Abstract
A 47-year-old woman with hypertension and rheumatoid arthritis presented with non-necrotizing scleritis in both eyes. Despite a course of oral corticosteroids, she continued to experience persistent symptoms. A rheumatologist was consulted and initiated treatment with tofacitinib, a JAK/STAT inhibitor. Treatment with tofacitinib and oral corticosteroids resulted in an improvement in the scleritis in both eyes. However, a fundus examination of her left eye revealed a superior-temporal branch retinal vein occlusion. Given the growing concern regarding the increased risk of thromboembolic events with tofacitinib therapy, it is essential to consider the risk of retinal vascular occlusions when starting tofacitinib therapy, particularly in patients with underlying systemic comorbidities.
Similar content being viewed by others
Introduction
The treatment of non-infectious scleritis involves the use of corticosteroids and immunosuppressive agents in a stepwise manner. The severity of the scleral inflammation, response to the treatment, and the underlying cause guide the treatment regime in these patients. Despite conventional therapies, some cases of non-infectious scleritis remain refractory, leading to an unmet need for alternative treatment options. In recent years, biological agents have shown promise in the management of non-infectious scleritis. These agents target specific pathways or components of the immune system and have been shown to be effective in reducing inflammation. Additionally, a new class of immunomodulatory agents that inhibit Janus kinase signal transducer and activator of transcription (JAK-STAT), an intracellular signaling pathway, has been introduced in the management of various systemic rheumatic diseases. JAK inhibitors have shown efficacy in the treatment of various autoimmune and inflammatory disorders, including rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Tofacitinib, a JAK inhibitor, has been recently employed in the management of treatment-resistant cases of uveitis and scleritis. While there are reports of thromboembolic events associated with the use of tofacitinib, no cases of retinal vascular occlusion suggesting a possibility of thromboembolic episodes inside the eye have been reported. We present a case of branch retinal vein occlusion (BRVO) in a patient with diffuse non-infectious non-necrotizing scleritis who was treated with tofacitinib. Tofacitinib, a JAK inhibitor, has recently been used to treat treatment-resistant cases of uveitis and scleritis. While thromboembolic events have been reported with its use, there have been no reports of tofacitinib-associated retinal vascular occlusion, which suggests the possibility of thromboembolic episodes occurring inside the eye.
Case report
A 47-year-old female with a history of hypertension and rheumatoid arthritis presented to our clinic with complaints of ocular pain and redness in both eyes. She was already being treated by a rheumatologist and was taking hydroxychloroquine 400 mg once daily. She had previously sought care elsewhere for her eye problem, where she was diagnosed with scleritis and treated with systemic corticosteroids. Her laboratory investigations, which were conducted elsewhere, revealed a negative Mantoux test, negative antinuclear antibody (ANA) and antineutrophil cytoplasmic antibody (ANCA) results. She was also under the care of an internist at her place of residence, who was monitoring her hypertension with routine laboratory tests and antihypertensive medications.
At the presentation to us, her best corrected visual acuity (BCVA) was 6/6 in both eyes, with intraocular pressure measured by applanation tonometry was 10 mm of hg in both eyes. Slit lamp examination of both eyes revealed diffuse deep episcleral congestion and scleral edema, with a quiet anterior chamber (Fig. 1a and b). Anterior segment optical coherence tomography confirmed the findings with an increased scleral thickness corresponding to areas of scleral inflammation in both eyes. Fundus examination of both eyes was unremarkable. A diagnosis of active non-necrotizing anterior scleritis was made, and consultation from a rheumatologist was sought to rule out systemic rheumatic diseases and initiate immunomodulatory therapy.
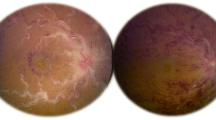
The patient was started on oral tofacitinib 5 mg twice daily, along with tapering doses of oral steroids. A follow-up visit after two months revealed complete resolution of scleral inflammation in both eyes. Her BCVA was 6/6 in both eyes, and intraocular pressure was 12 mm of Hg in both eyes. Fundus examination of the left eye revealed scattered superficial retinal haemorrhages with few cotton wool spots along the superior-temporal arcade with tortuous vessels (Fig. 2). Fundus examination of the right eye was unremarkable. Optical coherence tomography was normal in both eyes. No evidence of neovascularization was seen in fundus fluorescence angiography. The patient was advised to stop tofacitinib and was started on mycophenolate mofetil 1 gram twice daily and oral steroids in tapering doses. The patient was advised to come for a review after one month.
Discussion
Tofacitinib, an oral small-molecule Janus kinase inhibitor, has been reported by several authors, including our group, to be effective in treating scleritis at a dosage of 5 mg twice daily [1,2,3]. The drug has been approved by US Food and Drug Administration (FDA) for the treatment of rheumatoid arthritis (RA), psoriatic arthritis, and ulcerative colitis. Our patient was started on oral tofacitinib before using conventional immunosuppressives. Several studies have highlighted the effectiveness of tofacitinib as monotherapy, and there has been an increasing trend in the use of the drug in the management of RA in recent years [4]. However, the FDA has issued a warning about the increased risk of blood clots and death in patients with rheumatoid arthritis who were treated with a 10 mg twice-daily dose of tofacitinib. This warning was based on interim data from an ongoing safety study that showed a higher risk of pulmonary embolism and overall mortality in patients receiving the higher dose compared to those receiving a TNF inhibitor [5]. The risk was found to be higher in patients over 50 years old, with a history of cardiovascular disease, or receiving high doses of corticosteroids [6]. Patients with pre-existing thromboembolic risk factors, such as those on prothrombotic or antithrombotic treatments, were also found to be at increased risk of thromboembolic episodes with the use of tofacitinib [7]. Also, long-standing inflammatory systemic disorders, increased age, and traditional cardiovascular risk factors such as obesity, diabetes, hypertension, hyperlipidemia, and smoking, further increased the risk of thrombosis [8]. Other adverse events associated with the use of tofacitinib include increased risk of herpes zoster infection, [9] reactivation of tuberculosis, [10] malignancy, [11] increased levels of liver transaminases, and serum lipid derangements [12]. The index case presented with diffuse active scleral inflammation, along with a history of rheumatoid arthritis and systemic hypertension. Given the severity of the inflammation, its resistance to systemic corticosteroid treatment, and the patient’s underlying systemic disease, both a rheumatologist and ophthalmologist decided to begin tofacitinib therapy. Tofacitinib has been found to be helpful in the management of treatment-resistant cases of scleritis [1,2,3]. At our setup, the drug is often preferred over the TNF-alpha agents, particularly by the patients, as it is cheaper and available as oral formulation. The tofacitinib therapy was successful in resolving the scleral inflammation, but unfortunately, the patient developed superior-temporal BRVO. It is difficult to determine the exact cause of this event, particularly given the presence of systemic hypertension in the patient. However, it is worth noting that the patient was receiving regular medical care and was closely monitored by an internist. Nevertheless, the potential risk of ocular thromboembolic events must be considered when initiating tofacitinib therapy, particularly in patients with systemic comorbidities.
Availability of data and materials
Not relevant.
References
Pyare R, Kaushik V, Dutta Majumder P, Biswas J (2020) Tofacitinib in recalcitrant scleritis: first case report from India. Indian J Ophthalmol 68(9):1988–1990. https://doi.org/10.4103/ijo.IJO_534_20
Paley MA, Karacal H, Rao PK, Margolis TP, Miner JJ (2019) Tofacitinib for refractory uveitis and scleritis. Am J Ophthalmol Case Rep 13:53–55. https://doi.org/10.1016/j.ajoc.2018.12.001
Pyare R, Dutta Majumder P, Shah M, Kaushik V, Agarwal M, Biswas J (2022) Tofacitinib in Scleritis: a Case Series. Ocul Immunol Inflamm Published online September 20:1–7. https://doi.org/10.1080/09273948.2022.2113805
Dhillon S, Tofacitinib (2017) A review in rheumatoid arthritis. Drugs 77(18):1987–2001. https://doi.org/10.1007/s40265-017-0835-9
Pfizer (2023) PHASE 3B/4 Randomized safety endpoint study of 2 doses of tofacitinib in comparison to a tumor necrosis factor (TNF) INhibitor in subjects with rheumatoid arthritis. clinicaltrials.gov; 2021. Accessed April 3, https://clinicaltrials.gov/ct2/show/NCT02092467
Ytterberg SR, Bhatt DL, Mikuls TR et al (2022) Cardiovascular and Cancer Risk with Tofacitinib in Rheumatoid Arthritis. N Engl J Med 386(4):316–326. https://doi.org/10.1056/NEJMoa2109927
Thromboembolic Safety Reporting of Tofacitinib and Baricitinib: An Analysis of the WHO VigiBase - PubMed. Accessed 5 April 2023. https://pubmed.ncbi.nlm.nih.gov/32533433/
Mori S, Ogata F, Tsunoda R (2021) Risk of venous thromboembolism associated with Janus kinase inhibitors for rheumatoid arthritis: case presentation and literature review. Clin Rheumatol 40(11):4457–4471. https://doi.org/10.1007/s10067-021-05911-4
Winthrop KL, Baddley JW, Chen L et al (2013) Association between the initiation of anti-tumor necrosis factor therapy and the risk of herpes zoster. JAMA 309(9):887–895. https://doi.org/10.1001/jama.2013.1099
Curtis JR, Xie F, Yun H, Bernatsky S, Winthrop KL (2016) Real-world comparative risks of herpes virus infections in tofacitinib and biologic-treated patients with rheumatoid arthritis. Ann Rheum Dis 75(10):1843–1847. https://doi.org/10.1136/annrheumdis-2016-209131
Curtis JR, Lee EB, Kaplan IV et al (2016) Tofacitinib, an oral Janus kinase inhibitor: analysis of malignancies across the rheumatoid arthritis clinical development programme. Ann Rheum Dis 75(5):831–841. https://doi.org/10.1136/annrheumdis-2014-205847
Wollenhaupt J, Silverfield J, Lee EB et al (2014) Safety and efficacy of tofacitinib, an oral janus kinase inhibitor, for the treatment of rheumatoid arthritis in open-label, longterm extension studies. J Rheumatol 41(5):837–852. https://doi.org/10.3899/jrheum.130683
Acknowledgements
Nil.
Funding
The authors declare no financial interest or receiving any funding.
Author information
Authors and Affiliations
Contributions
JB and AM treated the patient. HA, PDM helped in manuscript preparation, JB Supervised the entire process.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not relevant.
Consent for publication
This paper has never been submitted to any journal nor published in any form of media before. Authors provide consent for publication into the journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manoharan, A., Atmakur, H., Dutta Majumder, P. et al. Branch retinal vein occlusion in a case of recalcitrant diffuse anterior scleritis treated with tofacitinib. J Ophthal Inflamm Infect 13, 45 (2023). https://doi.org/10.1186/s12348-023-00359-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-023-00359-w