Abstract
Background
The scientific publications of antimicrobial susceptibilities and resistance must be precise, with interpretations adjusted to the standard. In this frame, knowledge of antimicrobial resistance is fundamental in pathogenic microorganisms such as Salmonella spp., known for many annual deaths worldwide. The objective of this work was to compare the interpretation of standards, the concentrations, and the breakpoints, to study antimicrobial resistance in Non-Typhoidal Salmonella (NTS) isolated from beef, pork, and chicken meat, meat products, and propose additional considerations that improve the use and usefulness of published results.
Results
After refining the search based on meeting the inclusion and exclusion criteria, 48 papers were selected. In 33 (68.8%) of them, the disc diffusion method was used, in 11 (22.9%) the MIC determination method, and in 4 (8.33%) were used both. In 24 (50%) of the articles, the selection of a different (correct) standard could have had an impact on the interpretation of antimicrobial susceptibility, which observed when considering three scenarios, i) comparison between the year of the isolation versus the implemented standard, ii) comparison between the year of submission versus implemented standard and iii) comparison between the year of publication versus implemented standard.
Conclusions
The most frequent scenario was the inadequate selection of standards, indicating that some studies had not ensured that applied standards kept in line with the date of isolation, date of publication and interpretation of susceptibilities. We proposed 2 years for standards use for resistance and multi-resistance interpretations. On the other hand, we invite researchers to publish their results in the shortest possible time, and editors and reviewers of scientific journals to prioritise these types of studies and verify the correspondence between the standard cited and the one used and the one to be taken into account.
Similar content being viewed by others
Antimicrobial agent | Abbreviations used in the papers | Abbreviations for this paper |
|---|---|---|
Penicillins | ||
Ampicillin | AM, AMP, A, Amp, Ap | AMP |
Ticarcilin | TIC, TC, TI, Ti | TIC |
β-Lactam/β-Lactamase inhibitor combinations | ||
Amoxicillin/clavulanate | AUG, AMC, Amc, AC | AMC |
Ampicillin-sulbactam | SAM, AS | SAM |
Piperacillin-tazobactam | PPC-TAZ, TZP | TZP |
Cephems | ||
Cefazolin | CFZ, KZ, CZ, CF, CZD | CFZ |
Cephalothin | CF, CEP, CEF, KF | CEP |
Cefepime | CPM, FEP | FEP |
Cefotaxime | CTX, TAX, CT | CTX |
Ceftriaxone | AXO, CRO, Co, CTR | CRO |
Cefoxitin | FOX | FOX |
Cefuroxime | FUR, CXM | CXM |
Ceftazidime | CAZ, CTZ, CF | CAZ |
Cefoperazone | CFP | CFP |
Cefaclor | CEC, CFC | CFC |
Cefpodoxime | CPD | CPD |
Monobactams | ||
Aztreonam | ATM, AZT, AM | ATM |
Ertapenem | ETP | ETP |
Imipenem | IPM, IMP, IMI | IMI |
Meropenem | MEM | MEM |
Aminoglycosides | ||
Gentamicin | GM, G, CN, GE, Gm, GN | GEN |
Tobramycin | TOB, To | TOB |
Amikacin | AMI, AM, AMK, AN, Ak | AMK |
Kanamycin | KAN, K | KAN |
Streptomycin | S, STR, SM, EST | STR |
Fluoroquinolones | ||
Ciprofloxacin | CIP, Cp, CI, CPF, CPX | CIP |
Levofloxacin | Lvx | Lvx |
Ofloxacin | OFX | OFX |
Norfloxacin | NOR | NOR |
Quinolones | ||
Nalidixic acid | NA, NAL, Nx, N | NAL |
Folate pathway inhibitors | ||
Trimethoprim-sulfamethoxazole | SXT, COT, ST, TMP – SLF, TS | SXT |
Sulfonamides | SSS, SMX, sul, SUL, SMX | SUL |
Trimethoprim | TMP, TRIM, TP, W | TMP |
Phenicols | ||
Chloramphenicol | C, CHL, CM, CLF, CLO, CRO | CHL |
Nitrofurans | ||
Nitrofurantoin | FT, NIT | NIT |
Tetracyclines | ||
Tetracycline | TE, TET, T, TCY | TET |
Background
Antimicrobial resistance monitoring programmes assess isolation of interest associated with foodborne diseases (FBD) against a range of antibiotics of importance in humans [1] to understand the dynamics of microorganisms in a community.
Among the national surveillance systems are the Canadian Integrated Program for Antimicrobial Resistance Surveillance (CIPARS), the National Antimicrobial Resistance Monitoring System (NARMS) since 1996 in the United States of America [2], and in Japan since 1999, the Japanese Veterinary Antimicrobial Resistance Monitoring System (JVARM) [3]. International systems include the European Antimicrobial Resistance Surveillance Network (EARSS, at present EARS-Net) funded in 1998 [4], and Latin America, the Latin American Antimicrobial Resistance Surveillance Network (ReLAVRA) since 1996 [5].
The known and approved methods for the assessment of antimicrobial susceptibility are the determination of the minimum inhibitory concentration (MIC) by dilution (broth micro- or macro dilution, or agar-dilution), the disc diffusion method (Kirby Bauer), and the MIC determination by epsilometric test (E-test) [6]. The first two methods recognised by CLSI (Clinical and Laboratory Standards Institute) and EUCAST (European Committee on Antimicrobial Susceptibility Testing) which are frequently updated the breakpoints and allow viewing and downloading of the latest editions [7].
At present, for epidemiological analysis of antimicrobial susceptibility tests, two types of criteria exist. The first the Food and Drug Administration (FDA) Epidemiological Cut-off Values (ECV). In this test, “the MIC value or zone diameter value separates microbial populations into those with and without acquired and or mutational resistance, based on their phenotypes (wild-type [WT] or non-wild-type [NWT]); the ECV defines the upper limit of susceptibility for the wild-type population of isolates” [8]. Second, The EUCAST Epidemiological Cut-off Values (ECOFF). In this test, “values separate the naive, susceptible wild-type bacterial populations from isolates that have developed reduced susceptibility to a given antimicrobial agent. The ECOFFs may differ from breakpoints used for clinical purposes, which are set out against a background of clinically relevant data, including therapeutic indication, clinical response data, dosing schedules, pharmacokinetics and pharmacodynamics” [9].
However, breakpoints, also known as clinical breakpoints, are specific parameter values, such as MIC or zone diameter value used, according to which isolation is clinically classified (interpretative criteria), such as “susceptible (S)”, “intermediate (I)” and “resistant (R)” [8, 10].
Salmonella spp. is recognised as one of the most important pathogens causing FBD [11]. Non-typhoidal Salmonella serovars (NTS) cause gastroenteritis in various hosts [12], including human bacteraemia [13]. One of the transmission routes of NTS is the consumption of contaminated food [7, 11, 14, 15] as fresh meat and eggs [14]. The main transmission route involves the evisceration and intestinal contents removal, where occurs cross-contamination [16,17,18,19]. This scenario becomes more complicated due to microorganism biofilms formation [14]. Of course, much care is necessary for the remaining stages of production: processing, distribution, sale and handling, to avoid the spread of the microorganism [18].
One big problem with pathogens causing FBD is antimicrobial resistance. In 2019, EFSA reported 87,923 cases of salmonellosis as the most frequent cause of FBD. The entity reported that 25.4% of the human isolates were MDR (multidrug-resistant) [9]. In addition, risk estimation data for 2019 in NARMS “Antibiotic Resistance Threats 2019” describes 212,500 annual cases of antibiotic-resistant non-typhoidal Salmonella infections and 70 deaths annually [20].
Among the factors that have influenced the emergence of antimicrobial resistance is the indiscriminate use of human antibiotics in livestock farming. It has been estimated in some countries that almost 50% of the antimicrobials produced worldwide are for livestock activities as prophylactics, growth promoters and in the treatment of diseases [18, 21, 22]. For example, Australia import about 700 tons each year and about 500 tons (78%) are used [22] in livestock activities. All this justifies the importance of monitoring and controlling the use of antibiotics.
In the USA, the Food and Drug Administration (FDA) and the Center for Veterinary Medicine (CVM) control the use of antimicrobials. However, the USA has approved 17 antimicrobials classes as growth promoters for animals. It includes tetracyclines, macrolides and penicillins [22].
In the light of the above, the present review intended to analyze and compare the interpretation of standards, the concentrations of antimicrobials used in each study, and the breakpoints, to study antimicrobial resistance in Non-Typhoidal Salmonella (NTS) isolated from beef, pork, and chicken meat and meat products, and to improve by proposals the use and usefulness of published results.
Materials and methods
Search strategy
The article searches were conducted in Web of Science (WoS), SCOPUS, Science Direct, and JSTOR. Regional documents searched in “Biblioteca Virtual de Salud (BVS)” and PubMed. Search equations used were based on the interaction of three groups: The first included Salmonella / zoonotic Salmonella / foodborne pathogen/ Salmonella; the second antimicrobial resistance, antibiotic resistance/ multidrug resistance, and the third meat products/ meat poultry/ pork/ beef, employing the Boolean operator “AND”.
For BVS and PubMed, the following browsers were used Descriptors in Health Sciences (DECS) and Medical subject headings (MESH), respectively, to perform searches for the terms as dependent variables: Salmonella food poisoning/“intoxicación alimentaria por Salmonella and Salmonella enterica”. Among independent variables associated with resistance drug resistance were employed microbial/“farmacorresistencia microbiana”, and Microbial sensitivity tests/“pruebas de sensibilidad microbiana”.
For the search associated with meat and meat products the terms used were: meat products/“productos de carne”, meat product/“producto de carne”, poultry products/“productos avícolas”, food safety/“análisis de peligros y puntos de control críticos, inocuidad de los alimentos”, food contamination/“contaminación de alimentos”, foodborne diseases/“enfermedades transmitidas por los alimentos”, fast foods/“comidas rápidas” and raw foods/“alimentos crudos”.
Inclusion and exclusion criteria
Only included experimental studies performed between 1996 and 2019, covering the year that international observation and monitoring of antimicrobial resistance programs initiated. English and Spanish were the languages selected for articles, as described in the search equation. In the articles selected, the samples were meat or meat products collected at points of sale or intended for the same purpose and should identify Salmonella spp. and the non-typhoid serotype.
Selected articles were separated into two groups, the disc diffusion and minimal inhibitory concentration (MIC), to compare them. Likewise, was carrying out the verification of breakpoints and references for each of them (national or international). Articles that explicitly showed interpretative criteria or resistance frequency by isolate were selected.
Were excluded those articles whose title and abstract were unrelated to the present study. Articles involving isolations from collections were excluded due to lack of clarity on sample types, years of isolation or origin, such as food outbreak studies, as it was difficult to know the Salmonella spp., contamination source.
Extraction and data registry
The information extracted was the following, the country of the study, the type of meat or meat product, the method used (disc diffusion or MIC determination), the breakpoints, the standard used and the regime applied (national or international) and antimicrobial susceptibility results.
Families of antibiotics considered belong to the following classes: Penicillin, β-lactam/β-lactamase inhibitor combinations, cephems, monobactams, aminoglycosides, quinolones, fluoroquinolones, folate pathway inhibitors, phenols, nitrofurans, and tetracyclines.
Data analysis
Data analysis focused on three different facts: first, recognition of antimicrobial susceptibility test used, and national or international standard employed. Second, articles classified according to the method used disc diffusion or MIC determination for each group. Antibiotic concentration and breakpoints compared for each study. Additionally, the association between the date of submission, date of publication, and the year of the isolates versus the CLSI standard implemented. Third, was investigated the multi-resistance patterns and the percentage of prevalence according to serotype, taking into account the method described in each study.
Also suggested an optimal period of 2 years for the appropriate CLSI standard use, considering that the CLSI annually updates the M100 standards and includes a “tentative” period of 1 year for the manufacturer to implement the standard modifications. Additionally, we suggest that the peer review processes and the publication of antimicrobial resistance studies should not take more than 1 year, which would add up to the 2 years for the optimal period that we are proposing for standards use.
On the other hand, some studies have used the standard for the antimicrobial susceptibility evaluation of isolates from animal origin. M31 standard version was modified in 2013 and replaced by the VET01-S3 (2013). Subsequently, since June 2018, VET 01–04 (2018) changed into the VET08. Therefore, it is necessary to emphasize that to maintain the original information from the selected articles, in this work, the standard used was as it was published (M31) by authors.
Results
Number of articles, countries, and standard
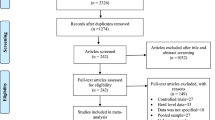
A total of 3802 articles were related to the topic, 1141 (30%) were preselected, and only 4% (48/1141) met all the defined inclusion and exclusion criteria (Tables 1 and 2).
When separating the articles according to the standard used to determine the susceptibility of the isolation, based on the breakpoints, we found that: 45/48 (93.8%) used the CLSI standards, 1/48 (2.08%) the NARMS or CIPARS standards, and 1/48 (2.08%) by Comité de l’antibiogramme de la société française de microbiologie (CA-SFM), and the European Committee on Antimicrobial Susceptibility Testing – EUCAST (Table 2).
Additionally, of the articles that used CLSI standards, 82.2% (37/45) used the M100, 7/45 (15.6%) used the M31 corresponding to disc diffusion and dilution susceptibility, and 1/45 (2.2%) used both standards [29] (Table 2).
Analysis of antibiotic concentration used according to each method
Disc diffusion method
The disc diffusion method grouped the highest number of articles with 68.8% (33/48). The studies that implemented the disc diffusion method used the same concentration (30 μg) in Cephems (CFZ, CEP, FEP, CTX, CRO, FOX, CXM, and CFP), in Monobactams (ATM), in Quinolone (NAL), and Phenolic Compounds (CHL). While in Aminoglycosides (TOB 10 μg and AMK 30 μg) and Fluoroquinolones (OFX 5 μg). However, for each GEN, SXT, SUL, AMP, CAZ, IMI, STR, TMP, AMC, CFP, SAM, CIP, KAN, NOR, CPD, three different situations were observed:
-
1.
In Zdragas et al. (2012), for CFP (cephems), the concentration cited was 30 μg, yet in the CLSI, M31-A3 (referred standard), the antibiotic is not included.
-
2.
Among the revised articles, the most occurring non-conformance to the standards was a discrepancy between the concentration used in the study and the one referenced.
-
a.
In Bada-Alambedji, et al. (2006), SXT (1.25–23.75 μg) concentration coincided between the Distributor (Bio-Rad) and the C.A.-S.F.M standard used. However, the antimicrobial concentration reported in the article was 1.25–25.75 μg.
-
b.
In Dallal et al. (2010), AMP (10 μg), CAZ (30 μg), IMI (10 μg), STR (10 μg), TMP (5 μg), AMC (20/10 μg), TET (30 μg) concentrations were similar between the Distributor (Mast Diagnostics) and those presented in the CLSI M100-S16, 2006 and CLSI M 100-S13 standard. However, those reported in the article differed from CLSI M100-S16, 2006 and CLSI M 100-S13 standard for AMP (30 μg), CAZ (100 μg), IMI (30 μg), STR (15 μg), TMP (15 μg), AMC (75/10 μg), TET (15 μg).
-
c.
In Molina et al., (2010), the concentration reported for AMC in the CLSI, M100-S19 standard and the distributor’s insert (BBL) was 20/10 μg. However, the antimicrobial concentration reported in the article was 75/10 μg.
-
d.
Cabrera-Díaz et al., (2013), used a concentration of 30 μg for CIP. However, the BBL, BD, Sparks, MD companies and the CLSI M100-S18 standard specify the use of discs containing 5 μg CIP.
-
e.
In Moawad et al., (2017), the concentration used for AMC and CPD was 20 μg, but that described by Oxoid and the CLSI, M100-S21 standard was of 20/10 μg and 10 μg, respectively.
-
f.
In Zhang et al., (2018), the concentration used for FEP was 5 μg, but the one described by the CLSI, M100:S23 standard references, and Oxoid (distributor) was 30 μg.
-
g.
In Aihua Zhu et al., (2019), NOR concentration described in the article was 5 μg, but the disc content defined by the CLSI, M100: S23 standard and Oxoid (distributor) was 10 μg.
-
a.
-
3.
Discrepancies were between the disc content reported in the article and the one defined by the standard used. These articles not mentioned discs distributor.
-
a.
In Kim et al. (2011), SAM is reported concentration was 30 μg, yet the one established by the cited standard (CLSI, M100-S21) was 10/10 μg.
-
b.
In Li et al., (2014), for KAN and NOR, they reported 20 and 5 μg, respectively. However, those reported by the cited CLSI, M100-S21 standard were 30 and 10 μg, respectively.
-
c.
In Cai et al., (2016), they reported a concentration of 5 μg for NOR, and that defined by the cited CLSI, M100-S23 standard was 10 μg.
-
a.
MIC method
22.9% of the articles implemented MIC method (11/48), and 8.3% (4/48) used MIC and Disk Diffusion (Table 2). In articles to MIC determination, in 7/15 (46.6%) of them, the test range were not indicated [32, 37, 43, 69, 72, 74, 84]. Information regarding the remaining seven articles appears in Table S1.
Breakpoints and interpretative criteria for MIC
When comparing the breakpoints for Salmonella spp., by the two methodologies, using the CLSI standards, in general terms, we observed that there was a variation between 2010 and 2019 for Monobactams, Cephems, Fluoroquinolones, and Tetracyclines. These changes started from the M100-S20 standard on (Tables S2A and B). However, some situations became evident concerning MIC determination:
-
A.
In the group of the articles using MIC determination, 4/11 (36.4%) [40, 43, 66, 72] implemented the CLSI, M31 standard. These works employed CTX, CRO, FOX, CAZ, ATM, STR, CIP, NAL, TMP, NIT that are not in the standard (Table S3). Therefore, the breakpoints used in the interpretation of susceptibility tests are unknown.
-
B.
In the four articles (Table 2), where isolates were analyzed by MIC determination and disc diffusion methods and evaluate the antimicrobial resistance and β-lactamases production; the breakpoints for AMP, AMC, TZP, FEP, FOX, GEN, AMK, and SXT were like those described in CLSI, M100-S19, M100-S22, and M100-S23. In these standards, breakpoints for the antibiotics did not vary in 2009, 2012 and 2013 (Tables S2 A and B).
Comparison among isolation collection date, date of manuscript submission, date of publication, and implemented CLSI standard
To evaluate the association between the implemented CLSI M100 standard for 37/48 (77.1%) of the studies and their possible scenario, the standard used were associated with the date of isolation, date of manuscript submission, and publication date. We observed that:
First scenario: comparison between the year of the isolation and the standard applied
A comparison of 26/37 (70.3%) of the articles appears in Additional file 2. In 5/37 (13.5%) was not described the isolation date. In 6/37 (16.2%), the isolates were collected in different years and included in the same study.
The articles using the CLSI standard within the optimal considered period were 16/26 (61.5%). According to our proposed period, in 4/26 (15.4%) of the studies, the standards were wrong since they were 2–8 years outdated concerning the optimal period.
Second scenario: comparison between the year of submission of the article versus implemented standard
The analysis of the year of submission versus the used standard included only 29/37 articles (78.4%), as no description of date of submission appear for 8/37 (21.6%) articles.
In Additional file 2, 15/29 (51.7%) studies were among the optimal range. Of these, the study published by Molina et al., (2010), in our criteria, used the correct standard CLSI, M100-S19 (2009). However, from the following year onwards, breakpoints modifications appear in the CLSI standard, M100-S20 (2010), (Tables S3A and B), [31]; however, were not considered in the article.
Third scenario: comparison between the year of publication versus implemented standard
When the 37 articles using the M100 standard compared, we observed 13/37 (35%) of the studies state in range with the standards. In contrast, 24/37 (65%) of the studies did not use adequate ones concerning the year of publication. Yet, it is necessary to consider publishing processes are usually lengthy (Additional file 2).
Studies where the use of the suggested standards could have an impact
The total number of studies where the correct standard use could impact was 24 (50%). Concerning this, different scenarios appear below.
First scenario. According to our criteria, in 4/26 (15.4%) publications, the standard used was inadequate since the implemented standard was 2–8 years outdated concerning the optimal period. On the other hand, 6/26 (23.1%) of the articles use a standard closer to the submission date rather than the isolation date. As a case in point, Gad et al., (2018) obtained their isolated in 2009, the CLSI standard used was M100-S21 (2011) and the manuscript submitted in 2018 (Table 3).
Second scenario. According to our criteria, 14/29 articles (48.3%) implemented an inadequate standard, as they were outside the range considered optimal. Moreover, in 13 studies, the interpretation of the results could change according to the breakpoints used (Table 3).
Third scenario. According to our criteria, 24/37 (65%) of the studies did not use the adequate standard concerning the year of publication. Yet it is necessary to take into account publishing processes are usually lengthy (Table 3).
Table 3 contains the 24 references, where using a different standard could have had an impact. Besides, we specify 56 cases where the interpretation may have been other than the published one. In 2/24 (8.3%) of studies, utilization of the suggested standard would not have caused a change in the interpretation of antimicrobial susceptibility because antibiotics used did not change (comparing the standard applied and the suggested one) (Table 3).
In 10/24 studies (41.6%), when analysing the antibiotics described and comparing them with the suggested norms within the optimal period, it was observed that there were no breakpoint values for STR, OFX, Lvx, NOR, CEP, and NAL (Table 3). By 2006 in M100-S16 says for STR that “aminoglycosides may appear active in vitro, but are not clinically effective and should not be reported, as susceptible”. M100-S23 says that re-evaluation of fluoroquinolones OFX and Lvx was ongoing. In M100-S26, antimicrobials such as NOR, CEP, and M100-S27, antimicrobials as NAL ceased to assayed for Salmonella spp.
During the study, we found 56 cases of antibiotics with possible changes in the susceptibility interpretation. In 2 (3.6%) cases, there was no impact. In other 2 (3.6%) cases, the suggested standard had different values in Moawad et al., (2017) for AMP, AMC, and SXT or lower/ higher values in Fakhr et al., (2006) for GEN, KAN, SXT, and SUL. In 17 (30.3%) cases, breakpoints were no found in the suggested standard. In 8 (14. 3%) cases, the interpretation could have changed from I to S or from R to I by applying the suggested standard. For 27 (48.2%) cases, the interpretive criteria could have changed from S to I or from I to R, once implemented the appropriate standards (Table 3).
Discussion
Antibiotic concentration analysis according to each method used
The most frequently used method in the articles was disc diffusion. However, MIC determination is the most recommended in monitoring programmes because quantitative tests are more accurate [89, 90], although disc diffusion tests are easier to perform and cheaper [89, 90].
Upon comparison, in both methods (Table 2), the antimicrobial agent concentration varied depending on the system, the distributor, and the methodology (as expected). 8.3% of the remaining articles used both techniques in a combined manner to complement antimicrobial susceptibility tests and to detect ß-lactamases in food, a logic strategy in many studies. However, in some studies [25, 34, 37, 52, 73, 81, 83, 87, 91], used antibiotic concentration in disc diffusion assays were different than the described in the standard referenced by those authors, suggesting the antimicrobial susceptibility interpretation (resistant, intermediate, or susceptible) lacks or lost the support of the breakpoints described in the standard.
Comparison of breakpoints and interpretative criteria for antimicrobial susceptibility tests
In 2017 the WHO, FAO, and the World Organization for Animal Health designed a guide for integrated surveillance of antimicrobial resistance in pathogenic bacteria responsible for foodborne diseases. This guideline establishes the antimicrobial surveillance perform of the clinical samples collected in livestock production from animal and environmental samples and in the finished product (food of animal origin) distributed in the retail trade (this being the most frequent route of human contamination). Also, the guideline mentions efforts to harmonise the interpretive criteria for antimicrobial susceptibility testing to get comparable data [92].
Usage of standards for both MIC-determination and disc diffusion methods and the inter and intra-laboratory quality control systems should lead to reproducible results [93]. Hence, the importance of complying with test specifications, quality control management, and updated standard version.
It is crucial to know that CLSI established breakpoints depending on the behaviour of pathogens worldwide, varying as a function of study and analysis by an international committee of experts. CLSI M100 changed breakpoints and interpretative criteria for Penicillins, Cephems, Monobactams, Fluoroquinolones, and Tetracyclines between 2006 and 2019 (Tables S3 A and B). The crucial change observed from the CLSI M100-S20 onwards was for the Cephems. This information is critical because an inadequate standard use; could result in over or underestimation of identified resistances.
On the other hand, in the articles [40, 43, 66, 72], the CLSI standard M31 was referred for defining the breakpoints of CTX, CRO, FOX, CAZ, ATM, STR, CIP, NAL, TMP, NIT; which are not in M31.
Comparison between isolate collection, article submission, and publication with the implemented CLSI standard
In the development of antimicrobial susceptibility tests, the laboratory is responsible for using the current CLSI standard or the standard to be implemented, and rigorously follow the system’s instructions by the manufacturer, as well as a strict adhesion to the established procedure to accordingly classify the isolate as susceptible, intermediate or resistant [94].
Table 3 shows 24 studies where the standard used did not coincide with the suggested and microbial susceptibility interpretation. From these, 8.3% (2/24) did not impact the results since the antimicrobials employed did not have breakpoints modifications for the proposed standard versus the implemented one. 11/24 (45.8%) of the impact of the articles was on the susceptibility interpretation to cephems. 7/24 (29.2%) articles impact was on the tetracyclines susceptibility interpretation. In 2/24 (8.3%) articles involve the susceptibility interpretation to folate pathway inhibitors. 1/24 (4.2%) articles impacted on the susceptibility interpretation to aminoglycosides.
Additionally, in the article by Yu et al., (2014) if using of suggested M100-S21, −S22, −S23, −S24 standards, “intermediate” isolate interpretation for ATM could change to “susceptible”. However, the study does not report intermediate isolates. On the other hand, in the article by Sodagari et al., (2015), all isolates were reported as susceptible to IMI; yet this interpretation can change as resistant if any of the M100-S22, −S23, −S24 standard would have implemented, as suggested in the optimal period proposed.
Studies by Cabrera-Diaz et al., (2013), Abd-Elghany et al., (2015), Yu et al., (2014), Sodagari et al., (2015), Gharieb et al., (2015) used CIP within the antimicrobial susceptibility tests. When analysed the susceptibility of isolates to CIP by using M100-S18, −S11, −S16, −S15 and -S20 standards (used by the authors) and M100-S22, −S23, −S24 and -S25 (suggested standards); the interpretation changed from susceptible to intermediate and from intermediate to resistant.
According to Jorgensen & Turnidge (2015), the clinic isolates classified as “intermediate” can be inhibited by non-toxic attainable antimicrobial concentration if the dosage is high or administration prolonged. Antimicrobials also can be safely used when the infection is in a site where the medication can remain physiologically concentrated (for example, the urinary tract).
Additionally, antimicrobials with “intermediate” results also can be used as a buffer zone in the interpretation, avoiding minor mistakes in technical factors causing discrepancies in antimicrobial susceptibility interpretation. For example, from “susceptible to intermediate” instead of from “susceptible to resistant” [92, 95], where the modification from “susceptible” to “intermediate” would not have an impact, as other interpretative mistakes would.
In contrast, when the isolate is mistakenly reported as “susceptible” when it is “resistant”, it is a big problem. In humans, S. Typhimurium isolates resistant to antimicrobials have been associated with an increased risk of infection, frequent hospitalization, disease, and risk of death, in contrast to susceptible S. Typhimurium isolates. Therefore, accurate, rapid, cost-effective classification of multi-resistant isolates is necessary for illness management [96].
The finding of food antimicrobial-resistant isolates, especially from livestock productions and production environments, have a human health impact due to the responsibility for the failure of human treatments and the capacity to generate disease. Additionally, in some studies, authors have described the spread of resistance genes through isolates obtained from food and environments to the intestinal microbiota [97, 98]. Hence, the importance of correct classification in antimicrobial susceptibility test as a source of information for antimicrobial resistance surveillance programs. However, in certain versions of CLSI standards supplements, the underlying method may change. Hence, the need for prior verification before using an updated version of the standards.
Antimicrobial resistance may be natural and evolutionary; however, the imprudent use of antimicrobials has accelerated it. In this regard, some authors predicted that by 2050 there could be close to 10 million deaths due to infections caused by antimicrobial-resistant microorganisms, a clinical situation that could be worst because of COVID 19 [99, 100].
Therefore, studies assessing antimicrobial resistance must be rigorous and describe aspects such as those highlighted by Van et al., (2007): sampling procedures, sample type, identification methods and selection of the appropriate standard, among others, as described in this review.
Conclusions
According to our criteria, the inappropriate standard selection was the most frequent scenario (date of publication vs standard implemented). We remark the necessity to review the standards employing, to assure they are in line with the isolation and publication dates, demonstrating whether there could be interpretations changes.
This systematic review proposed an optimal period of 2 years in the standard to use for multi-resistance interpretation to be homogenous since multiresistant isolates are the most virulent. Thus, they are known as “superbugs” [101]. In this regard, we call on researchers to publish their antimicrobial susceptibility results in the shortest time possible. For longitudinal retrospective studies, it is crucial to use the correct and current standard, according to isolation date, making the necessary clarifications.
We also suggest to editors and scientific journal reviewers to prioritize these types of studies. Besides, verify the correspondence between the cited standard and the one that should employ, knowing that international standards are usually updated every year. This systematic review also suggests that other publications regarding antimicrobial resistance of some other pathogenic microorganisms could be presenting the same discrepancies we describe.
Finally, we propose the generation of an international, codified and easily accessible database where researchers can record the results of antimicrobial susceptibility testing of isolates from different links in the production chain. This database should include the date and origin of the isolates, their identification, the methodology used and the standard used. It would also be interesting if the database could automatically process the results. It is clear that the database proposal is ambitious, but it would allow for better collaborative work on antimicrobial resistance trends.
Availability of data and materials
The results and data are mostly presented in the document and in the supplementary material; however, they are available upon request.
References
Silley P, de Jong A, Simjee S, Thomas V. Harmonisation of resistance monitoring programmes in veterinary medicine: an urgent need in the EU? Int J Antimicrob Agents. 2011;37(6):504–12. https://doi.org/10.1016/j.ijantimicag.2010.12.002.
Zhao S, Mcdermott PF, Friedman S, Abbott J, et al. Antimicrobial resistance and genetic relatedness among Salmonella from retail foods of animal origin: NARMS retail meat surveillance. Fooborne Pathogens Dis. 2006;3(1):106–17. https://doi.org/10.1089/fpd.2006.3.106.
Asai T, Esaki H, Kojima A, Ishihara K, Tamura Y, Takahashi T. Antimicrobial resistance in Salmonella isolates from apparently healththy food-producing animal from 2000 to 2003: the fistr stage of Japanese veterinary antimicrobial Resitance Monitorin (JVARM). J Vet Med Sci. 2006;68(8):881–4. https://doi.org/10.1292/jvms.68.881.
Bronzwaer SLAM, Goettsch W, Olsson-Liljequist B, Wale MCJ, Vatopoulos A, Sprenger MJW. European antimicrobial resistance surveillance system (EARSS): objectives and organisation. Eur J Infect Dis Surveil Epidemiol Prevent Contr. 1999;4(4):41–4.
Schmunis G, Salvatierra GR. Birth of a public surveillance system: PAHO combats the spread of antimicrobial resistance in Latin America. APUA Newslett. 2006;24(1):6–11.
Kiska DL. In vitro testing of antimicrobial agents. Semin Pediatr Infect Dis. 1998;9(4):281–91. https://doi.org/10.1016/S1045-1870(98)80017-4.
de Jong A, Bywater R, Butty P, Deroover E, Godinho K, Klein U, et al. A pan-European survey of antimicrobial susceptibility towards human-use antimicrobial drugs among zoonotic and commensal enteric bacteria isolated from healthy food-producing animals. J Antimicrob Chemother. 2009;63:733–44. https://doi.org/10.1093/jac/dkp012.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S28), vol. 38; 2018. p. 296.
European Food Safety Authority (EFSA), European Centre for Disease Prevention and Control (ECDC). The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2018/2019. EFSA J. 2021;19(4):6490. https://doi.org/10.2903/j.efsa.2021.6490.
International Standardizartion Organization. Susceptibility testing of infectious agents and evaluation of performance of antimicrobial susceptibility test devices — Part 1. In: Broth micro-dilution reference method for testing the in vitro activity of antimicrobial agents against rapidly growing aerobic bacteria involved in infectious diseases (ISO 20776-1). Geneva; 2019.
Sánchez-Vargas FM, Abu-El-Haija MA, Gómez-Duarte OG. Salmonella infections: An update on epidemiology,management, and prevention. Travel Med Infect Dis. 2011;9:263–77. https://doi.org/10.1016/j.tmaid.2011.11.001.
Achtman M, Wain J, Weill F-X, Nair S, Zhou Z, Sangal V, et al. Multilocus Sequence Typing as a Replacement for Serotyping in Salmonella enterica. Plos Pathogens. 2012;8(6):e1002776. https://doi.org/10.1371/journal.ppat.1002776.
Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of invasive salmonella infections. Clin Microbil Rev. 2015;28(4):901–37. https://doi.org/10.1128/CMR.00002-15.
Löfström C, Hansen T, Maurischat S, Malorny B. Salmonella: Salmonellosis. In: Caballero B, Finglas P, Toldra F, editors. Encyclopedia of Food and Health: Elsevier Inc.; 2015. p. 701–5.
Antunes P, Mourão J, Campos J, Peixe L. Salmonellosis: the role of poultry meat. Clin Microbiol Infect. 2016;22(2):110–21. https://doi.org/10.1016/j.cmi.2015.12.004.
Abd-Elghany SM, Sallam KI, Abd-Elkhalek A, Tamura T. Occurrence, genetic characterization and antimicrobial resistance of Salmonella isolated from chicken meat and giblets. Epidemiol Infect. 2015;143(5):997–1003. https://doi.org/10.1017/S0950268814001708.
Sallam KI, Mohammed MA, Hassan MA, Tamura T. Prevalence, molecular identification and antimicrobial resistance profile of Salmonella serovars isolated from retail beef products in Mansoura, Egypt. Food Contr. 2014;38:209–14. https://doi.org/10.1016/j.foodcont.2013.10.027.
Doménech E, Jiménez-Belenguer A, Pérez R, Ferrús MA, Escriche I. Risk characterization of antimicrobial resistance of Salmonella in meat products. Food Contr. 2015;57:18–23. https://doi.org/10.1016/j.foodcont.2015.04.001.
Nguyen DTA, Kanki M, Nguyen PD, Le HT, Ngo PT, Tran DNM, et al. Prevalence, antibiotic resistance, and extended-spectrum and AmpC β-lactamase productivity of Salmonella isolates from raw meat and seafood samples in Ho Chi Minh City, Vietnam. Int J Food Microbiol. 2016;236:115–22. https://doi.org/10.1016/j.ijfoodmicro.2016.07.017.
Center for Disease Control and Preventión (CDC). Antibiotic Resistance Threats in the United States, 2019 (2019 AR Threats Report). Atlanta; 2019. p. 150.
Chuanchuen R, Ajariyakhajorn K, Koowatananukul C, Wannaprasat W, Khemtong S, Samngamnim S. Antimicrobial Resistance and Virulence Genes in Salmonella enterica Isolates from Dairy Cows. Foodborn Pathogens Dis. 2010;7(1):63–69. https://doi.org/10.1089/fpd.2009.0341.
Ukuhor HO. The interrelationships between antimicrobial resistance, COVID-19, past, and future pandemics. J Infect Public Health. 2021;14(1):53–60. https://doi.org/10.1016/j.jiph.2020.10.018.
Fakhr MK, Sherwood JS, Thorsness J, Logue CM. Molecular characterization and antibiotic resistance profiling of Salmonella isolated from retail Turkey meat products. Fooborne Pathogens Dis. 2006;3(4):366–74. https://doi.org/10.1089/fpd.2006.3.366.
National Committee for Clinical Laboratory Standards: Performance standards for antimicrobial susceptibility testing (NCCLS M100-S11). 2000.
Bada-Alambedji R, Fofana A, Seydi M, Akakpo AJ. Antimicrobial resistance of Salmonella isolated from poultry carcasses in Dakar (Senegal). Braz J Microbiol. 2006;37(4):510–5. https://doi.org/10.1590/S1517-83822006000400020.
Comité de l’Antibiogramme de la Société Française de Microbiologie C. Communiqué 1997. In: Pathologie Biologie, vol. 45. Paris: Société Française de Microbiologie; 1997.
Valdezate S, Arroyo M, González-Sanz R, Ramíro R, Herrera-León Ç, Usera MA, et al. Antimicrobial resistance and Phage and molecular typing of salmonella strains isolated from food for human consumption in Spain. J Food Protect. 2007;70(12):2741–8. https://doi.org/10.4315/0362-028X-70.12.2741.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing (M100-S15), vol. 25; 2005. p. 172.
Van TTH, Moutafis G, Istivan T, Tran LT, Coloe PJ. Detection of Salmonella SPP. in retail raw food samples from vietnam and characterization of their antibiotic resistance. Appl Envinron Microbiol. 2007;73(21):6885–90. https://doi.org/10.1128/AEM.00972-07.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals (NCCLS M31-A2), vol. 22; 2002. p. 80.
Murmann L, dos Santos MC, Cardoso M. Prevalence, genetic characterization and antimicrobial resistance of Salmonella isolated from fresh pork sausages in Porto Alegre, Brazil. Food Contr. 2009;20:191–5. https://doi.org/10.1016/j.foodcont.2008.04.007.
Cook A, Reid-Smith R, Irwin R, Mcewen SA, Valdivieso-Garcia A, Ribble C. Antimicrobial resistance in campylobacter, Salmonella, and Escherichia coli isolated from retail Turkey meat from southern Ontario, Canada. J Food Protect. 2009;72(3):473–81. https://doi.org/10.4315/0362-028X-72.3.473.
Public Health Agency of Canada. Canadian Integrated Program for Antimicrobial Resistance Surveillance (CIPARS) 2003 report. Guelph: Public Health Agency of Canada; 2005.
Soltan Dallal MM, Doyle MP, Rezadehbashi M, Dabiri H, Sanaei M, Modarresi S, et al. Prevalence and antimicrobial resistance profiles of Salmonella serotypes, Campylobacter and Yersinia spp. isolated from retail chicken and beef, Tehran, Iran. Food Contr. 2010;21:388–92. https://doi.org/10.1016/j.foodcont.2009.06.001.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing (CLSI M100-S16), vol. 26; 2006. p. 188.
National Committee for Clinical Laboratory Standards: Performance standards for antimicrobial susceptibility testing (NCCLS M100-S13). 2003.
Molina N, Millán B, Araque M. Indicadores de calidad sanitaria y fenotipificación de Salmonella enterica aislada de pollo crudo comercializado en el área urbana de Mérida, Venezuela. Revista Infectio. 2010;14(3):174–85.
Clinical and Laboratory Standards Institute. Performance Standards for antimicrobial Susceptibility Testing (CLSI M100-S19), vol. 29; 2009.
Sirichote P, Bangtrakulnonth A, Tianmanee K, Unahalekhaka A, Oulai A, Chittaphithakchai P, et al. Serotypes and antimicrobial resistance of Salmonella enterica ssp in Central Thailand, 2001-2006. Southeast Asian J Trop Med Public Health. 2010;41(6):1405–15.
MIkanatha NM, Sandt CH, Localio AR, Tewari D, Rankin SC, Whichard JM, et al. Multidrug-resistant salmonella isolates from retail chicken meat compared with human clinical isolates. Fooborne Pathogens Dis. 2010;7(8):929–34. https://doi.org/10.1089/fpd.2009.0499.
Hyeon J-Y, Chon J-W, Hwang I-G, Kwak H-S, Kim M-S, Kim S-K, et al. Prevalence, antibiotic resistance, and molecular characterization of salmonella serovars in retail meat products. J Food Protect. 2011;74(1):161–6. https://doi.org/10.4315/0362-028X.JFP-10-327.
National Committee for Clinical Laboratory Standards. Performance Standards for Antimicrobial Susceptibility Testing (NCCLS M100-S9), vol. 39. 29th ed: National Committee for Clinical Laboratory Standards; 1999. p. 320.
Nunes Medeiros MA, Nunes de Oliveira DC, Rodrigues DP, Coradi de Freitas DR. Prevalence and antimicrobial resistance of Salmonella in chicken carcasses at retail in 15 Brazilian cities. Rev Panam Salud Publica. 2011;30(6):555–60. https://doi.org/10.1590/S1020-49892011001200010.
Aslam M, Checkley S, Avery B, Chalmers G, Bohaychuk V, Gensler G, et al. Phenotypic and genetic characterization of antimicrobial resistance in Salmonella serovars isolated from retail meats in Alberta, Canada. Food Microbiol. 2012;32:110–7. https://doi.org/10.1016/j.fm.2012.04.017.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S20), vol. 37; 2010. p. 160.
Thai TH, Lan NT, Hirai T, Yamaguchi R. Antimicrobial Resistance in Salmonella Serovars Isolated from Meat Shops at the Markets in North Vietnam. Foodborne Pathogen Dis. 2012;9(11):986–91. https://doi.org/10.1089/fpd.2011.1121.
Kim M-S, Lim T-H, Jang J-H, Lee D-H, Kim B-Y, Kwon J-H, et al. Prevalence and antimicrobial resistance of Salmonella species isolated from chicken meats produced by different integrated broiler operations in Korea. Poultry Sci. 2012;91:2370–5. https://doi.org/10.3382/ps.2012-02357.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S21), vol. 30; 2011. p. 172.
Zdragas A, Mazaraki K, Vafeas G, Giantzi V, Papadopoulos T, Ekateriniadou L. Prevalence, seasonal occurrence and antimicrobial resistance of Salmonella in poultry retail products in Greece. Lett Appl Microbiol. 2012;55(4):308–13. https://doi.org/10.1111/j.1472-765X.2012.03298.x.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial disk and dilution susceptibilitytests for bacteria isolated from animals (CLSI M31-A3), vol. 22. 3rd ed; 2008. p. 116.
Álvarez-Fernández E, Alonso-Calleja C, García-Fernández C, Capita R. Prevalence and antimicrobial resistance of Salmonella serotypes isolated from poultry in Spain: Comparison between 1993 and 2006. Int J Food Microbiol. 2012;153:281–7. https://doi.org/10.1016/j.ijfoodmicro.2011.11.011.
Cabrera-Diaz E, Barbosa-Cardenas CM, Perez-Montaño JA, Gonzalez-Aguilar D, Pacheco-Gallardo C, Barba J. Occurrence, Serotype Diversity, and Antimicrobial Resistance of Salmonella in Ground Beef at Retail Stores in Jalisco State, Mexico. J Food Protect. 2013;76(12):2004–10. https://doi.org/10.4315/0362-028X.JFP-13-109.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S18), vol. 27; 2008. p. 188.
Clemente L, Manageiro V, Ferreira E, Jones-Dias D, Correia I, Themudo P, et al. Occurrence of extended-spectrum β-lactamases among isolates of Salmonella enterica subsp. enterica from food-producing animals and food products, in Portugal. Int J Food Microbiol. 2013;167:221–8. https://doi.org/10.1016/j.ijfoodmicro.2013.08.009.
European Committee on Antimicrobial Susceptibility Testing E. Breakpoint tables for interpretation of MICs and zone diameters. Version 2.0. In: European Committee on Antimicrobial Susceptibility Testing; 2012. p. 73.
Li Y-C, Pan Z-M, Kang X-L, Geng S-Z, Liu Z-Y, Cai Y-Q, et al. Prevalence, Characteristics, and Antimicrobial Resistance Patterns of Salmonella in Retail Pork in Jiangsu Province, Eastern China. J Food Protect. 2014;77(2):236–45. https://doi.org/10.4315/0362-028X.JFP-13-269.
Yu T, Jiang X, Zhou Q, Wu J, Wu Z. Antimicrobial resistance, class 1 integrons, and horizontal transfer in Salmonella isolated from retail food in Henan, China. J Infect Dev Ctries. 2014;8(6):705–11. https://doi.org/10.3855/jidc.4190.
Yoon R-H, Cha S-Y, Wei B, Roh J-H, Seo H-S, Oh J-Y, et al. Prevalence of Salmonella Isolates and Antimicrobial Resistance in Poultry Meat from South Korea. J Food Protect. 2014;77(9):1579–82. https://doi.org/10.4315/0362-028X.JFP-14-018.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S22), vol. 32; 2012. p. 188.
Ahmed AM, Shimamoto T, Shimamoto T. Characterization of integrons and resistance genes inmultidrug-resistant Salmonella enterica isolated from meat and dairy products in Egypt. Int J Food Microbiol. 2014;189:39–44. https://doi.org/10.1016/j.ijfoodmicro.2014.07.031.
Bacci C, Lanzoni E, Vismarra A, Alpigiani I, Nuvoloni R, Bonardi S, et al. Antibiotic resistance and resistance genes in Salmonella enterica isolated from pork meat and pig carcasses in northern Italy. Large Animal Rev. 2014;20:201–7.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing (CLSI M100-S17), vol. 27; 2007. p. 182.
Donado-Godoy P, Clavijo V, León M, Arevalo A, Castellanos R, Bernal J, et al. Counts, Serovars, and Antimicrobial Resistance Phenotypes of Salmonella on Raw Chicken Meat at Retail in Colombia. J Food Protect. 2014;77(2):227–35. https://doi.org/10.4315/0362-028X.JFP-13-276.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S23), vol. 33; 2013. p. 206.
Ta YT, Nguyen TT, To PB, Thi GN, et al. Quantification, Serovars, and Antibiotic Resistance of Salmonella Isolated from Retail Raw Chicken Meat in Vietnam. J Food Protect. 2014;77(1):57–66. https://doi.org/10.4315/0362-028X.JFP-13-221.
Yang B, Cui Y, Shi C, Wang J, Xia X, Xi M, et al. Counts, Serotypes, and Antimicrobial Resistance of Salmonella Isolates on Retail Raw Poultry in the People’s Republic of China. J Food Protect. 2014;77(6):894–902. https://doi.org/10.4315/0362-028X.JFP-13-439.
Department of Health and Human Service, Centers for Disease Control and Prevention C, Food and Drug Administratio F, United States Department of Agriculture U: National Antimicrobial Resistance Monitoring System (NARMS). 2011 Executive Report; 2011. p. 123.
Sodagari HR, Mashak Z, Ghadimianazar A. Prevalence and antimicrobial resistance of Salmonella serotypes isolated from retail chicken meat and giblets in Iran. J Infect Dev Ctries. 2015;9(5):463–9. https://doi.org/10.3855/jidc.5945.
Choi D, Chon J-W, Kim H-S, Kim D-H, Lim J-S, Yim J-H, et al. Incidence, Antimicrobial Resistance, and Molecular Characteristics of Nontyphoidal Salmonella Including Extended-Spectrum p Lactamase Producers in Retail Chicken Meat. J Food Protect. 2015;78(11):1932–7. https://doi.org/10.4315/0362-028X.
Donado-Godoy P, Byrne BA, Leon M, Castellanos R, Vanegas C, Coral A, et al. Prevalence, Resistance Patterns, and Risk Factors for Antimicrobial Resistance in Bacteria from Retail Chicken Meat in Colombia. J Food Protect. 2015;78(4):751–9. https://doi.org/10.4315/0362-028X.JFP-14-349.
Gharieb RM, Tartor YH, Khedr MHE. Non-Typhoidal Salmonella in poultry meat and diarrhoeic patients: prevalence, antibiogram, virulotyping, molecular detection and sequencing of class I integrons in multidrug resistant strains. Gut Path. 2015;7:34. https://doi.org/10.1186/s13099-015-0081-1.
Tirziu E, Lazar R, Sala C, Nichita I, Morar A, Ere M, et al. Salmonella in Raw Chicken Meat from the Romanian Seaside: Frequency of Isolation and Antibiotic Resistance. J Food Protect. 2016;78(5):1003–6. https://doi.org/10.4315/0362-028X.JFP-14-460.
Cai Y, Tao J, Jiao Y, Fei X, Zhou L, Wang Y, et al. Phenotypic characteristics and genotypic correlation between Salmonella isolates from a slaughterhouse and retail markets in Yangzhou, China. Int J Food Microbiol. 2016;222:56–64. https://doi.org/10.1016/j.ijfoodmicro.2016.01.020.
Amin HS, Abdelrahman AA, Abdellrazeq GS. Occurrence of multidrug-resistant Salmonella enterica in retail chicken meat and development of a six genes-based multiplex PCR as alternative diagnostic method. J Food Protect. 2016;36:459–66. https://doi.org/10.1111/jfs.12260.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S24), vol. 34; 2014. p. 230.
Niyomdecha N, Mungkornkaew N, Samosornsuk W. Serotypes and antimicrobial resistance of Salmonella enterica isolated from pork, chicken meat and lettuce, Bangkok and Central Thailand. Southeast Asian J Trop Med Public Health. 2016;47(1):31–9.
Thung TY, Mahyudin NA, Basri DF, Wan Mohamed Radzi CW, Nakaguchi Y, Nishibuchi M, et al. Prevalence and antibiotic resistance of Salmonella Enteritidis and Salmonella Typhimurium in raw chicken meat at retail markets in Malaysia. Poultry Sci. 2016;95(8):1888–93. https://doi.org/10.3382/ps/pew144.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for BacteriaIsolated from Animals (NCCLS M31-S1), vol. 24; 2004. p. 40.
Nghiem MN, Nguyen VT, Nguyen TTH, Nguyen TD, Vo TTB. Antimicrobial resistance gene expression associated with multidrug resistant Salmonella spp. isolated from retail meat in Hanoi, Vietnam. Int Microbiol. 2017;20(2):85–93. https://doi.org/10.2436/20.1501.01.288.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial SusceptibilityTesting (CLSI M100-S25), vol. 35; 2015. p. 240.
Moawad AA, Hotzel H, Awad O, Tomaso H, Neubauer H, Hafez HM, et al. Occurrence of Salmonella enterica and Escherichia coli in raw chicken and beef meat in northern Egypt and dissemination of their antibiotic resistance markers. Gut Path. 2017;9:57. https://doi.org/10.1186/s13099-017-0206-9.
Gad AH, Abo-Shama UH, Harclerode KK, Fakhr MK. Prevalence, Serotyping, Molecular Typing, and Antimicrobial Resistance of Salmonella Isolated From Conventional and Organic Retail Ground Poultry. J Food Protect. 2018;9:2653. https://doi.org/10.3389/fmicb.2018.02653.
Zhang L, Fu Y, Xiong Z, Ma Y, Wei Y, Qu X, et al. Highly Prevalent Multidrug-Resistant Salmonella From Chicken and Pork Meat at Retail Markets in Guangdong, China. Front Microbiol. 2018;9:2104. https://doi.org/10.3389/fmicb.2018.02104.
Nhung NT, Van NTB, Cuong NV, Duong TTQ, Nhat TT, Hang TTT, et al. Antimicrobial residues and resistance against critically important antimicrobials in non-typhoidal Salmonella from meat sold at wet markets and supermarkets in Vietnam. Int J Food Microbiol. 2018;266:301–9. https://doi.org/10.1016/j.ijfoodmicro.2017.12.015.
Thung TY, Radu S, Mahyudin NA, Rukayadi Y, Zakaria Z, Mazlan N, et al. Prevalence, Virulence Genes and Antimicrobial Resistance Profiles of Salmonella Serovars from Retail Beef in Selangor, Malaysia. Front Microbiol. 2018;8:2697. https://doi.org/10.3389/fmicb.2017.02697.
Zwe YH, Tang VCY, Aung KT, Alikiiteaga Gutierrez R, Ng LC, Yuk H-G. Prevalence, sequence types, antibiotic resistance and, gyrA mutations of Salmonella isolated from retail fresh chicken meat in Singapore. Food Contr. 2018;90:233–40. https://doi.org/10.1016/j.foodcont.2018.03.004.
Zhu A, Zhi W, Qiu Y, Wei L, Tian J, Pan Z, et al. Surveillance study of the prevalence and antimicrobial resistance of Salmonella in pork from open markets in Xuzhou, China. Food Contr. 2019;98:474–80. https://doi.org/10.1016/j.foodcont.2018.07.035.
Yang X, Wu Q, Zhang J, Huang J, Chen L, Wu S, et al. Prevalence, Bacterial Load, and Antimicrobial Resistance of Salmonella Serovars Isolated From Retail Meat and Meat Products in China. Front Microbiol. 2019;10:2121. https://doi.org/10.3389/fmicb.2019.02121.
de Jong A, Moyaert H, Simjee S. Antimicrobial susceptibility testing of foodborne Bacteria related to national and international resistance-monitoring programs. In: Barros-Velázquez J, editor. Antimicrobial food packaging. Brussels: CEESA, Academic; 2016. p. 117–28. https://doi.org/10.1016/B978-0-12-800723-5.00009-7.
Nassar MSM, Hazzah WA, Bakr WMK. Evaluation of antibiotic susceptibility test results: how guilty a laboratory could be? J Egypt Public Health Assoc. 2019;94(1):4. https://doi.org/10.1186/s42506-018-0006-1.
Kim H, Baek H, Lee S, Jang Y, Jung S, Kim A, et al. Prevalence and antimicrobial resistance of Salmonella spp. and Escherichia coli isolated from pigs at slaughterhouses in Korea. Afr J Microbiol Res. 2011;5(7):823–30. https://doi.org/10.5897/AJMR10.850.
World Health Organization Advisory Group on Integrated Surveillance of Antimicrobial Resistance A, Food and Agriculture Organization of the United Nations F, World Organisation for Animal Health O. Integrated surveillance of antimicrobial resistance in foodborne bacteria: Application of a one health approach: World Health Organization; 2017.
Jorgensen JH, Turnidge JD. Susceptibility test methods: dilution and disk difusión methods. In: Jorgensen JH, Pfaller MA, Carroll KC, Funke G, Landry ML, Richter SS, et al., editors. Manual of Clinical Microbiology: ASM Press; 2015. p. 1253–73.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests (CLSI M02-A13), vol. 38; 2018. p. 92.
Brown D, MacGowan A. Harmonization of antimicrobial susceptibility testing breakpoints in Europe: implications for reporting intermediate susceptibility. J Antimicrob Chemother. 2010;65:183–5. https://doi.org/10.1093/jac/dkp432.
Mensah N, Tang Y, Cawthraw S, AbuOun M, Fenner J, Thomson NR, et al. Determining antimicrobial susceptibility in Salmonella enterica serovar Typhimurium through whole genome sequencing: a comparison against multiple phenotypic susceptibility testing methods. BMC Microbiol. 2019;19:148. https://doi.org/10.1186/s12866-019-1520-9.
Doyle MP, Busta FF, Cords BR, Davidson PM, Hawke J, Hurd HS, et al. Antimicrobial resistance: implications for the food system. Compr Rev Food Sci Food Saf. 2006;5:71–137.
Hu Y, Matsui Y, Riley LW. Risk factors for fecal carriage of drug-resistant Escherichia coli: a systematic review and meta-analysis. Antimicrob Resist Infect Contr. 2020;9:31. https://doi.org/10.1186/s13756-020-0691-3.
Murray AK. The Novel Coronavirus COVID-19 Outbreak: Global Implications for Antimicrobial Resistance. Front Microbiol. 2020;11:1020. https://doi.org/10.3389/fmicb.2020.01020.
Haque M, Dutta S. COVID-19: Questions of Antimicrobial Resistance. Bangladesh J Med Sci. 2021;20(2):221–7. https://doi.org/10.3329/bjms.v20i2.51527.
Jajere SM. A review of Salmonella enterica with particular focus on the pathogenicity and virulence factors, host specificity and antimicrobial resistance including multidrug resistance. Vet World. 2019;12(4):504–21. https://doi.org/10.14202/vetworld.2019.504-521.
Acknowledgments
Authors thank María Lucía Gutiérrez, Ph.D., for English editing.
Funding
This research (“Definición de un plan integral de intervención y mitigación con visión de cadena productiva en empresas de derivados cárnicos localizadas en Boyacá”) was funded by “Departamento Administrativo de Ciencia, Tecnología e Innovación” (COLCIENCIAS) Boyacá, Colombia throuhg contract No. FP 44842–186-2017 with “Pontificia Universidad Javeriana”, (PUJ), Bogotá, D.C. Colombia. Financing entity had no role in the study design, data collection or analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: Raúl A. Poutou-Piñales. Analyzed and interpreted the data: Sandra M. Rincón-Gamboa, Raúl A. Poutou-Piñales, Ana K Carrascal-Camacho. Wrote the paper: Sandra M. Rincón-Gamboa, Raúl A. Poutou-Piñales. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors agree with the publication of this systematic review.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 2:.
A. Selected articles relationship between year of the isolation Vs. Standard used. B. Selected articles relationship between Submission article year Vs. Standard used. C. Selected articles relationship between publication article year Vs. Standard used [16, 17, 19, 23, 27, 31, 34, 37, 39, 41, 44, 46, 47, 52, 56,57,58, 60, 61, 63, 65, 68,69,70,71, 73, 74, 76, 79, 81,82,83,84,85,86,87,88]
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rincón-Gamboa, S.M., Poutou-Piñales, R.A. & Carrascal-Camacho, A.K. Analysis of the assessment of antimicrobial susceptibility. Non-typhoid Salmonella in meat and meat products as model (systematic review). BMC Microbiol 21, 223 (2021). https://doi.org/10.1186/s12866-021-02268-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-021-02268-1