took place. The characteristic nature of Listeria it thrives in cold environments and foods kept at extended refrigeration conditions [63]. There is some consistency in the above findings about contamination levels of this current study with regards to the season of sampling, and this can be attributed to the ubiquitous nature of Listeria and its ability to withstand the cold weather environment. During the wet season, its survival ability could have been enhanced due to moisture and cool temperatures.
Additionally, during grazing, the animals are most likely to consume viable Listeria pathogens available in the pasture because of the conducive environment provided in the wet season. Bacteria multiplication, among others, depends on moisture availability; this could partly explain the differences in the isolation rates in this given study [64]. This current study gives a snapshot of Listeria prevalence from sampling in the dry and wet season mouths at commercial abattoirs, and differences not found in the report may be attributable to several factors, including processing plants, the weather, and more importantly sources of cattle presented for slaughter on the sampled days.
The L. monocytogenes species, especially in raw beef carcasses, poses public health threat mainly when the meat is consumed raw or undercooked. More importantly, the other risk can be through cross-contamination during production at retail levels, especially in processing areas with poor hygienic practices. Incidences of Listeriosis mostly cumulates from consuming contaminated food items like R.T.E. foods, sea foods, dairy, vegetables, and beef carcasses [50, 65]. Therefore, it is important to ensure the safety of the natural products because the quality of the final product largely depends on it, as earlier indicated in the study done in poultry abattoirs [22]. Changing consumer trends such as the consumption of raw vegetables and undercooked foods such as beef are major reasons for causing foodborne infections [66]. Danger is created, especially if beef is contaminated with pathogenic micro-organisms such as L. monocytogenes [67]. Codex Alimentarius Commission, an international regulating body, has set guidelines on the allowable limits of L. monocytogenes in different types of foods to help producers easily perform quality checks on their food products [68].
Contamination variances of Listeria contamination were recorded across the abattoirs in this study, with some recording more to zero contamination. Mainly contamination differences are expected where there are environmental dissimilarities such as slaughter throughputs schedules of individual abattoirs, with some having more than others. Increased workload may have an influence on the frequency of cleaning especially in hard to reach cervices. Observation was done in a study of poultry abattoirs where increased contamination was recorded in an abattoir with high process throughput [22]. Further evidence was seen from the results reported in another study of abattoirs which displayed a similar picture of the current results of this survey [69]. Abattoir designs, especially those without clear separation between the clean and the dirty section, pose a huge risk of contamination on the food product compared to those abattoirs [22, 69]. As earlier elaborated, differences may also arise due to lack of hygienic practices by the food handlers working in the processing abattoirs, quality of water used, including environmental factors of the farms where these animals are coming from [70, 71].
The part-swabbed was also found significantly related to the contamination of Listeria species, with the internal part being more contaminated than the outer swabbed part. Contrary to this current findings, results were reported indicating no significant Listeria contamination with the parts swabbed [72]. Discrepancies recorded in the two studies could also be linked to the beef samples collected by Eruteya and colleagues who sampled cut pieces at the market.Uniform distribution may represent bacteria across all parts of the beef meat, unlike the carcasses sampled from the abattoirs. Some portions like external parts were not exposed to cutting compared to internal parts. The linkage is attributable to the handling and use of the knives or equipment that may be unsterilized from one carcass to another.High possibility of intestinal contaminants may aid the spreading through the internal part. The beef carcasses slaughtered in the investigated abattoirs were sourced from various farms with unknown risk parameters that we may not explain due to lack of supporting data. In abattoirs where adherence to good hygienic practices lacks the possibility of cross-contamination may occur through various utensils used. Other studies have elaborated the role of knives used for evisceration and cutting of carcasses to be among the major drivers of cross-contamination [71, 73, 74].
Conclusion
This study has been able to elucidate the presence of L. monocytogenes and innocua in traditionally raised beef carcasses across various abattoirs in the Namwala district of Zambia using traditional and molecular methods. Additionally, in the present study, L. innocua was isolated at a comparatively higher rate than L. monocytogenes. The failure to find Listeria contamination in the abattoir environment may, to a greater extent intimate cattle carccases as primary sources of contamination. However, a more comprerehnsive study incorporating different geographical regions and increased sample size will be needed to affirmatively and conclusively ascertain our present findings.
Availability of data and materials
All sequences emanating from this study have been deposited in the D.N.A. Data Base of Japan with accession numbers LC629080 to LC629098. All the data concerning this manscript are contained within the text.
Abbreviations
- ATGC:
-
Adenine, Thymine, Guanine, Cytosine
- HACCP:
-
Hazard Analysis Critical Point
- WHO:
-
World Health Organization
- G.M.P.s:
-
Good Manufacturing Practices
- D.N.A.:
-
Deoxyribonucleic acid
- PCR:
-
Polymerase Chain Reaction
- rRNA:
-
Ribosomal ribonucleic acid
- prs:
-
Phosphoribosyl pyrophosphate synthetase
- C.S.O.:
-
Central Statistical Office
- N.C.C.:
-
Namwala Municipal Council
- e.g.:
-
Example given
- ISO:
-
International Standard Organization
- g:
-
Gram
- cm2 :
-
Centimeters squared
- 0 C:
-
Degrees Celsius
- NCBI:
-
National Center for Biotechnology Information
- MEGA6:
-
Molecular Evolutionary Genetics Analysis version 6.0
- ACEIDHA:
-
Africa Center of Excellence for Infectious Diseases of Humans and Animals
- MFLCSO:
-
Ministry of Fisheries and Livestock Central Statistical Office
- ml:
-
Millie litre
- ppm:
-
Parts per million
- CI:
-
Confidence Interval
- SOSs:
-
Standard Operating Systems
References
Radoshevich L, Cossart P. Listeria monocytogenes: towards a complete picture of its physiology and pathogenesis. Nat Rev Microbiol. 2018;16(1):32–46. https://doi.org/10.1089/fpd.2017.409.
Rodrigues CS, Sá CVGCD, Melo CBD. An overview of Listeria monocytogenes contamination in ready to eat meat, dairy and fishery foods. Ciência Rural 2017;47(2) https://doi.org/10.1590/0103-8478cr20160721.
Walland J, Lauper J, Frey J, Imhof R, Stephan R, Seuberlich T, et al. Listeria monocytogenes infection in ruminants: is there a link to the environment, food and human health? A review. 2015;157(6):319-28. https://doi.org/10.5167/uzh-122097.
Castro H, Jaakkonen A, Hakkinen M, Korkeala H, Lindström M. Occurrence, persistence, and contamination routes of Listeria monocytogenes genotypes on three Finnish dairy cattle farms: a longitudinal study. Appl Environ Microbiol 2018;84. https://doi.org/10.1128/AEM.02000-17(4).
Vázquez-Boland JA, Kuhn M, Berche P, Chakraborty T, Domı́nguez-Bernal G, Goebel W, et al. Listeria pathogenesis and molecular virulence determinants. 2001;14(3):584-640. https://doi.org/10.1128/CMR.14.3.584-640.2001.
Kulesh R, Shinde S, Khan W, Chaudhari S, Patil A, Kurkure N, et al. The occurrence of Listeria monocytogenes in goats, farm environment and invertebrates. 2019:1-10. https://doi.org/10.1080/09291016.2019.1660836.
Donnelly CW. Detection and isolation of Listeria monocytogenes from food samples: implications of sublethal injury. J AOAC Int. 2002;85(2):495–500.
Olaimat AN, Al-Holy MA, Shahbaz HM, Al-Nabulsi AA, Abu Ghoush MH, Osaili TM, et al. Emergence of antibiotic resistance in Listeria monocytogenes isolated from food products: a comprehensive review. Compr Rev Food Sci Food Saf. 2018;17(5):1277–92.
De Valk H, Jacquet C, Goulet V, Vaillant V, Perra A, Simon F, et al. Surveillance of listeria infections in Europe. Euro Surveill. 2005;10(10):9–10.
Dawson S, Evans M, Willby D, Bardwell J, Chamberlain N, Lewis DJE. Listeria outbreak associated with sandwich consumption from a hospital retail shop, United Kingdom. Euro Surveill. 2006;11(6):9–10.
Tack DM, Ray L, Griffin PM, Cieslak PR, Dunn J, Rissman T, et al. Preliminary incidence and trends of infections with pathogens transmitted commonly through food—Foodborne Diseases Active Surveillance Network, 10 US Sites. Morb Mortal Wkly Rep2016–2019. 2020;69(17):509.
WHO. WHO estimates of the global burden of foodborne diseases: foodborne disease burden epidemiology reference group 2007–2015. WHO. 2015. WHO Press, World Health Organisation. www.who.int. Accessed 4 Apr 2021.
Sibisi AS. Food hygiene, safety, handling practices and knowledge of food handlers in a food retail company in Durban, KwaZulu-Natal, Ssouth Africa. http://hdl.handle.net/10321/3212 2019.
Nguz K, Shindano J, Samapundo S, Huyghebaert A. Microbiological evaluation of fresh-cut organic vegetables produced in Zambia. Food Control. 2005;16(7):623–8. https://doi.org/10.1016/j.foodcont.2004.07.001.
Aguilar-Bultet L, Nicholson P, Rychener L, Dreyer M, Gözel B, Origgi FC, et al. Genetic separation of Listeria monocytogenes causing central nervous system infections in animals. 2018;8:20. https://doi.org/10.3389/fcimb.2018.00020.
Marian M, Aminah SS, Zuraini M, Son R, Maimunah M, Lee H, et al. MPN-PCR detection and antimicrobial resistance of Listeria monocytogenes isolated from raw and ready-to-eat foods in Malaysia. 2012;28(2):309-14. https://doi.org/10.1016/j.foodcont.2012.05.030.
Liu Y, Sun W, Sun T, Gorris LG, Wang X, Liu B, et al. The prevalence of Listeria monocytogenes in meat products in China: a systematic literature review and novel meta-analysis approach. 2020;312:108358. https://doi.org/10.1016/j.ijfoodmicro.2019.
Kurpas M, Wieczorek K, Osek J. Ready-to-eat meat products as a source of Listeria monocytogenes. J Vet Res. 2018;62(1):49–55. https://doi.org/10.1515/jvetres-2018-0007.
Tian F, editor A supply chain traceability system for food safety based on HACCP, blockchain & Internet of things. 2017 International conference on service systems and service management; 2017: IEEE. https://doi.org/10.1109/ICSSSM.2017.7996119.
Wu X, Suksawat F, Richards AL, Phommachanh S, Phongaran D, Angkititrakul S. Evaluation of the Containment of Antimicrobial-Resistant Salmonella Species from a Hazard Analysis and Critical Control Point (HACCP) and a Non-HACCP Pig Slaughterhouses in Northeast Thailand. Pathogens. 2020;9(1):20. https://doi.org/10.3390/pathogens9010020.
Panghal A, Chhikara N, Sindhu N, Jaglan S. Role of food safety management systems in safe food production: a review. J Food Saf. 2018;38(4):e12464. https://doi.org/10.1111/jfs.
Mpundu P, Mbewe AR, Muma JB, Zgambo J, Munyeme M. Evaluation of bacterial contamination in dressed chickens in Lusaka Abattoirs. Front Public Health. 2019;7:19. https://doi.org/10.3389/fpubh.2019.00019.
Sharif MK, Javed K, Nasir A. Foodborne illness: threats and control. Foodborne Diseases Elsevier. https://doi.org/10.1016/B978-0-12-811444-5.00015-4 2018. p. 501–23.
Mpundu P, Mbewe AR, Muma JB, Sitali GM, Mubita CM, Munyeme M. Comparison of Bacterial Cross-Contamination among Broiler Carcasses between Commercial and Non-Commercial Processed System and Its Public Health Implications. ID:106721,13 pages. J Vet Med https://doi.org/10.4236/ojvm.2021.111001. 2021.
Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis. 2011;17(1):7.
Leclercq A, Moura A, Vales G, Tessaud-Rita N, Aguilhon C, Lecuit M, et al. Listeria thailandensis sp. nov. Int J Syst Evol Microbiol. 2019;69(1):74–81. https://doi.org/10.1099/ijsem.0.003097.
Milillo SR, Friedly EC, Saldivar JC, Muthaiyan A, O'bryan C, Crandall PG, et al. A review of the ecology, genomics, and stress response of Listeria innocua and Listeria monocytogenes. 2012;52(8):712-25. https://doi.org/10.1080/10408398.2010.507909.
Leong D, NicAogáin K, Luque-Sastre L, McManamon O, Hunt K, Alvarez-Ordóñez A, et al. A 3-year multi-food study of the presence and persistence of Listeria monocytogenes in 54 small food businesses in Ireland. 2017;249:18–26. https://doi.org/10.1016/j.ijfoodmicro.2017.02.015.
Pesavento G, Ducci B, Nieri D, Comodo N, Nostro AL. Prevalence and antibiotic susceptibility of Listeria species isolated from raw meat and retail foods. Food control. 2010;21(5):708–13. https://doi.org/10.1016/j.foodcont.2009.10.012.
Zitz U, Zunabovic M, Domig KJ, Wilrich PT, Kneifel W. Reduced detectability of Listeria monocytogenes in the presence of Listeria innocua. J Food Prot. 2011;74(8):1282–7. https://doi.org/10.3389/fcimb.2018.00020.
Gebremedhin EZ, Hirpa G, Borana BM, Sarba EJ, Marami LM, Kelbesa KA, et al. Listeria Species Occurrence and Associated Factors and Antibiogram of Listeria monocytogenes in Beef at Abattoirs, Butchers, and Restaurants in Ambo and Holeta in Ethiopia. Infect Drug Resis. 2021;14:1493.
Gebremedhin EZ, Hirpa G, Borana BM, Sarba EJ, Marami LM, Tadese ND, et al. Detection of Listeria species, factors associated, and antibiogram of Listeria monocytogenes in beef at abattoirs, butchers, and restaurants of Ambo and Holeta Towns, Ethiopia. https://orcid.org/0000-0002-9432-6532. 2020.
Demaître N, Van Damme I, De Zutter L, Geeraerd A, Rasschaert G, De Reu K. Occurrence, distribution and diversity of Listeria monocytogenes contamination on beef and pig carcasses after slaughter. Meat Sci. 2020;169:108177. https://doi.org/10.1016/j.meatsci.2020.
Barocci S, Calza L, Blasi G, Briscolini S, De Curtis M, Palombo B, et al. Evaluation of a rapid molecular method for detection of Listeria monocytogenes directly from enrichment broth media. Food Control. 2008;19(8):750–6.
Nightingale K, Windham K, Martin K, Yeung M, Wiedmann M. Select Listeria monocytogenes subtypes commonly found in foods carry distinct nonsense mutations in inlA, leading to expression of truncated and secreted internalin A, and are associated with a reduced invasion phenotype for human intestinal epithelial cells. Appl Environ Microbiol. 2005;71(12):8764–72.
Graves LM, Swaminathan B. PulseNet standardized protocol for subtyping Listeria monocytogenes by macrorestriction and pulsed-field gel electrophoresis. Int J Food Microbiol. 2001;65(1–2):55–62.
MFL C. The 2017/2018 Livestock and Aquaculture Census. Summary Report. Lusaka, Zambia.; 2019.
Munyeme M, Muma JB, Munang’andu HM, Kankya C, Skjerve E, Tryland M. Cattle owners’ awareness of bovine tuberculosis in high and low prevalence settings of the wildlife-livestock interface areas in Zambia. BMC Vet Res. 2010;6(1):21. https://doi.org/10.1186/746-6148-6-21.
NMC. Data Entry Book. Namwala, Zambia; 2020.
Derra FA, Karlsmose S, Monga DP, Mache A, Svendsen CA, Félix B, et al. Occurrence of Listeria species in retail meat and dairy products in the area of Addis Ababa, Ethiopia. 2013;10(6):577–9. https://doi.org/10.1089/fpd.2012.1361.
Alsheikh A, Mohammed G, Abdalla M. Isolation and identification of Listeria monocytogenes from retail broiler chicken ready to eat meat products in Sudan. Int J Anim Vet Adv. 2013;5(1):9–14. https://doi.org/10.19026/ijava.5.5570.
Holah J, Bird J, Hall K. The microbial ecology of high-risk, chilled food factories; evidence for persistent Listeria species and Escherichia coli strains. J Appl Microbiol. 2004;97(1):68–77. https://doi.org/10.1111/j.365-2672.004.02272.
Doumith M, Buchrieser C, Glaser P, Jacquet C, Martin P. Differentiation of the major Listeria monocytogenes serovars by multiplex PCR. J Clin Microbiol. 2004;42(8):3819–22. https://doi.org/10.1128/JCM.42.8.3819-22.2004.
Leontiou CA, Hadjidaniel MD, Mina P, Antoniou P, Ioannides M, Patsalis PC. Bisulfite conversion of DNA: performance comparison of different kits and methylation quantitation of epigenetic biomarkers that have the potential to be used in non-invasive prenatal testing. PLoS One. 2015;10(8):e0135058. https://doi.org/10.1371/journal.pone.
Foley NM, Petit EJ, Brazier T, Finarelli JA, Hughes GM, Touzalin F, et al. Drivers of longitudinal telomere dynamics in a long‐lived bat species, Myotismyotis. 2020;29(16):2963-77. https://doi.org/10.1111/mec.15395.
Bright JA, Neville S, Curran JM, Buckleton JS. Variability of mixed DNA profiles separated on a 3130 and 3500 capillary electrophoresis instrument. Aust J Forensic Sci. 2014;46(3):304–12. https://doi.org/10.1080/00450618.2013.851279.
Muleya W, Namangala B, Mweene A, Zulu L, Fandamu P, Banda D, et al. Molecular epidemiology and a loop-mediated isothermal amplification method for diagnosis of infection with rabies virus in Zambia. Virus Res. 2012;163(1):160–8.
Muleya W, Chambaro HM, Sasaki M, Gwenhure LF, Mwenechanya R, Kajihara M, et al. Genetic diversity of rabies virus in different host species and geographic regions of Zambia and Zimbabwe. Virus Genes. 2019;55(5):713–9.
Allerberger F. Listeria: growth, phenotypic differentiation and molecular microbiology. FEMS Immunol Med Microbiol. 2003;35(3):183–9. https://doi.org/10.1016/S0928-8244(02)00447-9.
Rahimi E, Yazdi F, Farzinezhadizadeh H. Prevalence and antimicrobial resistance of Listeria species isolated from different types of raw meat in Iran. J Food Prot. 2012;75(12):2223–7. https://doi.org/10.4315/0362-028X.JFP-11-565.
Ojeniyi B, Wegener HC, Jensen N, Bisgaard M. Listeria monocytogenes in poultry and poultry products: epidemiological investigations in seven Danish abattoirs. J Appl Bacteriol. 1996;80(4):395–401.
Miettinen H, Wirtanen G. Ecology of Listeria species in a fish farm and molecular typing of Listeria monocytogenes from fish farming and processing companies. Int J Food Microbiol. 2006;112(2):138–46.
Wieczorek K, Dmowska K, Osek J. Prevalence, characterization, and antimicrobial resistance of Listeria monocytogenes isolates from bovine hides and carcasses. Appl Environ Microbiol. 2012;78(6):2043–5. https://doi.org/10.1089/fpd.2012.1137.
Maktabi S, Pourmehdi M, Zarei M, Moalemian R. Occurrence and antibiotic resistance of Listeria monocytogenes in retail minced beef distributed in Ahvaz, South-West of Iran. J Food Qual Hazards Control 2015;2(3):101–6. http://jfqhc.ssu.ac.ir/article-1-84-en.html.
Gombas DE, Chen Y, Clavero RS, Scott VN. Survey of Listeria monocytogenes in ready-to-eat foods. J Food Prot. 2003;66(4):559–69. https://doi.org/10.4315/0362-028X-66.4.559.
Matereke LT, Okoh AI. Listeria monocytogenes virulence, antimicrobial resistance and environmental persistence: a review. Pathogens. 2020;9(7):528. https://doi.org/10.3390/pathogens9070528.
Jinneman K, Wekell M, Eklund M. Incidence and behaviour of L. monocytogenes in fish and seafood products. Listeria, listeriosis and food safety. Dekker, New York. 1999;601(1):629.
Kaszoni-Rückerl I, Mustedanagic A, Muri-Klinger S, Brugger K, Wagner K-H, Wagner M, et al. Predominance of distinct Listeria innocua and Listeria monocytogenes in recurrent contamination events at dairy processing facilities. 2020;8(2):234. https://doi.org/10.3390/microorganisms8020234.
Matthews KR, Kniel KE, Montville TJ. Food microbiology: an introduction.: John Wiley & Sons. doi:10 1128/9781555819392; 2017.
Kells J, Gilmour A. Incidence of Listeria monocytogenes in two milk processing environments, and assessment of Listeria monocytogenes blood agar for isolation. Int J Food Microbiol. 2004;91(2):167–74. https://doi.org/10.1016/S0168-1605(03)00378-7.
McDermott P, Zhao S, Wagner D, Simjee S, Walker R, White D. The food safety perspective of antibiotic resistance. Anim Biotechnol. 2002;13(1):71–84. https://doi.org/10.1081/ABIO-120005771.
Dalzini E, Bernini V, Bertasi B, Daminelli P, Losio M-N, Varisco G. Survey of prevalence and seasonal variability of Listeria monocytogenes in raw cow milk from Northern Italy. Food Control. 2016;60:466–70. https://doi.org/10.1016/j.foodcont.2015.08.019.
Mpundu P, Mbewe AR, Muma JB, Sitali GM, Mubita CM, Munyeme M. Comparison of Bacterial Cross-Contamination among Broiler Carcasses between Commercial and Non-Commercial Processed System and Its Public Health Implications. Open J Vet Med. 2021;11(01):1.
Cohen SS. Growth requirements of bacterial viruses. Bacteriol Rev. 1949;13(1):1 (PMCID: PMC440941).
Shamloo E, Hosseini H, Moghadam ZA, Larsen MH, Haslberger A, Alebouyeh M. Importance of Listeria monocytogenes in food safety: a review of its prevalence, detection, and antibiotic resistance. Iran J Vet Res. 2019;20(4):241 (PMCID: PMC6983307).
Singh K, Verma AK, Jaiswal AK, Sudan V, Dhama K. Journals Menu. https://doi.org/10.14737/journal.aavs/2014/2.4s.24.32.
Guo M, Dubey JP, Hill D, Buchanan RL, Gamble H, Jones JL, et al. Prevalence and risk factors for Toxoplasma gondii infection in meat animals and meat products destined for human consumption. 2015;78(2):457-76. https://doi.org/10.4315/0362-028X.JFP-14-328
Luber P. The Codex Alimentarius guidelines on the application of general principles of food hygiene to the control of Listeria monocytogenes in ready-to-eat foods. Food Control. 2011;22(9):1482–3. https://doi.org/10.1016/j.foodcont.2010.07.013.
Prendergast D, Daly D, Sheridan J, McDowell D, Blair I. The effect of abattoir design on aerial contamination levels and the relationship between aerial and carcass contamination levels in two Irish beef abattoirs. Food Microbiol. 2004;21(5):589–96. https://doi.org/10.1016/j.fm.2003.11.002.
Guthmann JP, Klovstad H, Boccia D, Hamid N, Pinoges L, Nizou JY, et al. A large outbreak of hepatitis E among a displaced population in Darfur, Sudan, 2004: the role of water treatment methods. 2006;42(12):1685-91. https://doi.org/10.1086/504321
Fasanmi O, Makinde G, Popoola M, Fasina O, Matere J, Ogundare S. Potential risk factors associated with carcass contamination in slaughterhouse operations and hygiene in Oyo state, Nigeria. Int J Livest Prod. 2018;9(8):211–20. https://doi.org/10.5897/IJLP2018.0491CorpusID:73628257.
Eruteya O, Odunfa S, Lahor J. Listeria species in raw cow and goat meat in Port Harcourt, Nigeria. Br Biotechnol J 2014:204–14. https://doi.org/10.9734/BBJ/2014/6750.
Wambui J, Lamuka P, Karuri E, Matofari J, Njage PMK. Microbial contamination level profiles attributed to contamination of beef carcasses, personnel, and equipment: case of small and medium enterprise slaughterhouses. J Food Prot. 2018;81(4):684–91. https://doi.org/10.4315/0362-028X.JFP-17-402.
Wardhana DK. Risk factors for bacterial contamination of bovine meat during slaughter in ten Indonesian abattoirs. Vet Med Int 2019;2019. https://doi.org/10.1155/2019/2707064.
Acknowledgements
The authors would like to express their sincere gratitudes to ACEIDHA, Higher Education Loans and Scholarships, Levy Mwanawasa Medical University and Department of Disease control at the school of Veterinary Medicine, for providing acess to research facilities and financial support.
Limitation and strength of the study
- The findings of this study will help the policymakers to come up with interventions that can be used to address Listeria contamination in beef carcasses.
- Additionally, this is the first study that has incorporated culture and phylogenetic analysis of Listeria in Zambia in traditionally reared cattle which may be used for academic purposes, including national planning.
- The study's limitations can mainly be drawn from the beef carcasses sampled from the abattoirs. The carcasses came from different farms, and environmental factors were not assessed at the farm level to ascertain the contamination. Therefore,conclusiveness was limited on the source of Listeria contamination, whether at the abattoir or farm level. Furthermore, the failure to isolate Listeria from the environment also limits the ability of this study to link the environment as a possible source of contamination.
- Similar species of Listeria were obtained from different abattoirs; however this similarity could also not be established because of lack of information on which farms the swabbed carcasses originated.
- The power of the study was partly affected by the number of isolates recovered in this current study which later had a bearing on the anticipated outcome. Inadequate sampling could have probably influenced this current results.
Funding
This research was funded by the Africa Center of Excellence for Infectious Diseases of Humans and Animals (ACEIDHA) (Grant no. 5803-ZM).
Author information
Authors and Affiliations
Contributions
P.M, P.K, A.N.M, N.M, M.M, J.B.M, B.M.H. initiated the study, conducting of field and laboratory work, W.M. did the bioinformatics. All authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any study with human particpants. For the animal data, samples were collected based on abattoir survey from already slaughtered carccases meant for human food. For this purpose, Ethical approval was obtained from Excellence in Research Ethics Committee (ERES) under reference no. (Ref.no.2020-Jan-006).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Figure 1. Multiple sequence alignment of downloaded reference sequences and sequences generated in this study. Multiple sequence alignment was performed using ClustalW1.6.
Additional file 2: Supplementary Table 1.
Description of samples collected from cattle in Namwala district in 2020.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mpundu, P., Muma, J.B., Mukumbuta, N. et al. Isolation, discrimination, and molecular detection of Listeria species from slaughtered cattle in Namwala District, Zambia. BMC Microbiol 22, 160 (2022). https://doi.org/10.1186/s12866-022-02570-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-022-02570-6